surgical site infection
What is surgical site infection? Discuss the methods to reduce surgical site infection. Enumerate the factors responsible for surgical site infection.Nosocomial Infection An infection acquired in hospital by a patient who was admitted for a reason other than that infection .Infections occurring for more than 48 hours after admission are usually considered nosocomial Amongst surgical patients, SSI are the most common nosocomial infections
Classes of SSI Superficial incisional SSI: Infection occurs within 30 days after the operation and infection involves only skin of subcutaneous tissue of the incision and at least one of the following: –1–Purulent drainage with or without laboratory confirmation from the superficial incision –2–Organisms isolated from an aseptically obtained culture of fluid or tissue from the superficial incision
–3–At least one of the following signs or symptoms of infection: --Pain or tenderness --Localised swelling --Redness --Heat --And superficial incision deliberately opened by a surgeon, unless incision is culture negative
Deep incisional SSI: Infection occurs within 30 days after the operation if no implant is left in place or within one year if implant is in place and the infection appears to be related to the operation and infection involves deep soft tissues (e.g. fascial and muscle layers) of the incision and at least one of the following:
–1–Purulent drainage from the deep incision but not from the organ/space component of the surgical site –2–A deep incision spontaneously dehisces or is deliberately opened by a surgeon when the patient has at least one of the following signs or symptoms: --Fever (>38°C) --Localized pain --Tenderness unless site is culture-negative –3–An abscess or other evidence of infection involving the deep incision is found on direct examination, during re-operation or by histopathological or radiological examination
Organ/space SSI: Infection occurs within 30 days after the operation if no implant is left in place or within one year if implant is in place and the infection appears to be related to the operation and infection involves any part of the anatomy (e.g. organs or spaces), other than the incision, which was opened or manipulated during an operation and at least one of the following:
–1–Purulent discharge from a drain that is placed through a stab wound into the organ/ space –2–Organisms isolated from an aseptically obtained culture of fluid or tissue in the organ/space –3–An abscess or other evidence of infection involving the organ/space that is found on direct examination, during re-operation, or by histopathologic or radiological examination
Strategies to prevent SSI Objectives 1-Reduce the inoculum of bacteria at the surgical site 2-Surgical site preparation 3-Antibiotic prophylaxis strategies 4-Optimize the microenvironment of the surgical site 5-Enhance the physiology of the host (host defenses)
risk factors of SSI classified as: 1-Patient-related (intrinsic) 2-Preoperative 3-Operative
Patient-related factors a-Diabetes—recommendation Preoperative Control serum blood glucose—reduce HbA1C levels to <7% before surgery if possible Maintain the postoperative blood glucose level at less than 200 mg/dL b-Smoking, anemia, malnutrition c-Hypoalbuminemia, jaundice d-Obesity, hyperlipidemia e-Ascites, PVD f-Immunosupression.
2-Procedure-related risk factors a-Hair removal technique (clipping> on table shaving > previous night shaving) b-Preoperative infections control and bath c-Surgical scrub d-Skin preparation e-Antimicrobial prophylaxis f-Surgeon skill/technique/instruments g-Asepsis h-Operative time (should be within 1.5 times the normal) j-Operating room characteristics/OT sterility.
Surgeon skill and technique Excellent surgical technique reduces the risk of SSI Includes a-Gentle traction and handling of tissues b-Effective hemostasis c-Removal of devitalized tissues d-Obliteration of dead spaces e-Irrigation of tissues with saline during long procedures f-Use of fine, nonabsorbed monofilament suture material h-Wound closure without tension.
CellulitisCellulitis is a common infection of skin and subcutaneoustissues, most frequently caused by Streptococcuspyogenes and occasionally Staphylococcus species. Infectionoccurs after the skin is breached (e.g. insect bite,scratching, skin rash, minor trauma).
Cellulitis mayseem to occur spontaneously, although careful inspectionreveals a break in the skin After subcutaneous inoculation,streptococci release toxins which permit rapid spreadof organisms. The acute inflammatory response resultsin the clinical features of warmth, pain and tenderness,erythema, and oedema. Severe cellulitis may progressto suppuration and skin necrosis.
Differential diagnosis includes other causes of limbswelling, deep venous thrombosis, rupture of a Baker’scyst, calf haematoma and erythematous skin conditions.
excretion of penicillin. Erythromycin or a third generationcephalosporin is used in patients with penicillinallergy. Any predisposing cause (e.g. tinea pedis) istreated vigorously. If cellulitis does not resolve rapidly,the antibiotic is increased or changed.
LymphangitisLymphangitis is associated with bacterial infections ofextremities where the inflamed lymphatic vessels appearas several thin, red, tender lines on the slightlyoedematous skin progressing towards the regionallymph nodes which are enlarged and tender (lymphadenitis).
Cellulitis of an extremity is treated by elevation andimmobilisation with a splint or plaster ‘back slab’, andantibiotics. Penicillin (2 million units every 6 hours)or flucloxacillin (1–2 g every 6 hours) is given intravenouslyfor 3–5 days and then continued orallyfor a further 10 days. Blood levels of penicillin maybe increased by oral probenecid, which reduces renal
Lymphangitis usually is caused by streptococciand staphylococci. Chemical lymphangitis mayresult from irritative compounds used for lymphangiography.
Treatment is the same as for cellulitis, consistingof rest and elevation of the extremity and antibiotics.Rarely, suppurative regional lymph nodes require surgicaldrainage.
Folliculitis, furuncles and carbuncles‘Folliculitis’ refers to infection with pus formationwithin a hair follicle and is limited to the dermis. Itmay be extensive if many follicles are infected over awide area, such as the face.
A ‘furuncle’ is infection of a small number of hairfollicles within a small confined area. A ‘carbuncle’ isan abscess involving a number of adjacent hair follicleswhere the infection has penetrated through the dermisand formed a multiloculated subcutaneous abscess betweenthe fibrous septa which anchor the skin to thedeep fascia
Furuncles and carbuncles occur most frequentlyon the back of the neck, lower scalp, and the torso. Abscesses on the upper part of the body are usuallycaused by staphylococci, while infections belowthe umbilicus are due largely to aerobic and anaerobiccoliform organisms.
Local hygiene is usually sufficient to treat folliculitis,although antibiotics are required for extensive infections.Furuncles and carbuncles require incision anddrainage. Fibrous tissue septa must be broken downso that all pockets of pus can be drained completely.Antibiotics are indicated for severe and spreading infections,and in immunocompromised patients.
Hidradenitis suppurativaHidradenitis suppurativa refers to infection of apocrinesweat glands, and occurs in the axillae, around the externalgenitalia, and the inguinal and perianal regions
Apocrine sweat glands have tortuoussecretory ducts within the skin and produce thicksecretions, and infection occurs when ducts becomeblocked, most commonly during excessive glandularactivity at adolescence.Staphylococci or Gramnegativebacilli and anaerobes are causative organisms.
Patients present with multiple small but painfulabscesses and sinuses, often bilaterally. Repeated orlong-standing infection results in considerable scarring,
Antibiotic therapy alone isoften inadequate, although long-term antibiotic therapymay be useful in suppressing acute infections. Abscessesrequire incision and drainage. Excision of theaffected hair-bearing area and the subcutaneous fatusually is required, and results in good symptomaticrelief.
Synergistic gangrene‘Synergistic gangrene’ refers to a group of soft tissueinfections characterised by tissue necrosis and caused by severalspecies of microorganisms acting synergistically. Previousnomenclature (necrotising fasciitis, necrotisingerysipelas, Meleney’s gangrene, Fournier’s gangrene,non-clostridial gangrenous cellulitis)
Clinical featuresSynergistic gangrene is caused by micro-aerophilicstreptococci acting synergistically with aerobic staphylococci,with or without Gram-negative bacilli. It usuallyoccurs in debilitated patients with other disorders(e.g. diabetes, malnutrition, alcoholism, liver disease,renal failure, malignant disease, immune compromise).
Synergistic gangrene presents initially as cellulitiswith severe pain which is out of keeping with the minorlocal clinical signs but consistent with the seriousnessof the condition. Infection spreads rapidly along fascial and subcutaneous planes without a severe inflammatory reaction.
Bacterial toxins cause tissue and skinnecrosis. Crepitus occurs when gas-forming organismsare present. Signs of systemic sepsis and toxaemia occurquickly.‘Fournier’s gangrene’ is the name given to synergistic gangrene involving the perineum and scrotum. Itmay be extensive and involve the abdominal wall andbuttocks, and is a rare complication of anorectal andperineal surgery, trauma or minor infection.
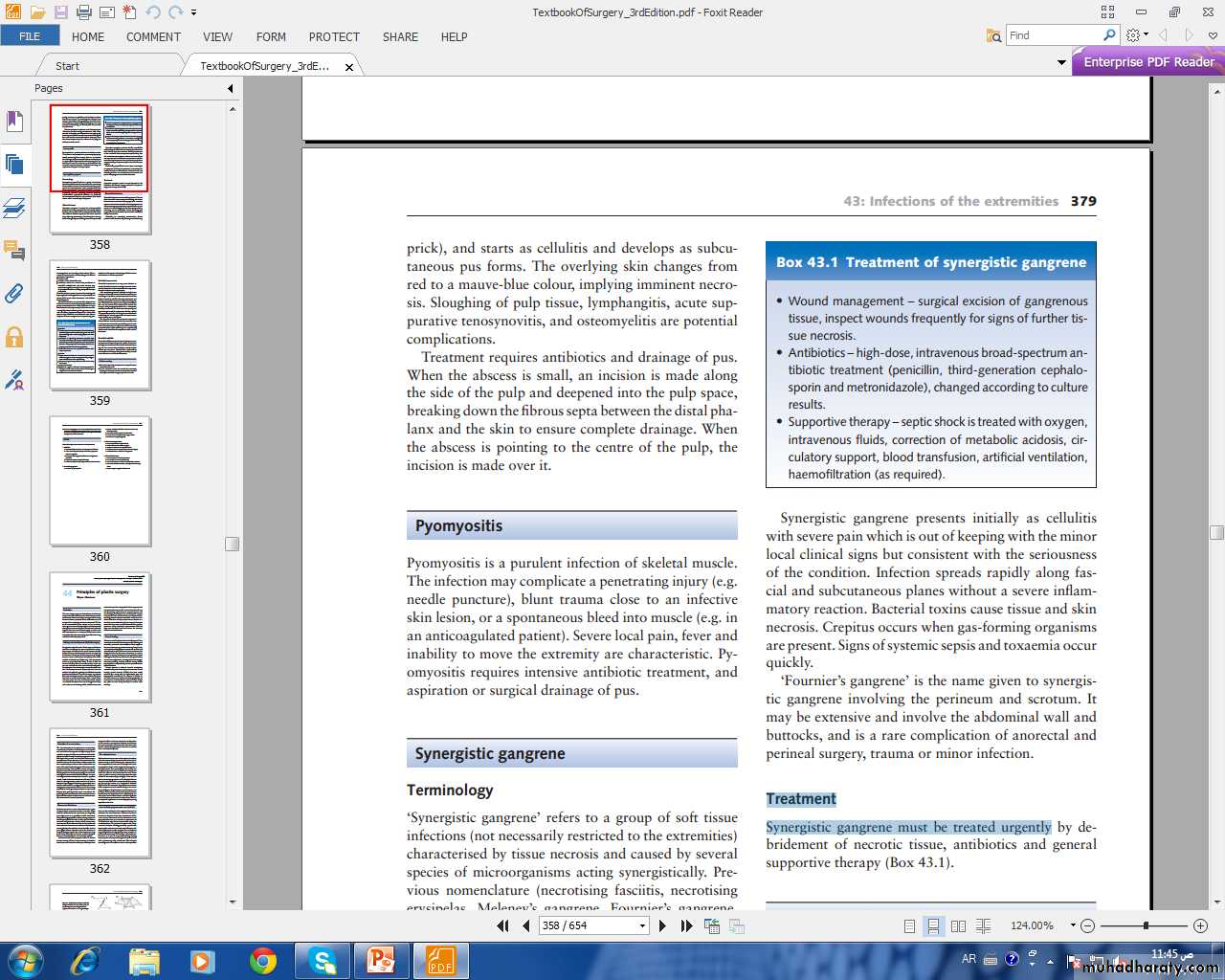
TreatmentSynergistic gangrene must be treated urgently by
Select the single correct answer to each question.1:Cellulitis:a-is occasionally caused by Gram-negative coliformsb-often occurs spontaneously without any apparentcause or organismc- is treated with rest, immobilisation and high-dosepenicillind-frequently requires surgical drainagee-is often complicated by suppuration and skin necrosis2:Fournier’s gangrene:a-is a form of pyomyositisb-occurs mainly in debilitated patients and can belife-threateningc -is usually due to stapylococcal infectiond-can be treated by hyperbaric oxygen alonee-is seldom managed surgically