1
2

3
Lec:6
Surgery
Hematuria
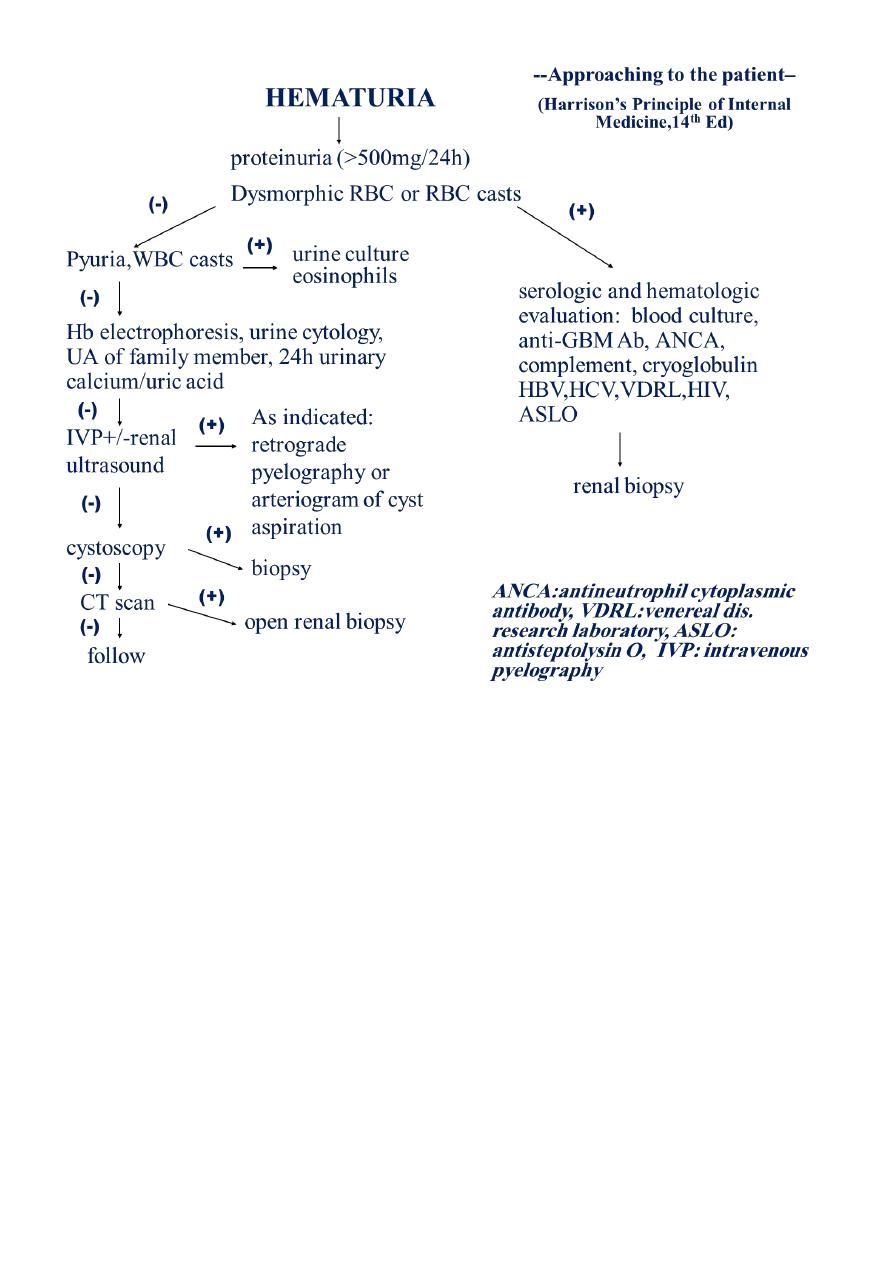
DEFINITION
More than three red blood cells are found in
centrifuged urine per high-power field microscopy
( > 3 RBC/HP).
Normal urine:
no red blood cell or less than three red blood cell
According to the amount of RBC in the urine, hematuria can be classified as:
microscopic hematuria: normal colour with eyes
gross hematuria: tea-colored, cola-colored, pink or even red
ETIOLOGY
#Diseases of the urinary system—the most common cause
a. Vascular
arteriovenous malformation
arterial emboli or thrombosis
arteriovenous fistular
nutcracker syndrome
renal vein thrombosis
loin-pain hematuria syndrom
cogulation abnormality
excessive anticogulation
b. Glomerular
IgA nehropathy
thin basement membrane disease (incl.Alport syndrome)
other causes of primary and secondary glomerulonephritis
c. Interstitial
allergic interstitial nephritis
analgesic nephropathy
renal cystic diseases

4
acute pyelonephritis
tuberculosis
renal allograft rejection
d. Uroepithelium
malignancy
vigorous excise
trauma
papillary necrosis
cystitis/urethritis/prostatitis(usually caused by infection)
parasitic diseases (e.g. schistosomiasis)
nephrolithiasis or bladder calculi
e. Multiple sites or source unknown
hypercalciuria
hyperuricosuria
#System disorders
a. Hematological disorders
aplastic anemia leukemia
allergic purpura hemophilia
ITP (idiopathy thrombocytopenic purpura)
b. Infection
infective endocarditis
septicemia
epidemic hemorrhagic fever (Hantaan virus)
scarlet fever (
-hemolytic streptococcus)
leptospirosis (leptospire)
filariasis (Wuchereria bancrofti, Brugia malayi)
c. Connective tissue diseases
systemic lupus erythematosus (SLE)
polyarteritis nodosa
d. Cariovascular diseases
hypertensive nephropathy
chronic heart failure
renal artery sclerosis
e. Endocrine and metabolism diseases
gout
diabetes mellitus

5
#Diseases of adjacent organs to urinary tract
appendicitis salpingitis
carcinoma of the rectum
carcinoma of the colon
uterocervical cancer
#Drug and chemical agents
sulfanilamides anticogulation
cyclophosphamide mannitol
#miscellaneous
exercise “idopathic” hematuria
CLINICAL FEATURE
Color
depends on the amount of red blood cell in the urine and the pH (see slide 4)
normal: light yellow, pH 6.5
pH acidic: more darker (brown or black) // alkaline: red
DIFFERENTIAL DIAGNOSIS
Polluted urine: menstruation
Drug and food: phenosulfonphtha lein (PSP),uric acid, vegetable
Porphyrism: porphyrin in urine (+)
Hemoglobinuria
hemolysis
soy-like, very few RBC under the microscopy
occult blood test (+)
HEMOGLOBINURIA
RBC abnormality
Defects of RBC membrane structure and function (hereditary spherocytosis)
Deficiency of enzymes (favism)
Hemoglobinopathy (thalassemia)
PNH
6
Mechanical factor (artificial heart valve), infection
or mismatched blood transfusion
LABORATORY TESTS
#Three-glass test
Method: collecting the three stages of urine of a patient during micturition
Result:
the initial specimen containing RBC—the urethra
the last specimen containing RBC—the bladder neck and trianglar area,
posturethra
all the specimens containing RBC—upper urinary tract, bladder
#Phase-contrast microscopy
To distinguish glomerular from post glomerular bleeding
post glomerular bleeding: normal size and shape of RBC
glomerular bleeding: dysmorphic RBC (acanthocyte)
ACCOMPANIED SYMPTOMS
Hematuria with renal colic
o renal stone, ureter stone
o if with dysuria, miction pause or staining to void: bladder or urethra stone
Hematuria with urinary frequency,urgency and dysuria
o bladder or lower urinary tract (tuberculosis or tumor)
o if accompanied by high spiking fever, chill and loin pain: pyelonephritis
Hematuria with edema and hypertension
o glomerulonephritis
o hypertensive nephropathy
Hematuria with mass in the kidney
o neoplasm
o hereditary polycystic kidney
Hematuria with hemorrhage in skin and mucosa
o hematological disorders
o infectious diseases
Hematuria with chyluria
o filariasis
7

8

9
Lec:7
Surgery
Trauma in Urology
#Renal injuries
RI account for 1-5% of all traumas
BLUNT – car, sport accidents –majority!
PENETRATING –gunshots, stab wounds
AAST classification
(American Associaton for the Surgery of Trauma)
1. Contusion, non-expanding subcapsular haematoma, no laceration
2. Non-expanding perirenal haematoma, cortical laceration < 1 cm deep, no urinary
extravasation
3. cortical laceration > 1cm, no u.extravasation
4. Laceration: through corticomedullary junction into collecting system OR vascular:
segm. renal artery or vein injury with contained haematoma
5. Shattered kidney OR major vascular injury (renal pedicle injury or avulsion)
1,2 = minor injuries – 85-95% 3,4,5 = major injuries
Diagnosis
Trauma history, past renal injury, surgery or renal abnormalities
examination (haematuria, flank pain, flank abrasions, rib fractures, abd.tenderness)
Urinalysis, blood count, creatinine
Primary imaging -> USG!!
Enhanced abdominal CT !
Intraoperative one/shot IVP
Second/line imaging – MRI,Scinti,Angiography
Treatment
WW – grade I-III in stable patients
Surgery (all penetrating injuries, in blunt injuries if: major blood loss, unstable
patient, urinary extravasation, nonviable kidney, pedicle avulsion,...)
Complications
1. Early: Haemorrhage, retroperitoneal urinoma, haematoma, abscess
2. Late: Hypertension, AV fistula, calculi, PNF, late bleeding

11
#Ureteral injuries
1. Pelvic surgery (uro, gyn, gen.s.)
2. Pelvic/abdomninal masses
3. PID
4. post RT
5. Penetrating injury
Clinical findings
Flank pain, tenderness
Sepsis
Hydronephrosis
Paralytic ileus
VV / UV fistula / watery discharge via vagina
Labs /CRP,Leu,urinalysis,creatinine
Imaging
1. USG
2. IVU / enhanced CT !
3. APG
4. Radionuclide scanning
Treatment
1. First-line urinary diversion !!! (nephrostomy, ureteral stenting)
2. Reconstructive surgery /reanast., reimpl., substitutions, crossed diversion,
autoTPL…/
#Bladder injuries
1. direct external force, road accidents
2. iatrogenic / gyn-obs, uro, sur/
3. intraperitoneal disruption
4. extraperitoneal disruption
Clinical finding
Haematuria
Pelvic , abd. pain (pelvic fracture presented in 90% of bladder inj.)

11
Haemorrhage, Shock
Acute abdomen !!! (intraperit)
Imaging
1. Pelvic & Abdominal USG
2. Cystography (300ml) !
3. CT cystography
Treatment
1. Extraperit. – bladder drainage (epi, catheter)
2. Intraperit. – open surgery required!
#Urethral injuries
1. Posterior/ Anterior urethra
2. Laceration, transection, contusion
3. External forces (falls astride an object, perineal blow, …)
4. Iatrogenic (catheter, uro )
Posterior urethra
assoc. w/ pelvic fractures - > prostate avulsion from the membranous u. -> apical
displacement of the prostate - > Pelvic urinoma, haematoma
Diagnostic radiology (DR Exam.) :
1. blood at the urethral meatus
2. X- Ray (pelvic fracture)
3. Urethrography
Treatment
1. drainage (suprapubic cystostomy)
2. immediate surgery (suspected bladder lacerations, disruptions, massive pelvic
bleeding, etc.)
3. delayed surgery (>3 months after the injury)
Complications after delayed surg.repair
1. ED 30-35%
2. Incontinence 5%
3. Stricture 5%

12
Anterior urethra
1. straddle injury
2. iatrogenic instrumentations
3. self-instrumentations
Clinical findings
perineal, penile, scrotal haematoma
urethral bleeding
normal DRE
Diagnosis:
by
Urethrography
Treatment
1. suprapubic cystostomy
2. surgical repair (in case of urethral laceration, bleeding w/o extravasation)
3. follow-up (stricture!)
#Penile & Scrotal injuries
1. Penile fracture (sex. intercourse -> disruption of the tunica albuginea -> haematoma,
CAVE: urethral injury)
2. Penile constriction – rings
3. Penile amputation
4. Scrotal injury (hematocele, testicular disruption, torsion, skin avulsion, traumatic
amputations)

13
Lec:8
Surgery
Neurogenic bladder
NEUROGENIC BLADDER
Description of NB
Dysfunction of the urinary bladder due to disease of the central nervous system or
peripheral nerves involved in the control of micturition.
Epidemiology
Prevalence of voiding dysfunction (VD) is reported for specific conditions:
1. Cerebrovascular accident: 20-50%
2. Parkinson disease: 35-70%
3. Multiple sclerosis: 50-90%
4. Diabetes mellitus: 5-60%
Risk factors
1. Neurologic disease, injury, or congenital malformation
2. DM
3. Radical pelvic surgery
Genetics
Genetic diseases that may be associated with NB include:
1. Muscular dystophy
2. Hereditary spastic paraplegia
3. Neurofibromatosis
4. Familial dysautonomia
Classification of Neurogenic Bladder
Most often done using urodynamic classification scheme:
1. Neurogenic DO (hyperreflexia): uncontrolled reflex bladder contraction
o Loss of inhibitory impulses from cortical centers; primitive reflex pathways
2. Detrusor underactivity (areflexia):
o Interruption of sacral reflex arc; no detrusor contraction
o Typically low-pressure storage of high volume up to 500 ml

14
3. DSD: abnormal reflexive sphincter contraction during involuntary detrusor
contraction
o Functional BOO, elevated intravesical pressure
o Secvondary damage: pressure, infection, urolithiasis
Pathophysiology
Voiding center include:
Higher centers (suprapontine):
o Function: inhibit sacral micturition center
o Predicted type of VD with suprapontine lesion would be detrusor overactivity (DO)
due to loss of inhibition on sacral micturition center
Pontine micturition center (PMC):
o Function: coordinates sphincter relaxation during bladder contraction
o Predicted type of VD with lesion between pontine and sacral micturition center is DO
and detrusor-sphinecter dyssynergia (DSD)
Sacral micturition center (SMC):
o Function: mediates reflex and voluntary bladder contraction
o Predicted type of VD with lesion of SMC is detrusor underactivity or areflexia
Peripheral lesions: VD is variable including:
1. Detrusor underactivity
2. Impaired bladder sensation
3. Impaired sphincteric function
o Upper motor neuron lesion: spastic, uninhibited: injury above spinal cord micturition
center
o Lower motor neuron lesion: flaccid, atonic, areflexic: injury in the pelvic nerves or
spinal micturition center
o Spinal shock: Immediately after injury, regardless of the level, there is a stage of
flaccid paralysis with numbness below the level of the injury that lead to bladder
overfilling to the point of overflow incontinence & rectal impaction. It lasts few
weeks up to 6 months .
o Autonomic dysreflexia (AD): A potentially life threatening condition that can cause
rapid, extreme BP elevation, headache, diaphoresis, bradycardia, sweating, nausea
and piloerection in patients with spinal cord lesions at and above the 6th thoracic
15
vertebral level (T6). Causes: noxious stimulus below the level of injury such as:
bladder distention, bowel distention, or pain activate sympathetic neurons causing
unopposed reflex sympathetic activity
Commonly associated conditions
A. CNS diseases:
1. CVA
2. SCI
3. TM
4. MS
5. PD
6. Normal-pressure hydrocephalus
B. PNS disease:
1. Radical pelvic surgery:
2. AP resection
3. radical hysterectomy
4. DM
5. IDP
6. Spinal stenosis
7. GB syndrome
C. Neural tube defects (NTD)
D. Static disorders of development: as CP
Diagnosis
History:
1. Voiding symptoms:
o Irritative or obstructive
o UI: urge, stress
o Spastic Neuropathic Bladder:
The severity of symptoms depends on the site and extent of the lesion as well as
the length of time from injury.
OAB syndrome: urinary urgency with or without UUI, usually associated with
frequency and nocturia

16
o Flaccid (Atonic) Bladder:
principal urinary symptom is urine retention with overflow incontinence. Male
patients lose their erections.
Extremity reflexes are hypoactive or absent. Sensation is diminished or absent
2. History of any risk factor:
neurologic disease: onset, duration
DM
Congenital disorders: NTD , CP .
3. Method of urinary management:
Volitional or reflex voiding
Condom catheter urinary collection
CISC
Indwelling urethral or suprapubic catheter
Crede, Valsalva voiding
4. UTI:
Severity of infection: febrile, hospitalization, IV antibiotics required
Frequency of recurrence
5. Urolithiasis :
episodes
surgical intervention
calculus composition
6. AD: SCD above T6
Physical Examination
1. HTN: renal dysfunction, AD
2. Generalized edema: severe renal insufficiency
3. Palpable flank mass: HN
4. Flank tenderness: ureteral obstruction, pyelonephritis
5. Abdominal mass: distended bladder, urinary retention
6. UI: stress maneuvers, Marshall test
7. Testicular mass: epididymitis/epididymo-orchitis, secondary abscess
8. prostate: size: BPH may coexist with NB dysfunction
9. Sacral abnormalities: sacral dimple or tuft of hair, sacral agenesis

17
10. Neurologic: sacral root, perianal sensation, sensory level, anal tone, sphincter
control, bulbocavernosal, knee, ankle, and toe reflexes.
Diagnostic tests
A. Blood studies:
1. Serum chemistry: RFT
2. CBC: elevated WBC, secondary anaemia due to ↓ renal function or chronic infection
B. Urinalysis:
1. Proteinuria: renal dysfunction
2. pyuria, nitrite, leukocyte esterase: acute or chronic infection
3. Hematuria: infection or lithiasis
Imaging
Imaging is most important in pts with risk factors for upper tract compromise:
A. DSD: particularly males who void reflexively
B. Impaired bladder compliance
1. Renal US: to screen for calculus, HN, or mass
2. KUB: radio-opaque calculi
3. Excretory urography:
Delayed excretion of contrast with high urinary-storage pressures
HUN: marked elevation of intravesical pressure (ie, NDO/DSD) or calculi
4. VCUG: for VUR, urethral abnormaity
5. Nuclear medicine renal scan: Sequential studies detect deterioration of renal function
6. MRI: bladder neck and posterior urethra
Diagnostic procedures
1) Cystourethroscopy: degree of trabeculation, diverticuli, bladder capacity, stone, ureteral
orifice competency, integrety of BN and external sphincter, Cx of chronic catheterization
and infection

18
2) Urodynamics: Technique used to obtain graphic recording of activity in UB, urethral
sphincters , & pelvic musculature .
Components include:
1. Uroflowmetry.
2. Cystometry.
3. Urethral pressure profile.
4. EMG.
Necessary to determine effective urologic management for all pts with neurogenic lower
urinary tract dysfunction
Differential Diagnosis
1. Cystitis.
2. Chronic urethritis.
3. Vesical irritation secondary to stone.
4. Interstitial cystitis.
5. Cystocele.
6. Infravesical obstruction (LUTS).
Treatment
1. UDS are essential to detrmine lower urinary tract function or dysfunction and to plan
urologic Mx
2. Control intravesical pressure and empty the bladder effectively: in order to protects
upper tracts, preserve renal function, continence, & control infection
Spontaneous voiding with continence is possible with NDO controlled medically
Voiding by trigger technique: tapping the abdomen suprapubically, tugging on the
pubic hair, squeezing the penis, or scratching the skin of the lower abdomen,
genitalia, or thighs.
Urinary darinage: SCIC or external collection appliance (condom)
SCIC: most effective Rx; requires low storage pressure
Indwelling cath: avoid due to Cx (UTI, erosion, calcui, etc)
Treatment of spinal shock
1. Bladder drainage: must be instituted immediately and maintained: by clean self
intermittent catheterisation(CSIC), indwelling catheter or suprapubic cystostomy
2. Increase fluid intake to 2 – 3 L/day
19
3. Prophylaxis for calculus formation by reducing calcium & oxalate intake & decrease vit
D from diet
Spastic neuropathic bladder
Medication:
First line:
1-- Anticholinergics: to improve urinary storage
pressure/↓ involuntary contraction:
a. Oxybutynin
b. Hypscyamine
c. Tolterodine
2-- 1-adrenergic blockers:↓internal sphincter
resistance, lower voiding pressure; ineffective for
DSD, may control symptoms of AD:
a. Doxazosin
b. Terazosin
c. tamsulosin
Second line:
1-- Botulinum toxin:
a. Injection into external sphincter
for DSD: short-lived , requires
repeated inj.
b. Inj. Into detrusor muscle for DO:
Duration of action is 3-9 mon
requires repeated inj.
2-- Vanilloid agents instillation:
capsaicin and resiniferatoxin:
Suppress uninhibited involuntary
detrusor contraction
Surgery
1. Endoscopic sphincter ablation or stenting
Only males with DSD
Requires condom catheter
2. Augmentation cystoplasty: using intestinal segment to enlarge the badder: Intermittent
cath for urine drainage
3. Cystectomy with continent urinary reservoir and catheterizable stoma:
For pts with limited dexterity specially in females
Ileal or colon pouch
Continent cathetrizable stoma (appendix or terminal ileum)
4. Ileovesicostomy (bladder chimney): for those unable to perform CSIC (quadriplegia)
5. Cystectomy with ileal conduit
6. Sacral rhizotomy at S3-4: Conversion of the spastic bladder to a flaccid bladder
7. Sacral neuromodulation (bladder pacemaker): of the sacral nerve roots to accomplish
bladder evacuation in selected cases

21
Flaccid neuropathic bladder
1. Crede maneuver (manual suprapubic pressure) accompanied by straining
2. Bladder training & care , voiding every 2hr
3. CSIC every 3-6 hr
4. Parasympathomimetic drugs like bethanecol chloride ( Urecholine), 5 – 50 mg every 6-
8hr
5. Surgery:
o TURP in hypertrophied bladder neck or BPH
o Implanting an artificial sphincter.
Complications
1. Recurrent UTI: cystitis, periurethritis, prostatitis, epididymoorchitis, pyelonephritis
2. Calculus formation
3. Urinary retention
4. HUN
5. Renal impairment and amyloidosis
6. Neoplastic transformation: associated with chronic catheter
7. Urethral erosion
8. Sexual dysfunction
9. AD
Mx of AD
1. Acute management: removal of triggering stimulus by bladder drainage or rectal
decompression
2. Chronic treatment:
blockers
calcium channel blocker
Botulinum toxin injection
3. Prophylaxis before cystoscopy: Oral nifedipine (20mg), 30 min before cystoscopy as
prophylaxis
Prognosis:
Proper urologic Mx greatly improves QoL in pts with NB dysfunction
Follow up
Annual evaluation in high risk pts may include:
1. UDS
2. imaging: typically renal US
3.
Serum creatinine

21
Lec:9
Surgery
Renal Parenchyma Neoplasm
Adenocarcinoma
(Renal cell carcinoma) :
Adenocarcinoma of kidney represent about 3% of adult cancer
Male-female ratio 2-1
equal in whites and blacks
Etiology
The cause is unknown.
There are various theories:
o Environmental and occupational factors
o Cigarette smoking
o Chromosomal aberration and tumor suppressor genes(chromosome 3 and 8)
o
Aquired cystic disease
Pathology
The tumor occur in equal frequency in either kidney , originates in the cortex , grow
out in the perinephric tissue
it is characteristically yellow to orange because of high lipid content
Pathogenesis
RCC is a vascular tumor , tend to spread by Direct invasion , Vascular invasion is
through renal vein
About 1\3 of patients have metastasis at presentation
The most common site of distant metastasis is lung oppposite kidney Followed by
liver, bone
.
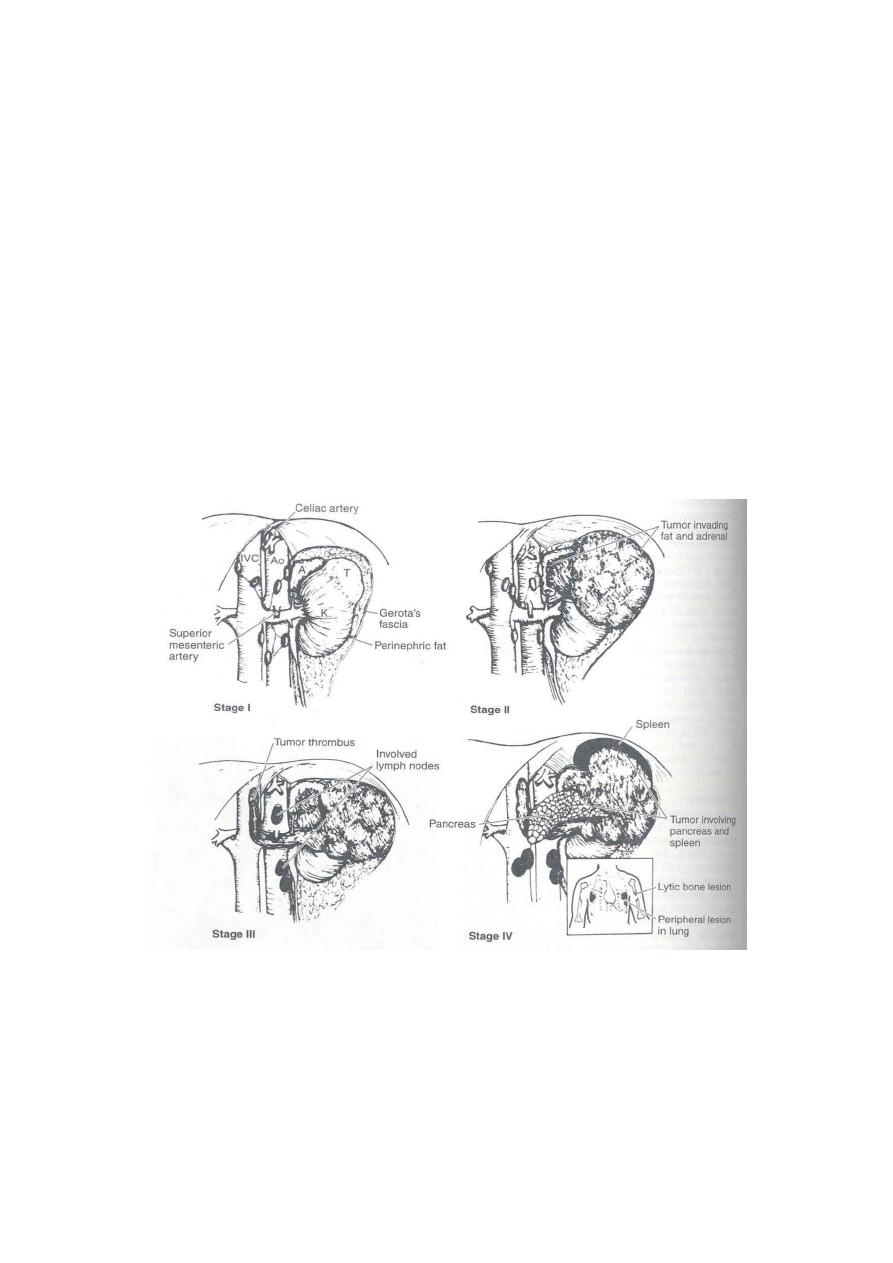
Tumer staging
Stage 1: tumor is confined within kidney parenchyma
Stage II : tumor involve perinephric fat but is confined within Gerota,s fascia
Stage IIIa : tumor involve the main renal vein or inferior vena Cava
Stage IIIb :tumor involve regional lymph node
Stage IIIc : tumor involve both local vessels and regional lymph node
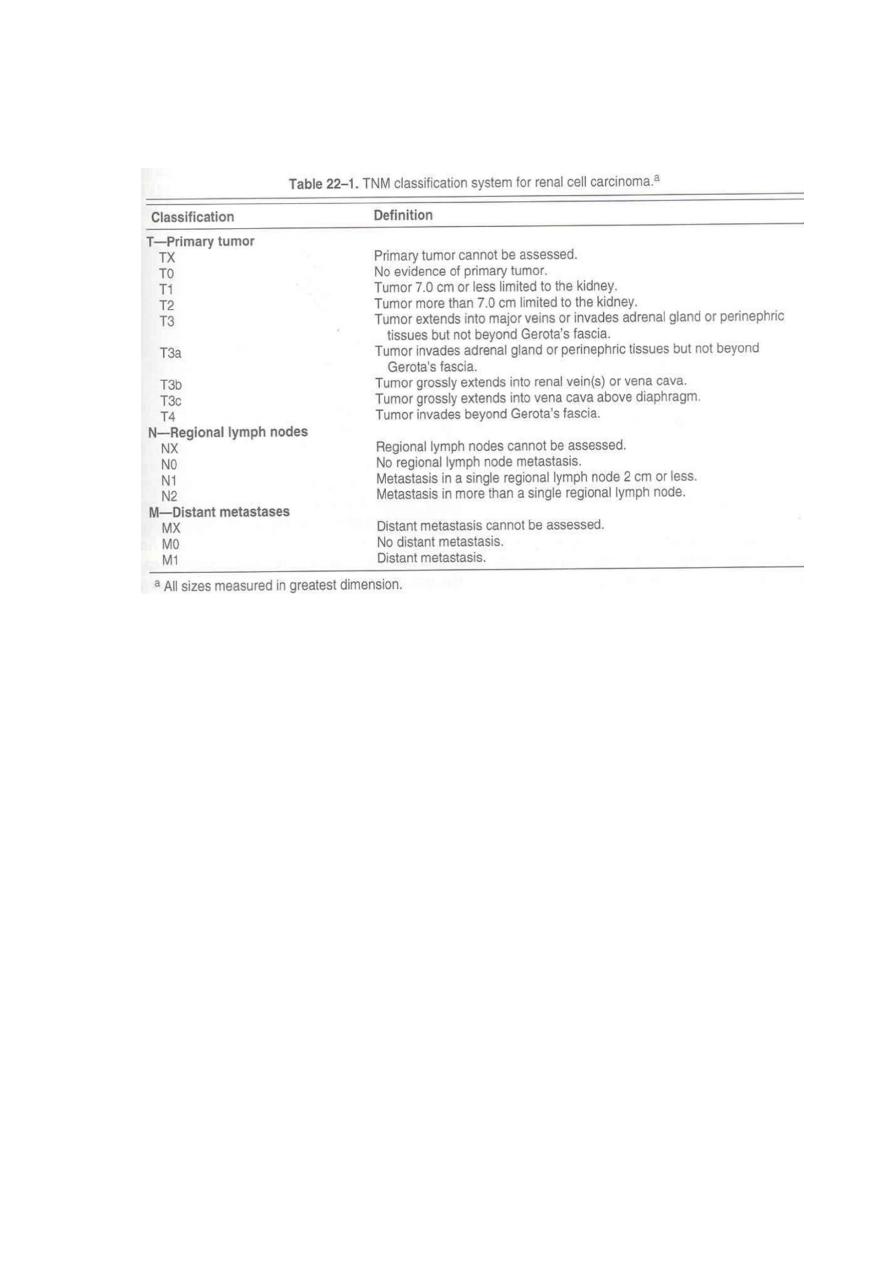
22
Stage IVa : tumor involves adjacent organs (colon,pancreas,….)
Stage IVb :distant metastasis
TNM Classification
Clinical picture
It has a wide variety of presentation
Classic triade :
1. gross haematuria
2. Flank pain
3. Palpable mass
Occur in about 10-15% of patients, frequently in advanced disease.
Abd pain , abd mass,
(30%) Symptoms of metastasis disease: Dyspnea ,cough ,headache ,bone pain
Paraneoplastic syndrome
Erythrocytosis
Hypercalcemia
Hypertention
Nonmetastatic hepatic dysfunction
3-10% of RCC present by paraneoplastic syndrome
RCC is the most common cause of paraneoplastic erythrocytosis
Hypercalcemia occur in about 20% of patients with RCC
Hypertention in 40%
23
Laboratory findings:
CBC anemia (30%)
High ESR
Haematuria (60%)
Imaging:
IVP 75% accurate
U\S
CT scan it is the leader for diagnosis and staging And detect distant metastasis
Renal angiography
MRI
Fine needle aspiration idicated in :
1. metastatic disease , planned for nonsurgical management
2.
establishing diagnosis in patients who are not surgical Candidate
Differential diagnosis:
1. Carcinoma of renal pelvis
2. Renal lymphoma
3. Adrenal cancer
4. Benign renal tumor
5. Renal cysts
6. Renal abscess

24
Treatment:
Localised disease : Stage (I, II , IIIa ) –
< Radical nephrectomy
Disseminated disease:
o 30% of RCC are metastatic
o The role of radical nephrectomy is limited
o It is a palliative therapy
o Radiotherapy (RCC is a radioresistant)
o Chemotherapy (is also chemotherapy resistant )
Prognosis is according to stage:
T1 disease 5 years survival 88-100%
T2 T3a 5 years survival 60 %
T3a 5 years survival rate 15-20 %
Benign tumer
Renal adenoma is the most common benign tumor
Renal oncocytoma occur in variant organ ( adrenal, salivary gland, thyroid,…)
represent about 3% of kidney tumor
Angiomyolipoma: is very rare
Bladder carcinoma
Male- female ratio 3-1
Common in wights than in blacks
Is the second most common cancer of genitourinary tract
Average age is 65 years
85% are Localised , 15 % have distant sites
Pathogenesis and Etiology
o Cigarette smoking account for 50 % of men and 30% of women the causative agent
are to be alpha and beta naphthylamine wich are secreates in urine of smokers
o Occupational exposure to certain chemicals(rubber ,petroleum, printing industries)
o Cyclophosphamide
o Artificial sweeeners
o Calculi and infection
o Genetic predisposition
25
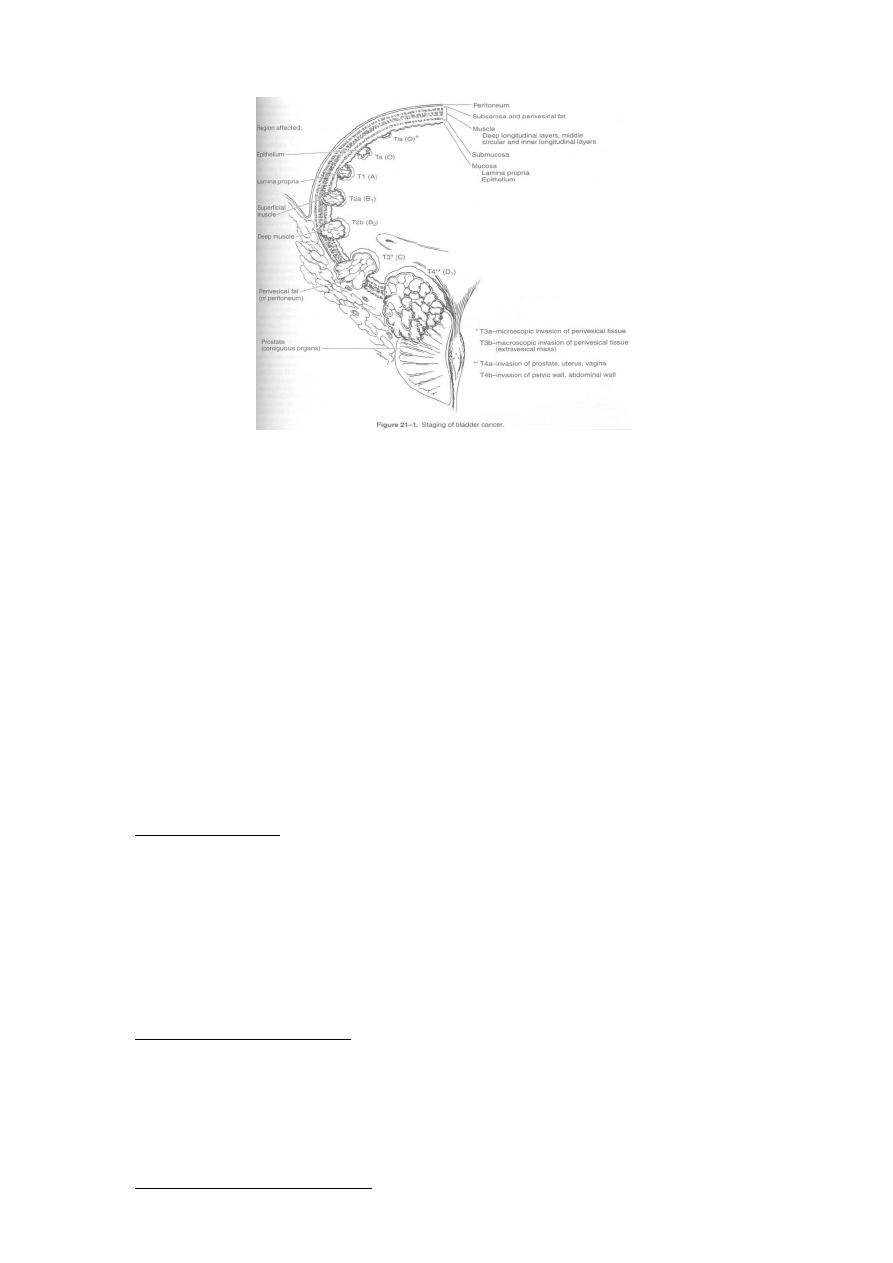
Staging
Hystopathology
Papiloma
: is uncommon
o Represent about <2 % of all transiotional cell
o Tumor , has a very good prognosis
Transitional cell carcinoma:
o Accounts for 90% of all bladder cancer
o Appears as papillary exophytic lesion
o May be sessile or ulcerated
Non Transitonal cell carcinoma
1- Adenocarcinoma :
Accounts for <2% of bladder cancer
Mucous secreting tumor
Arise along the floor of bladder
Muscle invasion is usually present
5 years survival <40%
2- Squamous cell carcinoma :
Accounts for 5-10% of bladder tumor
Often associated with H\O bilharsial infectionVesical caculi , chr ctheterisation
In Egypt represent about 60% of bladder cancer
3- Undifferentiated carcinoma :

26
Is rare , represent < 2% of bladder carcinoma
4 mixed carcinoma
Constitute 4-6% of all bladder carcinoma
Composed of transitional , squamous, or Undifferentiated carcinoma
Clinical picture
A – Symptoms :
Haematuria is the presenting symptom in 85-90%
o May be gross or micriscopic
o Intermittent rather than constant
Symptoms of vesical irritability
Symptoms of advanced disease
B - Signs :
The majority of patients have no pertinent physical signs.
patients with advanced disease may have a Palpable mass, Hepatomegaly and
supraclavicular lymph node Indicates advanced disease.
Laboratory findings:
The most common is hematuria
Azootemia in case of ureteral occlusion
Anemia may be a presenting symptom due to chr blood loss and replacement of
bone marrow by metastatic cells.
Urine cytology .
Imaging
:
Used To:
1- Evaluate the upper urinary tract
2- Assess the depth of muscle infiltration
3- Presence of regional or distant metastasis
IVU: the most common imaging test for evaluation of hematuria
CTscan
Cystourthroscopy
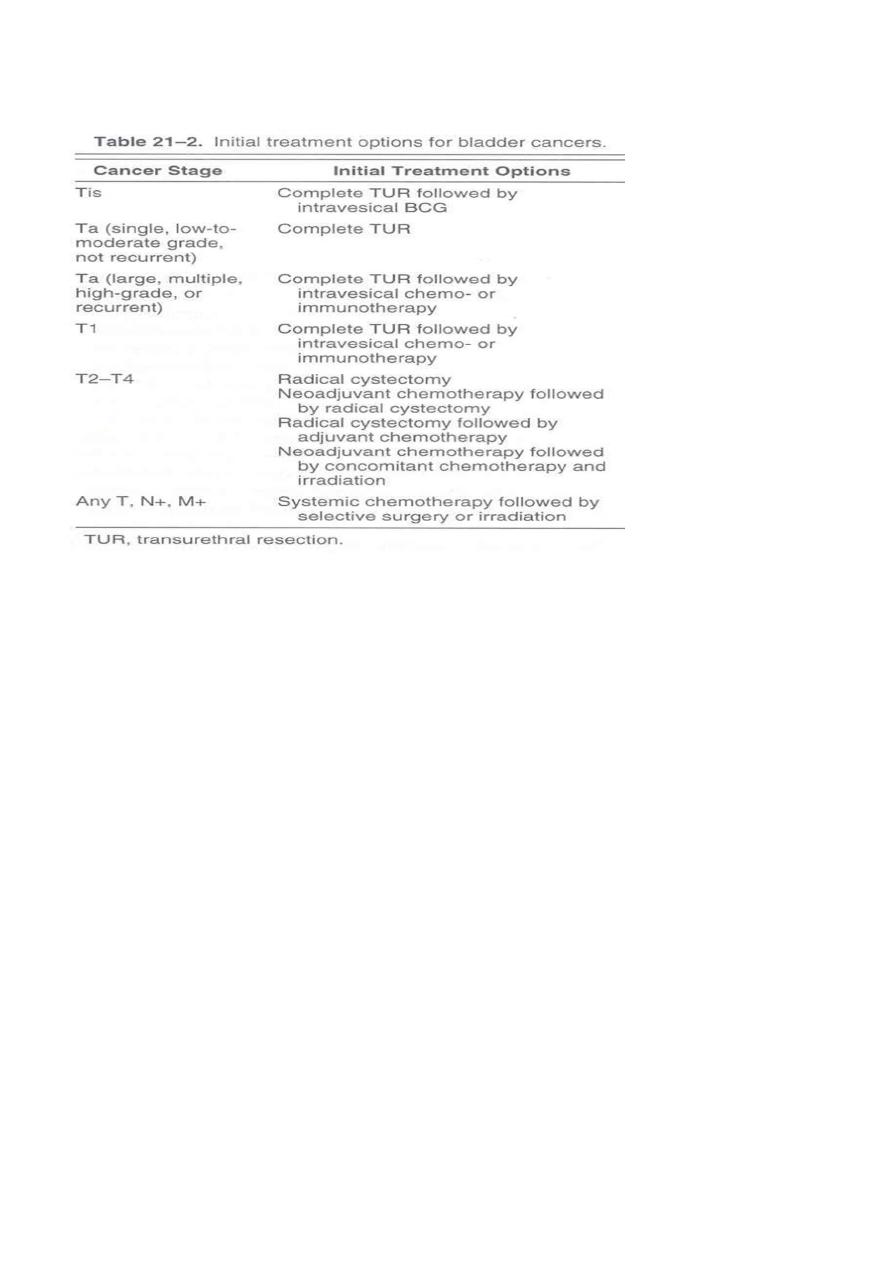
Treatment:
TUR or laser vaporization : For patients with single low grade, noninvasive tumor
27
Partial cystectomy : For solitary infiltrating tumor (t1-t3) cancer of bladder diverticula
Radical cystectomy : In locally advanced disease
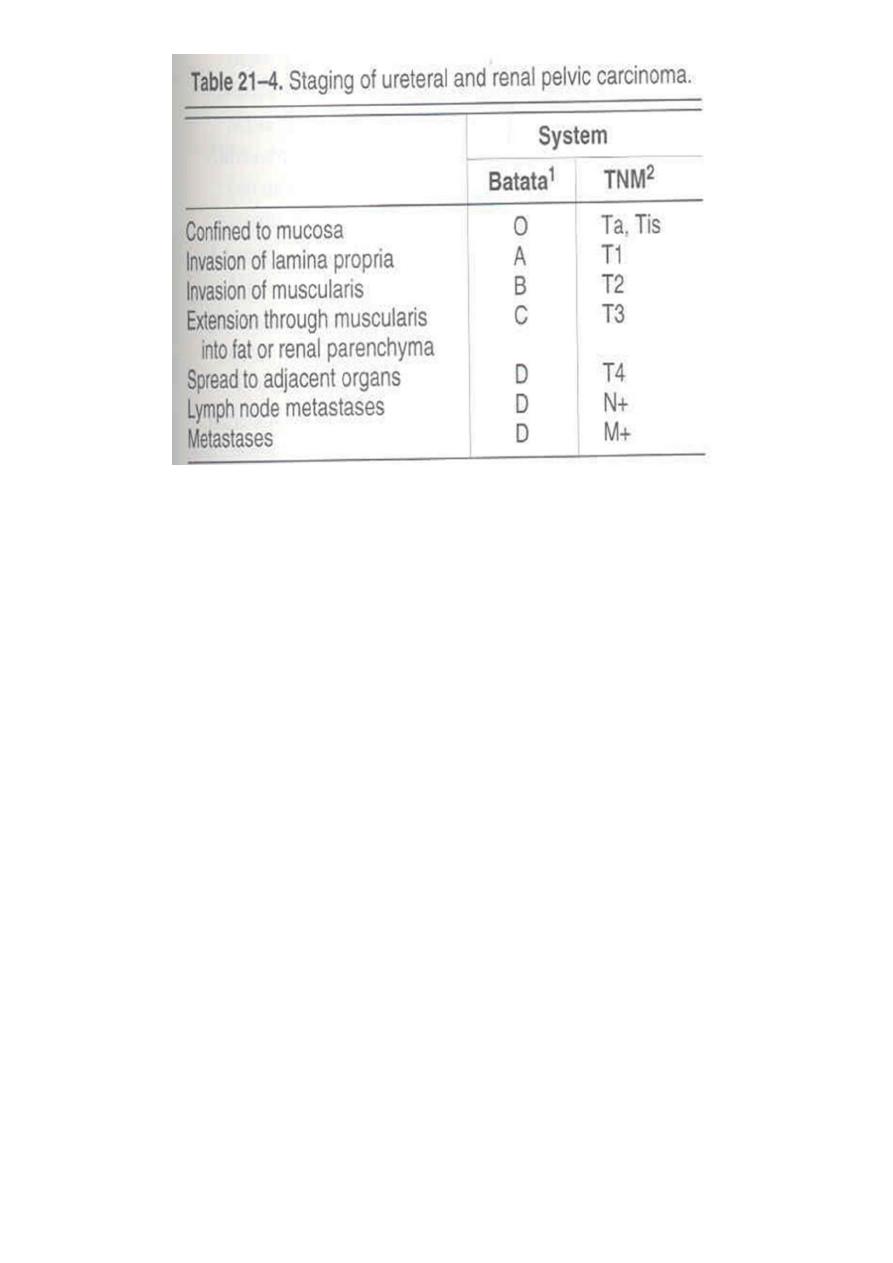
Ureteral and Renal pelvis
Carcinoma of renal pelvis and ureter are rare , Represent about 4% of all utothelial
cancer
Ratio: bladder renal pelvis ureter
51 3 1
Age group > 65 years
Patients with single upper tract carcinoma are at risk of Developing bladder
carcinoma (30-50%) and contralateral Upper tract (2-4%).
Etiology and pathology
As urinary bladder carcinoma
28
Clinical picture :
Haematuria 70-90%
Flank pain 50%
Irritative symptoms
Weight loss
Flank mass
Laboratory fingings :
Hematuria is identified in majority of cases
Anemia
Elevated liver function
Imaging :
IVU
Retrograde pyelography is more accurate
CTscan identify soft tissue abnormality of renal pelvis
Ureteropyeloscopy allow direct visualization of upper urinary tract
Treatment :
Based on: grade, stage, position and multiplicity
The standard therapy is nephroureterectomy .
Tumor of distal ureter
:
distal ureterectomy and ureter reimplantation
.

29
Lec:10
Surgery
Benign diseases of male genitalia
MALE GENITAL SYSTEM
PENIS
SCROTUM, TESTIS, & EPIDIDYMIS
PROSTATE
PENIS
MALFORMATIONS
INFLAMMATORY LESIONS
NEOPLASMS
MALFORMATIONS OF THE PENIS
ABNORMAL LOCATION OF URETHRAL ORIFICE ALONG PENILE SHAFT
1. HYPOSPADIAS (VENTRAL ASPECT) MOST COMMON (1/250 LIVE MALE BIRTHS)
2. EPISPADIAS (DORSAL ASPECT)
Both MAY BE ASSOCIATED WITH OTHER GENITAL ABNORMALITIES
INGUINAL HERNIAS
UNDESCENDED TESTES
CLINICAL CONSEQUENCES
1. CONSTRICTION OF ORIFICE
2. URINARY TRACT OBSTRUCTION
3. URINARY TRACT INFECTION
4. IMPAIRED REPRODUCTIVE FUNCTION
INFLAMMATORY LESIONS OF THE PENIS
1-) SEXUALLY TRANSMITTED DISEASES
2-) BALANITIS (BALANOPOSTHITIS)
INFLAMMATION OF THE GLANS (PLUS PREPUCE) ASSOCIATED WITH POOR LOCAL HYGIENE
IN UNCIRCUMCISED MEN

31
SMEGMA
DISTAL PENIS IS RED, SWOLLEN, TENDER
+/- PURULENT DISCHARGE
3-) PHIMOSIS
PREPUCE CANNOT BE EASILY RETRACTED OVER GLANS
MAY BE CONGENITAL
USUALLY ASSOCIATED WITH BALANOPOSTHITIS AND SCARRING
PARAPHIMOSIS (TRAPPED GLANS)
URETHRAL CONSTRICTION
4-) FUNGAL INFECTIONS : CANDIDIASIS
ESPECIALLY IN DIABETICS
EROSIVE, PAINFUL, PRURITIC
CAN INVOLVE ENTIRE MALE EXTERNAL GENITALIA
NEOPLASMS OF THE PENIS
SQUAMOUS CELL CARCINOMA (SCC)
EPIDEMIOLOGY
1. UNCOMMON – LESS THAN 1 % OF CA IN US MEN
2. UNCIRCUMCISED MEN BETWEEN 40 AND 70
PATHOGENESIS
1. POOR HYGIENE, SMEGMA, SMOKING
2. HUMAN PAPILLOMA VIRUS (16 AND 18)
3. CIS FIRST, THEN PROGRESSION TO INVASIVE SQUAMOUS CELL CARCINOMA
CLINICAL COURSE
USUALLY INDOLENT
LOCALLY INVASIVE
HAS SPREAD TO INGUINAL LYMPH NODES IN 25% OF CASES AT PRESENTATION
DISTANT METS RARE
5 YR SURVIVAL
70% WITHOUT LN METS
27% WITH LN METS

31
LESIONS INVOLVING THE SCROTUM
1- ) INFLAMMATION : TINEA CRURIS (JOCK ITCH)
SUPERFICIAL DERMATOPHYTE INFECTION
SCALY, RED, ANNULAR PLAQUES, PRURITIC
INGUINAL CREASE TO UPPER THIGH
2- ) SQUAMOUS CELL CARCINOMA
HISTORICAL SIGNIFICANCE
SIR PERCIVAL POTT, 18TH CENTURY ENGLISH PHYSICIAN
CHIMNEY SWEEPS
3- ) SCROTAL ENLARGEMENT
1. HYDROCELE - MOST COMMON CAUSE
ACCUMULATION OF SEROUS FLUID WITHIN TUNICA VAGINALIS
INFECTIONS, TUMOR, IDIOPATHIC
2. HEMATOCELE
3. CHYLOCELE : FILIARIASIS - ELEPHANTIASIS
4. TESTICULAR DISEASE
LESIONS OF THE TESTES
CONGENITAL
INFLAMMATORY
NEOPLASTIC
CRYPTORCHIDISM AND TESTICULAR ATROPHY
FAILURE OF TESTICULAR DESCENT
EPIDEMIOLOGY :
ABOUT 1% OF MALES (AT 1 YR)
RIGHT < LEFT, 10% BILATERAL
PATHOGENESIS
1. HORMONAL ABNORMALITIES

32
2. TESTICULAR ABNORMALITIES
3. MECHANICAL PROBLEMS
CLINICAL COURSE
1. WHEN UNILATERAL, MAY SEE ATROPHY IN CONTRALATERAL TESTIS
2. STERILITY
3. INCREASED RISK OF MALIGNANCY (3-5X)
4. ORCHIOPEXY
MAY HELP PREVENT ATROPHY
MAY NOT ELIMINATE RISK OF MALIGNANCY
OTHER CAUSES OF TESTICULAR ATROPHY
1. CHRONIC ISCHEMIA
2. INFLAMMATION OR TRAUMA
3. HYPOPITUITARISM
4. EXCESS FEMALE SEX HORMONES
i.
THERAPEUTIC ADMINISTRATION
ii.
CIRRHOSIS
5. MALNUTRITION
6. IRRADIATION
7. CHEMOTHERAPY
INFLAMMATORY LESIONS OF THE TESTIS
1. USUALLY INVOLVE THE EPIDIDYMIS FIRST
2. SEXUALLY TRANSMITTED DISEASES
3. NONSPECIFIC EPIDIDYMITIS AND ORCHITIS
SECONDARY TO UTI BACTERIAL AND NON-BACTERIAL
SWELLING, TENDERNESS
ACUTE INFLAMMATORY INFILTRATE
4. MUMPS
20% OF ADULT MALES WITH MUMPS
EDEMA AND CONGESTION
CHRONIC INFLAMMATORY INFILTRATE
MAY CAUSE ATROPHY AND STERILITY

33
5. TUBERCULOSIS
GRANULOMATOUS INFLAMMATION
CASEOUS NECROSIS
6. AUTOIMMUNE GRANULOMATOUS ORCHITIS
RARE FINDING IN MIDDLE AGED MEN
TESTICULAR NEOPLASMS
EPIDEMIOLOGY
MOST IMPORTANT CAUSE OF PAINLESS ENLARGEMENT OF TESTIS
5/100,000 MALES, WHITES < BLACKS (US)
INCREASED FREQUENCY IN SIBLINGS
PEAK INCIDENCE 20-34 YRS
MOST ARE MALIGNANT
ASSOCIATED WITH GERM CELL MALDEVELOPMENT
CRYPTORCHIDISM (10%)
TESTICULAR DYSGENESIS(XXY)
PATHOGENESIS
1. 95% ARISE FROM GERM CELLS
ISOCHROMOSOME 12, i(12p), IS A COMMON FINDING
INTRATUBULAR GERM CELL NEOPLASMS
2. RARELY ARISE FROM SERTOLI CELLS OR LEYDIG CELLS ; THESE ARE OFTEN BENIGN
3. Lymphoma ; men < 60 yo
WHO CLASSIFICATION OF TESTICULAR TUMORS
ONE HISTOLOGIC PATTERN (60%)
1. SEMINOMAS (50%)
2. EMBRYONAL CARCINOMA
3. YOLK SAC TUMOR
4. CHORIOCARCINOMA
5. TERATOMA
MULTIPLE HISTOLOGIC PATTERNS (40%)
1. EMBRYONAL CA + TERATOMA
2. CHORIOCARCINOMA + OTHER
3. OTHER COMBINATIONS
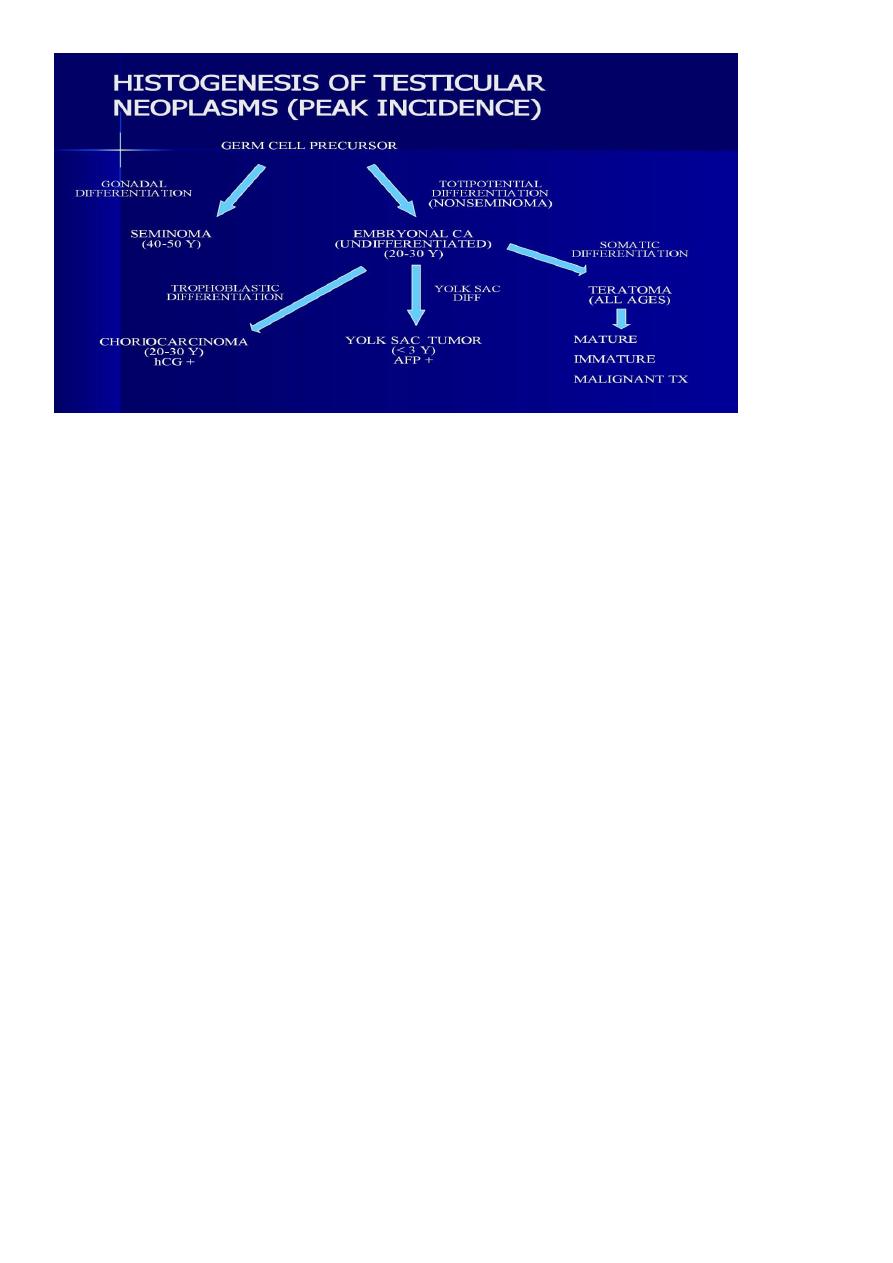
34
CLINICAL COURSE OF TESTICULAR TUMORS
USUALLY PRESENT WITH PAINLESS ENLARGEMENT OF TESTIS
MAY PRESENT WITH METASTASES
a. NONSEMINOMAS (MORE COMMON) : LYMPH NODES, LIVER AND LUNGS
b. SEMINOMAS : USUALLY JUST REGIONAL LYMPH NODES
TUMOR MARKERS (hCG AND AFP)
TREATMENT SUCCESS DEPENDS ON HISTOLOGY AND STAGE
SEMINOMAS VERY SENSITIVE TO BOTH RADIO- AND CHEMOTHERAPY
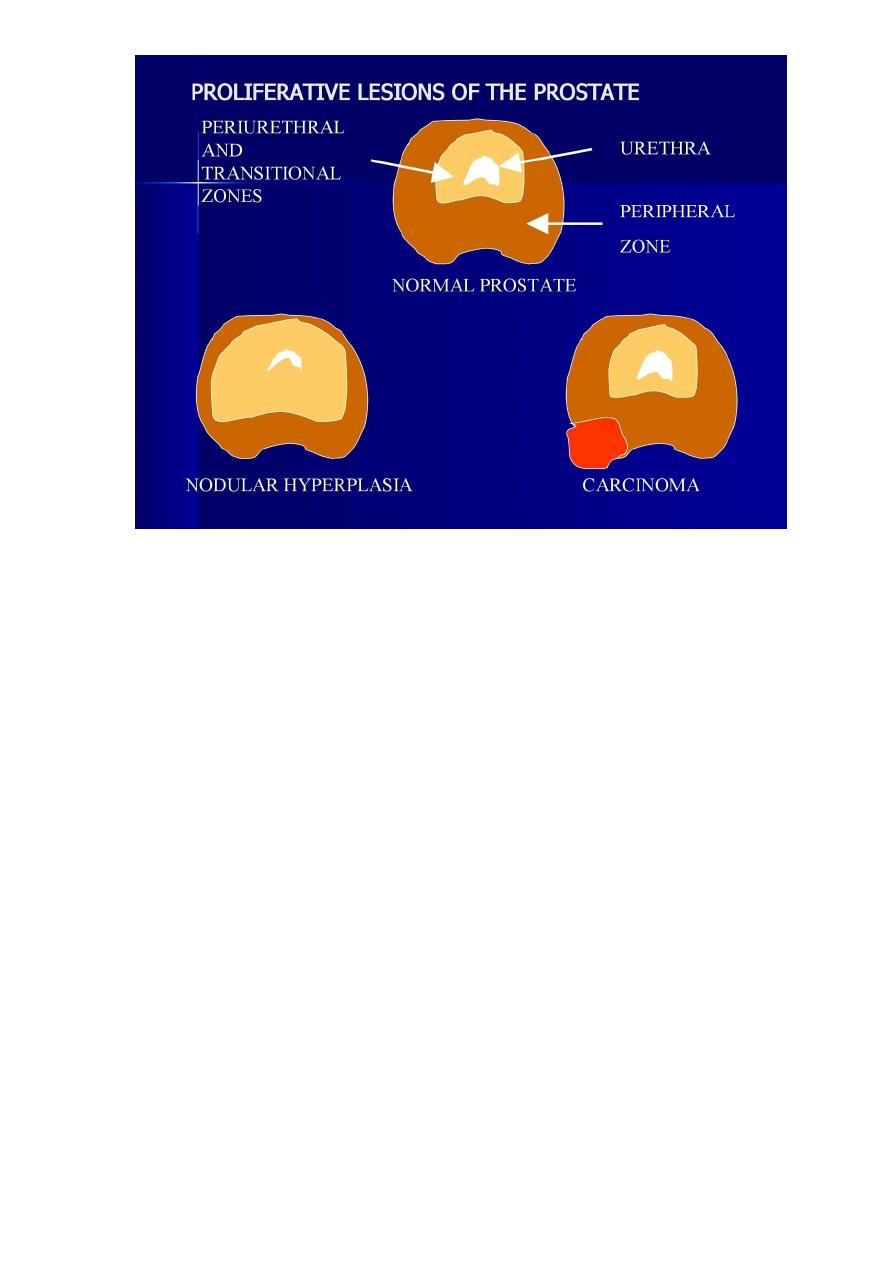
DISEASES OF THE PROSTATE
PROSTATITIS
NODULAR HYPERPLASIA
CANCER
PROSTATITIS
ACUTE BACTERIAL PROSTATITIS
CHRONIC BACTERIAL PROSTATITIS
CHRONIC ABACTERIAL PROSTATITIS

35
ACUTE BACTERIAL PROSTATITIS
ETIOLOGY
SAME ORGANISMS THAT CAUSE UTI as : E coli, OTHER GNR
PATHOGENESIS
ORGANISMS ASCEND FROM URETHRA AND URINARY BLADDER
RARELY, HEMATOGENOUS SPREAD
MORPHOLOGY
ACUTE INFLAMMATION, ESPECIALLY IN THE GLANDS, WITH MICROABSESSES
CONGESTION, EDEMA
CLINICAL COURSE
1. DYSURIA, FREQUENCY, LOW BACK PAIN, PELVIC PAIN
2. ENLARGED, EXQUISITELY TENDER
3. +/- FEVER OR LEUKOCYTOSIS
4. USUALLY RESOLVES WITH WITH AB RX
CHRONIC PROSTATITIS
ETIOLOGY
1. MAY FOLLOW ACUTE PROSTATITIS
2. MAY DEVELOP INSIDIOUSLY
3. CULTURE POSITIVE (BACTERIAL) : SAME ORGANISMS THAT CAUSE AP
4. CULTURE NEGATIVE (ABACTERIAL)
MAY BE RELATED TO : CHLAMYDIA TRACHOMATIS , UREAPLASMA UREALYTICUM
MOST COMMON FORM OF CP
MORPHOLOGY
LYMPHOCYTIC INFILTRATE
NEUTROPHILS AND MACROPHAGES
SOME EVIDENCE OF TISSUE DESTRUCTION
CLINICAL COURSE
SIMILAR TO AP ; LESS ACUTE SYMPTOMS , MORE RESISTANT TO AB RX
CBP OFTEN ASSOCIATED WITH RECURRENT UTI
36
NODULAR HYPERPLASIA
OTHER TERMS USED
GLANDULAR AND STROMAL HYPERPLASIA
BENIGN PROSTATIC HYPERTROPHY (HYPERPLASIA)
EPIDEMIOLOGY
OCCURS IN 20% OF MEN OVER 40
OCCURS IN 90% OF MEN OVER 70
PATHOGENESIS OF NODULAR HYPERPLASIA
PROLIFERATION OF BOTH EPITHELIAL AND STROMAL ELEMENTS
BOTH ANDROGENS AND ESTROGENS MAY PLAY A ROLE
NOT SEEN IN MALES CASTRATED BEFORE PUBERTY
INHIBITORS OF TESTOSTERONE METABOLISM USEFUL IN TREATMENT
RELATIVE INCREASE IN ESTROGENS IN OLDER MEN MAY INCREASE DHT RECEPTORS
IN PROSTATE
CLINICAL COURSE OF NODULAR HYPERPLASIA
SYMPTOMS OCCUR IN ONLY 10% OF MEN WITH NODULAR HYPERPLASIA
HESITANCY
URINARY RETENTION

37
URGENCY, FREQUENCY, NOCTURIA, UTI
TREATMENT : MEDICAL or SURGICAL
COMMON CAUSE FOR ELEVATED PROSTATE SPECIFIC ANTIGEN (PSA)
CARCINOMA OF THE PROSTATE
EPIDEMIOLOGY
MOST COMMON VISCERAL CANCER
o ABOUT 70/100,000 MEN IN US
o 200,000 NEW CASES/YR IN US
o 20% ARE LETHAL
SECOND MOST COMMON CAUSE OF CANCER DEATH IN MEN
PEAK INCIDENCE OF CLINICAL CANCER IS 65-75 YO
LATENT CA IS EVEN MORE PREVALENT : >50% IN MEN > 80 YO
PATHOGENESIS
1. HORMONAL FACTORS
DOES NOT OCCUR IN EUNUCHS
ORCHIECTOMY AND/OR ESTROGEN TREATMENT INHIBITS GROWTH
2. GENETIC FACTORS
INCREASED RISK IN FIRST ORDER RELATIVES
BLACKS > WHITES (SYMPTOMATIC CA)
3. ENVIRONMENTAL FACTORS
GEOGRAPHIC DIFFERENCES IN INCIDENCE OF CLINICAL CANCER (NOT OF LATENT CA)
CHANGE IN INCIDENCE WITH MIGRATION
CLINICAL COURSE
OFTEN CLINICALLY SILENT
DIGITAL RECTAL EXAM (DRE)
PROSTATE SPECIFIC ANTIGEN (PSA)
4 ng/ml IN PERIPHERAL BLOOD
o FREE PSA < 25%
TRANSRECTAL ULTRASOUND
NEEDLE BIOPSY
PROSTATISM (LIKE BPH)

38
METASTASES ; OSTEOBLASTIC
TREATMENT- SURGERY, RADIATION, HORMONES, CHEMO
STAGING
A (T1) MICROSCOPIC ONLY
B(T2) MACROSCOPIC (PALPABLE)
C(T3 &T4) EXTRACAPSULAR
D(N1-3,M1) METASTATIC
PROGNOSIS DEPENDENT ON STAGE AND HISTOLOGIC GRADE
1. 90% 10 YR SURVIVAL FOR A AND B
2. 10-40% 10 YR SURVIVAL FOR C AND D
