1
2
3
Lec:11
Surgery
Advances in the Management of BPH
The Scale of the Problem
Moderate to severe Lower Urinary Tract Symptoms (LUTS) occur in 25% of men over 50
years, and the incidence rises with age
Approximately 90% of men will develop histological evidence of BPH by 80 years of age
Increasing because:-
1. Men are living longer
2. Proportion of Men over 50 years will increase
3. Men are better informed about health matters
Difficulties in Diagnosis and Management
The symptoms of BPH are the same as those of early Prostate Cancer
Confirmation of the presence of prostate cancer may be difficult
The need to treat (proven) cancer may not always be clear cut
Understanding Lower Urinary Tract Symptoms (after Abrams, Bristol, UK)
Storage Symptoms
Frequency
Nocturia
Urgency
Urge incontinence
Bladder Pain
Voiding Symptoms
Slow stream
Intermittent flow
Detrusor Instability
Bladder Hypersensitivity
Bladder Outlet Obstruction
Detrusor Failure
4
Hesitancy
Straining
Terminal dribble
Physical Signs
May be few
Look for obvious uraemia
Palpate for full bladder
Examine urethral meatus and palpate urethra for stricture
DIGITAL RECTAL EXAMINATION (DRE) !!
Investigations for BPH
Urea and electrolytes if clinically indicated
PSA (should we counsel patients?)
Ultrasound urogram
Flow rate (if you have access)
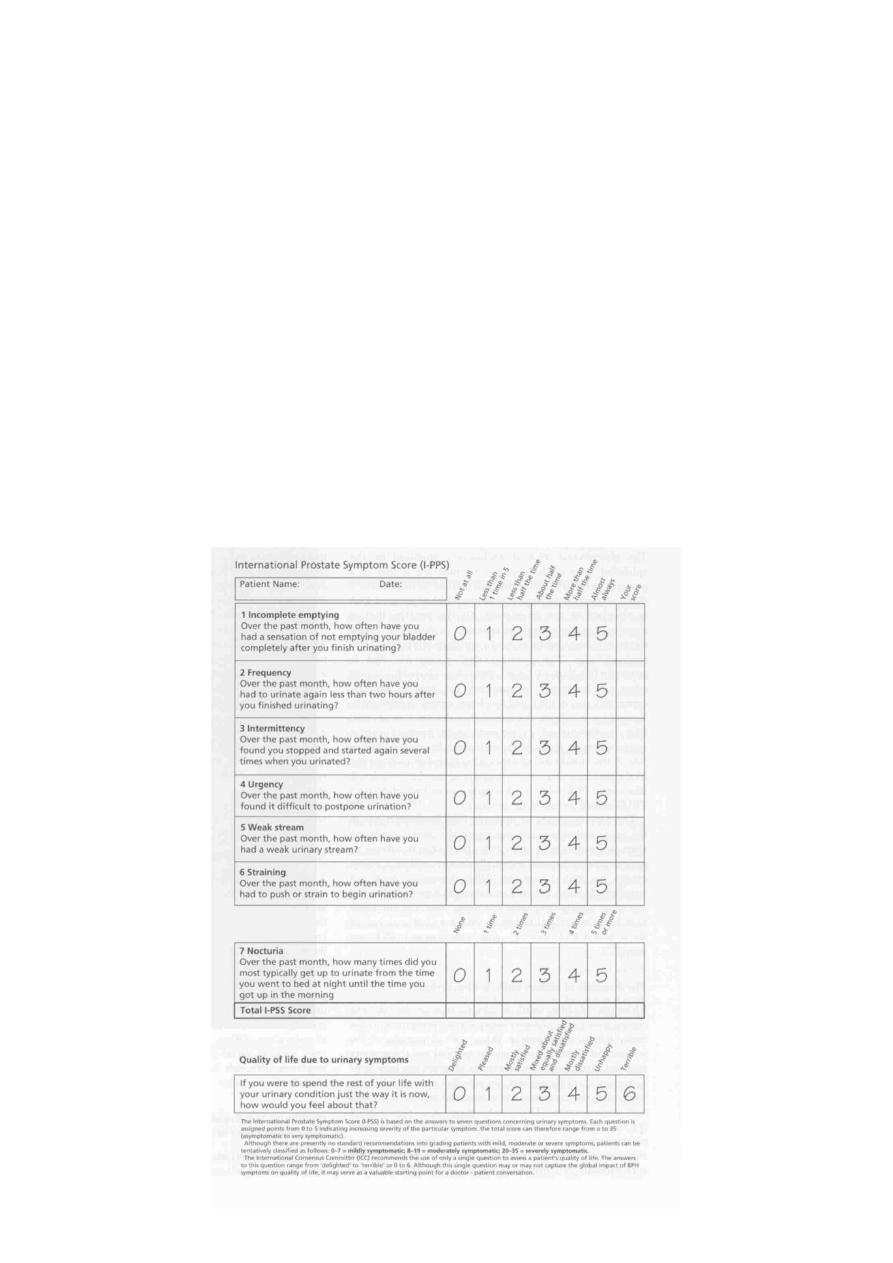
IPSS
IPSS

5
A word about Prostate Cancer
No symptoms specific for early prostate cancer
Presenting symptoms are therefore those of BPH
Biopsy of the prostate should be performed in those with abnormal DRE, or PSA
above age-specific reference range
Prostate Specific Antigen
Single-chain glycoprotein of 240 aa residues and 4 carbohydrate side chains
Physiological role in lysis of seminal coagulum
Prostate specific, but NOT cancer specific
In addition to prostate cancer, an elevated level may be found in
Increasing age
Acute urinary retention / Catheterisation
after TURP / Prostate Biopsy
Prostatitis
BPH
A reduced level may be found in patients treated with Finasteride
The Problem with PSA
Men with Prostate Cancer may have a normal PSA
Men with BPH or other benign conditions may have a raised PSA
May not even be prostate-specific!
What to do with men with a PSA of 4-10 ng/ml
PSA = Persistent Source of Anxiety
?
Refinements in the use of PSA
PSA density
PSA Velocity
Age-Specific PSA
40-49 Years old
<2.5ng/ml
50-59 Years old
<3.5ng/ml
60-69 Years old
<4.5ng/ml
70-79 Years old
<6.5ng/ml
Free:Total PSA ratio (<0.15 strongly suggests possibility of Ca
6
Prostate)
Prostate Specific Antigen
Possibly
Some
Attributes
The Management of BPH
Advances in the Management of BPH
New treatment modalities for BPH
1.
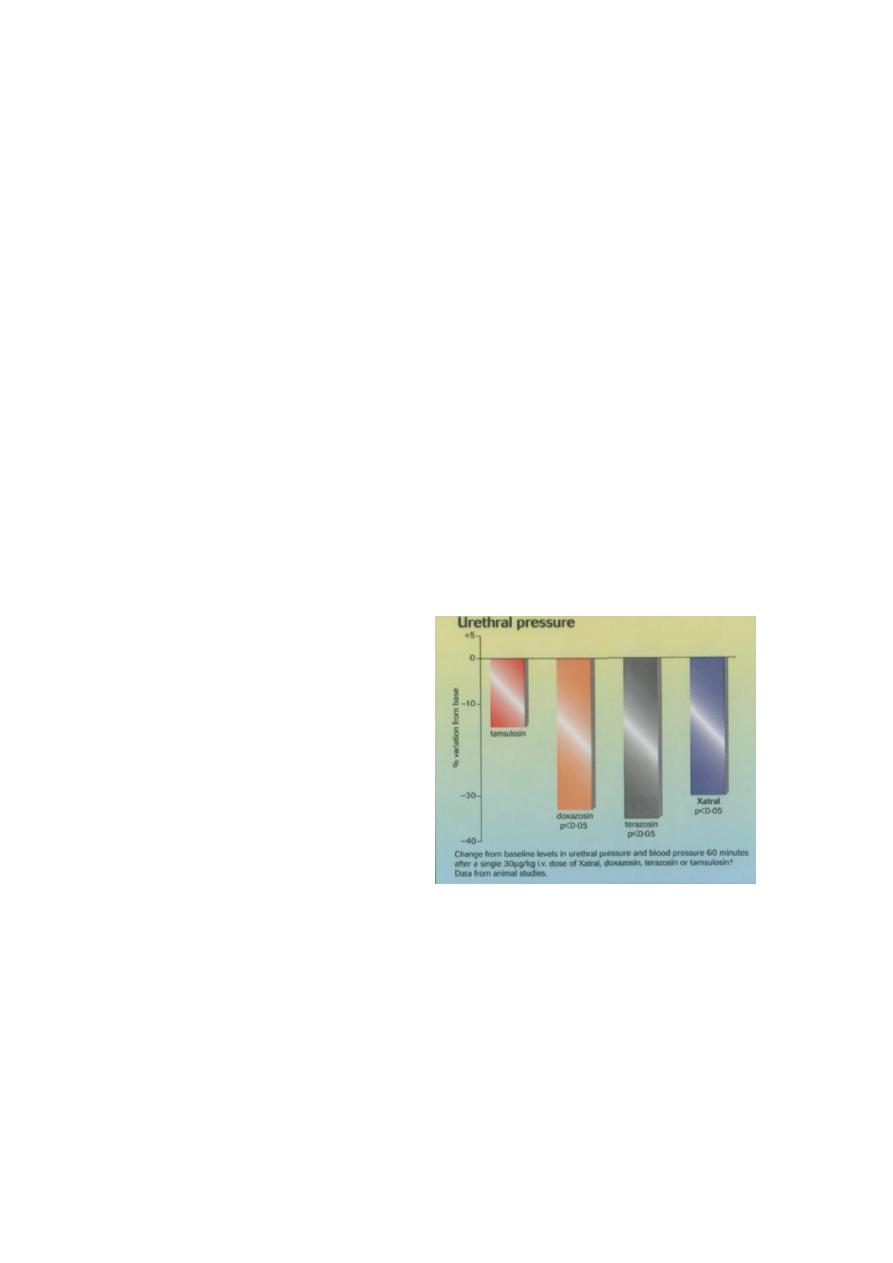
-blocker therapy (including selective blockers of
-1a receptors)
2. 5-
-reductase inhibitors - Finasteride (Proscar)
3. Minimally invasive Techniques
o Transurethral Microwave Thermotherapy (TUMT)
o Transurethral Needle ablation (TUNA)
o Transrectal high-intensity focused ultrasound (HiFU)
o Transurethral electrovaporisation (TUVP)
1. Alpha blocker therapy
2. Finasteride (Proscar) - PLESS study has confirmed that men with large prostates
(>40cc), taking long-term therapy, less likely to develop acute retention, or require
surgical intervention
3. Minimally invasive therapies
High energy TUMT, and TUNA, have proven clinical efficacy between that of drug
therapy and TUVP or laser therapy
HiFU currently requires GA, is costly and time consuming, and appears unlikely to
be popular at present
7
The subjective response after MITs and TURP appear similar, but objective results
superior for TURP
Surgical Therapies
TURP still the gold standard therapy, with which all other therapies must be
considered
Laser therapy
o expensive to set up
o Significantly reduced blood loss
o Catheter may be required post operatively
Open Prostatectomy rarely required
Guidelines for the Management of BPH
Produced after discussion between working party of General Practitioners and
Consultants
Agreed within the department of Urology
Protocol for the management of BPH
Eligible for Shared Care
Prostate Clinic
Normal
DRE and PSA
Outpatient appt with
Consultant
Abnormal
DRE and PSA
Referral to Urology Department
Management by GP
(See next slide)
Options
Flow rate and Residual volume if possible
History
IPSS Score
DRE
U+E and PSA
GP Assesses Patient
8
Future perspectives for the management of BPH
Much more emphasis on Quality of Life
Minimally invasive therapies are improving and may yet challenge the superiority of
TURP
Conclusions - BPH
Remains an important cause of patient morbidity
Correct approach to assessment is important
Many men may have their symptoms relieved by alpha blocker therapy or Finasteride,
which has also been shown to reduce the likelihood of surgery or acute urine
retention
A large variety of MITs exist for BPH who fail drug therapy, but for most patients the
gold standard surgical procedure remains TURP
The next few years will see many more techniques available to challenge the position
of TURP
Severe
IPSS > 20
Flow rate < 10 mls/s
Resid vol > 200 mls
Moderate
IPSS 7-20
Flow rate < 15mls/s
Resid vol <200 mls
Mild
IPSS<7
Flow Rate >15 mls/s
Resid vol < 100 mls
IPSS Score
Refer to the Urology
Department
alpha-blockers:
Refer if no improvement
Watchful Waiting
Management

9
Lec:12
Surgery
Prostate Carcinoma
Prostate cancer is the most common cancer diagnosed and is the second leading cause
of death
The prevalence of cancer increase with age, the probability of Ca P developing
in men under age of 40 is 1/10.000, for men 40-59 it is 1/103, 60-79 it is 1\8.
Blacks are at higher risk than whites.
Positive family history of CaP increase RISK of CaP.
High dietary fat intake increase the relative risk of CaP.
Etiology
The gene responsible for familial Ca P resides on chromosome 1
The region most commonly identified are chromosome 8p, 10Q, 13Q, 17P and 18Q.
Epithelial stromal interaction under the influence of growth factors Such as :
1. Transforming growth factors –B.
2. Platelets-derived growth factor.
3. Neuroendocrine peptide.
Pathology
Over 95% of CaP are adenocarcinoma
Of 5% : 90% Transitional cell carcinoma
Neuroendocrine carcinoma
Sarcoma
The cytological characters of CaP include:
Hyperchromatic, enlarged nuclei, with prominent nucleoli.
Cytoplasm is often abundant, blue-tinged or basophilic.
The basal cell layer is absent in CaP, it is present in normal gland.
Prostatic intraepithelial neoplasia (PIN) is the precursor to invasive CaP.
The distinguishing feature of invasive CaP is that the basal Cell layer is absent.
60 -70% of CaP originate in the peripheral zone.
10- 20% transition zone.
5-10% central zone.
11
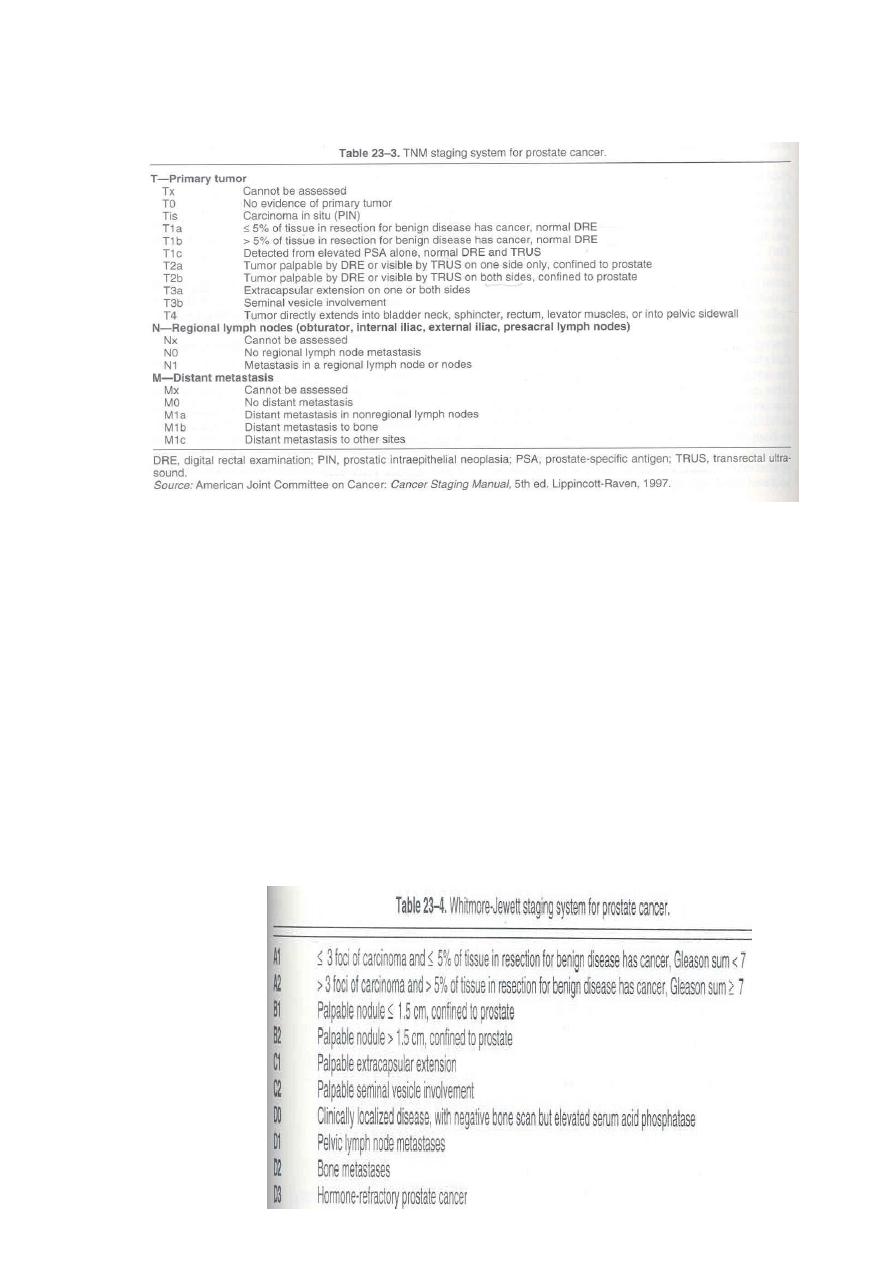
Grading and Staging
TNM Staging System
Gleason grade
Gleason grade range from 1 to 5, gleason score range from 2 to 10.
Well differentiated tumor have a gleason score of 2-4.
Mod differentiated tumor 5-6.
Poorly differentiated tumor 8-10.
Gleason score of 7 is grouped with mod differentiated tumor.
Gleason grade 1 and 2 characterized by small uniformly shaped gland, with little
intervening stroma.
Gleason grade 3 characterized by variable sized gland.
Gleason grade 4 has a several histologic appearance.
Gleason grade 5 has single infiltrating cell, no gland formation.
Comedocarcinoma is a variant of gleason grade 5.
Whitmore-Jewett

11
Clinical
Picture
Symptoms:
Most patient are asymptomatic in early stage.
Obstructive and irritative voiding symptoms can result from Local growth pf tumor
(urethra, bladder neck).
Bone pain in metastatic disease.
Symptoms of spinal cord compression (paresthesia, weakness, urinary and fecal
incontinence).
Signs:
DRE: induration.
Lympadenopathy.
Lymphedema.
Signs of metastases.
Lab Findings:
Azotemia.
Anemia.
Alkaline phosphatase elevated in bone metastasis.
Acid phosphatase.
Tumor Markers
PSA.
Prostate biopsy is the most commonly employed technique.
Increase the sensitivity of cancer detection.
Indicated in elevated PSA, abnormal DRE.
Imaging
TURS: useful in performing prostate biopsy.
Provide local staging.
Measure prostate volume.
CT scan confirm local or distant metastasis.
MRI.
Bone scan is the standard part of initial evaluation.
Molecular staging
Detection of circulating CaP cells in peripheral blood.
By using (RT-PCR) revers transcription-polymerase chain reaction).

12
Differential Diagnosis
Not all patients with elevated PSA have prostate cancer as it elevates in:
1. BPH.
2. Urethral instrumentation.
3. Infection.
4. Prostatic infarction.
5. Prostate calculi.
6. Alkaline phosphatase increase also in Paget disease.
Pattern of progression
Local extension outside the prostate (extra capsular extension) or seminal vesicle
invasion and distant metastasis increase with increase tumor volume.
Small and well differentiated cancer usually confined to prostate
Large volume and poorly differentiated (G 4-5)>4cm often locally extensive, metastatic
to lymph node or bone.
Locally advanced CaP invade bladder trigone, lead to ureteral obstruction.
Lymphatic metastases most identified to:
Obturator lymph node, common iliac, presacral and periaortic.
The axial skeleton is the most usual site of distant metastases (Lumbar spine, femur,
thoracic spine, Ribs, sternum, skull) can lead to pathologic fracture.
Visceral metastases (lung, liver, adrenal gland).
Diagnosis
DRE.
PSA.
TRUS.
Prostate biopsy.
Grading and staging.
Treatment
Localised Disease
Radical prostatatectomy: provide removal of prostate, seminal vesicle,block dissection
of obturator and ext iliac lymph node.
Radiation therapy.
Cryosurgery.
13
Locally advanced disease
Radiation therapy also indicated in unfit patient and symptomatic metastases (it leads to
relief of pain).
TUR: in patients with urinary outflow obstruction.
Bil Orchidectomy.
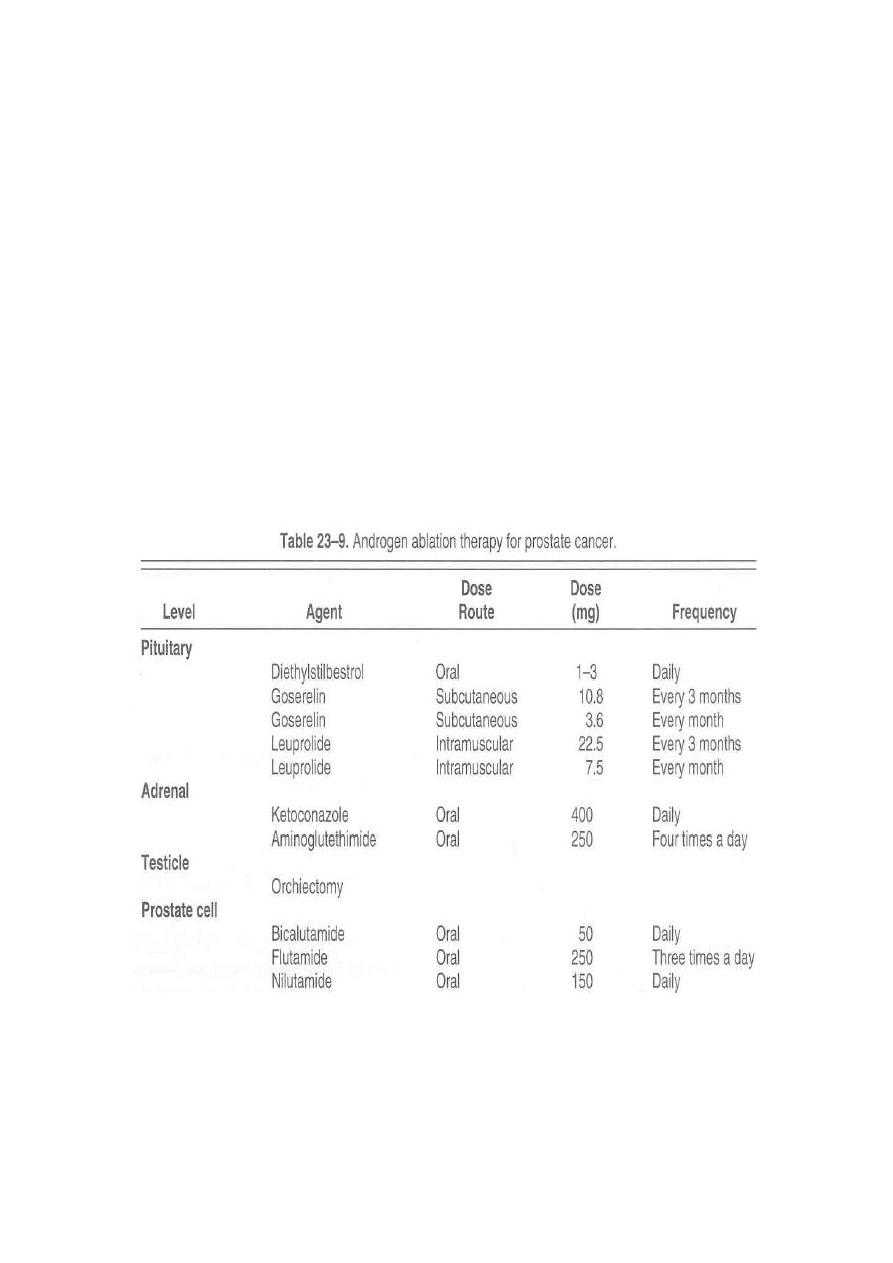
Hormonal Therapy:
Is the main line of treatment in metastases disease.
Is used in unfit patient for surgery or radiotherapy.
Bilateral orchidectomy (removal of testicular tissue).
LHRH agonist (zoladex)
It causes initial rise in testosterone level for (4-6) weeks then drop to castration level.
Antiandrogen (block testosterone receptors)
It is used as adjuvant therapy.
Prognosis
Organ confined cancer, 10 years free survival range 70-85%.
Focal extracapsular extension, free survival 70% at 5 years 40% at 10 years.
High grade, free survival 15%at 10 years.

14

15
Lec:13
Surgery
Scrotal Pathologies
Scrotal Pathologies
Anatomy
Incompletely descended testis (Undescended Testis):
The testis is arrested in some part of its path to the scrotum.
Incidence: 4% of boys are born with one or both testes incompletely descended.
Half of these reach the scrotum during the first month of life.
two thirds of these reach the scrotum during the first three months of life
incidence of testicular maldescent at the age of one year is around 1 per cent
In 10% of unilateral cases there is a family history.
Pathology
The epithelial elements are immature histologically and by late puberty irreversible
destructive changes halt spermatogenesis and limit the production of androgens.
Early repositioning of an incompletely descended testis can preserve function
Clinical features
The scrotum is empty & underdeveloped
More common on the right
Bilateral in 20% of cases.
Secondary sexual characteristics are typically normal.

16
The testis may be:
intra-abdominal, lying extraperitoneally above the internal inguinal ring.
inguinal, it may or may not be palpable
in the superficial inguinal pouch, in which case it must be distinguished from retractile
testis.
Hazards of incomplete descent
Sterility in bilateral cases (especially intra-abdominal testes)
Pain as a result of trauma
Indirect inguinal hernia often present
Torsion of the testis
Epididymo-orchitis
Atrophy of an inguinal testis before puberty may possibly be caused by recurrent
minor trauma
Testicular cancer is more common in an incompletely descended testes
N.B. orchidopexy may or may not diminish the risk of testicular cancer but it does improve
the prospect of early diagnosis .
Treatment
Orchidopexy is usually performed after the age of one year
The testes should be brought down into the scrotum before the boy starts school.
Orchidectomy should be considered if the incompletely descended testis is atrophic
Hormone treatment with human chorionic gonadotrophin is appropriate only when
there is established hypogonadism.
ECTOPIC TESTIS
The testis is abnormally placed outside this path
The sites of ectopic testis are:
• at the superficial inguinal ring: superfecial to the inguinal canal
• the perineum
• the root of the penis
• the femoral triangle.
An ectopic testis is usually fully developed. The main hazard is liability to injury.
Treatment: orchidopexy
N.B.: Retractile testis is normal testis with active cremasteric reflex
17
INJURIES TO THE TESTIS
Blunt or penetrating trauma
Contusion and rupture of the testis are associated with a collection of blood around
the testis and cannot usually be distinguished with certainty without exploration.
O/E: scrotal swelling, bruises, Loss of testicular contour
U/S is the investigation of choice
Haematocele ( collection of blood between two layers of tunica vaginalis) should be
drained and the tunica albuginea repaired after evacuation of haematoma.
A severely damaged testis may have to be removed.
ABSENT TESTIS
‘Vanishing’ testis: a condition in which a testis develops but disappears before birth.
Cause: prenatal torsion.
True agenesis of the testis is rarer.
Laparoscopy is useful in distinguishing these causes of clinically absent testis from
intra-abdominal maldescended testis.
Scrotal Swelling
Scrotal swelling with pain:
Epididymitis
Orchitis
Testicular trauma
Testicular torsion
Incarcerated scrotal hernia
Testicular tumor
Scrotal Swelling without pain:
Hydrocele
Spermatocele
Varicocele
Hematocele
Scrotal hernia
Testicular tumor
18
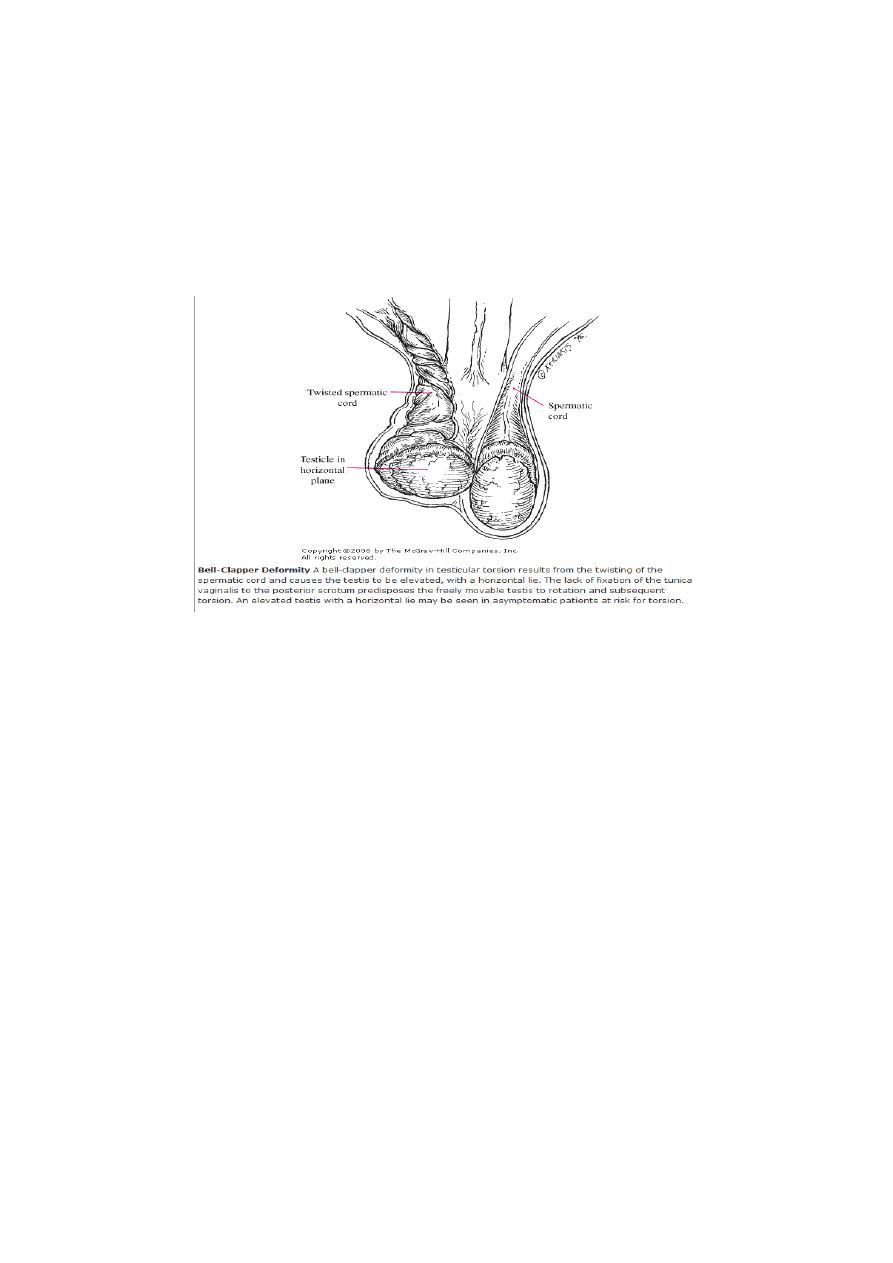
TORSION OF THE TESTIS ( Torsion of spermatic cord)
Rotation of the testis around the vertical axis of the cord
It is time limited due to arterial obstruction & the patient might lose his testis by
ischemia (gangrene) if the diagnosis is delayed (6 hours).
It may develop spontaneously during sleep.
Straining at stool, lifting a heavy weight, trauma, and coitus are all possible
precipitating factors.
Clinical features
Most common between 10 and 25 years of age
Sudden agonizing pain in the groin and the lower abdomen.
The patient feels nauseated and may vomit.
The testis lie transversely high and the tender twisted cord can be palpated above it.
Testicular elevation does not relief pain
Loss of cremasteric reflex
Diagnosis
Doppler ultrasound scan will confirm the absence of the blood supply to the affected testis
Treatment
Exploration for torsion
If the testis is viable when the cord is untwisted then it is fixed (orcheopexy).
An infarcted testis (gangrenous) should be removed (orchidectomy).
The other testis should also be fixed because the anatomical predisposition is likely to
be bilateral.
N.B: In the first hours it may be possible to untwist the testis manually, then early
orcheopexy to avoid recurrent torsion
19
VARICOCELE
It is a varicose dilatation of the veins draining the testis ( abnormal dilatation of the
pampiniform plexus)
Most varicoceles present in adolescence or early adulthood
Usually on the left.
Clinical Features
Usually symptomless
There may be dragging scrotal discomfort
The scrotum on the affected side hangs lower than normal
On palpation, with the patient standing, the varicose plexus feels like a bag of worms.
Infertility ?
Investigations:
Scrotal Doppler U/S
Treatment
Operation is not indicated for asymptomatic varicocele.
Indicatioins: pain, infertility, cosmetic
Types of operations:
• Varicocele ligation
• laparoscopic ligation
• Embolisation of the testicular vein under radiographic control
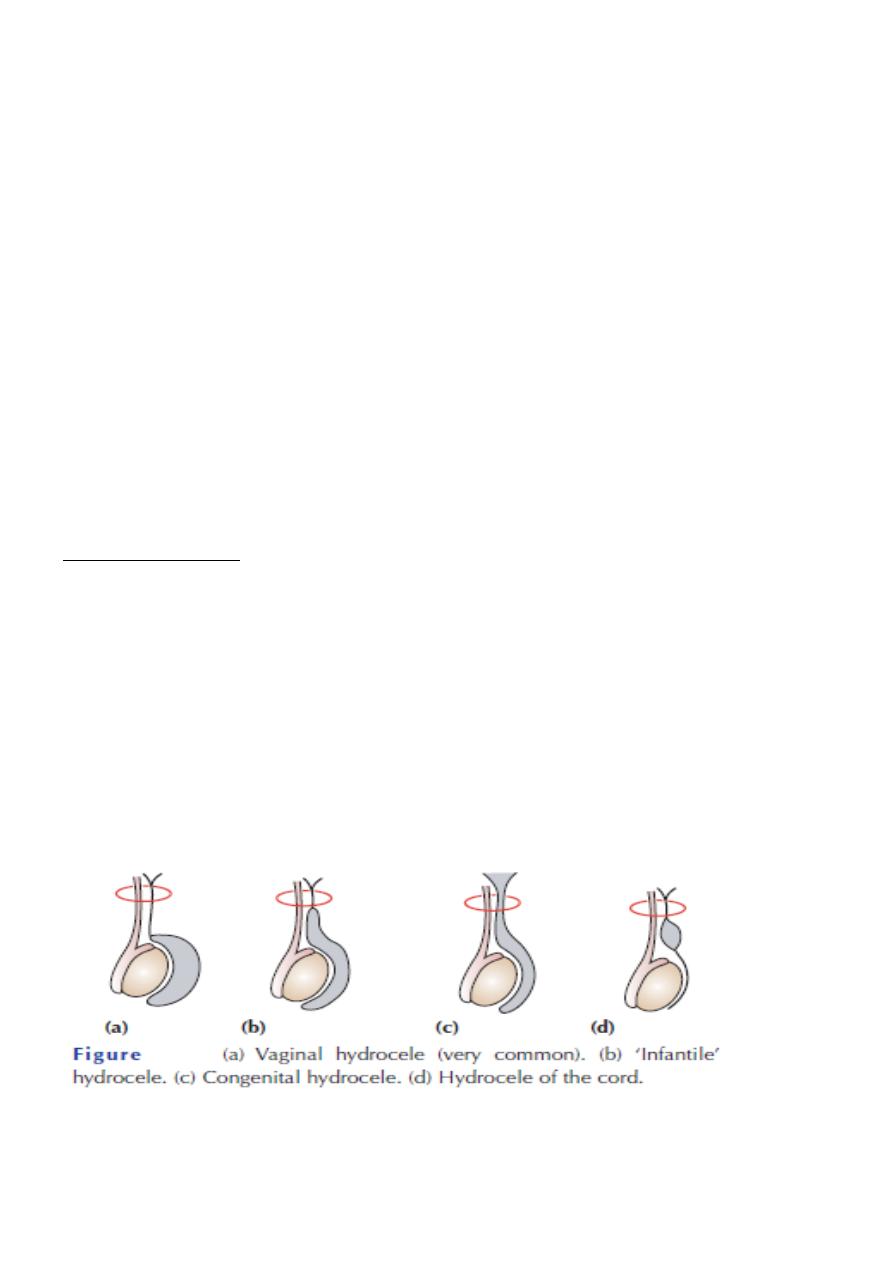
HYDROCELE
Hydrocele is an abnormal collection of serous fluid in a part of the processus vaginalis,
usually the tunica.
Vaginal hydrocele abnormal collection of serous fluid between the two layers of tunica
vaginalis.
In congenital hydrocele, the processus vaginalis is patent and connects with the peritoneal
cavity.
Etiology
Acquired hydroceles are primary (idiopathic), or secondary to testicular disease.
A hydrocele can be produced in four different ways
• by excessive production of fluid within the sac, e.g. secondary hydrocele

21
• by defective absorption of fluid; this appears to be the explanation for most primary
hydroceles although the reason why the fluid is not absorbed is obscure
• by interference with lymphatic drainage of scrotal structures
• by connection with the peritoneal cavity via a patent processus
vaginalis (congenital).
Clinical features
Primary vaginal hydrocele is most common in middle and later life but can also occur in
older children presents with scrotal swelling
Painless
Typically translucent (transillumination +ve)
It is possible to ‘get above the swelling’ on examination of the scrotum
N.B: in a young man; there may be a testicular tumour, so scrotal US should be done.
Treatment
Congenital hydroceles are treated by herniotomy if they do not resolve spontaneously
Acquired hydroceles: excision of the wall
N.B: A secondary hydrocele may subsides when the primary lesion resolves.
Epididymal cysts
They represent cystic degeneration of the epididymis.
Filled with a crystal-clear fluid.
Found in middle age
The cysts are multilocular
Excision may cause obstruction of the epididymis therefore it is better to leave it.
Spermatocele
A unilocular retention cyst derived from some portion of the sperm-conducting mechanism
of the epididymis.
Typically lies in the epididymal head above and behind the upper pole of the testis.
The fluid contains spermatozoa
Small spermatoceles can be ignored. Larger ones can be aspirated or excised through a
scrotal incision.
EPIDIDYMO-ORCHITIS
Inflammation confined to the epididymis is epididymitis
Infection spreading to the testis is epididymo-orchitis.
Acute epididymo-orchitis
Mode of infection
Infection reaches the epididymis via the vas from a primary infection of the urethra,
prostate or seminal vesicles

21
Blood-borne infections of the epididymis are less common
N.B: Acute epididymo-orchitis can follow any form of urethral instrumentation. It is
particularly common when an indwelling catheter is associated with infection of the
prostate.
Clinical features
The initial symptoms are those of urinary tract infection.
The epididymis and testis swell and become painful.
Fever
The scrotal wall, at first red, oedematous and shiny, may become adherent to the
epididymis.
Resolution may take 6–8 weeks to complete.
Occasionally, an abscess may form and discharge of pus through the scrotal skin.
N.B: Acute epididymo-orchitis develops in about 18% of males suffering from mumps.
The main complication is testicular atrophy, which may cause infertility if the condition is
bilateral.
Investigations
GUE
Urine C&S
WBC count
Scrotal U/S
Treatment
Broad spectrum antibiotics for 2 weeks (3
rd
generation cephalosporin or quinolones)
Scrotal support
Supportive therapy (analgesics, antipyretics, anti emetics, IVF)
If suppuration occurs(Abscess): drainage is necessary.
TUMOURS OF THE TESTES
• Most testicular neoplasms are malignant
• It is one of the most common forms of cancer in young men.
• Maldescent predisposes to malignancy
• The lymphatic drainage of the testes is to the para-aortic lymph nodes near the origin
of the gonadal vessel.
• The inguinal lymph nodes are affected only if the scrotal skin is involved.
Classification
They are classified according to their predominant cellular type:
1. GCTs:
o Seminoma (40%):
The enlarged testis is smooth and firm.
metastasize via the lymphatics.
Hematogenous spread is uncommon.
o Nonseminomatous GCT or Teratoma (32%):
22
Arises from totipotent cells in the rete testis and often contains a variety of cell
types, of which one or more predominate.
They may secrete human chorionic gonadotrophin (HCG) & alpha-fetoprotein.
o Combined seminoma and teratoma (14%)
2. Interstitial tumours (1.5%):
arise from Leydig or Sertoli cells
3. Lymphoma (7%)
4. Other tumours (5.5%)
Clinical features
• testicular lump which is usually painless
• sensation of heaviness occurs when the testis is two or three times its normal size
• The testis is enlarged, smooth, firm and heavy
• Secondary hydrocele
• Secondary retroperitoneal deposits may be palpable, just above the umbilicus,
hepatic enlargement, enlarged supraclavicular nodes
• Symptoms of metastatic disease: abdominal or lumbar pain, chest pain, dyspnoea
and haemoptysis
• Rarely, patients present with severe pain and acute enlargement of the testis because
of haemorrhage into a neoplasm
Between 1% and 5% of cases have gynaecomastia (mainly the teratomas).
Investigations
• Tumour markers (HCG, alpha-fetoprotein and lactate dehydrogenase)
• U/S scanning of the testis
• CXR: pulmonary metastases especially in teratoma
CT scan and MRI are the most useful means of detecting secondaries and of monitoring the
response to therapy.
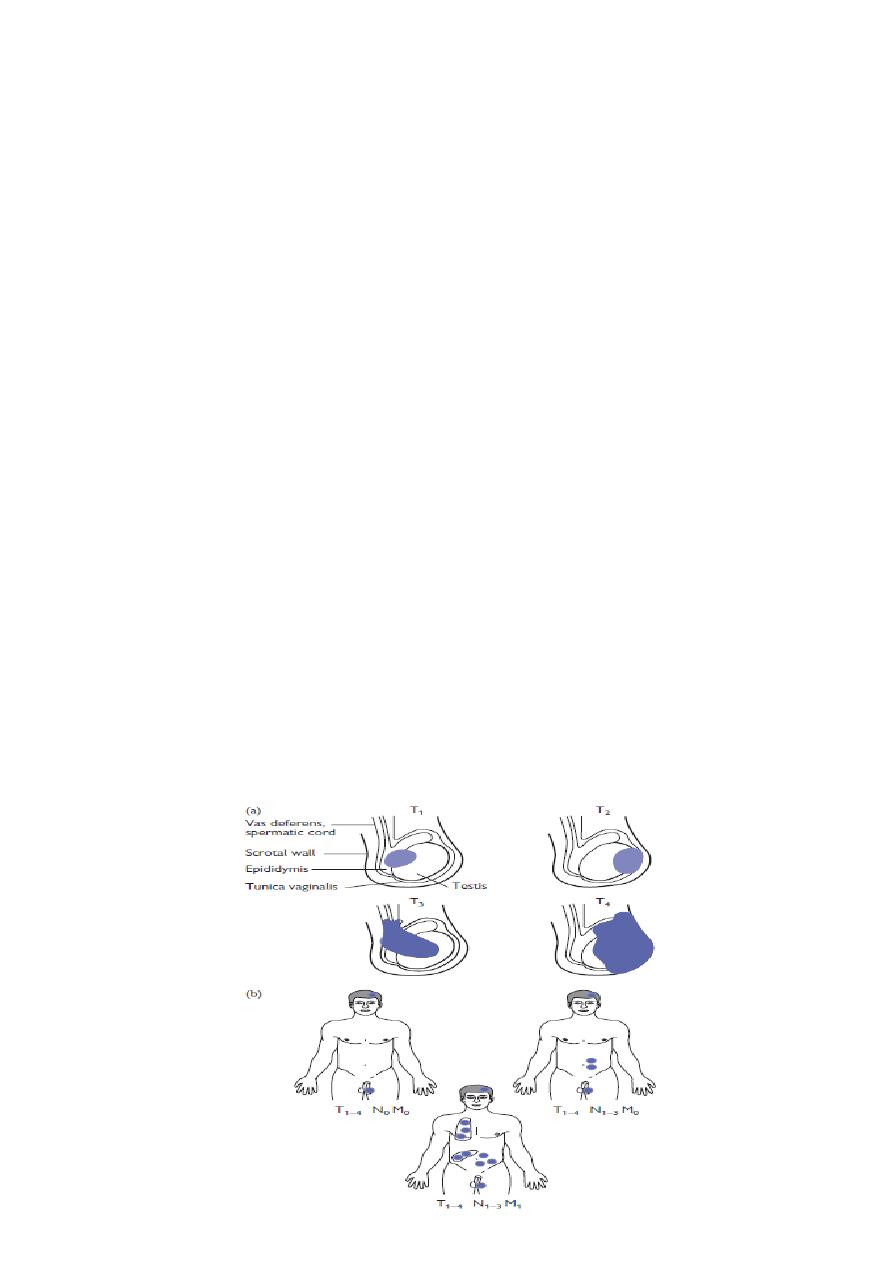
Staging

23
Treatment
Radical orchidectomy through inguinal approach.
Further Mx:
Further treatment depend on staging and histological diagnosis (after orchidectomy):
Seminomas
-
Radiosensitive
-
Highly sensitive to cisplatin, which is used for patients with metastatic disease.
Teratomas
-
less sensitive to radiation
-
Chemotherapy:
Cisplatin, methotrexate, bleomycin and vincristine : used in combination with great
success.
For both seminoma & teratomas: Retroperitoneal lymph node dissection is sometimes
needed when retroperitoneal masses remain after chemotherapy
Prognosis
Seminoma: the 5 years survival after orchidectomy and radiotherapy or chemotherapy:
If there are no metastases 95%.
If there are metastases 75%
Teratoma: 5-year survival rate:
stage 1 - 2: of more than 85%
stage 3 - 4 : about 60%
Idiopathic scrotal gangrene- Necrotizing fasciatis (Fournier’s
gangrene)
Fulminating inflammation of the subcutaneous tissues, which results in an obliterative
arteritis of the arterioles to the scrotal skin
Most commonly occurs in immunocompromised patients
Causative organisms:
mixed infection of Haemolytic streptococci (sometimes
microaerophilic), Staphylococcus, E. coli, Clostridium welchii.
Clinically:
Sudden scrotal inflammation
Rapid onset of gangrene and loss of scrotal skin leading to exposure of the scrotal contents
The absence of any obvious cause in over half the cases.
The condition can follow minor injuries or procedures in the perineal area, such as a bruise,
scratch, urethral dilatation, injection of haemorrhoids or opening of a periurethral abscess.

24
Clinical features
Sudden pain in the scrotum, prostration, pallor and pyrexia.
Cellulitis spreads until the entire scrotal coverings slough, leaving the testes exposed but
healthy
Treatment
The microorganisms are usually sensitive to gentamicin and a cephalosporin
Wide excision of the necrotic scrotal skin
Many patients die despite active treatment
Vesicoureteral reflux (VUR )
Definition:
VUR results from abnormal retrograde flow of urine from the bladder into the upper urinary
tract.
It is caused by primary or secondary incompetence of the ureterovesical valve mechanism.
Epidemiology
• Overall incidence in children is >10%
• Asymptomatic children have an incidence of 17%
• VUR is present in 70% of infants with urinary tract infection.
• More importantly, between 30% and 50% of children with reflux will have renal
scarring.
• Reflux is the second most common cause of prenatal hydronephrosis and accounts for
37% of cases.
• Adults with urinary tract infection (UTI) have a 5% incidence of reflux.
• Younger children affected more than older children
• Girls more than boys (female–male ratio 5:1)
• VUR occurs more often in Caucasian than in Afro-Caribbean children.
• Siblings of an affected child have a 40% risk of reflux, and routine screening of siblings is
recommended.
Pathogenesis
• The ureter passes obliquely through the bladder wall (1–2 cm), where it is supported by
muscular attachments that prevent urine reflux during bladder filling and voiding.
• The normal ratio of intramural ureteric length to ureteric diameter is 5:1.
• Reflux occurs when the intramural length of ureter is too short (ratio <5:1).
• The appearance of the ureteric orifice changes with increasing severity of reflux,
classically described as stadium, horseshoe, golf-hole, or patulous.
25
Classification
Primary reflux (1%) results from a congenital abnormality of the ureterovesical junction.
Secondary reflux results from urinary tract dysfunction associated with elevated intravesical
pressures.
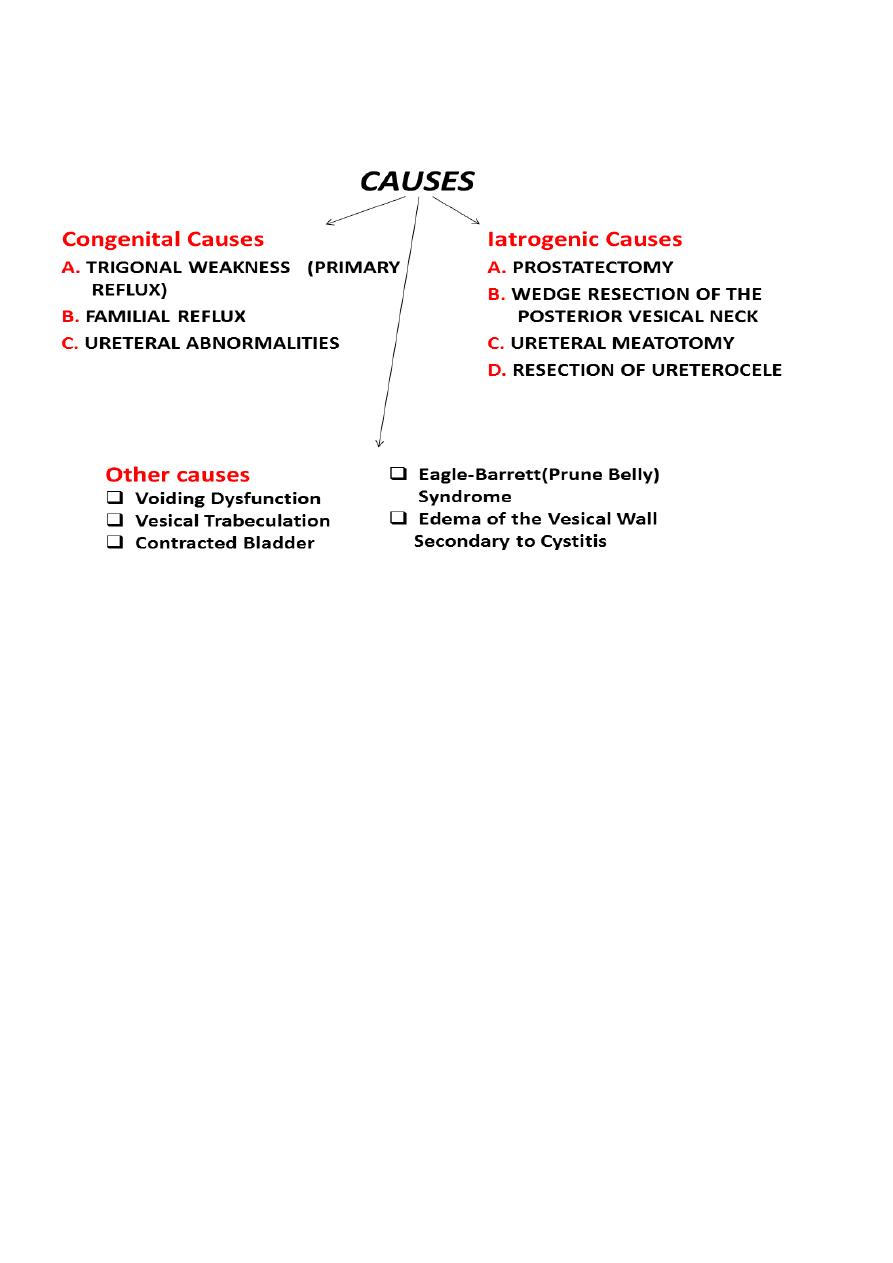
Etiology
1. Primary reflux is caused by lateral displacement of the ureteral orifice during
embryogenesis and a shorter intramural tunnel for the ureter, resulting in a poor
muscular backing. A weaker valve mechanism is therefore available to close the orifice
during bladder contractions.
2. Ureteral duplication is commonly associated with reflux into the lower pole ureter, again
owing to its abnormally short intramural tunnel.
3. Ureteral ectopia without ureterocele may be associated with reflux.
4. Abnormalities of the bladder wall such as diverticula, radiation cystitis, and
cyclophosphamide cystitis may predispose to vesicoureteral reflux. UTI may be associated
with transient reflux, due to the inflamed bladder wall.
5. Elevated intravesical pressure from any cause may lead to reflux. Common causes are
posterior urethral valves, detrusor hyperreflexia, and prostatic enlargement in adults.
6. Prune-belly syndrome is a congenital condition characterized by deficient anterior
abdominal musculature, bilateral cryptorchidism, bilateral megaureter, and often bilateral
vesicoureteral reflux.
7. Iatrogenic reflux may result from any surgical procedure that disrupts the trigonal
muscle, such as prostatectomy. Resection of the ureteral orifice can also produce reflux.
8. Dysfunctional voiding or elimination syndromes can lead to reflux. Voiding patterns
should always be elicited in the medical history.
Grading of VUR
• The degree of reflux is graded I–V.
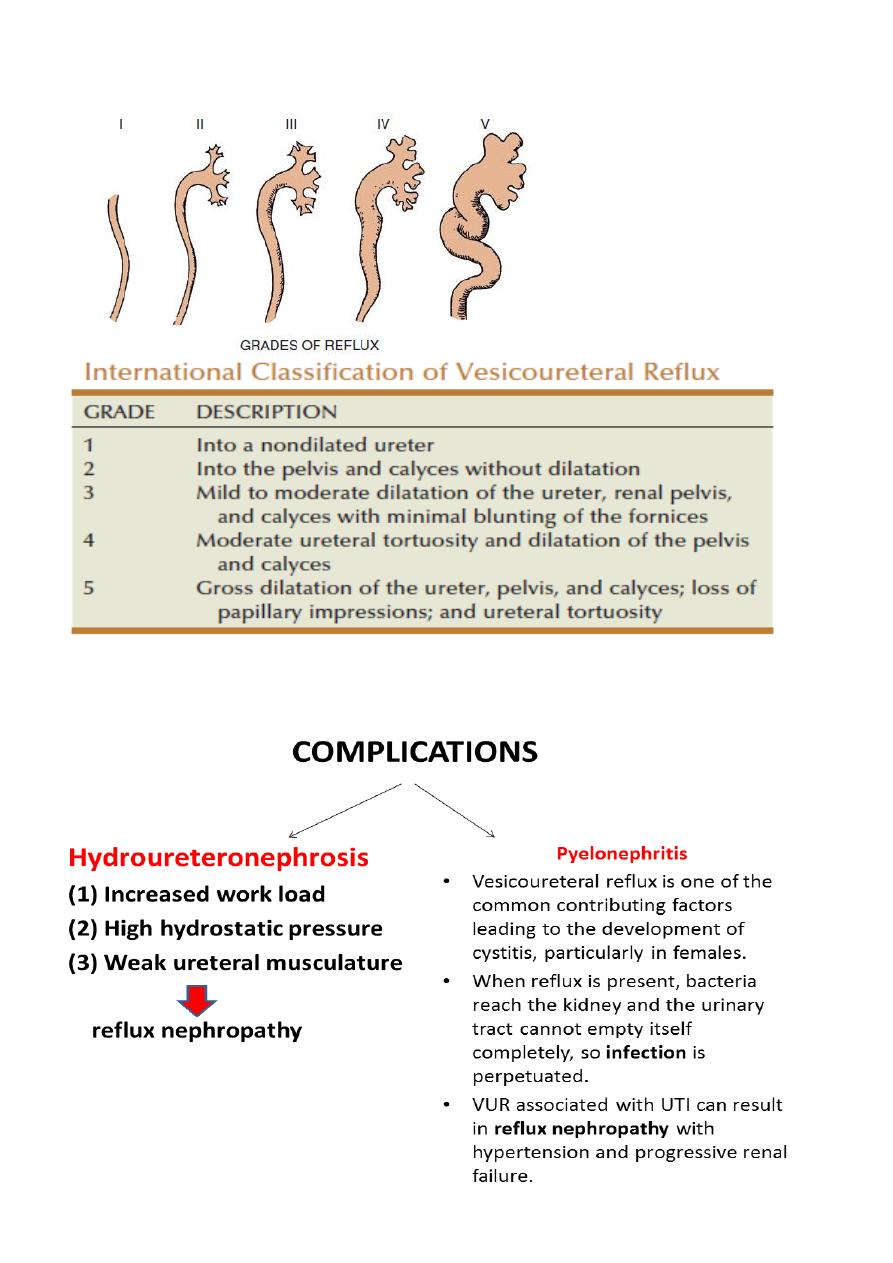
26
• Grading is based on the appearance of contrast agent in the collecting system during
voiding cystourethrography (VCUG(.
Complications

27
Presentation
Vesicoureteral reflux rarely causes symptoms.
Most patients present as recurrent UTI or pyelonephritis: have symptoms of fever, dysuria,
suprapubic or abdominal pain, failure to thrive, vomiting, and diarrhea.
In more advanced stages, the patient may present with uremia or hypertension.
Investigations
Urinalysis and culture to diagnose UTI
Urinary tract ultrasound scan to diagnose reflux
The VCUG:
the definitive examination
to diagnose and grade reflux and establish reversible causes
must include a voiding phase:
in some cases, reflux may be seen only during the elevated intravesical
pressures associated with micturition.
in visualizing the urethra, may allow the diagnosis of outflow obstruction to be
made (e.g., posterior urethral valves).
DMSA scan to detect and monitor associated renal cortical scarring.
The intravenous urography (IVU) findings are usually normal in lower grades of reflux.
Urodynamic assessment if suspicious of voiding dysfunction
Cystoscopy: to study position and morphology of ureteric orifices and exclude secondary
causes.
Management
• Correct underlying problems contributing to secondary reflux.
• Depending on:
o the grade of reflux as determined by VCUG
o the age of the patient at diagnosis
o unilateral versus bilateral disease
• Most primary VUR grade I–II cases will resolve spontaneously (~85%), with 50%
resolution in grade III.
• Observation and medical treatment are initially recommended.
Medical management
• Low-dose antibiotic prophylaxis should be given to keep the urine sterile and lower the
risk of renal damage until reflux resolves.
o Indicated in cases of low-grade vesicoureteral reflux without outlet obstruction
or another abnormality.
o Good patient compliance is necessary.
o Long-term antibiotic suppression with a regimen of amoxicillin (neonate),
trimethoprim/sulfamethoxazole, nitrofurantoin, or other antibiotic agent at one-
fourth to one-half the usual dose daily is commonly used.
• Anticholinergic drugs are given to treat bladder overactivity.

28
Medical management
If the patient remains asymptomatic, urine cultures are obtained periodically (e.g., every 3
months) during treatment. US and radionuclide cystogram should be obtained at yearly
intervals.
If acute (breakthrough) infection occurs, a full course of appropriate antibiotics is given and
a prophylactic regimen is then instituted.
Clinicians perform a dimercaptosuccinic acid scan (DMSA) to look for renal scarring at this
juncture.
Surgery is often recommended after breakthrough UTI.
Resolution of vesicoureteral reflux with antibiotic prophylaxis
• G1= 90%
• G2= 60%
• G3= 50%
• G4= 30%
• G5= 0%
Surgical therapy
• Indicated in patients with:
o high-grade primary reflux (grades 4 and 5)
o those with low-pressure reflux and significant hydroureter
o persistant reflux in girls after puberty
o patients in whom medical management has failed:
persistence of reflux after 3 to 4 years of antibiotic prophylaxis
multiple breakthrough infections
new or increased renal scarring
deterioration of renal function
noncompliance with medication
• Techniques of ureteral re-implantation include the following:
o Intravesical methods involve mobilizing the ureter and advancing it across the
trigone (Cohen repair) or reinsertion into a higher, medial position in the
bladder (Politano–Leadbetter repair(
o Extravesical techniques involve attaching the ureter into the bladder base and
suturing muscle around it (Lich–Gregoir procedure(
• Has a 98% cure rate.
• Approximately 1% of patients have obstruction of the ureterovesical junction after
ureteral reimplantation that requires reoperation.
• In patients with massive ureteral dilatation, tapering of the distal ureter may be
necessary during reimplantation.
• Rarely, temporary supravesical diversion is necessary in patients who are severely
uremic.
• Alternatively, endoscopic subtrigonal injection of Deflux into the ureteral orifice has
70% success, and 95% with repeated treatments.

29
Lec:14
Surgery
ANDROLOGY (Erectile Dysfunction)
Goals and Objectives
Define erectile dysfunction (ED)
Discuss the most common causes of ED
Review a practical evaluation of men with ED
Review the treatment options
Provide suggestions for urologic referral
What is ED?
ED is the inability to achieve and maintain an erection adequate for intercourse to the
mutual satisfaction of the man and his partner.
Remember, both partners in a relationship are affected.
Incidence
20-30 million American men suffer ED
Age dependent
o 2% men age <40 years
o 25% men age 65
o 75% men >75 years
Not a necessary occurrence of the aging process
How Does an Erection Occur?
The brain controls all sexual functions, from perceiving arousal to initiating and
controlling the psychological, hormonal, nerve, and blood flow changes that lead to an
erection.
Hormones, including testosterone, control the male sex drive
Nerve impulses relay signals of arousal and sensation to and from the penis
Arteries deliver extra blood to the penis that causes it to stiffen.
Veins then drain the blood out of the penis after intercourse.

31
Physical or Psychological Stimuli Results
Sacral parasympathetics (S2,3,4) stimulation to the penile nerves
Dilation of the penile arteries
Relaxation of the smooth muscle in the corporal bodies of the penis
Decrease venous outflow
An Erection Requires a Coordinated Interaction of Multiple Organ Systems
Psychological
Endocrine
Vascular
Neurologic
Mechanism of Smooth Muscle Relaxation
Release of Neurotransmitters-nitric oxide
Conversion of GTP to cGMP - erection
Breakdown of cGMP by PDE type 5 - detumesence
Cause of ED
Psychogenic Causes:
o Anxiety
o Depression
o Fatigue
o Guilt
o Stress
o Marital Discord
o Excessive alcohol consumption
Organic Causes
o Cardiovascular disease
o Diabetes mellitus
o Surgery on colon, bladder, prostate
o Neurologic causes (lumbar disc, MS, CVA)
o Priapism
o Hormonal deficiency

31
Risk Factors
Massachusetts Male Aging Study (Feldman Ha, J Urol 1994; 151:54-61)
Treated heart disease
39%
Treated diabetes
28%
Treated hypertension
15%
Other risk Factors (Benet et al. Urol Clinic North Am. 1995; 151:54-61)
Diabetes
27% - 59%
Chronic renal failure
40%
Hepatic failure
25% - 70%
Multiple Sclerosis
71%
Severe depression
90%
Other (vascular disease, low HDL, high cholesterol)
Causes of ED
Hormone Deficiency
End Organ Failure
Blockage of Blood Vessels
Venous Leak
Spinal cord injuries: 5% - 80%
Pelvic and urogenital surgery and radiation
Substance abuse
Alcohol: >600ml/wk
Smoking amplifies other risk factors
Medications may be responsible for ~25% of cases of ED
Bicycle riding
Medication:
o Most common cause of ED in men >50
o Many men are polymedicated
o Also have co-morbid conditions
o Anti-hypertensive drugs
All capable
Common: thiazides and beta blockers
Uncommon: calcium channel blockers, alpha-adrenergic blockers, and ACE
inhibitors
o CNS drugs:
Antidepressants, tricyclics, SSRIs

32
Tranquilizers
Sedatives
Analgesics
o H1 and H2 receptor blockers
o Anticholinergics
o LHRH agonists (Lupron, Zolladex)
o Alcohol
o Tobacco
o Drug abuse
o Estrogens, Ketoconazole
A Practical Evaluation of Men with ED
#Basic evaluation
Medical History
Cardiovascular history
Endocrine history
Sexual history/questionnaire
Physical exam:
o Focused neurovascular exam
o Size of testis
o DRE
Lab tests
o UA
o Testosterone, CMP, Lipid panel
o PSA in men >50 years
#Sexual History
Premature ejaculation
Retarded ejaculation
Painful intercourse
Anorgasmia
Decreased Libido
Dissatisfaction with sex life
Do you have any problems with intimacy with your partner?
Do you have early morning erections?
Do you have erections with self-stimulation?

33
Are you able to consistently obtain and maintain an erection sufficient for sexual
intimacy?
Does it hurt to have an erection or intercourse?
Do you ejaculation sooner than you would like?
Does it take too long to reach an orgasm?
Do you fail to reach an orgasm?
Did your erection problems start suddenly or over time?
#ED Questionaire³
When you had erections with sexual stimulation, how often were your erections hard
enough for penetration?
How do you rate your confidence that you could get and keep an erection?
³The International Index of Erectile Function, Urol 1997;49:822-830
During sexual intercourse, how often were you able to maintain your erection after you
had penetrated your partner?
During sexual intercourse, how difficult was it to maintain your erection to completion
of intercourse?
When you attempted sexual intercourse, how often was it satisfactory for you?
#Differentiating Psychogenic from Organic ED
Psychogenic Impotence:
Younger patient (<40)
Preservation of morning erections and nocturnal erections
Achieve erection with masturbation
May be partner-specific
Often sudden onset
Organic ED:
Gradual deterioration
Decrease in morning erections and nocturnal erections
No erections with masturbation
No loss of libido
Presence of co-morbid conditions

34
#Physical Examination
Blood pressure
Examine penis (R/O Peyronie’s disease)
Determine size and consistency of testes
Digital rectal exam
Focused vascular exam/peripheral pulses
Focused neurologic exam
#Laboratory Tests
UA (glycosuria) – Fasting if elevated
PSA in men over 50
Testosterone (best to draw in A.M.)
Prolactin, Thyroid function, Lipid profile, Liver function, Creatinine
#Other Tests
NPT – Nocturnal Penile Tumescence Test
Penile doppler
Injection of vasoactive drugs
NEVA (Nocturnal Electobioimpedance Volumetric Assessment)
Treatment Options
#Goal directed therapy
Find out what the patient wants
Try to tailor the treatment to the patients needs and wants
Etiology rarely affects treatment choice for the patient
Nonpharmacologic
Non-invasive
Minimally invasive
Invasive
Counseling and/or sex therapy
Oral medications - Viagra, Levitra, Cialis

35
Urethral suppositories (MUSE)
Injection therapy - Caverject, Trimix, Bimix
Vacuum constriction device
Surgery
Sex therapy
#Counseling and/or Sex Therapy
Rule out depression
Try oral medication in patient with psychogenic impotence
Refer to sex therapist or psychiatrist for sever psychopathology
#Nonpharmacologic Treatment Options
Lifestyle changes:
Reduce fat and cholesterol in diet
Decrease or limit alcohol consumption
Eliminate tobacco use and substance abuse
Weight loss if appropriate
Regular exercise
#Ideal Medication for Treatment of ED
Effective
Available on demand
Free of toxicity and side effects
Easy to administer
Inexpensive
#Medication
(Viagra, Levitra, Cialis)
Mechanism of Action:
PDE inhibitor and increases the cGMP that promotes and sustains smooth muscle
relaxation
(PDE Inhibitors)
Indications:
Psychogenic ED
Mild vasculogenic ED
Neurogenic ED
Side effects from medication(s) patient is already taking

36
Side effects:
Headache
Flushing
Dyspepsia
Nasal congestion
Visual disturbances
Priapism
Contraindications:
Organic Nitrites:
o Oral
o Sublingual
Severe cardiac disease
o Obtain stress testing
(Yohimbine, Yocon, Erex, Yohimex)
Alpha 2 andrenoreceptor antagonist
Dose: 5.4 mg TID
Results: ~20% (same as placebo)
Side effects: increase blood pressure, tachycardia, anxiety
Trazodone(Desyrel)
Anti-depressant associated with priapism
Mechanism of action nor fully understood
Nor FDA approved for ED
Side effects: drowsiness, dry mouth, sedation, priapism
Apomorphine (Spontane)
Dopaminergic mechanism with hypothalamic activity
Sublingual administration
64% to 67% response rate with ED
Side effects: nausea, sweating, hypotension, yawning
Awaiting FDA approval
Phentolamine (Vasomax)
Alpha-blocker
Relaxes smooth muscle tissue
40% efficacy in mild organic ED
Side effects: nasal congestion, tachycardia, dizziness, hypotension
Awaiting FDA approval

37
Side effects
Discontinue tobacco, alcohol, and abusive drugs
Alter dosage of drugs with ED side effects
Change to another class of drugs
Transurethral Therapy (Alprostadil – MUSE)
Mechanism of Action: vasodilator
Administration: 125, 250, 500. 1000ug
Insert in the urethra
Erection occurs 10-15 minutes later
Erection lasts 30-45 minutes
Results: 10-65%
Side effects: Pain, bleeding, priapism (<3%)
Penile Injection Therapy (Caverject, Edex, Tri/Bi-Mix)
Mechanism of action: smooth muscle vasodilator
Administration: 10, 20, 40ug
Inject directly into corporeal bodies of the penis
Results: 70%-90%
Dropout rates: 25%-60%
Side effects: pain (36%), priapism (4%), fibrosis
Androgen Replacement Therapy
Indications: hypogonadism (<285ng/dl)
Avoid oral estrogens-increase LFTs
Injectable – 200mg testosterone (cypionate, enathate, propionate), q2-3 weeks
Transdermal (Patch or gel)
Avoid in patients with prostate or breast cancer
Slight increase risk of BPH
Monitor all patients with annual DRE and PSA
Vacuum Constriction Device
Mechanism of Action:

38
Penis placed in plastic tube
Air evacuated from the tube
Blood trapped in penis with constricting ring
Erection limited to 30 minutes
Results: 80%-90%
Contraindications: bleeding disorders, sickle cell disease, anticoagulation
Complications: coolness, petechiae, numbness, pain with ejaculation
High drop out rate
Was previously first-line treatment for ED
Seldom used now that oral therapy is available
Considered an alternative if patient fails oral therapy and does not want to proceed
with surgery
Penile Prosthesis
Indications:
Patients who have failed other therapies
Peyronie’s disease
Severe vasculogenic disease
Choosing a Penile Prosthesis
Considerations:
Medical condition
Lifestyle
Cost
Insurance coverage
As with all prescription products, complications are possible
Malleable Prosthesis
Easy for patient and partner to use
Few mechanical parts
Same-day surgery usually possible
Least expensive type of prosthesis
Two-Piece Inflatable Prosthesis
Small inflation pump provides comfort and ease
Fast and easy one-step deflation procedure
Better conceal ability when flaccid than with malleable or self-contained devices

39
Three-Piece Inflatable Prosthesis
Most closely approximates the feel of a natural erection
Cylinders expand in girth
Some cylinders have the potential to expand in length
When inflated, it feels more firm and more full than other prosthetic erections
When deflated, it feels softer and more flaccid with better conceal ability than with
other prosthetic devices
Penile Prosthesis
Advantages:
Low-morbidity
Low-mortality surgery
Low complication rates
High success rates – 5% malfunction rate at 5 years
High satisfaction rate – 87%
High partner satisfaction rate
Good rigidity
Freedom from medications
Outpatient/24HR surgery
Resume sexual activity 4-6 weeks
No loss of ability to ejaculate or achieve orgasm
Disadvantages:
Surgery
Expensive
Possible mechanical failure
Insurance Reimbursement
Covered by most companies, including Medicare
No co-payment for men with Medicare supplemental insurance

41

41
Lec:15
Surgery
INFERTILITY
The inability of a sexually active, non-contracepting couple to achieve pregnancy in one year
EPIDEMIOLOGY
25% of couples don’t achieve pregnancy within one year, 15% of them seek medical
treatment.
The chance of normal couples conceiving is estimated to be:
o 20% per month
o 75% by 6 months
o 90% by 1 year
20% of infertility cases are due to male factors & 30-40%of them due to both male &
female factors.
Fertility rates are at their peak in men & women at age 24 years,beyond that age,they
decline in both sexes.
25-35% of infertility couples will conceive at sometime by intercourse alone.
Goals of evaluation of infertile men
1. Identification of reversible disorders.
2. Identification of irreversible conditions.
3. Identification of chromosomal & genetic abnormalities that may affect the offspring.
4. Identification of idiopathic cases.
Prognostic factors
1. Duration of infertility.
2. Primary or secondary infertility.
3. Results of seminal fluid analysis(SFA).
4. Age & fertility state of female partner.
Evaluation of infertile male
History.
Physical examination.
SFA.
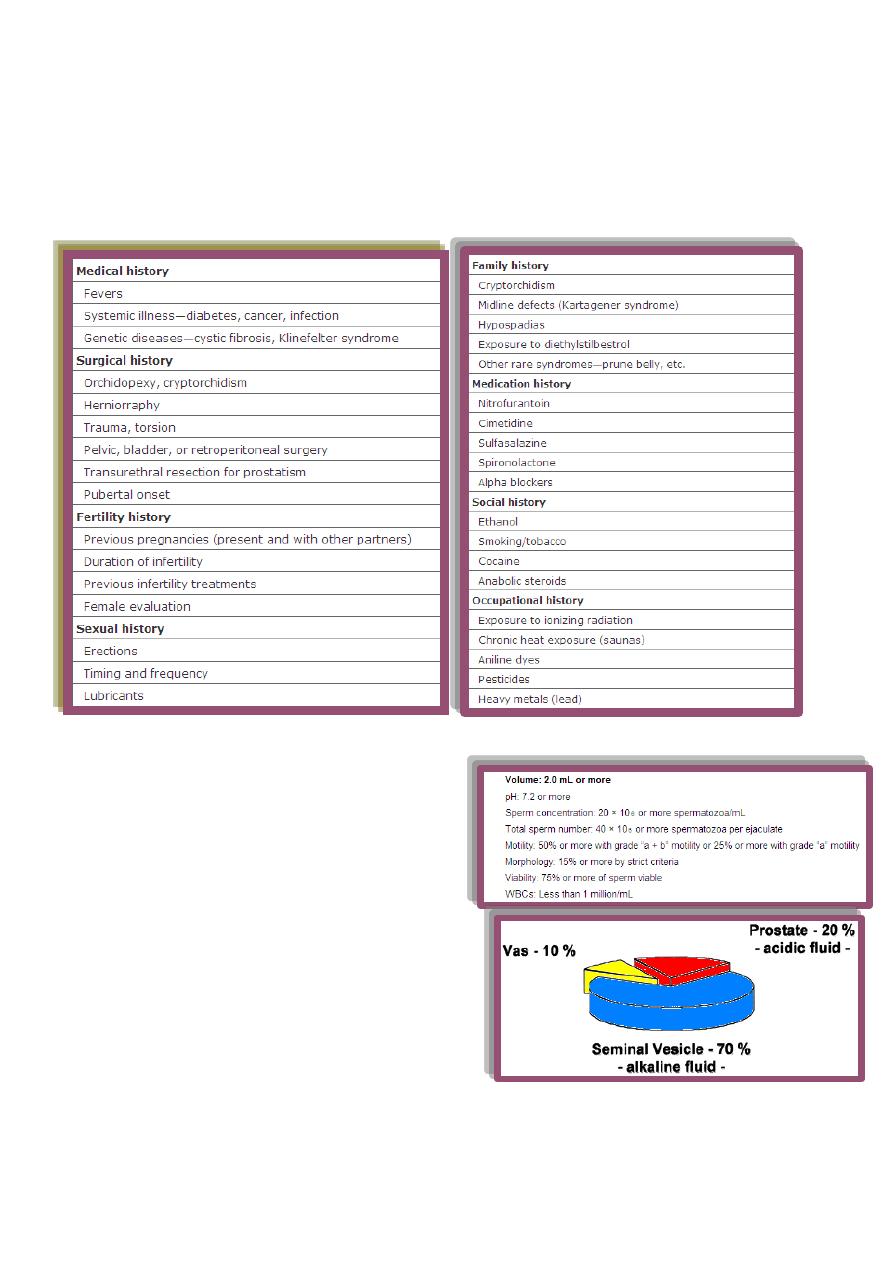
42
Adjunctive laboratory investigations.
Radiologic investigations.
Testicular biopsy.
History
Physical examination
Abnormal secondary sexual characters.
Gynecomastia.
Genital examination:
Penis
Scrotum
Spermatic cord.
DRE.
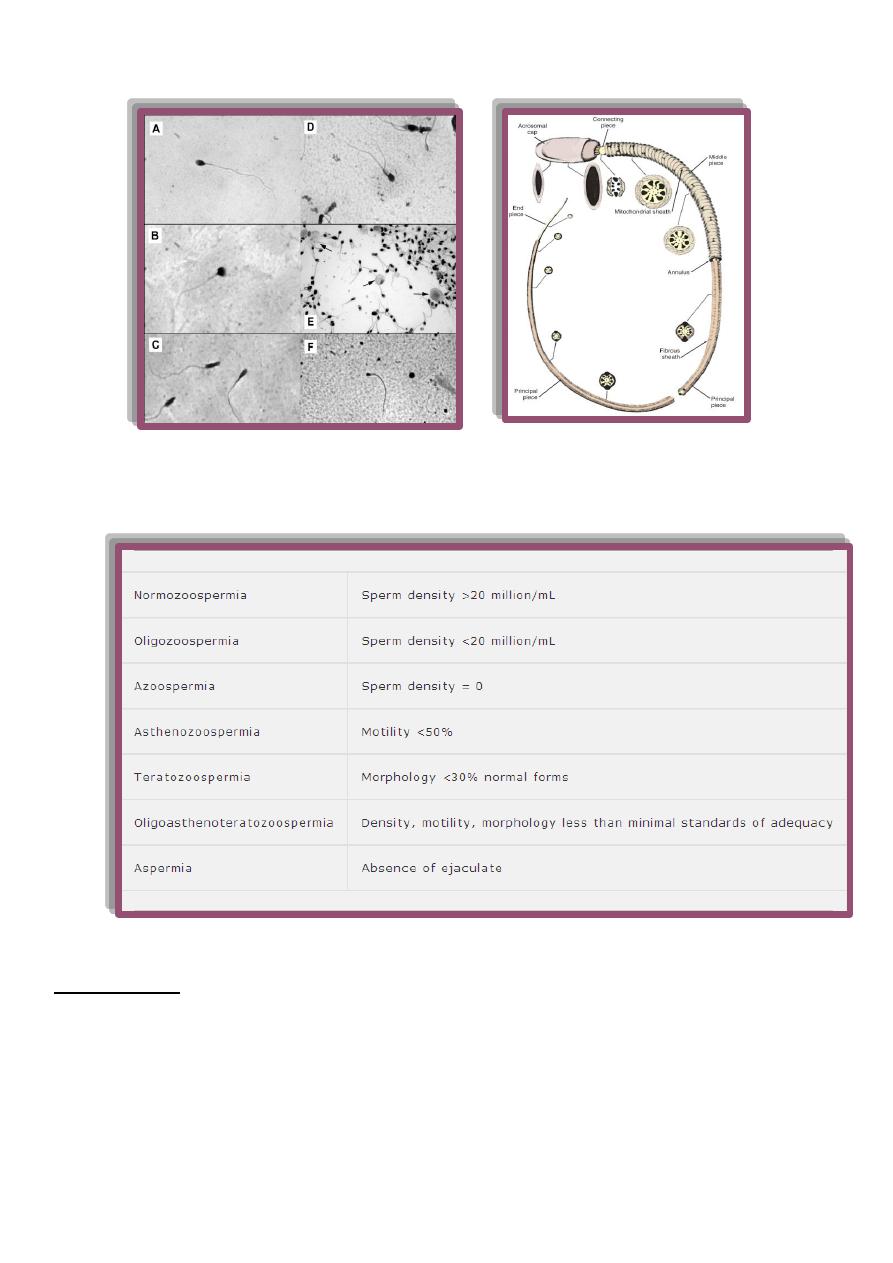
Seminal fluid analysis (SFA)
2 0r 3 samples examined over a period of several weeks for more accuracy.
Sample collection.
43
Sperm morphology
SFA nomenclature
Adunctive laboratory tests
Semen culture
For pyospermia (3-23% of infertility case).
Immature germ cells vs. leukocytes ??
Indications :
1. History of genital infection.
2. Presence of > 1000 pathogenic bacteria/ml.
3. Presence of >10⁶ WBC/ml.
44
Semen fructose
Indicated in seminal fluid with low ejaculate volume, acidic PH & no sperms.
Absent in seminal vesicle agenesis or obstruction.
Post ejaculate urinalysis
For suspected retrograde ejaculation.
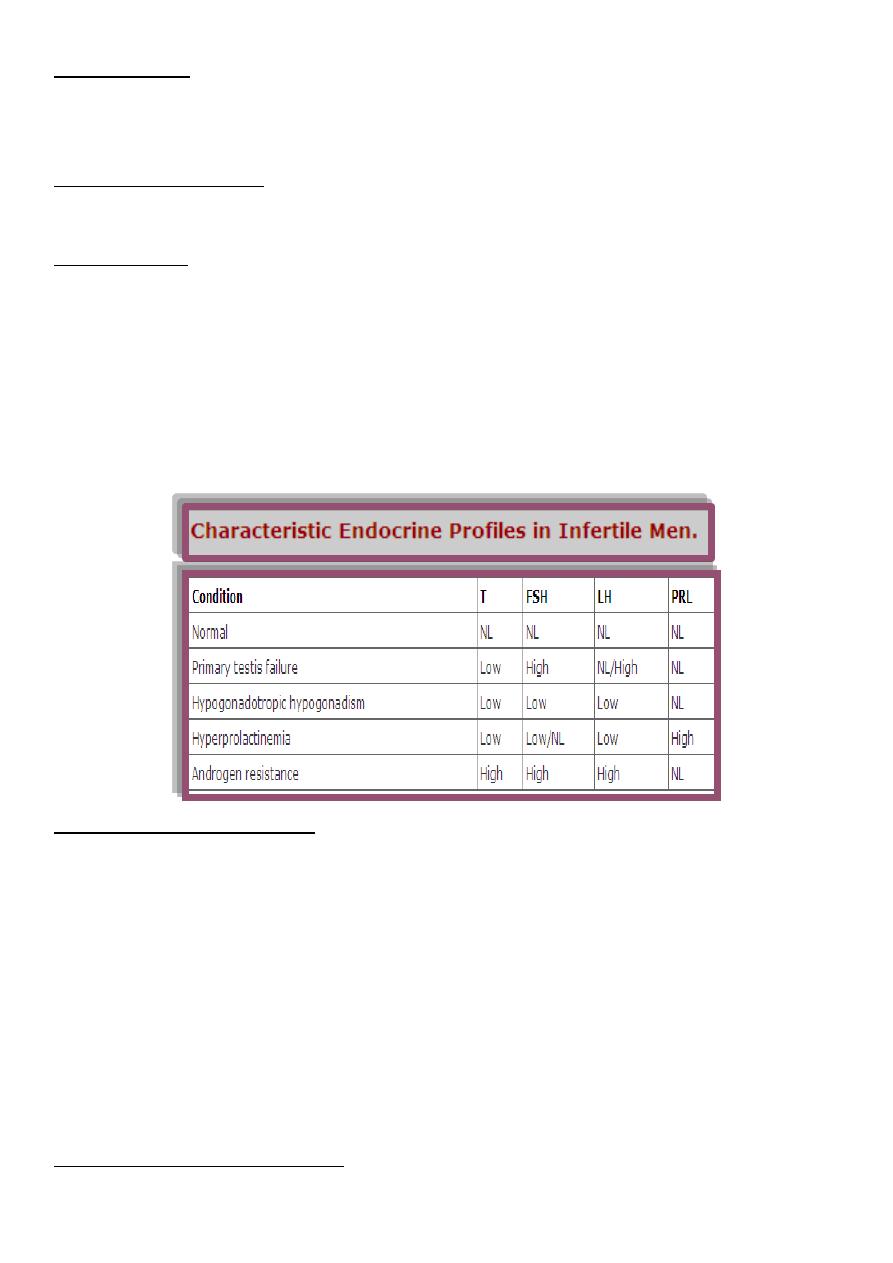
Hormonal tests
Less than 3% of infertile men have hormonal etiology.
Used to evaluate the hypothalamo-pituitary-gonadal axis.
Testosterone,LH,FSH &prolactin are the main hormones.
Indications of hormonal evaluation:
1. Sperm density< 10x10^6/ml
2. Impaired sexual function.
3. Findings suggestive of a specific endocrinopathy.
Antispermantibody (ASA) test
These antibodies occur if the blood-testis barrier is broken(by testicular trauma or
torsion or by vasectomy).
Indirect Ab. or direct Ab.
Commonly measured by mixed agglutination reaction.
ASA are detected in 10% of infertile men vs. 2% of fertile men.
Indications:
1. Sperm agglutination or clumping by SFA.
2. +ve postcoital test(PCT).
3. Low sperm motility with history of testicular injury or surgery.
4. Unexplained infertility.
Chromatin/DNA integrity testing.
45
Electron microscopy
For ultrastructural defects in sperms.
Indicated if sperm motility < 5-10 % with good viability of sperms.
Sperm function tests
1.Sperm-cervical mucus interaction
Indicted in:
Hyperviscous semen.
Low volume semen with normal sperm count.
Suspected cervical mucus abnormalities.
Unexplained infertility.
2.Sperm viability assay (hyposmotic swelling test)
Used if sperm motility<5-10%.
3.Sperm penetration assay
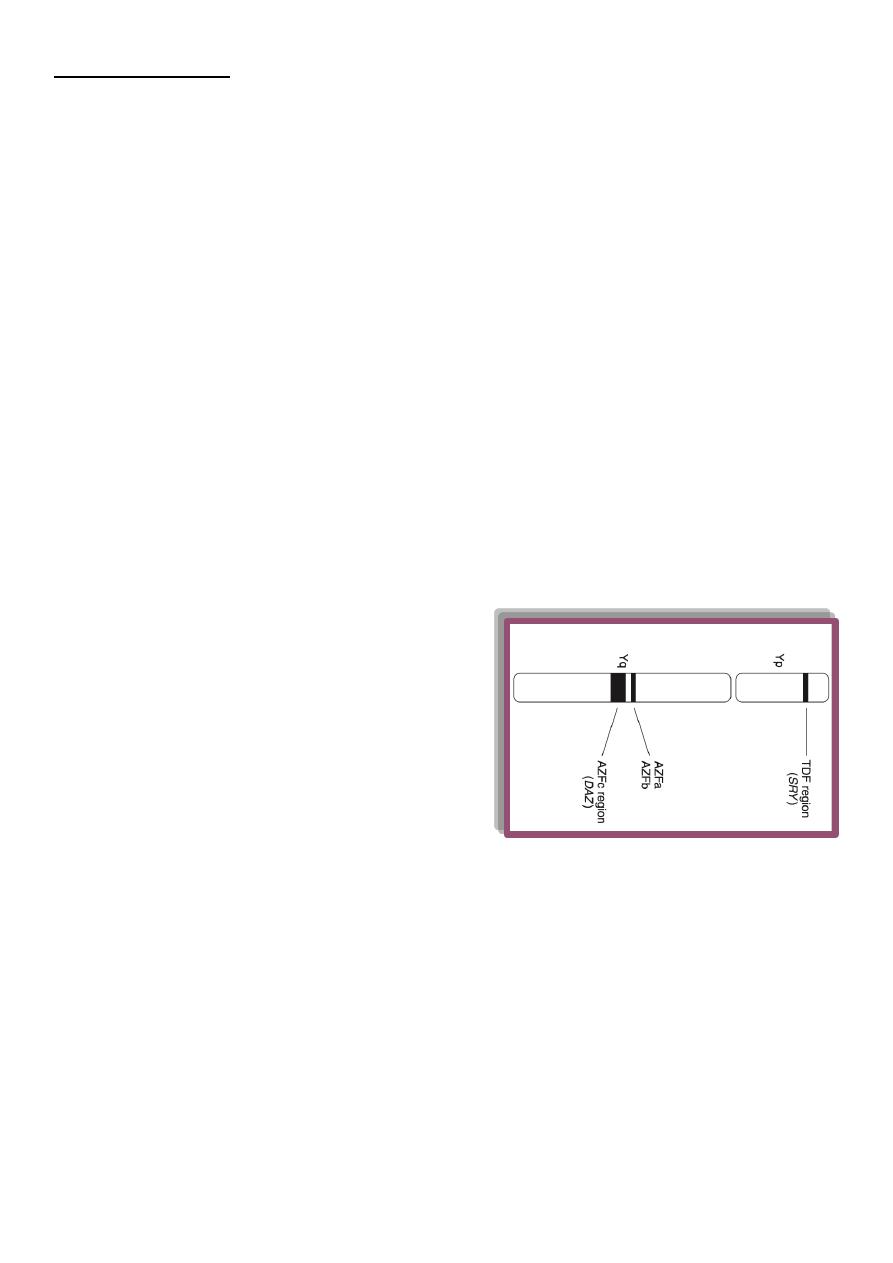
Genetic (chromosomal) tests
Indicated in azospermia or severe
oligospermia.
5.8%of infertile men have genetic defects.
The defects are either:
o Numerical (e.g. klinefilter syndrome).
o Structural (e.g. CFTRG mutations).
The defects are in the sex chromosomes or
autosomes.
Y chromosomes microdeletions ( AZFc is the most common).
Radiologic investigations
Vasography
Used to assess the patency of the vas, seminal vesicles & ejaculatory duct & to aspirate
vasal fluid.
The best timing of it is prior to vasal reconstructive surgery.
Indicated in :
1. Azospermia with normal testicular biopsy.
2. Severe oligospermia
46
Venography
The best tool to diagnose varicocele & to treat it by embolization (via femoral or internal
iliac veins).
Ultrasonography (US)
1. Scrotal US: for varicocele or testiculr tumors.
2. Abdominal US: to detect renal agenesis (in 80% of pt. with unilateral CAVD).
3. Transrectal U.S.(T.R.U.S.)
To assess the prostate,seminal vesicles,ejaculatory duct &vas.
Indicated in azospermia with suspected ejaculatory duct obstruction.
Equivocal TRUS findings in suspected ejaculatory duct obstruction can be confirmed by
seminal vesicle aspiration.
Testicular biopsy
Either
diagnostic( to differentiate obstructive from non-obstructive azospermia in pt.with normal
testicular size & normal FSH level).
Or
theraputic (to harvest sperms for IVF or for cryopreservation).
Histological forms seen in testis biopsy
1. Normal testis.
2. hypospermatogenesis.
3. Maturation arrest.
4. Germ cell aplasia(Sertoli cell only syndrome).
5. End stage testis(sclerotic testis).
47
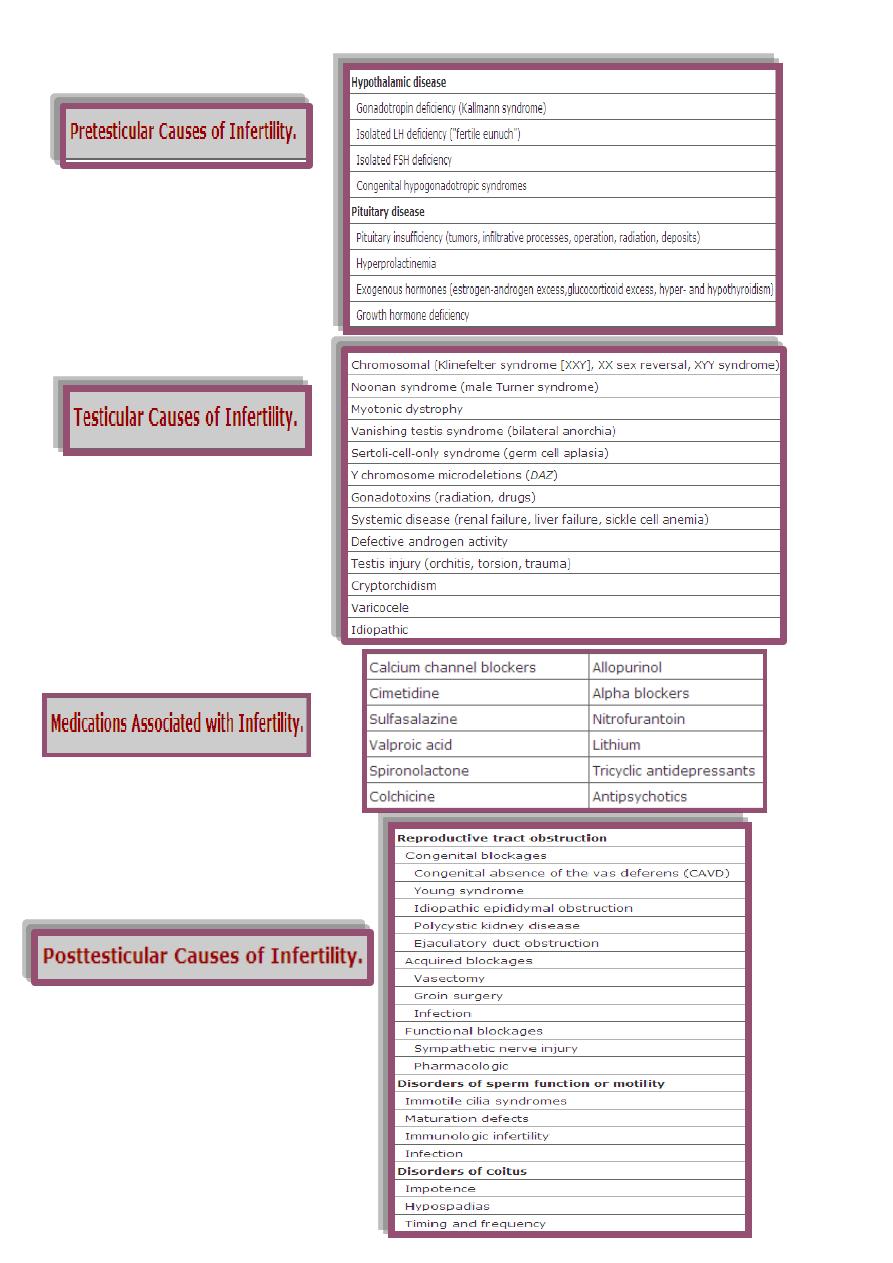
Causes of male infertility
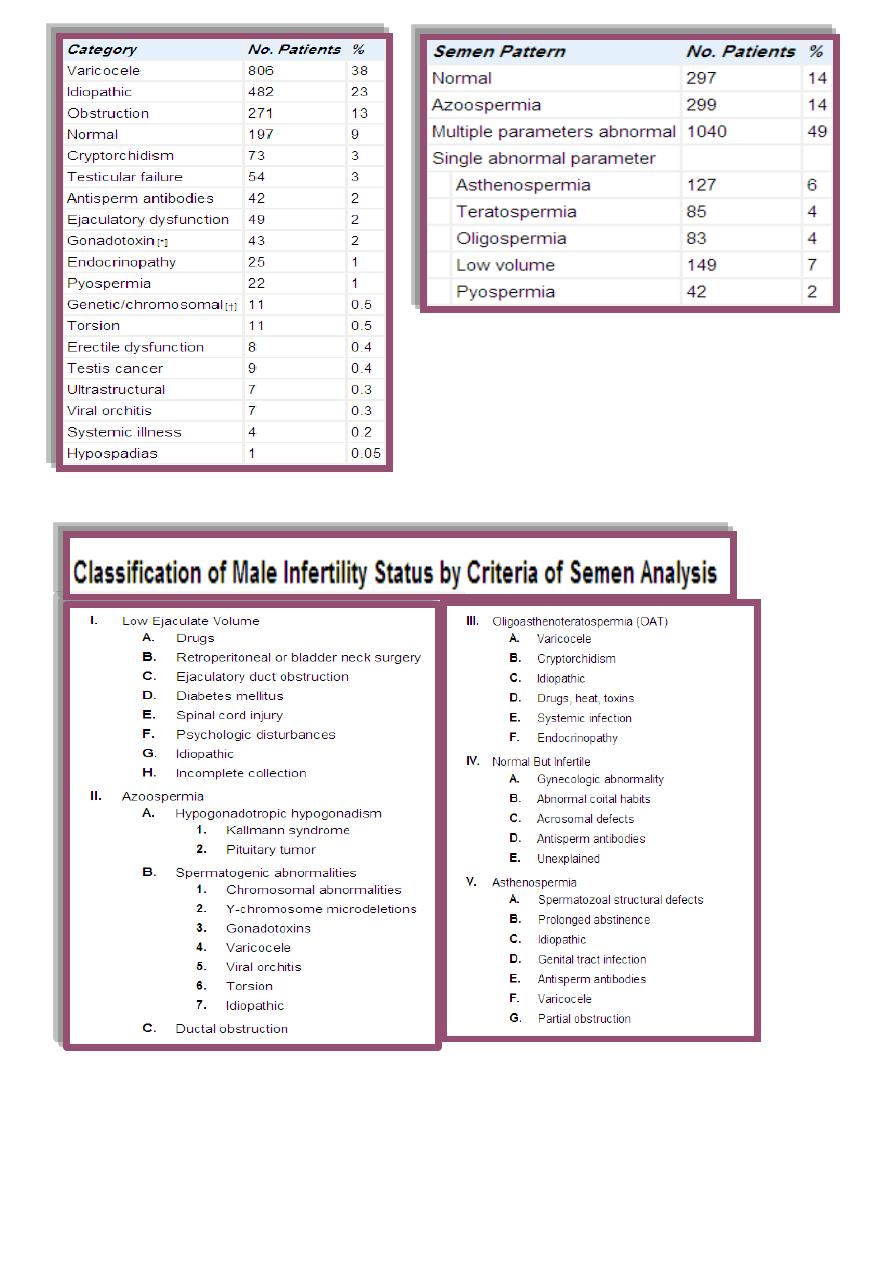
48
49
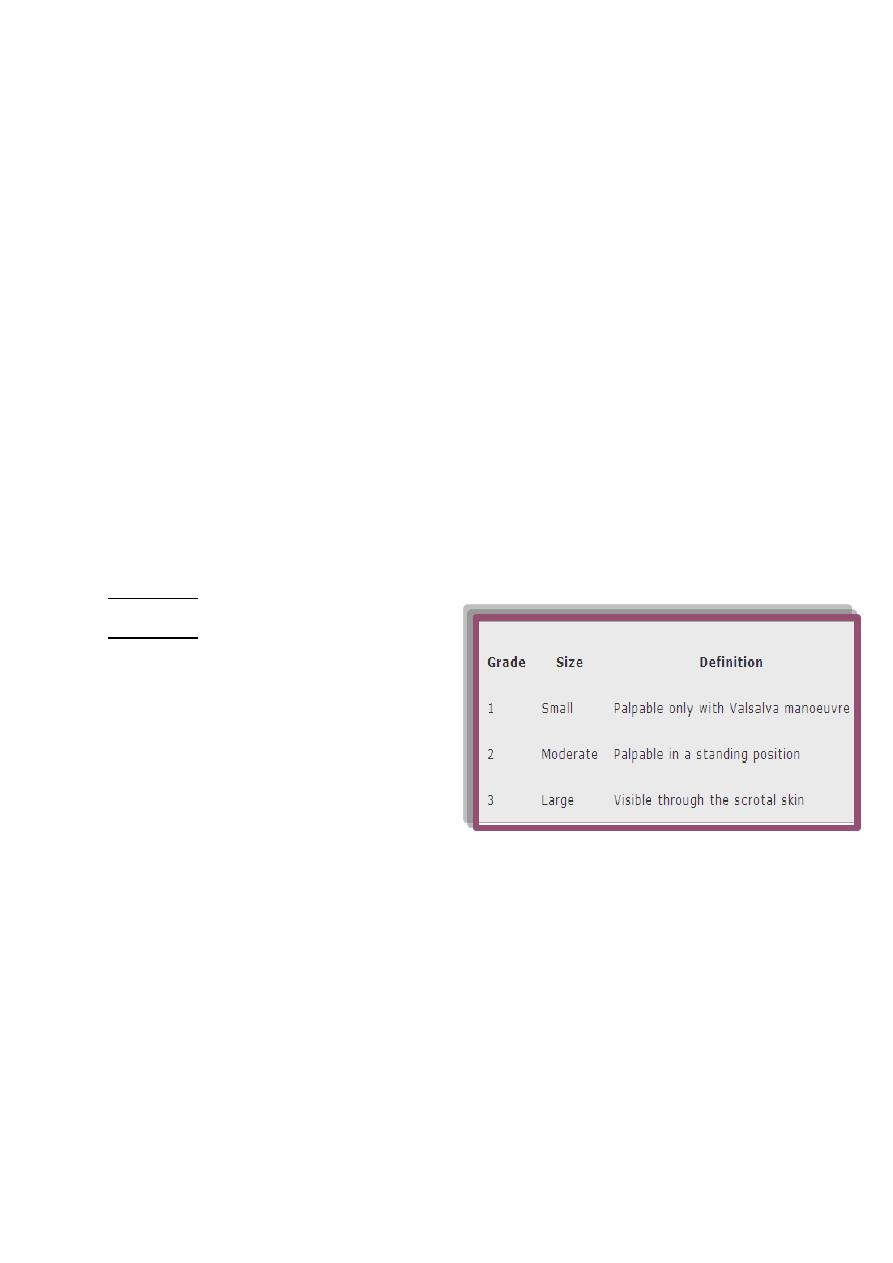
varicocele
Abnormally dilated testicular veins within the spermatic cord.
o Clinical vs. subclinical varicocele.
o Affects 15%of normal adolescents vs. 20-40% of infertile men.
o 90% left sided-10% bilateral.
o The most common surgically correctable cause of infertility.
Why it occur?
MULTIFACTORIAL
o Anatomic variations.
o Raised Hydrostatic pressure.
o Raised Testicular temperature.
o Reflux of renal &adrenal metabolites from renal vein.
ALLreduced testicular size,sperm motility & count infertility.
Diagnosed: clinically, SFA, oppler scrotal U.S.
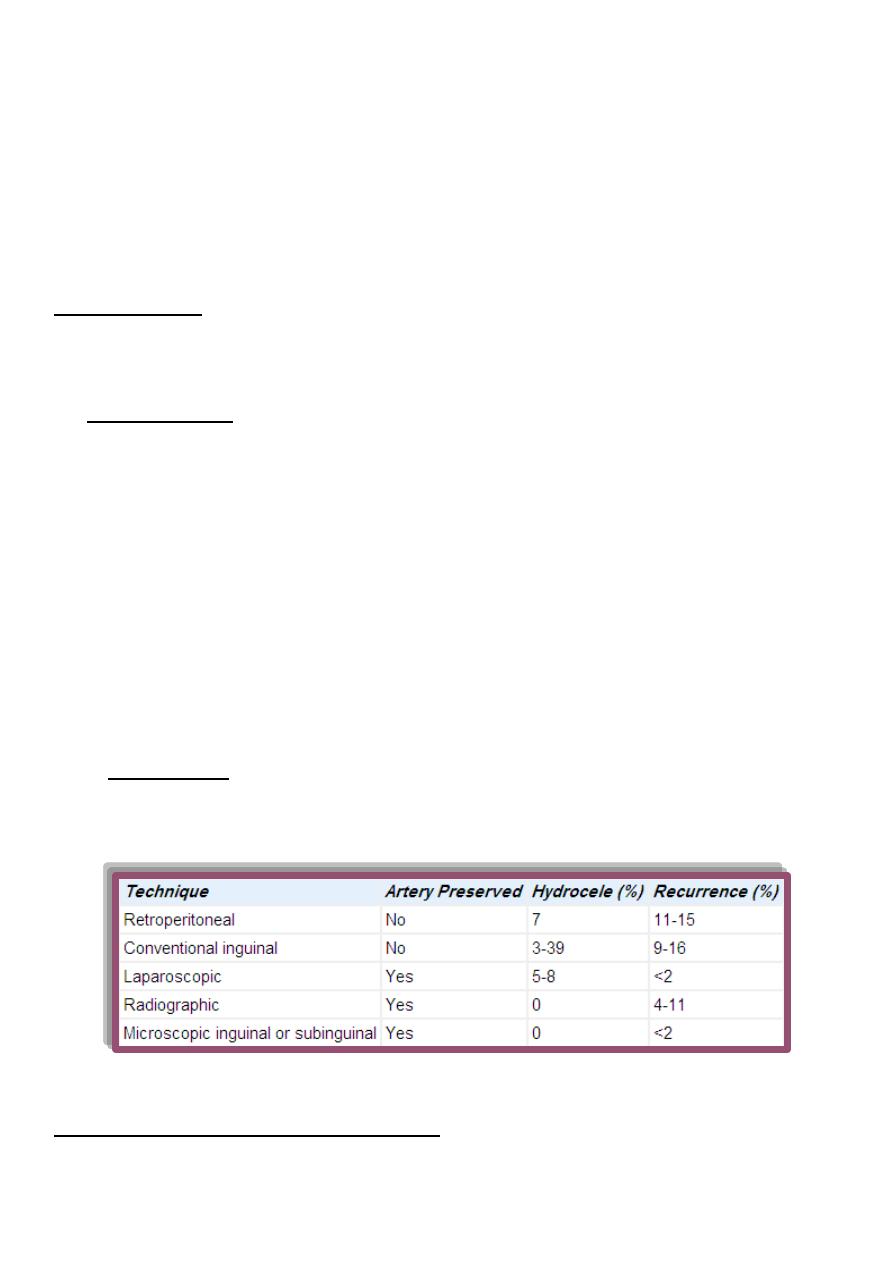
Treatment
surgical
1.embolization.
2.ligation of dilated testicular veins:
*retroperitoneal
*inguinal
*subinguinal
*laparoscopic
This Rx. Improve seminal parameters in 70% of pt. & improve conception rate in 40-
50% of couples.
For whom to do surgery?
clinical varicocele.
abnormal SFA or infertility.
affected testicular growth especially adolescents.

51
Treatment of male infertility
o It is better to improve male/female fertility & to allow natural conception
o If this is not successful, assissted reproductive techniques(ART) are used.
o Types:
medical Rx.
surgical Rx.
ART.
Medical Rx.
1. Life style modifications.
2. Hormonal Rx.
o Gonadotropins(LH/FSH)
*Used for hypogonadotrophic hypogonadism.
*Formulae: HCG, HMG or recombinent FSH.
o GnRH
uesed only for hypogonadotrophic hypogonadism with intact pituitary function.
o Testosterone Rx.
different formulae are used to induce virilisation in pt. with primary or secondary
testicular failure.
excess testosterone is a male contraceptive.
Antiprolactinaemic drugs For hyperprolactinaemia.
Treatment of thyroid disorders, estrogen excess & corticosteroid excess.
Corticosteroids
*used for immunologic infertility( it accounts for 10% of infertility cases).
*It achieves pregnancy rate = 30-40%.
3. Treatment of pyospermia
proper antibiotics
antioxidants.
frequent ejaculation.
4. Empirical medical Rx.
for idiopathic infertility(25% of *infertility cases).
Not proven effective.
Includes clomiphen citrate, tamoxifen & GnRH/gonadoropins
51
5. Other drugs
kallikreins,antioxidants,zinc,arginine& L-carnitine.
6. Growth hormones
For oligospermia(under investigations).
Surgical treatment
1. Varicocele Rx.
Ligation of dilated testicular veins to eliminate retrograde reflux of venous blood
via gonadal veins.
Types of surgery:
*percutaneous embolization.
*surgical ligation via:
-retroperitoneal
-inguinal
-subinguinal
-laparoscopic routes.
Improved seminal parameters in 70% of pt.
Improved pregnancy rate in 40-50% of pt.
Complications:
1. recurrence 2. hydrocele
3. vasal injury 4. testicular atrophy.
2. Repair of vasal or epididymal obstruction.
Vasovasostomy
52
*indicated for vasectomy reversal.
*Complications
1.testicular atrophy 2. hematoma 3.recurrence(3-12%).
*patency & pregnancy rate:
Vaso-epididymostomy
indicated in
reversal of vasectomy for >15 years(if vasovasostomy failed).
epididymal obsruction.
Patency rate: 30-65%.
Pregnancy rate: 20-40%.
3. Rx. Of ejaculatory duct obstruction
Ejaculatory duct obsruction accounts for 1-5% of infertility cases.
Treated by transurethral ejaculatory duct resectionn(TUEDR).
Patency rate: 65-70%.
Pregnancy rate: 20-30%.
4. orchidopexy.
5. Surgical Rx. Of pituitary tumors.
6. Rx. Of ejaculatory dysfunction
a. Retrograde ejaculation(RGE)
treated by alfa-agonists or TCA or sperm retrieval for IVF.
b. Anejaculation
absent seminal emission.
mostly caused by spinal cord injury& retroperitoneal lymph nodes dissection &
sometimes psychologic.
Treated by
penile vibratory stimulation or electroejaculation.
The semen obtained is used for IVF.
Success rate: 75%.
53
7. Rx. Of anatomic,congenital & organic causes of male infertility
Hypospadias repair.
Plication of peyronies disease.
Rx. Of erectile dysfunction.
Assissted reproductive technologies(ART)
Intrauterine insemination(IUI).
In vitro fertilization(IVF).
Intracytoplasmic sperm injection(ICSI).
Gamete intrafallopian transfer(GIFT)
-zygote intrafallopian trasnfer(ZIFT)
-tubal embryo transfer(TET)
Intrauterine insemination
(IUI)
*Indicated in:
male factor infertility.
unexplained infertility.
cervical mucus or anatomic abnormalities that interfere with sperm deposition at the
cervical os.
*Office procedure, no anasthesia.
*Success rate: 15-20%.
*Complications
1.Uterine cramps 2.pelvic infections. 3.Multiple gestations.
IVF
It includes harvesting the oocyte & sperm in order to incubate them for fertilization then
transferring the embryo to the uterine cavity.
Pregnancy rate: 20-30% per cycle.
Costs: 12000-15000 $ per cycle.
Indications:
failed medical or surgical Rx. or IUI.

54
CBAVD.
severe oligospermia.
cryopreserved sperms.
azospermia( obstructive or non).
few viable sperms in the ejaculate.
Sperms are retrieved for IVF by:
percutaneous epididymal sperm aspiration (PESA)
microsurgical epididymal sperm aspiration (MESA).
Testicular sperm aspiration (TESA).
Testicular sperm extraction (TESE) microsurgical, nonmicrosurgical
Intracytoplasmic sperm injection(ICSI)
A special micromanipulation of the sperm into the cytoplasm of a harvested oocyte.
Useful in severe oligosprmia,azospermia & ultrasructural sperms defects.
Conception rate: 50% per cycle.
Varicocele repair,vasovasostomy or vasoepididymostomy are more cost effective
with a better pregnancy rate than IVF/ICSI.
MOST COUPLES PREFER,
NATURAL FOODS,
NATURAL FIBERS,
AND
NATURALLY CONCEIVED BABIES
