Metacarpal periostitis(Bucked Shins, Sore Shins and Stress Fracture )
Periostitis and stress fracture of the dorsal surface of the third metacarpal bone constitute a spectrum of diseases that are commonly observed in young(2 to 3 years of age) fast gaited horses.The term "bucked shins" traditionally implied a painful condition of the dorsal metacarpal region resulting from subperiosteal hemorrhage and in some cases microfracture. Compression, concussion, and external trauma were thought to be the cause. Continued irritation from pulling the attachments of the paratendon of the common digital extensor tendon was believed to be responsible for appearance of the clinical sings.
Etiology:-
Concussion is probably the most important etiological factor, especially in young horses.In adult horses the periosteal attachments to the bone is more mature, and periostitis is rarely evident after three years of age.
The condition often occurs in both forelimbs at about the same time.
Injuries to the periosteum from direct trauma may also produce periostitis.
Direct trauma to the metacarpal or metatarsal areas can produce periostitis in the mature horse.
Clinical Sings:-
The disease can be classified into three types:--Type 1:-
Dorsal metacarpal disease is usually observed in young Thoroughbred racehorses(8-36months of age), and occasionally in older horses that have not been trained or raced as 2-year-olds.
Radiographs taken at this time are usually negative, factures are occasionally observed as well as a minimal amount of superficial cortical osteolysis.
Type 2:-
Dorsal metacarpal disease is considered the subacute or chronic from this disease complex. It is invariably develops as a result of acute Type 1 disease that is unresponsive to therapy or has gone unrecognized.It is most frequently seen in horses 26 to 24 months of age.
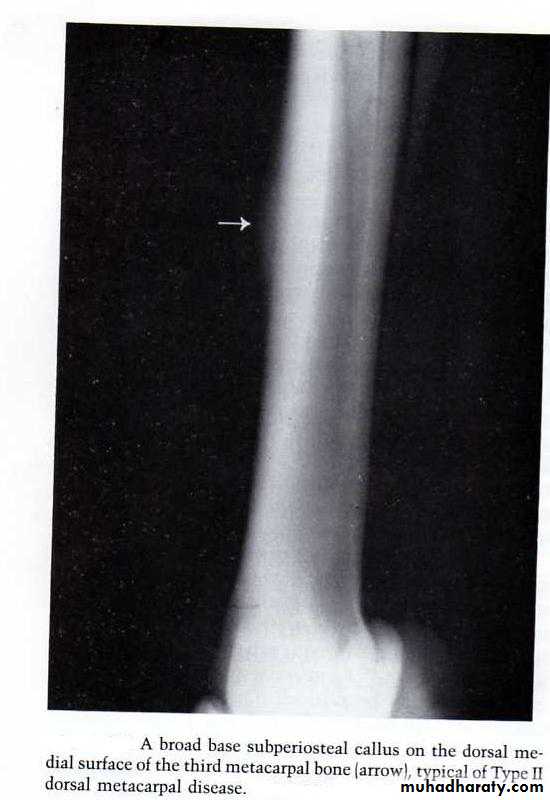
On radiographic examination a subperiosteal callus is usually observed.
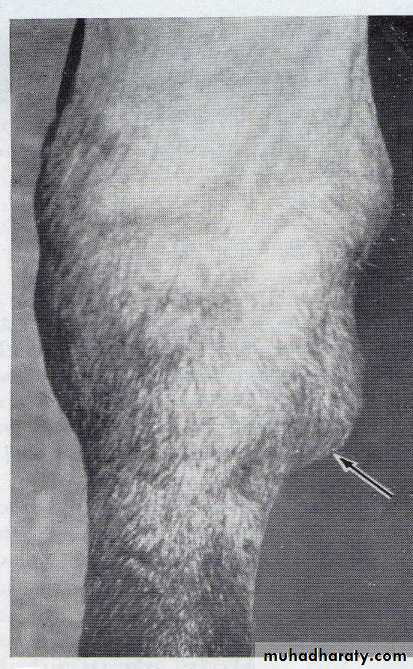
A broad base subperiosteal callus on the dorsal medial surface of the third metacarpal bone (arrow) typical type 2 dorsal metacarpal disease.
Type 3:-
Dorsal metacarpal disease results from a fracture in the dorsal or dorsolateral cortex of the third metacarpal bone.It is usually observed in older horses 3-5 years of age.
Radiographs usually point to a cortical fracture on the dorsolateral surface.
Diagnosis:-
Metacarpal periostitis or stress fracture can be made from the clinical findings and the age relationship.
A definitive diagnosis can only be made with radiographs. A series of four radiographic views should be taken.
With Type 1 disease it is rare to see anything radiographically.
With Type 2 disease subperiosteal lysis may be observed early, and later a thickening of the dorsomedial cortex with associated subperiosteal callus is seen.
With Type 3 the cortical fracture usually enters the cortex distally and progresses proximad at 35 to 45 degree angle. Most frequently the fracture appears in radiographs as a straight or slightly concave fracture line (tongue fracture). Occasionally it will proceed proximad to exit through the dorsal cortex (saucer fracture).
Treatment:-
Type 1 lesions:-Usually respond to varying periods of rest.
Daily hand walking exercise is permitted and can be increased when the metacarpus is no longer painful.Local hyperthermia may be beneficial initially along with the administration of phenylbutazone.
A sterile needle drainage of the subperiosteal hematoma that may be present was recommended. This is done 4 to5 days after the acute phase of the disease, it will lead to a marked decrease in pain after drainage of hematoma was complete.
A controlled exercise program should be employed when the horse is returned to work.
Type 2 lesions:-
Type 2 dorsal metacarpal lesions can be the most difficult to treat of the three types.Some may never resolve, whereas other require a year or more to resolve.
The same controlled exercise program recommended for Type 1 is also recommended here.
It is possible the use of pulsing electromagnetic fields may be beneficial for this type condition.
Type 3 lesions:-
Dorsal cortical fractures in young horses may resolve with the conservative approach mentioned in Type 1 lesions. Convalescent periods may extend from 4-6 months.
However older horses often do not respond to conservative treatment and surgery is required. In either case serial radiographic studies should be performed at least 30 to 45 days apart to assess the bone healing.
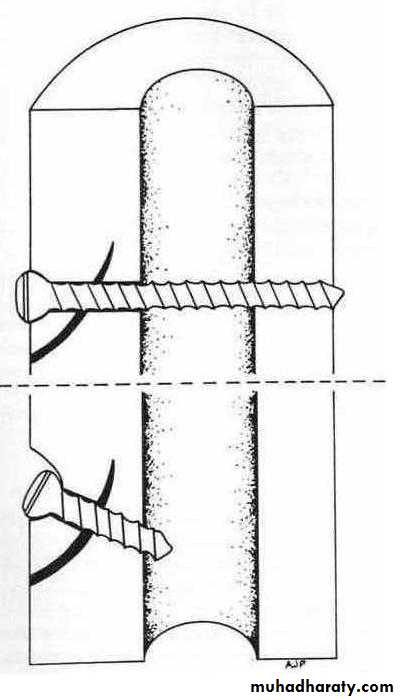
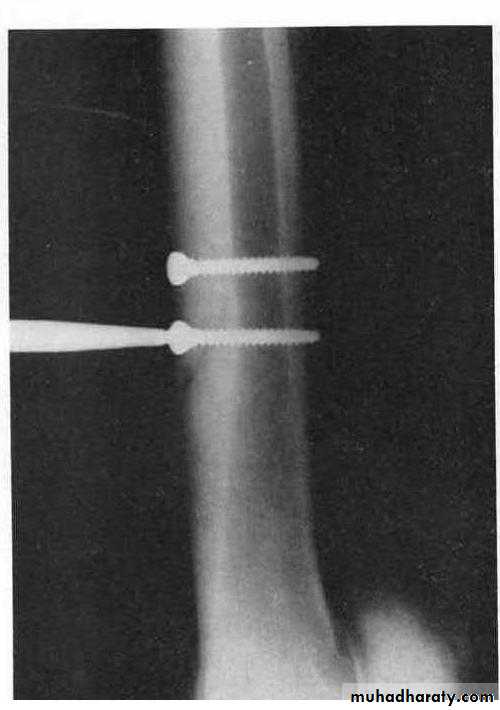
Surgical procedure by internal fixation of the fracture either with transcortical or unicortical method using bone screw. Avoids placing the screw close enough to the second metacarpal bone that it may cause irritation or deviation of it.
Postoperative management includes limiting the exercise until the surgical site is no longer painful. In most cases 6 weeks of rest is recommended.
Upper, Illustrates the transcortical method. Lower, Illustrates unicortical method.
Two screws placed transcortically are used to repair saucer fracture.Splints
Splints is a disease of young horses, most often affect the fore limb. Splints most commonly are found on the medial aspect of the limb between the second and third metacarpal bones. This is a disease associated with hard training, poor conformation, improper hoof care, or malnutrition of a young horse.The second and fourth metacarpal bones and metatarsal bones are commonly called splint bones. Each is attached intimately to the respective third metacarpal or third metatarsal bone by an interosseous ligament.
The terminology used to identify diseases of the small metacarpal and metatarsal bones is variable:-
True splint : refers to a sprain or tear of the interosseous ligament. The resultant enlargement is most frequently observed 6 to 7 cm below the carpus on the medial side at the junction of the second and third metacarpal bones.
Blind splint: refers to an inflammatory process of the interosseous ligament that it is difficult to detect on physical examination because the swelling occurs on the axial (inner) side of the splint, between the small metacarpal bone and suspensory ligament.
Knee splint: refers to the enlargement of the proximal portion of the splint bone that may lead to osteoarthritis within the carpometacarpal joint.
Etiology:-
Tearing of the interosseous ligament that binds a small metacarpal bone to the large metacarpal or metatarsal bone.External trauma.
Healing of a transverse or longitudinal fracture.
Conformation abnormalities that increase the stress on the small metacarpal bones also increase the incidence of this disease.
Imbalanced nutrition or overnutrition in young horses helps in the development of splints. Imbalances in calcium and phosphorus as well as deficiencies in these minerals have been associated with an increased incidence of splints.
Clinical Sings:-
Lameness is the most common in two-year-old horses undergoing heavy training, but cases occasionally occur among three- or four-year-olds.Splints most often are found on the medial aspect of the limb, because the second metacarpal bone normally bear more weight than the fourth metacarpal bone.
Heat, pain, and swelling over the affected region may occur along the length of the splint bone.
If new bone growth occurs near the carpal joint, it may cause carpal arthritis(knee splints).
Splint lameness becomes more marked with exercise on hard ground. In mild cases no lameness may be evident in the walk, but lameness is exhibited during the trot.
Diagnosis:-
If the affected limb is examined carefully, the obvious sings will lead to a diagnosis.
Heat, pain, and swelling over the regions mentioned, plus lameness, are enough for diagnosis.Fracture of the splint bone is commonly confused with splints. In a fractured splint bone, the edema of the limb usually is distributed over a larger area and the animal remains chronically lame for a longer period.
An important part of diagnosis is to determine whether the carpal joint is involved or not and whether the new bone growth has extended palmarly so that the suspensory ligament is involved.
New bone growth resulting from trauma may occur on the third metacarpal or third metatarsal bones and may be mistaken for splints.
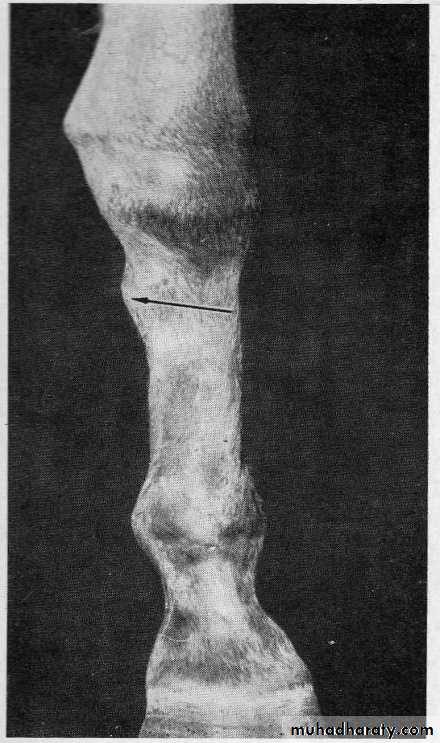
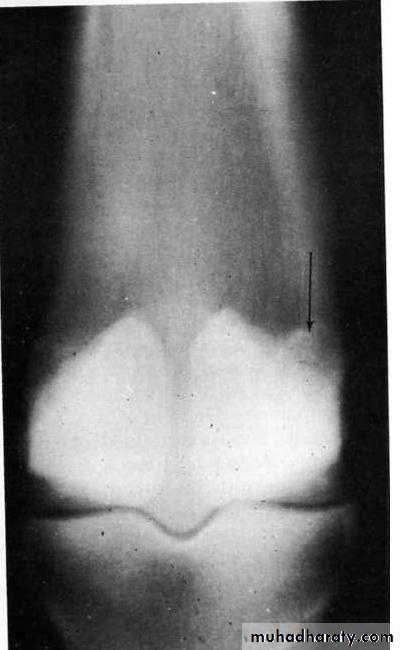
Medial Splint (arrow)
An example of a periostitis of the splint bone (arrow)Treatment:-
In the acute phase, the administration of phenylbutazone coupled with the application of hypothermia and the application of pressure support wraps appears to be most beneficial to decrease the heat, pain, and swelling.
Hypothermia can be attained with ice packs, which should be applied for 30 to 45 minutes 2 times a day for at least 5 to 7 days.
Hand massage was recommended for 10 minutes after each treatment after which a support bandage is applied.
Affected horses should be confined to a stall for at least 30 to 45 days and hand walking exercise for 10 to20 minutes 2 times a day should be begun after the acute inflammation subsides.
Counterirritation in the form of pin firing, local injection o f sclerosing agents, topical application of blisters, and radiation are frequently used in subacute and chronic cases.
In some cases it is necessary to surgically remove a bony Exostosis that interferes with the action of the suspensory ligament or the carpal joint or one is so large that is being hit repeatedly by the opposite foot.
The Tarsus
Bone Spavin (Osteoarthritis or Degenerative Joint Disease of the Distal Tarsal Joints)Bone spavin (true spavin or jack spavin) is an osteoarthritis and periostitis that involves the distal intertarsal, tarsometatarsal, and occasionally the proximal intertarsal joints.
Jack spavin is a bone spavin of large proportions. Degenerative joint disease of the distal joints is considered to be the most common cause of clinical lameness associated with the tarsus.
Etiology:-
Bone spavin is observed most frequently in mature horses that are ridden hard at a gallop and canter, and also in horses that jump.Repeated compression and rotation of the tarsal bones and excessive tension of the major dorsal ligaments.
Bone spavin is commonly associated with poor conformation..
Mineral imbalances, as well as endocrine imbalances.
Several reports have correlated hypothyroidism in foals with collapse of the central and third tarsal bones.
Clinical Sings:-
Horses with bone spavin usually have a lameness history of gradual onset.
The horse may feel stiff or jerky when circled to the affected side.Bone spavin lameness tends to be worse when the horse is first used.
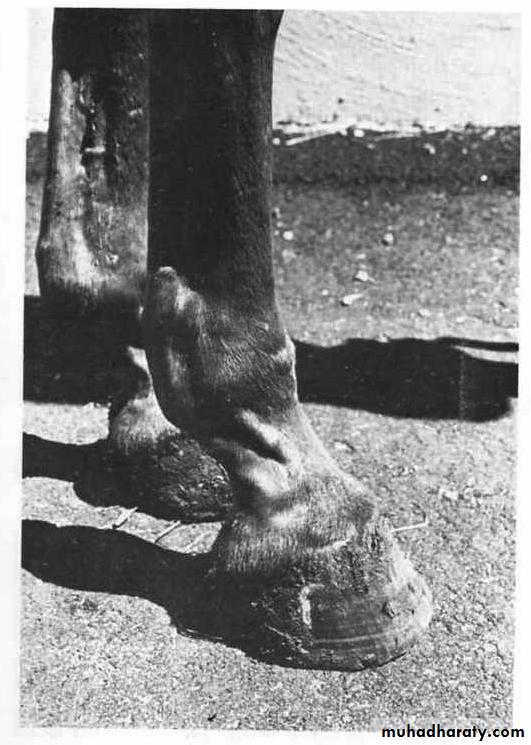
Bone spavin causes enlargement of variable size on the inner aspect of the hock.
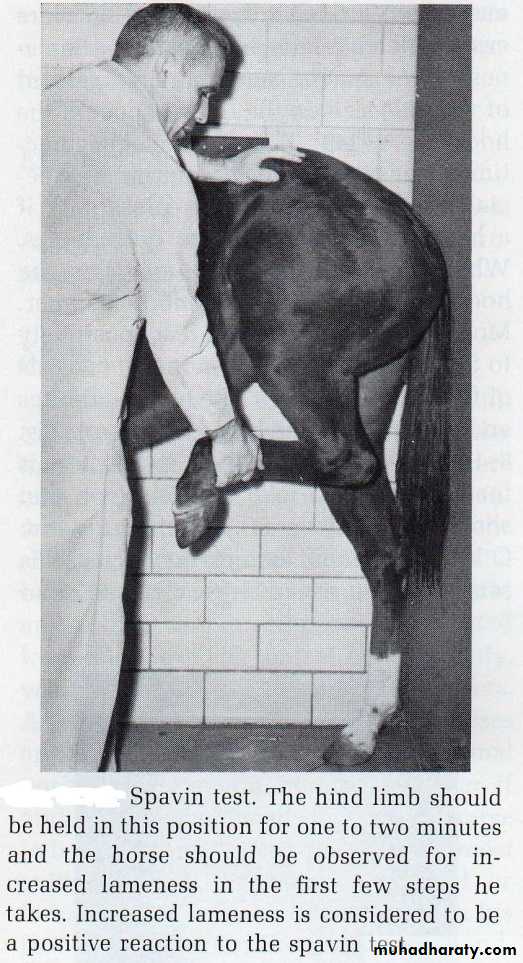
Most cases of bone spavin react positively to the spavin (hock flexion) test. The spavin test consists of flexing the hock for 1 to 2 minutes and then putting the horse into a trot. A positive reaction to the test is for the horse to take several steps that show more lameness than before the test..
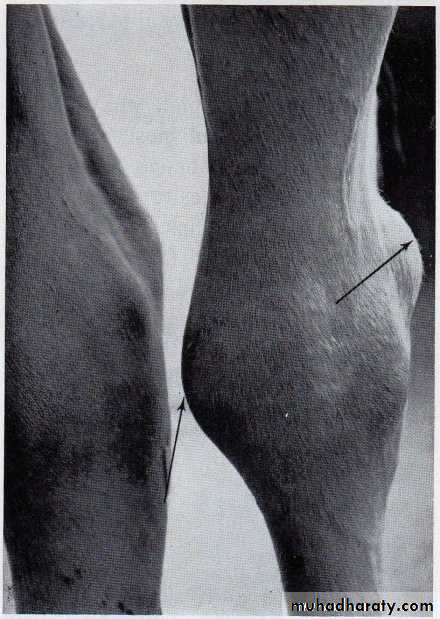
Bone spavin. Black pointer indicates ankylosis of the distal intertarsal joint. The white arrow indicates new bone growth on the medial aspects of the third and central tarsal bones. These are typical changes in bone spavin.
Site of bone spavin on the right hind limb. The arrow indicates the prominence of new bone growth.
Diagnosis:-
The reduced arc of the foot flight, reduced flexion of the hock, and the spavin test are used in diagnosis.The hocks must be examined carefully both from in front of the horse, comparing the two hocks by observing between the front limbs, and from behind by observing the hocks straight-on and from oblique views.
A routine radiographic examination of the tarsus should include several views in the normal of the hock and in flexion position.
Treatment:-
In spite of numerous types of therapy for treatment of bone spavin, many affected horse remain lame and resistant to all conventional methods of therapy. Treatments used include;Cunean tenectomy.
Firing into the distal tarsal bones, with or without previous Cunean tenectomy.
Cunean Tenectomy:-
It is a removal of a portion of the Cunean tendon from the tibialis cranailis muscle. The surgery can be performed with the horse in the standing or recumbent position as follow:The area over the tendon should be clipped, shaved, and prepared with skin antiseptics.
A local anesthetic should then be injected over the tendon and an incision 1.5 inch long made over the center of the longitudinal axis of the Cunean tendon where it crosses the medial aspect of the hock.
The incision can be made vertically if desired. The tendon should be isolated and a 1 to 1.5 inch section removed .
The skin then should be sutured with noncapillary, nonabsorbable suture, which should be removed in 10 to 14 days.
The horse should be rested at least 2 months.
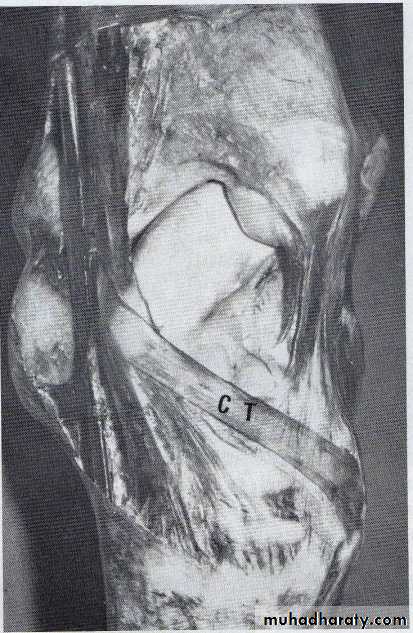
Dorsomedial view of the Cunean tendon (CT). Approximately 1 inch of this tendon is removed to treat bone spavin.
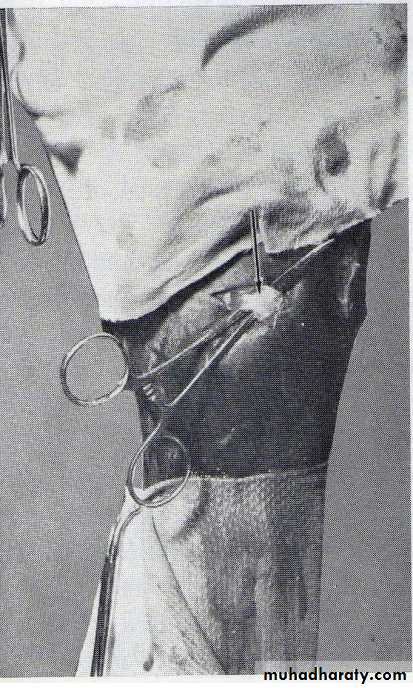
The white tape indicates the course of the Cunean tendon where it crosses the medial aspect of the tarsal joint. This is the site of incision for Cunean tenectomy
The Cunean tendon is seen over the hemostat, which has been placed underneath it (black arrow). 1 to1.5 inches of this tendon are removed.
Bog Spavin (Idiopathic Synovitis)
Bog spavin is a descriptive term for chronic distention of the tarsocrural (tibiotarsal) joint capsule of the hock, causing swelling of the dorsomedial aspect of the hock joint. Although there are many causes, the distention is due to an acute or chronic low grade Synovitis.Etiology:-
Faulty conformation:- A horse that is too straight in the hock joint is predisposed to bog spavin. If a horse with straight limbs is not affected by bogs as a young horse, it may develop them after training begins.
Trauma:- Injury to the hock joint as a result of quick stops, quick turning or other traumas, will cause bog spavin due to injury of the joint capsule or tarsal ligaments.
Mineral or Vitamin Imbalance:- Deficiencies of calcium, phosphorus, vitamin A or vitamin D, alone or in any combination, apparently can produce bog spavin. Chronic zinc intoxication has also been a cause of tarsal joint effusion.
Clinical Sings:-
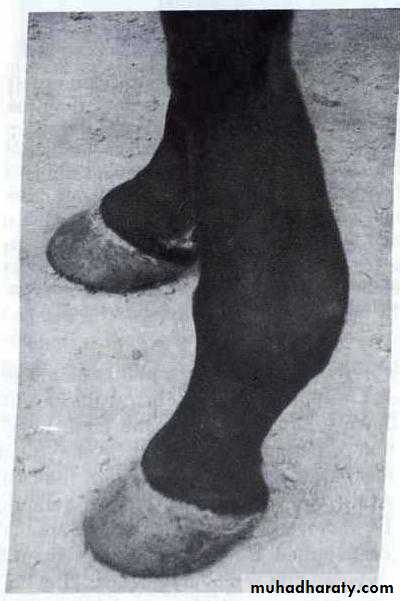
Bog spavin has three characteristic fluctuating swellings, the largest of which is located at the dorsomedial aspect of the hock joint.Two smaller swellings occasionally occur on either side of the surface of the hock joint. .
Lameness, which usually accompanies only traumatic bog spavin, results in heat, pain, and swelling over the hock joint.
A hock flexion test may or may not increase lameness.
Diagnosis:-
Sings of bog spavin are diagnostic, the only variation is in the size of the three swellings.In most cases the dorsomedial swelling is the largest, but in some cases the two planter swellings are more prominent.
The most important factor in diagnosis is to determine the etiology, whether the condition is due to conformation, trauma, osteochondrosis, or nutritional deficiency.
Bog spavin. Arrows illustrate the swellings that occur in typical bog spavin. The dorsomedial swelling is the largest. The swellings at the planter aspect of the hock on the medial and lateral sides will vary in size.
Treatment:-
When trauma is the cause of bog spavin, injection of a corticoid into the joint capsule at weekly intervals for 2 to 3 injections is recommended if there are no radiographic changes. Corticoids decrease inflammation of the synovial lining and help prevent formation of excess fluid.
The horse is twitched and the skin shaved and prepared with antiseptics. A 2-inch 20 gauge needle should be inserted into the capsule and after all fluid is drained that will come out easily, the corticoid is injected.
Counterpressure by bandaging, following injection of the capsule, is also recommended. Best results with counterpressure are obtained if elastic bandages are used.
Other injectable drugs that may be beneficial include Orgotein, Ontosein, Hyaluronic acid, and Artypyrone.
Treatment of bog spavin caused by nutritional deficiencies is usually made by proper correction in the diet.
Sesamoiditis
Sesamoiditis, or inflammation of the proximal sesamoid bones, is usually accompanied by a periostitis and osteitis of these bones. The suspensory ligament and the distal sesamoidean ligaments may also be affected and show calcified areas. Demineralization of the sesamoid bones may result from inflammation and impaired blood supply.Etiology:-
Any unusual strain to the fetlock area may produce Sesamoiditis.Most common observed in race horses, hunters, and jumpers between 2 and 5 years of age.
It is caused by injury to the attachment of the suspensory ligament to the sesamoid bones.
Injury to the distal sesamoidean ligaments may also occur at their attachment to the basilar portion of the sesamoid bones.
Clinical Sings:-
Symptoms are similar to those caused by fracture of the sesamoid bones, pain and swelling of the fetlock joint, especially at the volar aspect.
Pressure over the sesamoid bones will cause the horse to flinch.
The horse will not allow the fetlock to descend to normal level.
After the disease becomes chronic, radiographs will show periosteal new bone growth on the convex surface of the sesamoid bones.
In addition calcification of the suspensory ligament above the sesamoid bones, or in the distal sesamoidean ligaments below may occur.
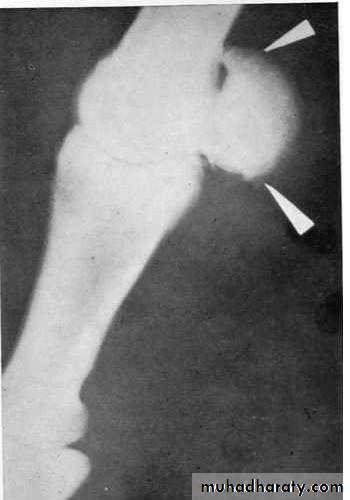
Arrows indicate new bone growth on the sesamoid bone in Sesamoiditis. The bone growth resulted from irritation caused by injury to the suspensory ligament, at the top, and to the distal sesamoidean ligaments, below.
Sesamoiditis with calcification extending into the suspensory ligament (arrow).
Diagnosis:-Diagnosis can be made by careful examination of the limb.
Radiographs may have to be taken approximately 3 weeks after onset of the condition to determine if bony changes will occur on the sesamoid bones.Also, careful radiographic interpretations of the mottled trabecular pattern seen in the proximal sesamoid bone are necessary to differentiate a fracture.
Treatment:-
Efforts should be made to reduce the inflammation. Alternating cold and hot packs, as well as antiphlogistic packs, should be used.
Immobilization of the limb, from the hoof wall to just below the carpus, with a cast, this cast should be left in place for 2 to 3 weeks and then removed and replaced, if necessary.
X-ray and gamma-ray radiation are considered to be valuable therapy in this condition, as well as in the treatment of calcification in the suspensory ligament.
Prolonged rest is essential to prevent possible fracture.
Synovitis:- Inflammation of any synovial lining-joint, tendon sheath, or bursa.
Tendinitis:- Tendinitis implies inflammation of the tendon only. This occurs where the tendons have no sheath.Tenosynovitis (Tenovaginitis):- Tenosynovitis may be defined as inflammation of the synovium surrounding the tendons. This inflammation is usually due to strain from severe overuse or may be due to direct blow or infection.
Sprain:- A sprain may be defined as the stretching or tearing of a supporting ligament of a joint by forced movement beyond its normal range. In its simplest form there is minimal disruption of fibers, swelling, pain, and dysfunction. Severe sprains may cause total rupture of ligaments, marked swelling, and hemorrhage and joint instability.
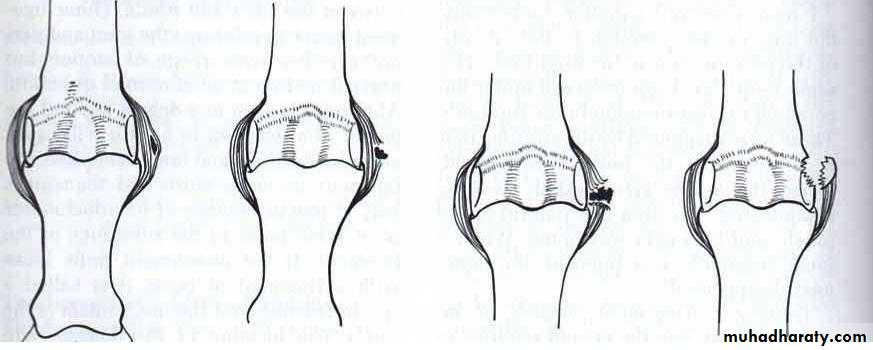
Sprains are classified as follows:-
Mild Sprain:- This is a sprain in which a few fibers of the ligament have been torn with some hemorrhage into the ligament, but integrity is not lost. Rest and a support bandage are the appropriate treatment of this problem.
Moderate Sprain:- A moderate sprain is one in which some portion of the ligament is torn and some degree of functional loss is sustained. The amount of damage may vary from a tear of a relatively small portion of the ligament to almost complete avulsion. Union can therefore proceed in an orderly manner as a result of healing with fibrosis. The use of a cast is indicated in the appropriate joint to support this healing.
Severe Sprain:- In sever sprain there is complete loss of function of the ligament. The stress tears it completely away from one of its attachments or pulls it apart along its length. The loss of integrity of the ligament may result in luxation of the joint. Some form of surgical intervention is generally indicated with a severe sprain, but this depends on the ligament and the joint.
Sprain Fracture:- In this case, the portion of bone to which the ligament is attached becomes avulsed.
Strain:- Strain has been defined as damage to a tendon or muscle caused by overuse or stress. Strain of a tendon can range from minor inflammation to disruption of the tendon or avulsion of the tendon from its bony attachment.
B
Moderate sprain-hemorrhage in the fibers of the ligaments and some of the fibers are torn
A
Mild sprain- hemorrhage occurs in the fibers of the ligament
DSprain fracture- the function of the ligament is lost and portion of bone to which the ligament was attached is fractured
C
Severe sprain- complete tearing of the ligament and loss of function
Tendon Structure
A tendon is a dense band of fibrous connective tissue that acts as intermediary in the attachment of muscle to bone. Tendons are composed of dense, regular connective tissue and have a specific arrangement that reflects the mechanical requirements of this tissue. The chief constituents of tendons are thick, closely packed parallel bundles of longitudinally oriented collagen. Fibroblasts(tenoblasts) are arranged in long parallel rows in the spaces between the collagenous bundles.Tendinitis, Tendosynovitis (Bowed Tendon, Tendovaginitis)
Tendinitis is inflammation of tendon and tendon- muscle attachments. In the horse it refers specifically to inflammation of the flexor tendons due to excessive strain. The term tendinitis, if used correctly, applies to strain –induced inflammation involving tendon that is surrounded by paratendon and not tendon sheath. If the region of involved tendon is associated with a tendon sheath the term Tendosynovitis is used.
Tendinitis and tendosynovitis are most common in the forelimb in racing Thoroughbreds and Quarter Horses and typically involve the superficial digital flexor tendon.
Tendinitis or tendosynovitis has also been classified according to position:-
High- just distal to the carpus or tarsus.
Middle- in the middle third of the metacarpus or metatarsus.
Low- distal third of the metacarpus or metatarsus.
Etiology
Tendinitis or tendosynovitis usually results from a severe strain to the flexor tendons which associated with excessive loading and overstretching of the tendon.
The higher incidence of the disease in race horses and hunters compared with other horses confirms that the injuries are directly related to excess physical stress.
The most common site of injury is in the central metacarpal region where the superficial digital flexor tendon has its smallest cross-sectional area.
Abnormal angulation of the fetlock associated with muscle weakness or conformation increases the stresses on the tendon.
Uneven and slippery ground or sudden turns may load one side of a tendon, in addition to other fatigue factors.
Pathophysiology of Tendinitis and Tendon Injury:-
Tendon injury and degeneration occurs in all degrees of severity ranging from slight subclinical injuries that may be detected only thermography up to those associated with complete tendon rupture.Loads above the safe limit may produce minor fiber displacement and rupture. This separation results in capillary hemorrhage within the tendon.
Typically, acute tendon injury is accompanied by hemorrhage, edema, fibrin accumulation, and local swelling.
Transudation and hemorrhage into the tendon separates an d weakens remaining normal fibers.
Hydrolytic enzymes are also released and can cause further damage to collagenous fibrils and interfibrillar matrix.
Disruption of blood supply in the damaged region also occurs. The amount of necrosis occurring in the region can be related to the degree of vascular compromise.
Diagnosis:-
In the acute phase, there is diffuse swelling over the region with heat and pain on palpation.
Severe lameness is present, and the limb is held in a flexed position.
Major disruption of tendon fibers or stretching of the tendon will be represented by dropping of the fetlock.
The chronic stage is manifested by fibrosis and hard swelling on the palmer or planter aspect.
The horse may be sound at the walk and trot but becomes lame with hard work.
Anular ligament constriction may be present in association with a chronic bow at the level of the fetlock.
Thermography may be useful to diagnose early inflammation in the tendons when other clinical sings are not obvious.
Tendinography using of air tendograms will provides additional information about bowed tendon. Air is initially injected into the digital flexor tendon sheath and then subcutaneously between the flexor tendons to outline them.
More recently, diagnostic ultrasound has been used to define of damage in a tendon as well as the degree of adhesion formation.
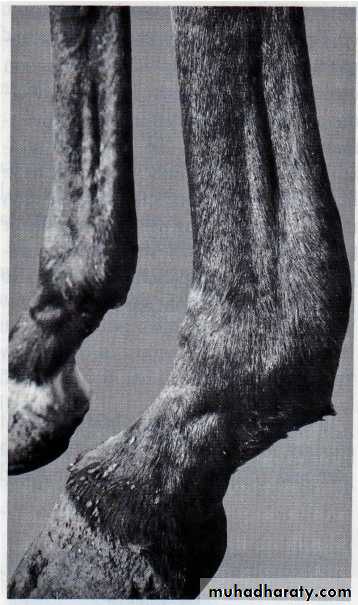
Chronic low tendinitis(bowed tendon) of the left forelimb. Notice extent of swelling from the superficial flexor encompassing the deep flexor. This indicates tearing and adhesions of the common sheath. The left fetlock dropped lower than the right when the horse walked.
Tendosynovitis (bowed tendon). Note the extensive swelling above the sesamoid bones in the area of flexors. This involvement includes all of the classification of high, middle and low tendinitis.
Constriction of the palmer anular ligament. Note distention of digital flexor tendon sheath above the anular ligament.
Treatment:-
In the acute case the aim of the therapy is minimize inflammation, so initial therapy includes the application of cold hydrotherapy or ice-packs to minimize hemorrhage and edema.Immobilization using either a plaster cast or soft casting.
The use of parenteral corticosteroids as well as nonsteroidal anti-inflammatory drugs has been advocated.
Peritendinous injection corticosteroids may be used to minimize Peritendinous adhesions, but intratendinous injection is contraindicated.
Topical dimethylsulfoxide may be of value in reducing edema.
Corrected shoeing with raised heels has been recommended.
An important aspect of treating tendinitis is rest, it may be better that complete rest is given for the first two weeks.
For chronic tendinitis, the most common forms of treatment have included some form of Counterirritation, including firing, surface or injected irritants, irradiation, ultrasound, and surgical incision of the tendon.
Other treatments of chronic tendinitis, include tendon transplants, implantation of artificial tendon sheaths, and carbon fiber implants.