1
2
3
Lec:9
Community medicine
Maternal and child health care - 1
At the end of the lecture you will be able to
1. Describe the demographic profile of Iraqi population by the use of population pyramid.
2. Describe the health profile in Iraq in relation to mothers and their children.
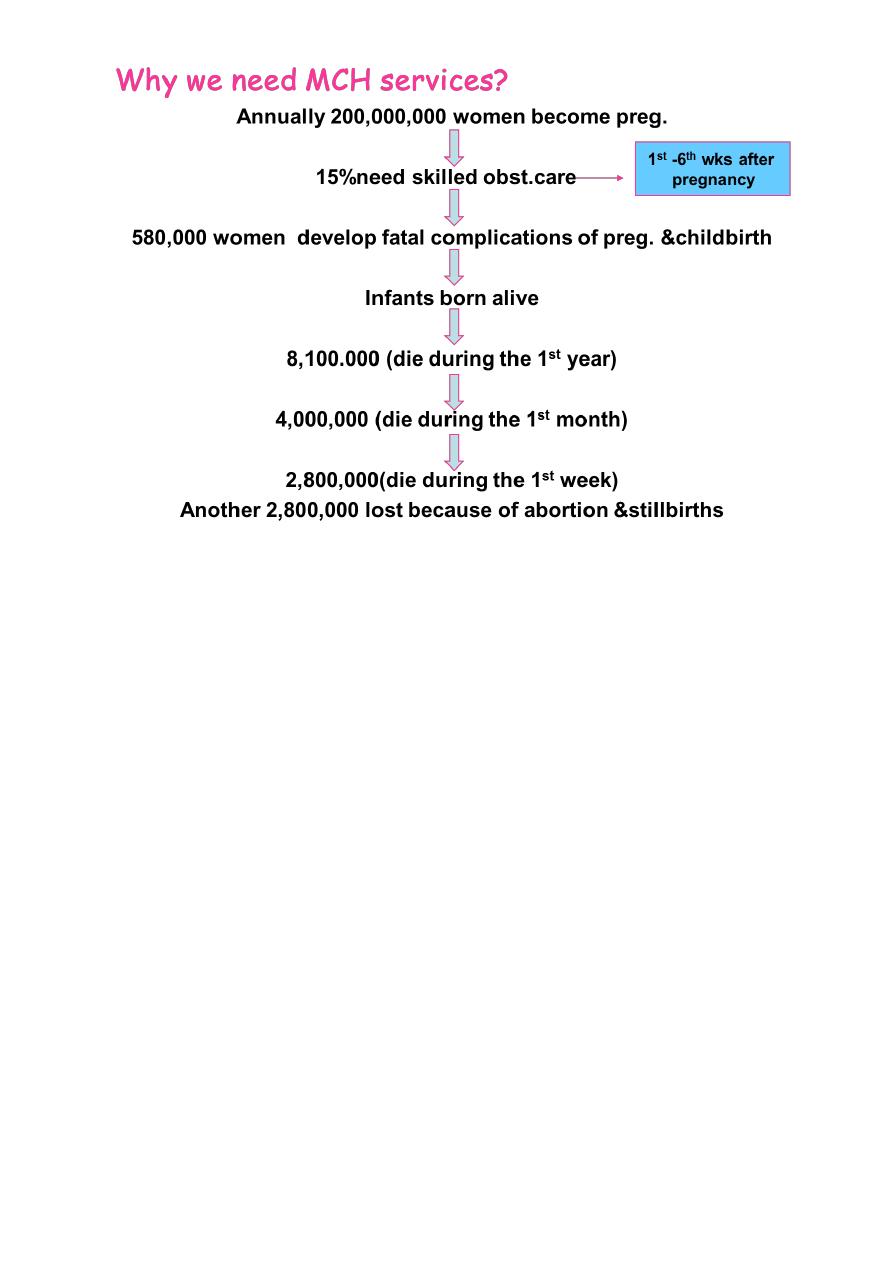
3. Identify the need for MCH services .
4. Define maternal death.
5. Enumerate causes of maternal death.
6. Define maternal mortality rate, ratio and lifetime risk of maternal death .
7. Define PHC.
8. Enumerate components of PHC.
9. State the objectives and justification of providing MCH services.
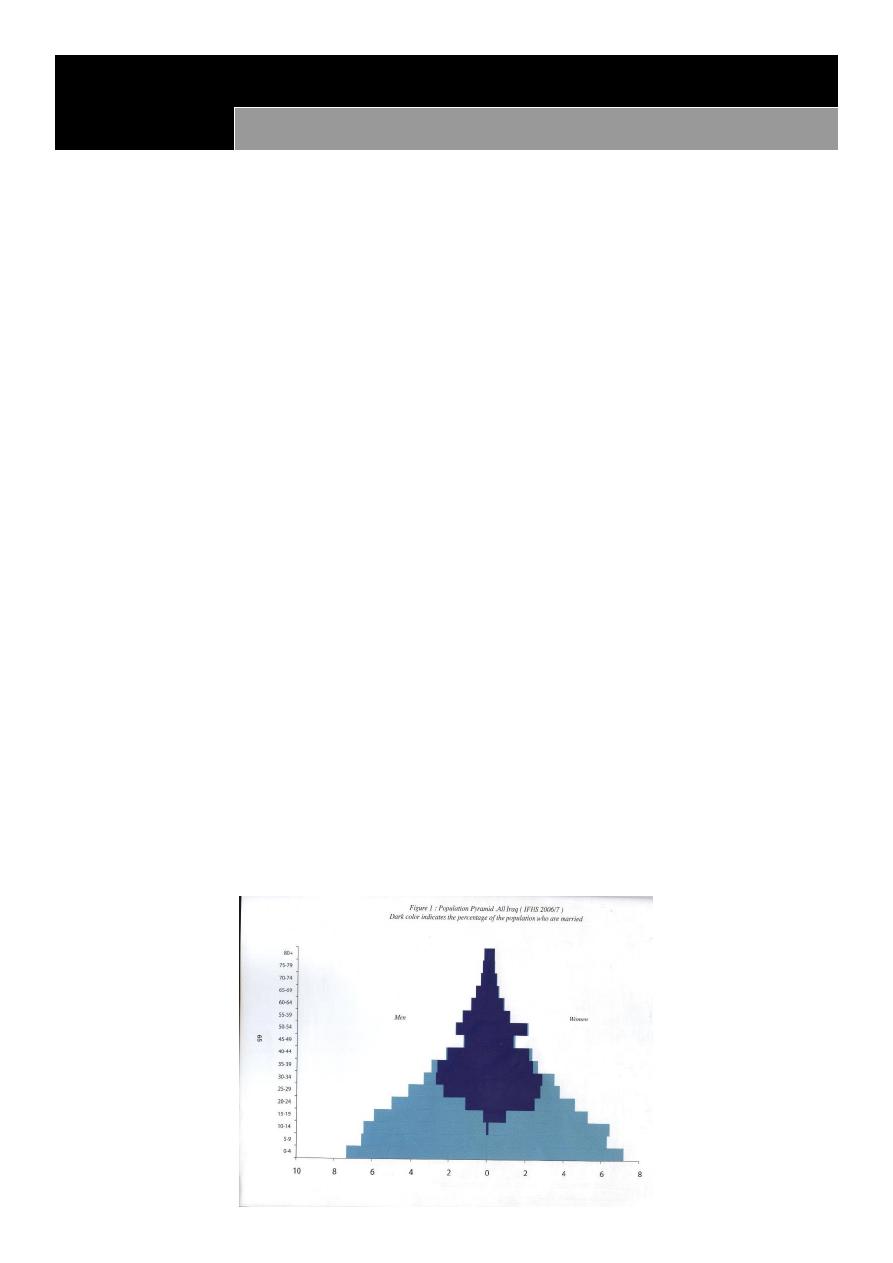
Population Profile
The population of Iraq during 2013 was estimated to be 35,000,000 with an
urban:rural ratio of 67:33.
Ninevah governorate: 3,335,200
The age distribution of the population in Iraq is typical of high fertility.
The population is young as more than half are <20 years and about 5% are 60+.
The proportion of infants to population 3.9% and that of the <5s is 16.9%.
The proportion of < 15s is 44%.
The proportion of women in childbearing age is 25%.
consequently, 69% of Iraqi population is women in child bearing age and their children.
The sex ratio is balanced at the younger age group.
There is a sever male deficit in (40-54).
Specific marital status shows that women married younger than men.

4
Health Profile
Maternal mortality ratio was 294 per 100,000 live births, in 2002.
Maternal mortality ratio was 84 per 100,000 live births, in 2006.
It was 24 per 100, 000 live births, in 2009.
Became 26 per 100, 000 live births in 2011
And it dropped down to 20 per 100,000 live births in 2012 (Nineveh figure)
The health Profile for Iraq
Abortion rate is 9.7 per 100 pregnancy (2006).
Still birth is 0.9 per 100 pregnancy (2006).
The estimated lifetime risk of maternal death for women in Iraq is 1 in 57*. *(Local
survey)
Health Profile
Almost 17% of women in child bearing age in Mosul have collective high fertility behaviors
66.44% of deliveries took place at hospitals (Ninevah governorate) in 2012
18% are attended by TBA and
39% by licensed midwives and nurse.
Only 43% of Mosuli women in child bearing age use contraceptive methods &
only 29% of them use the modern of contraception.
Health Profile for Iraq
Child mortality rate (U5)
It was 58.9 per 1000 live birth(2003-2005), it dropped to 29.5 per 1000 live births in 2009 and
22 per 1000 live births in 2010 and to 21.4 in 2012
Health Profile
Infant mortality rate
It was 42 per 1000 live birth(2003-2005) and it dropped to 24 per 1000
live births in 2009, to be 19 in 2010.
Neonatal mortality rate
It was 23 per 1000 live births in 2006
Incidence of low birth weight is 6.5% in 2011 and 2012.
5
What is maternal death?
It is the death of a woman while pregnant or within 42 days of termination of pregnancy,
regardless of site or duration of pregnancy,
from any cause related to or aggravated by pregnancy or its management, but not from
accidental or incidental causes.
Direct obstetric deaths
result from obstetric complications occurs during pregnancy,
Labor,
or at the post partum period.
They are usually due to one of five major causes:
Hemorrhages (usually post partum)
Sepsis
Eclampsia
Obstructed labour
Complications of unsafe abortion
as well as
6
intervention,
omissions,
incorrect treatment,
or events resulting from any of these .
Indirect obstetric deaths
Result from previously exiting diseases or from diseases arising during pregnancy (but
without direct obstetric causes), which were aggravated by the physiological effects of
pregnancy.
Pregnancy related death
The death of a women while pregnant or within 42 days of termination of pregnancy,
irrespective of the cause of death. ICD10
Lecture question: Define pregnancy related death as it was stated in the ICD-10.
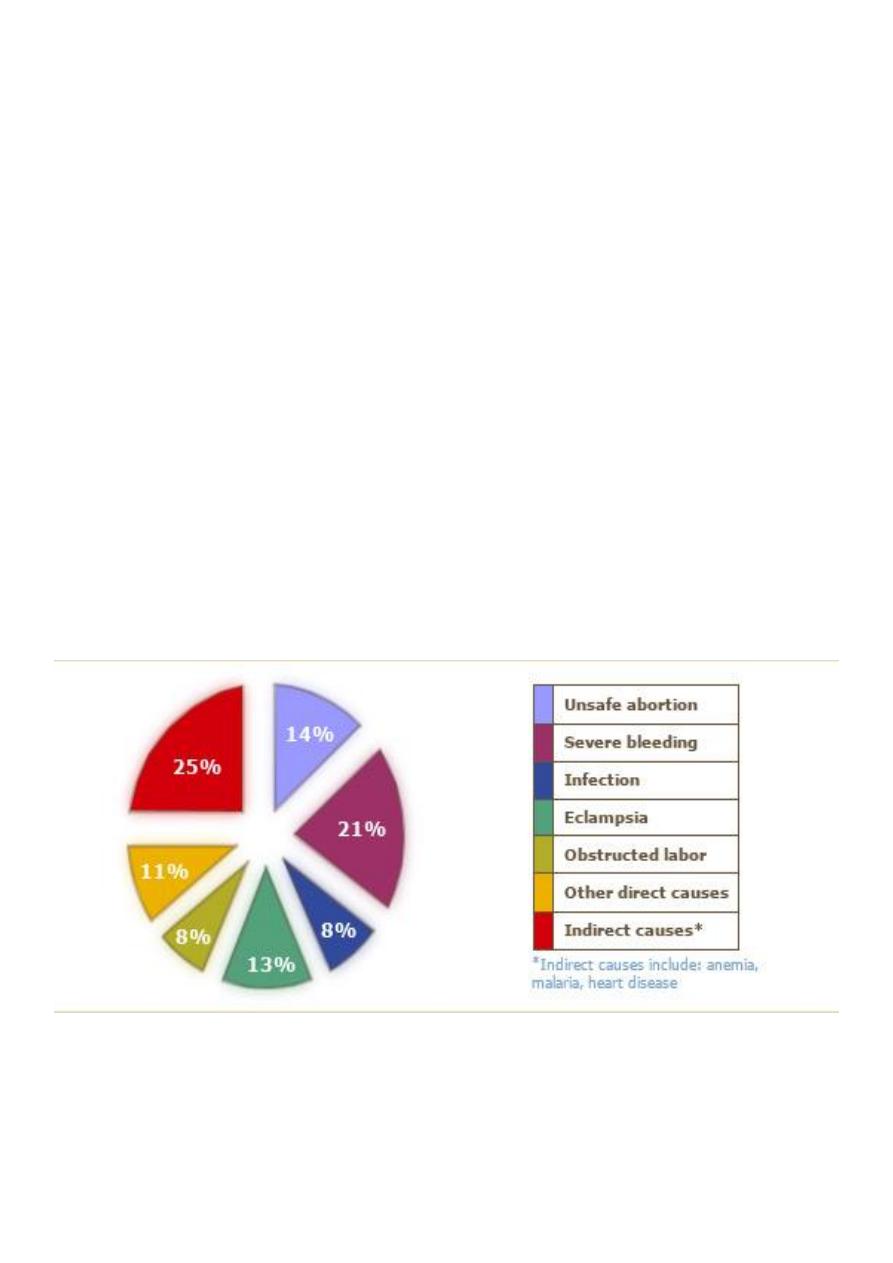
More than 80 percent of maternal deaths worldwide are due to five direct causes:
Maternal Mortality Ratio
Represents the risk associated with each pregnancy ,i.e the obstetrical risk.
7
It is the number of maternal deaths during a given year per 100,000 live births during the
same period .Although the measure has traditionally been referred to as a rate it is actually
a ratio.
Maternal Mortality Rate
Measures both the obstetric risk &the frequency with which women exposed to this risk .
It is the number of maternal deaths in a given period per 100 000 women of reproductive
age (usually 15-49years).
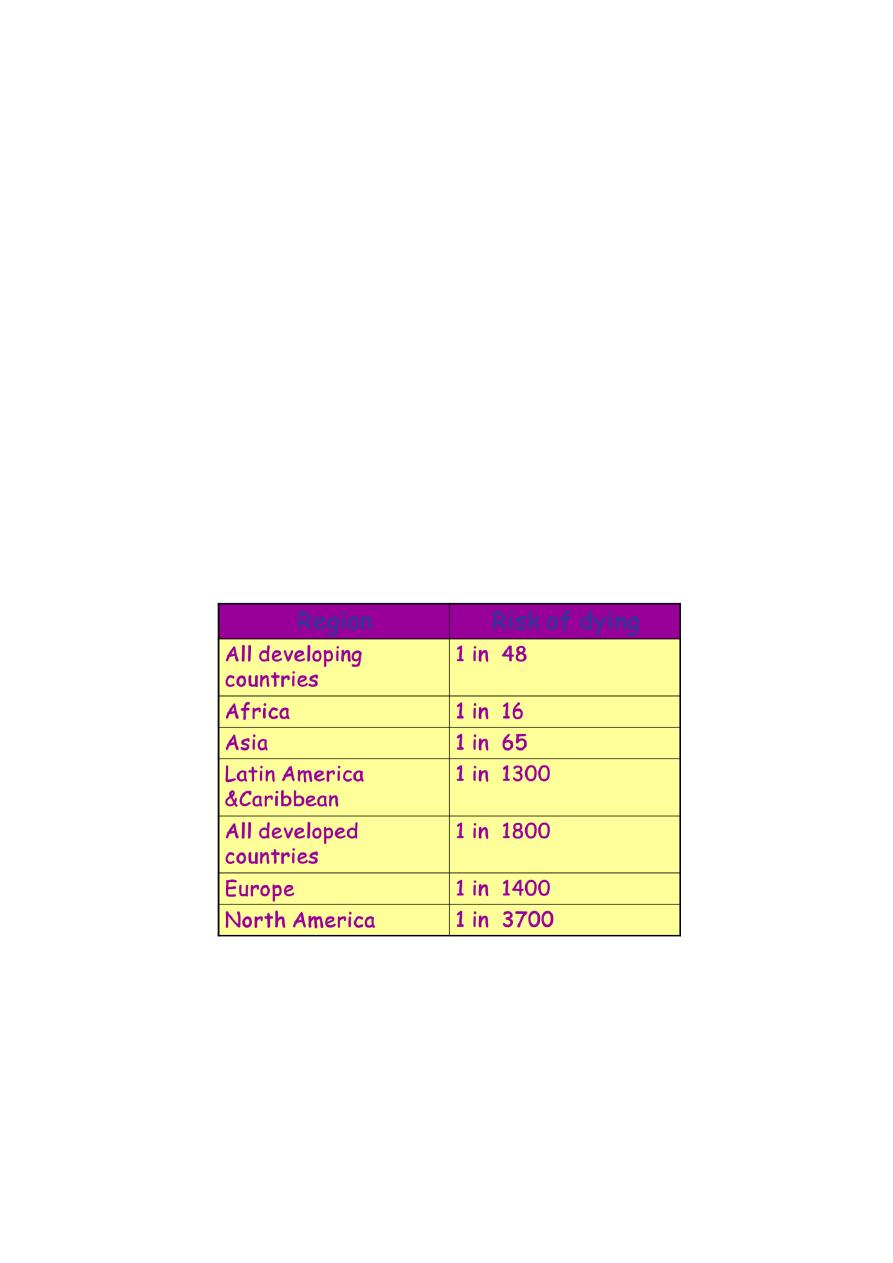
Life Time Risk of Maternal Death
Takes into account both the probability of becoming pregnant & the probability of dying as
the result of the pregnancy cumulated across woman’s reproductive years.
Maternal mortality rate х 35
Women’s risk of dying from pregnancy & childbirth
Primary Health Care
Is essential health care based on practical ,scientifically sound &socially acceptable methods
&technology ,made universally accessible to individuals & families in the community through
their full participation &at a cost the community &country can afford to maintain at every
stage of their development in the spirit to self-reliance &self determination.

8
Main elements of PHC program
1. Health Education
2. Proper Nutrition
3. Immunization
4. Maternal & Child Health Care (MHC) &Family Planning (FP)
5. Provision of Safe Water Supply & Sanitation
6. Control of Endemic Diseases
7. Treatment of Common Diseases
8. Provision of Essential Drugs
Promotion of Mental Health
School Health Services
Justification to provide MCH services
1. Mothers & children form majority of the population in developing countries
2. Deaths of mothers & children is major determinant of mortality in developing
countries
3. Many of health problems encountered by mothers & children are preventable .
4. Stress of pregnancy, lactation, growth & development
5. Mother & children represent the least powerful sector of the community .
Objectives of MCH service
Every pregnant woman maintains good health, is prepared both physically & mentally to
look after her child, goes through normal & safe delivery & bears healthy child.
Every child grows up in healthy surrounding receives proper nutrition & adequate
protection of diseases.
Communicable diseases are controlled by taking adequate preventive measures & by
health education.
All pregnancies are wanted & planned by couples who are in good physical, mental &
socio–economic circumstances for rearing children.
Sickness is detected & treated before it becomes serious & chronic.
Conclusion
MCH services is an important components of primary health care.
It is essential since almost two thirds of the Iraqi population is formed from children and their
mothers.

9
Lec:10
Community medicine
Maternal and child health care - 2
Essential Elements (phases) of MCH Services in PHC Center
Specific Objectives : At the end of the lecture you will be able to
1. Enumerate elements of MCH services
2. Define components of pre-conception care.
3. Define antenatal care.
4. State objectives of antenatal care
5. Describe the standard antenatal care given in the first and subsequent visits in terms
of quantity and quality.
6. Use the antenatal card present in primary health care centers.
Elements of MCH
Care before conception (pre-marital care )
Ante-natal (pre-natal) care
Delivery (natal) care
Post-natal care
Care of new born
Child health care
1-4 maternal care
5-6 child health care (young child clinic)
Pre-marital care
1- Complete family, history of consanguinity & medical history : thalasemia, sickle cell
anemia, hemophilia, mental retardation, congenital anomalieas, TB, STDs…..etc.
2- Full clinical examination including chest X-ray
3- Laboratory investigation
Serology for syphilis +HIV
Rh + ABO group
MCV, MCH, PCV
HBs antigen
Genetic assessment for thalasemia
One dose of tetanus toxoid.
Health education, genetic counseling &STDs education.

11
Antennal care (ANC)
Defines as complete health supervision & routine care of pregnant women to :
Maintain, protect & promote health & well being of mother, fetus & newborn infant . It
includes every aspect from screening to intensive life support .
Aims & Objectives
1- To supervise health of the mother & provide advice & treatment for disorders
associated with pregnancy.
2- To ensure good health for the baby & good start for life.
3- To provide opportunities for health education with respect to child’s health & wellbeing.
Components of ANC
1- Monitoring of health through antenatal examination.
2- Risk screening & assessment.
3- Preventive measures.
4- Health education.
Lecture question: Enumerate components of MCH services
The follow –up should be
Adequate which includes quantity & quality
1- Quantity
Time of onset…….it has to start during the 1st trimester.
No. of visits………should be at least (7) well distributed throughout pregnancy.
2- Quality
The standard care & all information should be recorded in the maternity record:
- Confirmation of pregnancy
- Family, medical, past obstetrical ,present pregnancy history
- Physical examination
- Fetal heart sound determination after the 1st trimester
- Ultrasound
- Recording all the information
Standards of ANC
At first visit most important
A- General information
11
1-Preparation of pregnancy file which contains name, age, address, occupation…..etc
2-Start by confirming pregnancy
B- History 6 items
1-General medical history
2-Family history
3-Past-obstetrical history
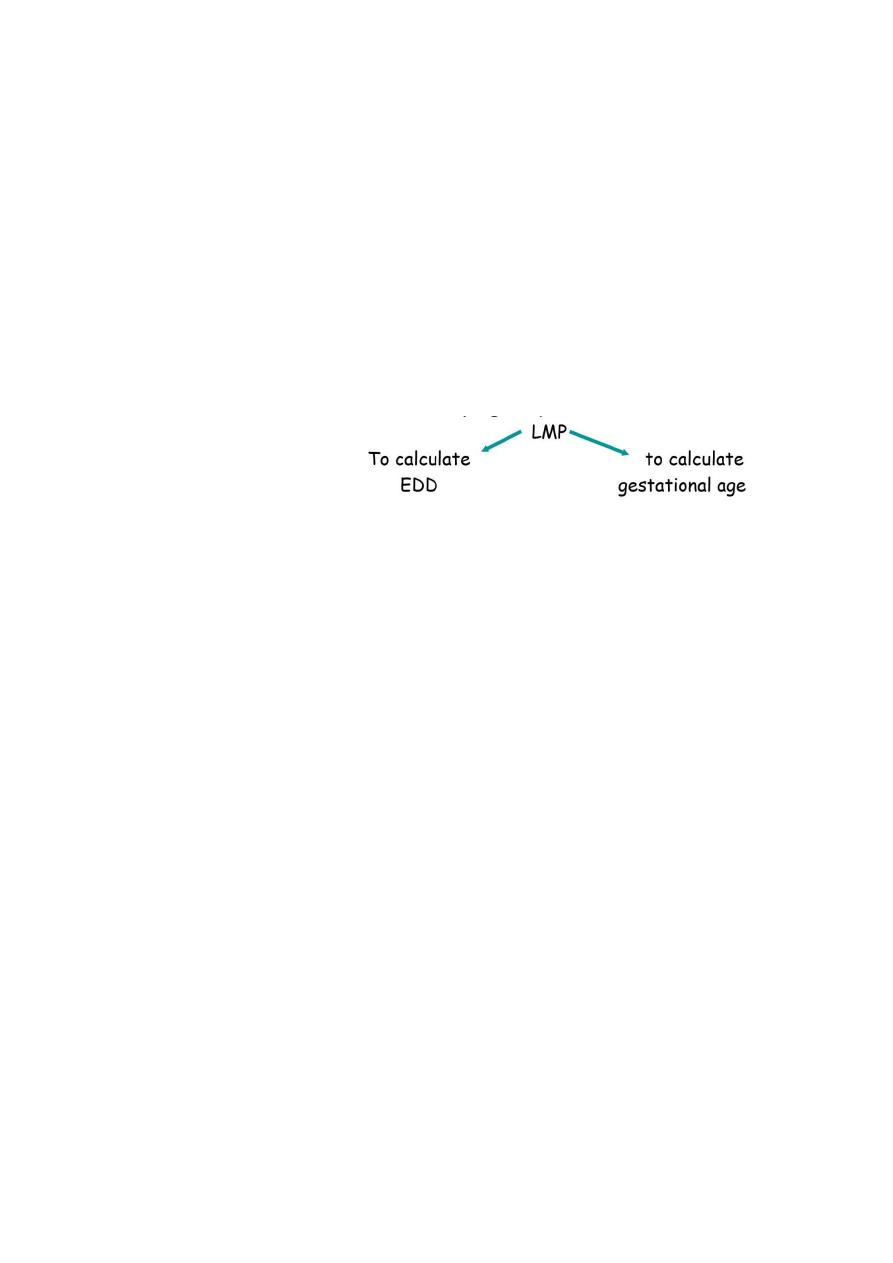
4-Menstrual history
5-Present pregnancy :
nausea ,
vomiting ,
lower abdominal pain,
bleeding ,
discharge….etc
6- History of drug use , still lactating, sensitivity ,B.T.
C- Physical Examination
Wt +Ht if <150 cm risk of contracted pelvis
Sudden wt gain pre-eclampsia
Blood pressure
Breast abnormality
Heart abnormality
Chest
Teeth caries
Legs varicosity +oedema
Abdominal Examination
- Fundal height
-Fetal heart sound
Pelvic examination
-Evaluation of bony pelvis for symmetry
-Examination of cervix for infection & dilatation
D-Laboratory Investigation:
GUE look for the following:
1- Pus cells UTI
2- Protein Pre-eclampsia
3- Bacteria UTI
12
Serology
1- syphilis
2- HIV
3- Rubella antibodies
4- HBs screening
History of chronic liver disease
Working in hemodialysis unit
House hold contacts
Multiple episodes of STDs
Multiple exposure to blood
Rh ABO group
Hb & PCV
E- Subsequent visits
Frequency
One visit every month ,till 28
th
week
28
th
-36
th
week every 2 weeks
36
th
onward once weekly
Examination
Blood pressure each visit
Weight is checked each visit
- little increase during the 1
st
12 weeks
- 16
th
-28
th
week 6kgs
after that 2kgs every 4 weeks
Ankle edema, hands, face…..
Fundal height should be recorded in every visit , similarly fetal heart sound & from
32th week onward presentation should be also checked.

13
Laboratory investigation
GUE ,Hb level during 2
nd
3
rd
trimester.
Rh –ve mother perform Ab determination test.
Repeated blood sugar estimation if there is family history of Diabetes
Note : if complication arise more frequent visits are needed
Conclusion
Elements of MCH are many started by premarital care which is directed to couples before
marriage to determine their suitability to their future life. This is followed by antenatal care
which is the care provided to the pregnant woman during pregnancy. It aims to Maintain,
protect & promote health & well being of mother, fetus & newborn infant . It includes
every aspect from screening to intensive life support .

14

15
Lec:11
Community medicine
Maternal and child health care - 3
Risk assessment & Screening
Nutrition during pregnancy
Other preventive measures
Health education during antenatal care
Specific Objectives
At the end of the lecture you will be able to
1. Appreciate risk screening as a major function of antenatal care and the intention to
use this approach.
2. Recall risk factors listed by the MOH present in the antenatal card .
3. Use the WHO scoring system to categories woman in to very high , high and usual risk
(low risk) categories.
4. Use MOH scoring system and its categories.
5. State actions taken to deal with a women in each category in both systems.
6. Describe nutritional requirements in pregnancy.
7. Describe common nutritional problems among pregnant women in Iraq with stress
on anemia.
8. Enumerate other preventive measures applied during antenatal care i.e vaccination,
supplements malaria chemoprophylaxis, treatment of hook worm infestation and
STDs treatment and prevention.
9. Suggest an important topics that should be discussed during health education
sessions during antenatal care.
Risk screening is a major function of ANC it involves using a list of risk factors & some form
of scoring system to separate women into risk categories ,typically
High risk &
Low risk.
The intention of risk screening is to
Predict problems even before they occur &
Identify women whose pregnancy or delivery is likely to raise problem &
To refer them at the appropriate time to hospital facility where necessary
medical equipments & expertise are available.

16
Criteria put by Ministry of Health for risk factors included
Maternal age
Primi < 16 yrs
Primi > = 30 years
Multi >35 years
Weight
Less than 45 kgs
more than 90 kgs
Height
<150 cm
Previous obstetric history
Threatened abortion
Habitual abortion
Missed abortion
More than 2 abortions
Stillbirth
HDP
Prematurity
Previous delivery history
Premature labour
Post mature labour
Previous Cs
Previous obstructed labour
Fetal abnormality
Medical history
Hypertension, renal diseases, DM, CVD, Thyroid disease, epilepsy.
Present obstetrical History
HDP
Anemia
Rh isosensetiation
High parity (>4)
Too short or too long spacing
Abnormal fetal presentation
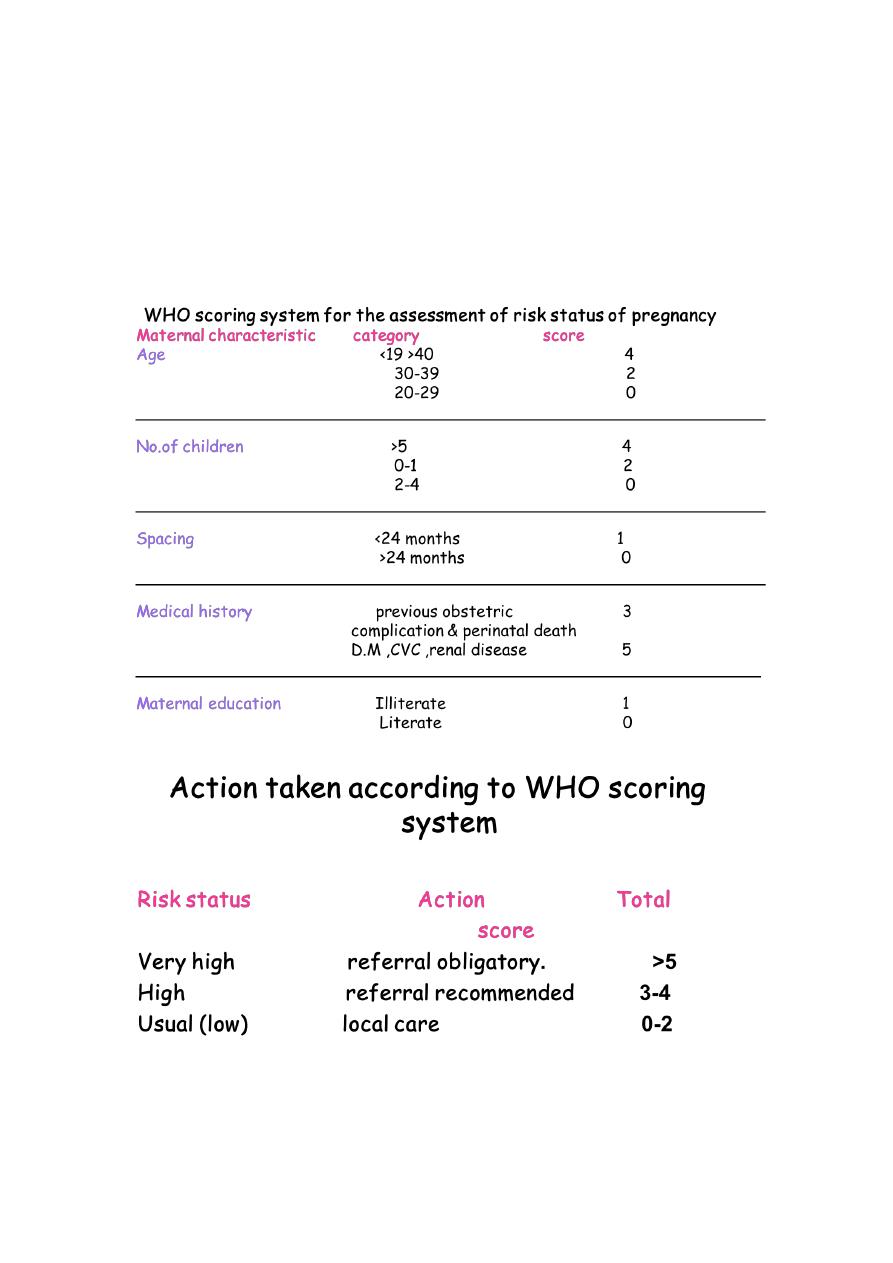
17
APH
Present obstetrical History
Twins
Minimum or no weight gain
Intra uterine growth retardation
Post-term pregnancy
Smoker mother

18
Nutrition During Pregnancy
Fetal development is accompanied by extensive changes in composition & metabolism of
maternal body. Many of these changes begin very early in pregnancy & may be under
hormonal control.
General increase in metabolism.
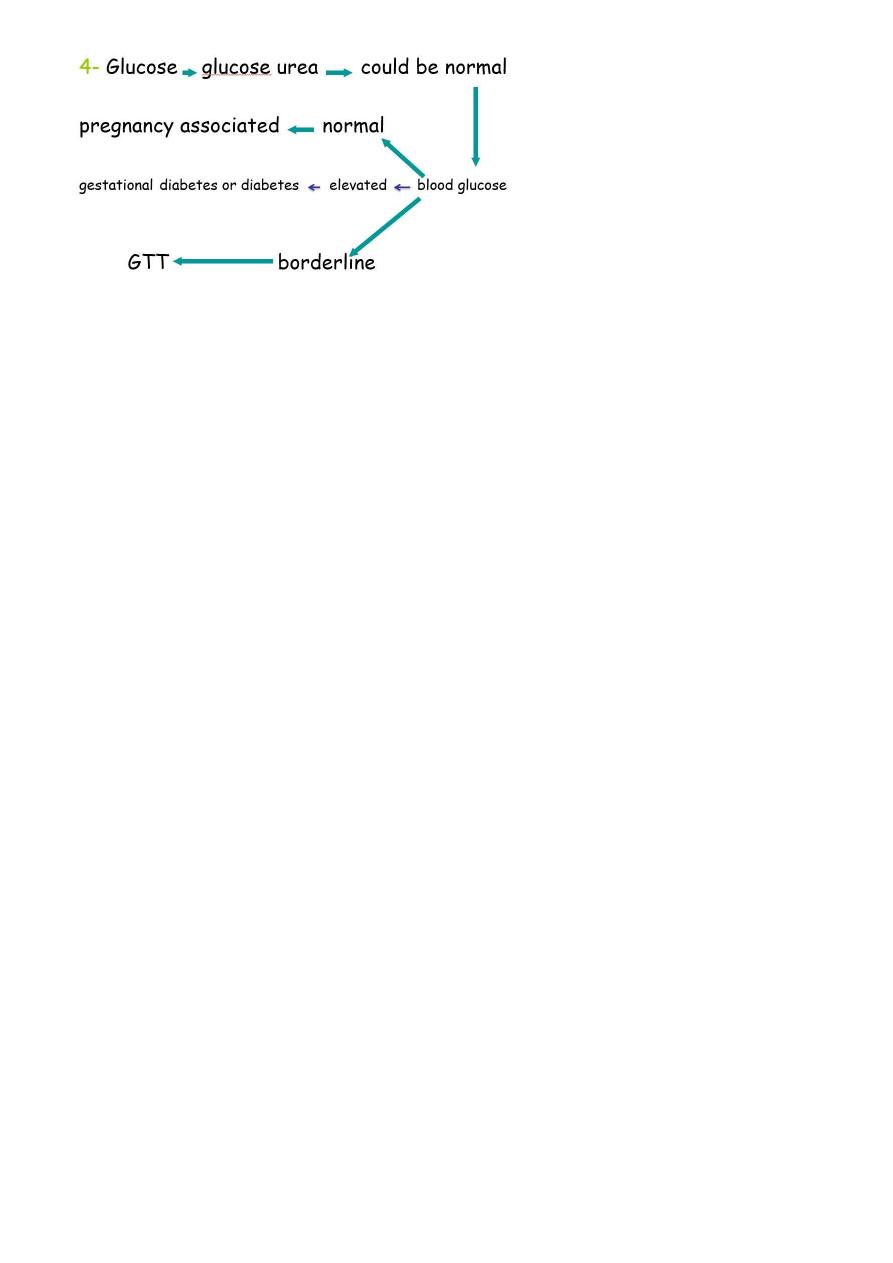
Changes in renal functions ( GFR, excretion of creatinin , excretion of same amino
acids ) & glucose urea.
GIT changes: changes in g.I mucosa to high absorption of Iron & Vits. (2times more
than normal).
Heamodilution & relative anemia.
Water overload (edema).
Weight Gain During Pregnancy
Products of conception, fetus, placenta , amniotic fluid & membrane.
Enlargement of organs of reproduction.
Increase in stored fat.
Retention of fluid.
o Healthy pregnant women gain 10-12 kgs.
o Undernourished women will gain <7 kgs.
o Gain in weight of <6 kgs indicates high risk.
Outcomes of Maternal Malnutrition
LBW & Prematurity
Fetal & neonatal Mortality & Morbidity
Increased chance of death in neonatal period
congenital Malformations
Possible Outcomes of Maternal Under-Nutrition
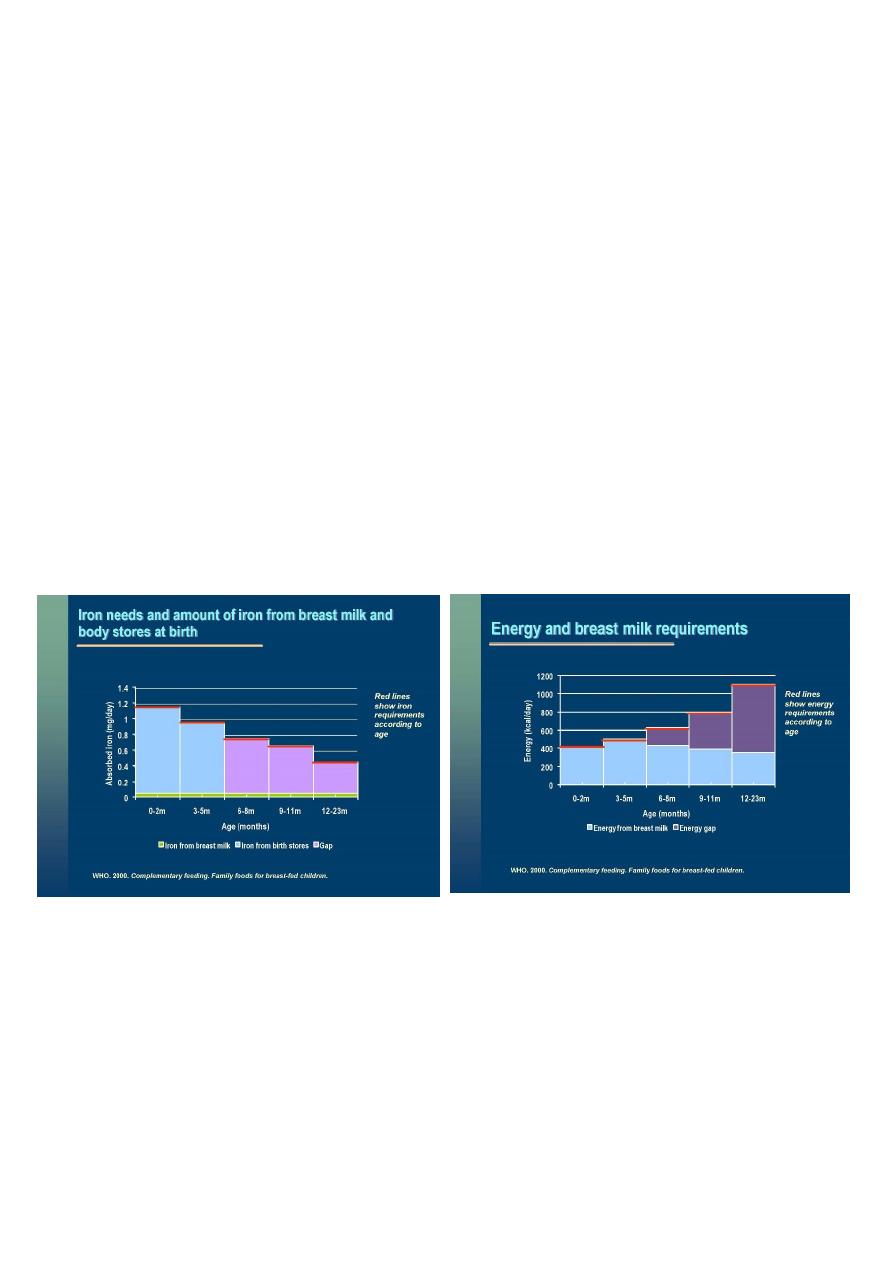
Anaemia in pregnancy
Defined as a hemoglobin concentration of less than 11gm/dl
During pregnancy plasma volume increases by 50% and the red cell mass increases by
20% leading to relative anaemia of pregnancy.
The iron stores, are usually depleted due to the successive periods, pregnancy and
lactation and diets containing low iron, mostly of low bio-availability.

19
Degree of anaemia
Moderate (Hb 7 -10 gm/dl)
Severe (Hb 4 -6.9 gm/dl)
Very severe (Hb less than 4 gm/dl)
Corresponding haematocrit (PCV) values are:
Moderate (24 – 37 %)
Severe (13 – 23 %)
Very severe (< 13 %)
WHO estimates that more than half pregnant women in the world & approximately
2/3 of pregnant women in developing countries have a Hb level indicative of
anaemia. This anaemia is associated with a five fold increase in maternal mortality.
Iron & folic acid supplementation may prevent the deterioration during the increased
physiological burden of pregnancy.
causes:
high iron requirement due to fetal & placental growth.
Impairment of Iron metabolism.
Short spacing.
Dietary iron low level.
Blood loss (Intestinal parasites).
It may be due to folic acid &Vit B deficiency leading to severe anemia ( 7 gm/dl).
It may be due to protien deficiency.
If anemia doesn't respond to iron therapy then it may be Thalesemia
Other preventive measures applied during antenatal care
Active immunization by tetanus toxiod 5 doses.
first dose at the beginning of the second trimester
one month
2
nd
dose
6months
1
st
booster
one year
2
nd
booster
one year
3
rd
booster
Iron & folic acid supplementation to treat anemia.
Nutritional supplementation (low weight gain during pregnancy & low pre
pregnancy weight )
High protein biscuit

21
Dried skimmed milk
In endemic area for malaria chemoprophylaxis.
Treatment of hook worms & other helminthes.
Prevention & treatment of STDs.
Health Education
Proper nutrition.
Personal hygiene & environmental sanitation.
Normal changes during pregnancy & important dangerous signs.
Importance of tetanus toxoid vaccination.
Home activities: sleep ,rest ,exercise ,avoidance of exhausting work.
Training for child birth & clean delivery.
Preparation for :BF , principles of child care , feeding , weaning , vaccination ….,etc
Conclusion
Essential element in MCH services include six elements. Pre-conceptional care is the first
step followed by antenatal care which is a vital and called a normal care. Services provided
during such care are intended to promote and protect health and well being of mothers
and their fetus.

21
Lec:12
Community medicine
Maternal and child health care - 4
22

23

24

25

26

27
Lec:13
Community medicine
Young child clinic
At the end of the lecture you will be able to
1. Realize the importance of young child clinic in health promotion and prevention of
childhood diseases.
2. List components of essential services provided by this clinic.
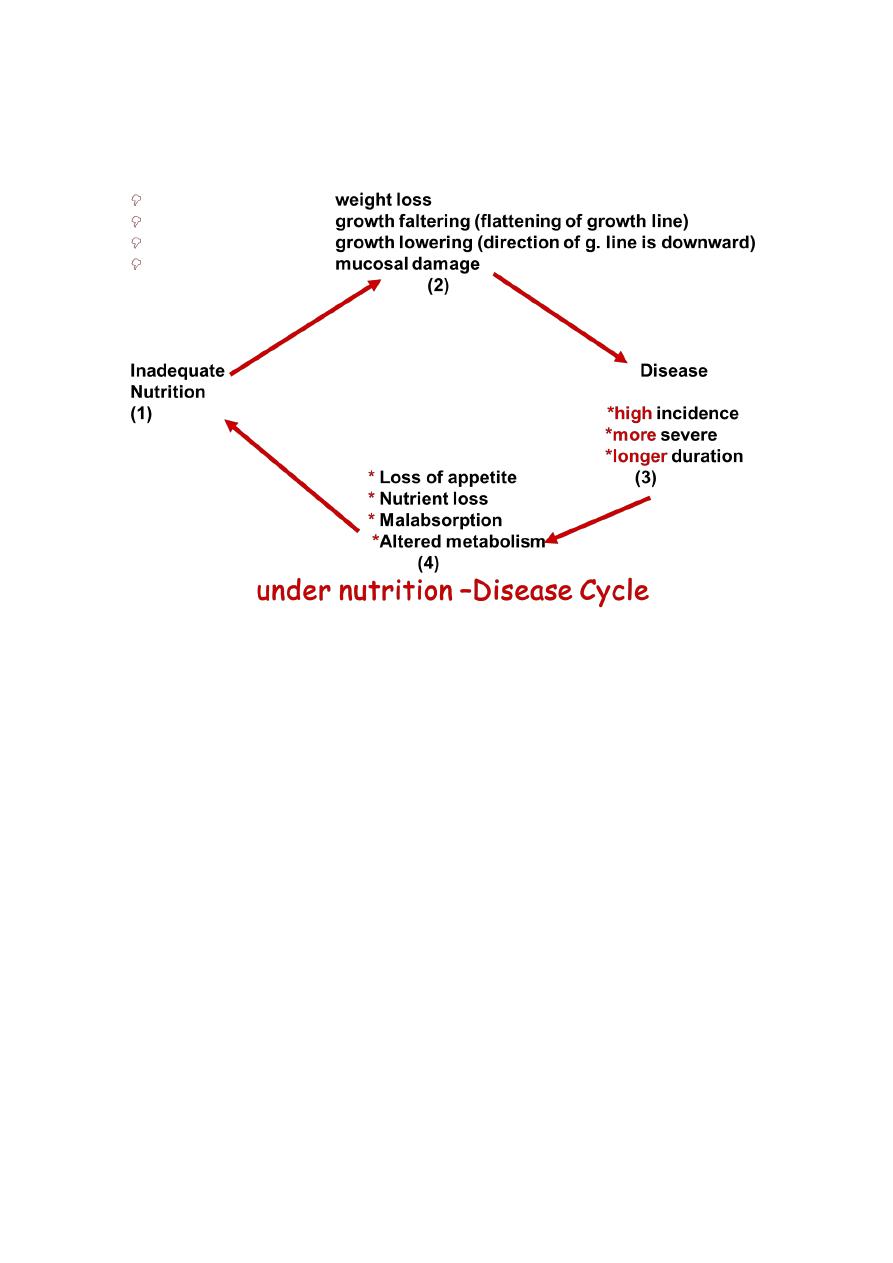
3. Draw under nutrition-disease cycle.
4. State objectives of growth assessment.
5. Describe the significance of growth assessment as an effective approach to the
prevention of malnutrition
6. Use growth chart (weight for age) to explain the normal variations in weight of children.
7. Use growth chart as a tool helpful
in assessing the rate of growth and detection of nutritionally at risk child.
8. Define and interpretate height for age and weight.
9. Define Body Mass Index (BMI).
10. Calculate BMI.
11. Realize the importance of BMI.
12. Identify children at high risk.
Child health care
Young child clinic
Preventive services are important for children
1- Many causes of morbidity & mortality are avoidable e.g. different type of accidents,
infectious disease namely the childhood targeted diseases.
2- Existence of socio-economic difference. IMR in developed countries: e.g.UK <10/1000
Live Births.
In developing countries : e.g. Afghanstan 125/1000 LB
3- Children are exposed to variety of health hazard (infection +malnutrition)
4- Children are more vulnerable due to the stress of growth & development
Child health care includes the following strategies instituted by WHO:
Growth monitoring (assessment, surveillance)
and ARI Control of diarrheal diseases
Breast feeding
28
Immunization
Family planning
Food supplementation
Females education
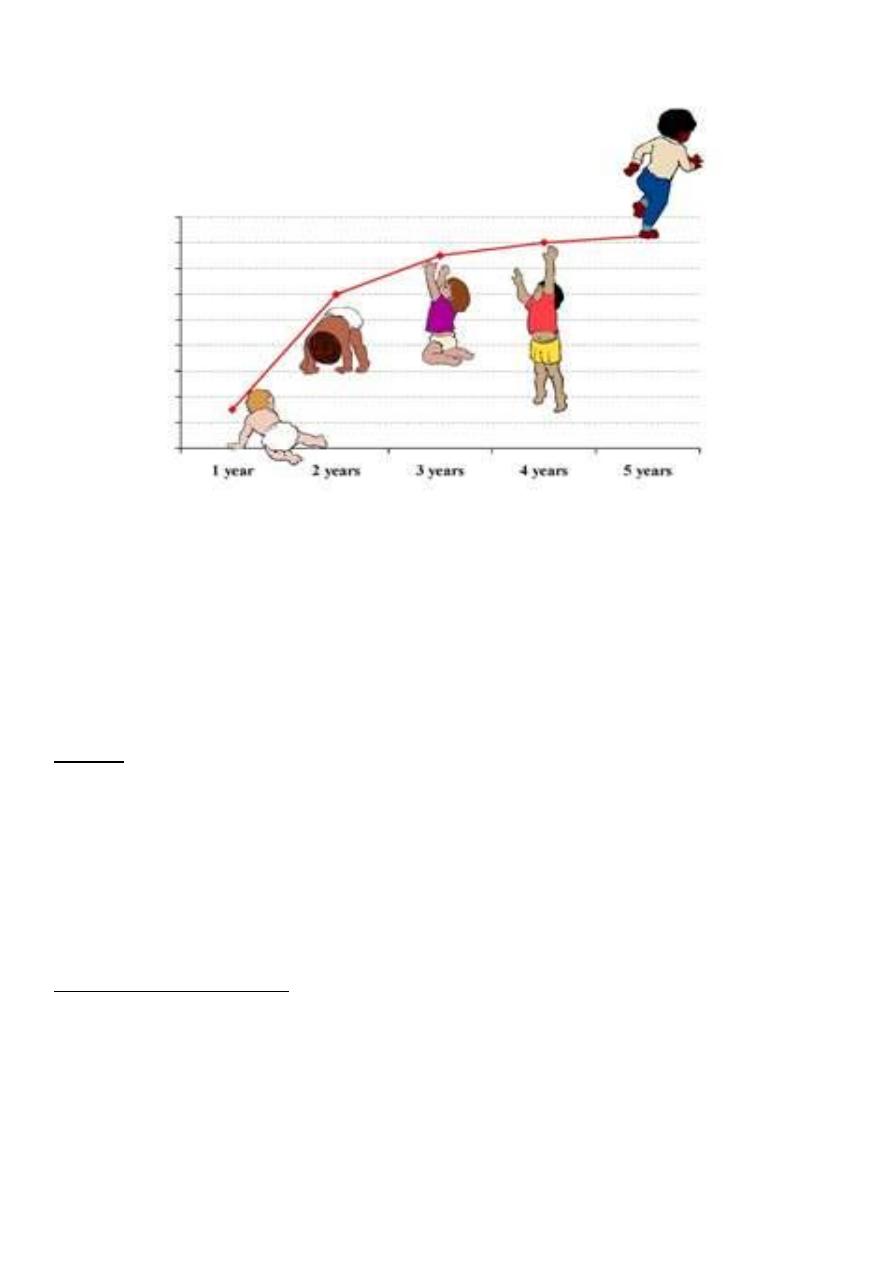
Growth monitoring (assessment, surveillance)
It is a process of sequential measurements of weight of children under the age of 5 years,
in order to detect growth failure as early as possible and to correct this failure.
This process should start soon after birth with the measurement of birth weight and
height and recording on the growth chart.
Child growth assessment
Basic growth assessment involves measuring a child’s weight and length or height and
comparing these measurements to growth standards. (WHO Standard)
The purposes (objectives) are to determine whether :
o Child is growing “normally” or
o Has a growth problem (detection of growth failure) .
Child health care
Careful growth assessment is best available tool of measuring the overall nutritional status
& evaluate health of children under five & plan appropriate follow –up activities.
29
Surveillance of growth and development
Growth assessment
Weight-for-age
Scale used in portable & relatively inexpensive.
Weighing is relatively easy.
Measure is not time consuming.
It is sensitive.
Benefits
o To compare the measurement with standers.
o To examine trends and changes of growth.
o To interpret the progress of growth when the child age is unknown.
Single record indicates child size at moment. It does not give any information about child's
weight is increasing, stationary or declining.
Ideal weight measurement:
o Monthly during the1st year..
o Every 2 months in 2nd year
o Every 3 months up to the end of the 5th years.
o Minimum weight gain in 1st 3 months is 500 gm/ month
o Gaining weight less than 500gm means growth failure.
o Usually 1 Kg/month
o Double the birth weight by 5 months of age.
31
o Treble by end of 1st year of life.
o Quadruple by the age of two years.
Facts
o Most growth failure is invisible.
o Most children with growth failure live in homes where there is no absolute shortage of
sufficient food.
Height (length) –for- age
Height should be taken in a standing position without foot wear.
If the machine is not available, the measuring scale fixed to the wall can be employed
It is suitable for children 2 years and above
Length of baby at birth about 50 cm.
Increasing by 25 cm during 1st years
Increasing by 12 cm during 2nd years
Low height for age (Nutritional Stunting, Dwarfing)
It reflects past or chronic malnutrition.
Weight in relation to height is important than weight alone.
It determines whether a child is within range of normal weight for his height
Low weight for height (acute malnutrition, wasting, emaciation)
It is associated with high mortality and morbidity rate
A child who is less than 70% of the expected weight –for-height is classified as severely
wasted.
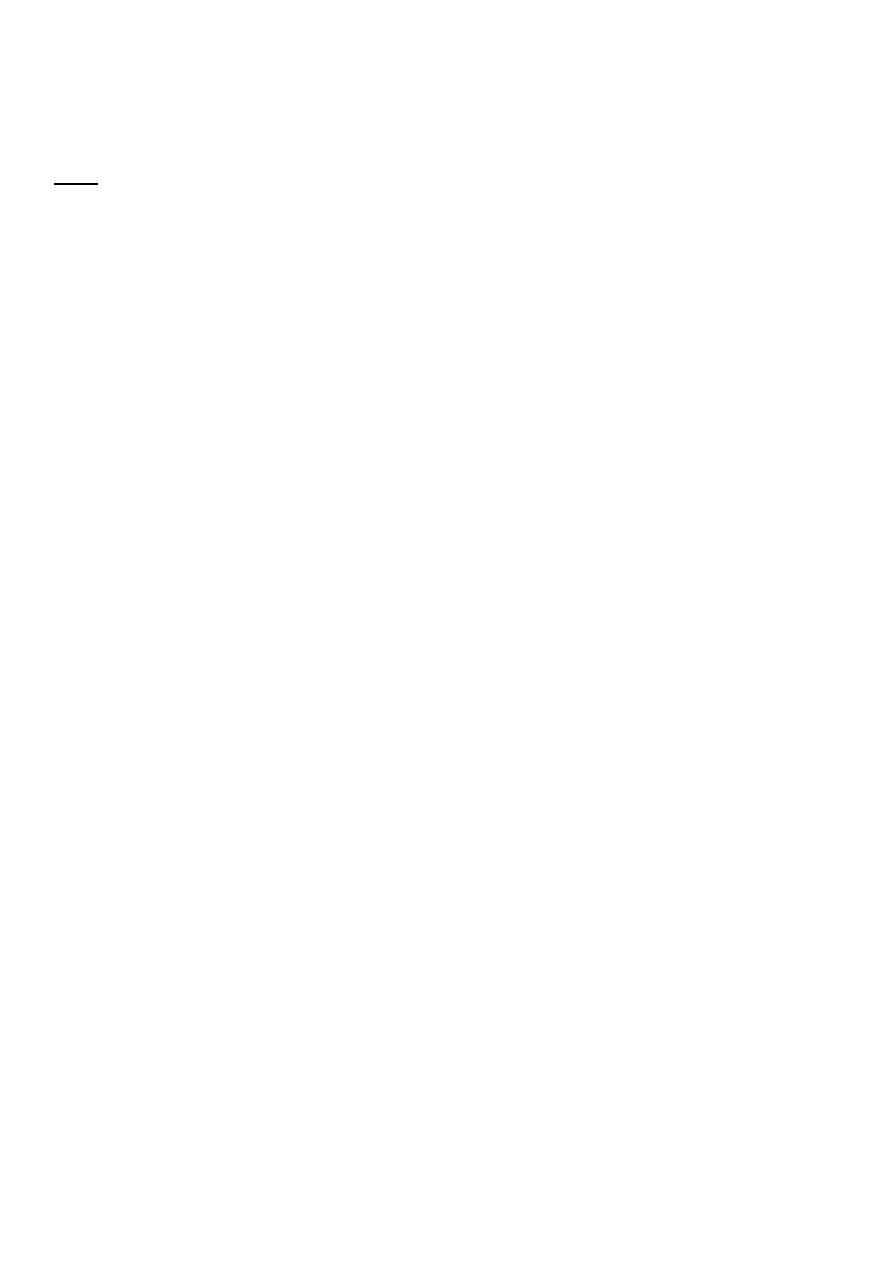
Body mass index (BMI)
BMI is a number that associates a person’s weight with his or her height/length.
BMI is calculated as follows: Weight in kg ÷ squared height/length in meters
Another way to show the formula is kg/m2.
BMI is rounded to one decimal point.
It is very important to use a length measurement for a child less than 2 years old and a
height measurement for a child age 2 years or older
31
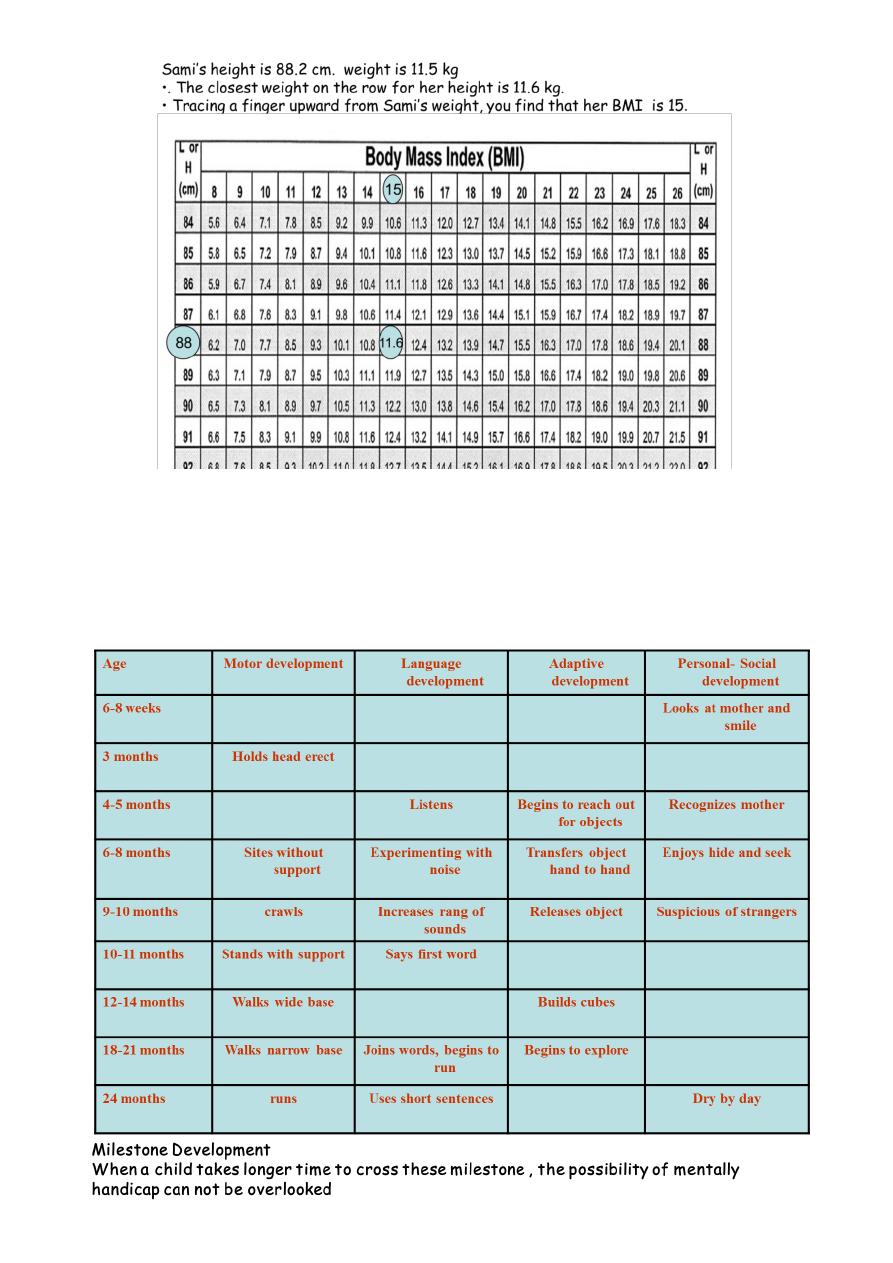
Behavioral Development
Motor development
Personal- Social development
Adaptive development
Language development
32
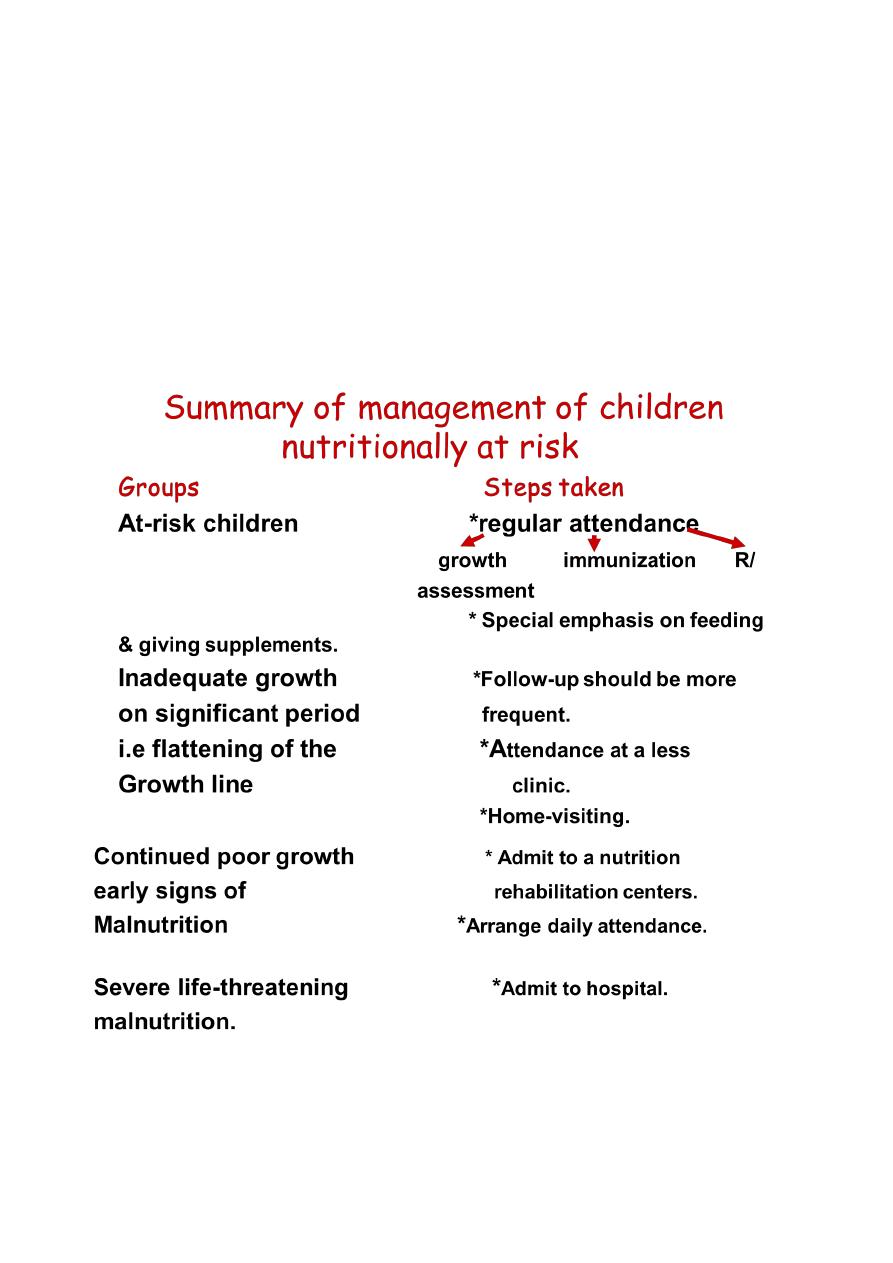
Identification of at risk children
Basic criteria include :
Birth weight <2.5 kg
Twins
Birth order >= 5
Artificial feeding
Failure to gain weight during succesive months
Children with PEM, repeated attacks of diarrhea, and ARI
Low socio-economic strata
Illiterate mother
Conclusion
Under fives clinic is a part of MCH services it is intended to promote heath and wellbeing of
the under fives through growth monitoring oral rehydration, immunization, breast feeding
and family planning female education and food supplementation.
33
Lec:14
Community medicine
Family Planning
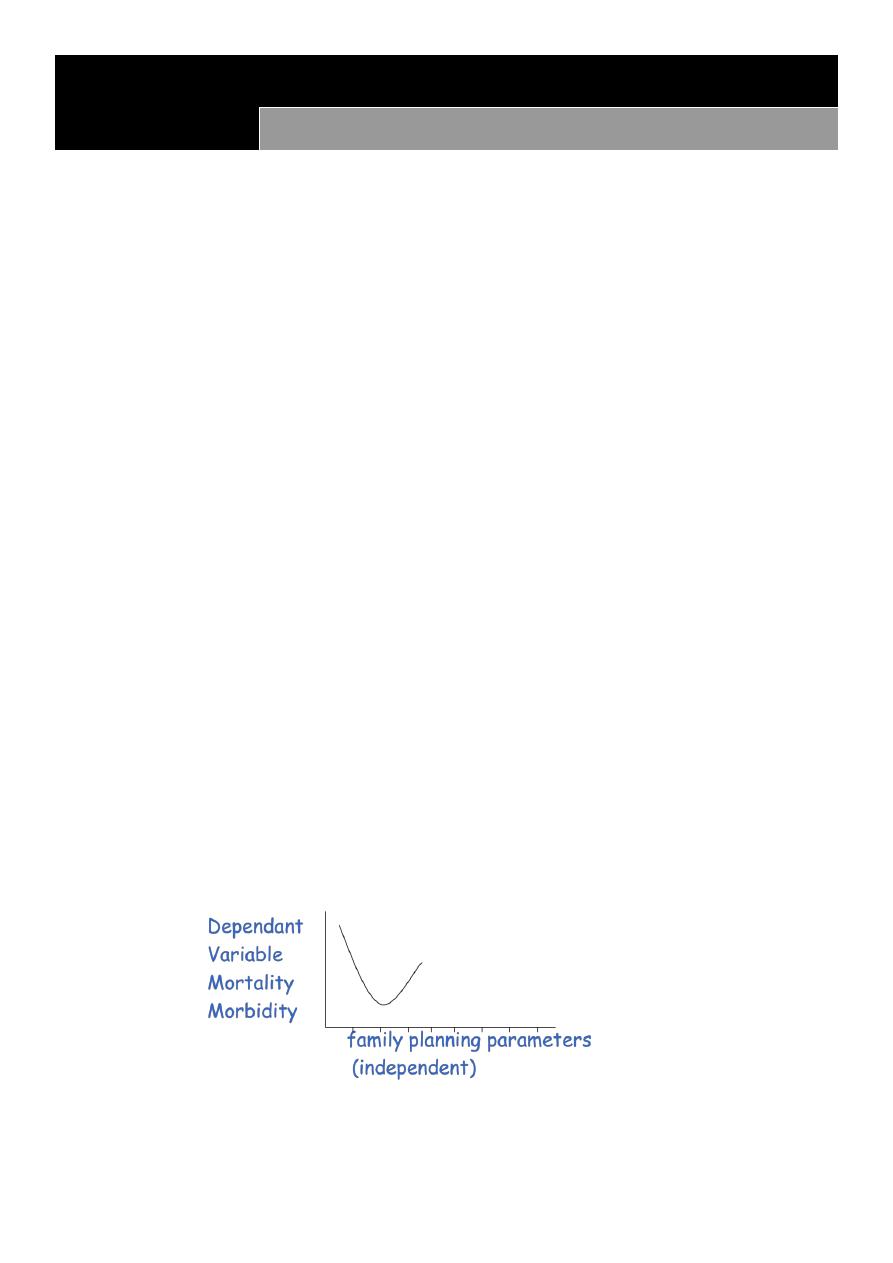
At the end of the lecture you will be able to
1. Define family planning (FP), its objectives and parameters.
2. Draw a line diagram shows the association of FP parameters and maternal ,perinatal,
neonatal and infant mortality and morbidity.
3. Realize the importance, way of administration and target groups for food
supplementation.
4. Define food fortification.
5. Enumerate most common micro-nutrients used.
6. State way of administration with stress of Vit A (target group outcome, prevention of
Vit A deficiency.
7. Realize the importance of female education in enhancing overall family health.
8. Define low birth weight (LBW), small – for-date and preterm newborns.
9. Enumerate common causes of LBW.
10. State importance and incidence of LBW (worldwide and Iraq).
11. .Suggest a plan for prevention of LBW.
Family Planning
Practice that help couples to attain certain objectives:
To avoid unwanted pregnancy.
To regulate intervals between pregnancies (spacing).
To control time at which birth occurs in relation to age of parents particularly mothers
(timing).
To determine the ideal number of children within the family (family size).
Risk to mothers & infants is greatest at the following situations
<18 years of age (too young)
>35 years of age (too old)
34
After the 4th birth (too many )
Less than 2 years apart (too close)
Food Supplementation
Three specific forms of food supplements that have proved to be high cost-effective:
1. Food supplements directed to target groups
Pregnant women at risk of delivering LBW Extra food supplements(3
rd
trimester) (500
cal+10g PTN /day) Extra gain in WT of 1.5 kg 300g in BW
2. Food fortifications
A process where by micro-nutrients are added to food to maintain or improve the quality of
diet of a community.
In order to deal with specific nutritional deficiencies & is typically used with conjunction with
staple foods.
Iodine added to salt
Vit A capsules or drops every 6mnths
Iron changing dietary habits
Iron supplements to pregnant +lactating
food fortification (salt, sugar).
Vitamin A
Impact of Vit on child survival
Improving vit A status in children results in global mortality reduction of 23%.
Vit A helps to prevent 1.3-2.5 million deaths annually in children less than 5 years of
age.
Vit A is used in treatment and prevention
Indications
Current Xerophthalmia
Measles
Severe malnutrition

35
Vit A: prevention
Combining the administration of vitamin A supplements with immunization is an
important part of this effort together with measles immunization and National
immunization days to eradicate polio.
Providing high – dose supplementation to new mothers soon after delivery has
provided further benefits to young infants through enriched breast milk (200 000 IU)
during immunization contact. (only once)
Periodic oral supplementation
o Children age 9-12 months, 100.000 IU every 4-6 month.
o 12 months, 200.000 IU every 4-6 months.
Optimal interval between doses is (4 – 6 months).
A dose should not be given soon after a previous dose of vitamin A supplement.
Interval can be reduced in order to treat clinical vitamin A deficiency and in measles
cases.
Food fortification : Vit A fortified sugar
Food diversification
o Yellow fruits
o Carrots
o Green leafy vegetable
o Liver and oil
Female Education
Act as a powerful independent force in reducing number of infants & children deaths. How?
1. Schooling enhances women’s ability to provide adequate care.
2. Education enhances women status & power within the family.
3. Educated mothers can use health services & facilities properly.
Considering low birth weight (LBW) There are two main groups
Those born prematurely
Those with fetal growth retardation
In Iraq…….which is more common?????
Definition….
Birth weight (BW) less than 2.5 kg ( up to and including 2499 gm)
Measurements being taken preferably with the first hour of life.
36
Apart from BW , babies can be classified into 3 groups
Preterm born before 37 wks of gestation
Term… 37-42 completed wks of gestation
Post term… 42 completed wks and over
Preterm
Causes ..multifactorial….
multiple births, acute infection, hard physical work, hypertensive disorders of pregnancy.
Prevention …
good antenatal care, discouragement of adolescent pregnancy, and treatment of
hypertension.
Small for date…
The weight is less than the 10
th
percentile for the gestational age ..it is the result of
intrauterine growth retardation.
Maternal causes.
malnutrition, severe anemia, heavy physical work during pregnancy, hypertension, toxemia,
smoking, malaria, short maternal stature, high parity, short spacing, too young mothers ….etc
Percentage of low BW babies (incidence) =
No. of live birth babies with weight less than 2.5 kg
Total no. of live births x 100%
Incidence……world wide is 17%
95% in developing countries.
The target reduction in the incidence is to less than 10%
Importance of low BW
Low BW is the most serious challenge in MCH in both developed and developing countries.
Its public health significance may be ascribed to ..
High incidence.

37
Its association with mental retardation.
High risk of perinatal and infant mortality.
Human wastage and suffering.
Very high cost of special care.
Its association with socio-economic under development.
Prevention
Direct intervention measures
Identification of at risk pregnant women and steps should be taken to reduce the
risk……use the high risk approach
Some of the direct intervention are as follows:
Prevention
Proper feeding of pregnant women.
Treatment of anemia by iron folic acid supplementation.
Supplementary feeding.
Fortification and enrichment of food…..etc.
Controlling infection..e.g. UTIs, malaria, rubella, toxoplasmosis, syphilis.
Early detection and treatment of hypertension, toxemia, and diabetes.
Indirect intervention
Family planning.
Avoidance of smoking.
Measures aimed to improve health and nutrition of young girls.
Improvement of socio-economic and environmental conditions conditions.
Distribution of health services especially in the under-served areas.
Government support through maternity leaves with full wages and child benefits.
Treatment
Incubatory care.
Feeding.
Prevention of infection.

38
Leading Causes of Death
Atelactasis
Malformation
Pulmonary hemorrhage
Intracranial hemorrhage secondary to birth trauma or anoxia
Pneumonia and other infections
Conclusion
Family planning, female education and food fortification play an important role in the
child health care strategy.
Low birth weight is an important problem. Its public health significance is ascribed to
its high icidence and significant association with high infant and childhood mortality
and morbidity, which is reflected on the community development as a whole.
39
Lec:15
Community medicine
Integrated Management of Childhood Illnesses
At the end of this lecture you will be able to:
1. Enumerate most common causes o underfives death in developing countries.
2. Define IMCI.
3. Identify objectives of IMCI.
4. Discuss elements of IMCI.
5. Draw charts show summary of IMCI for children 2months-5 years and 1 week to 2
months.
Integrated Management of Childhood Illnesses (IMCI)
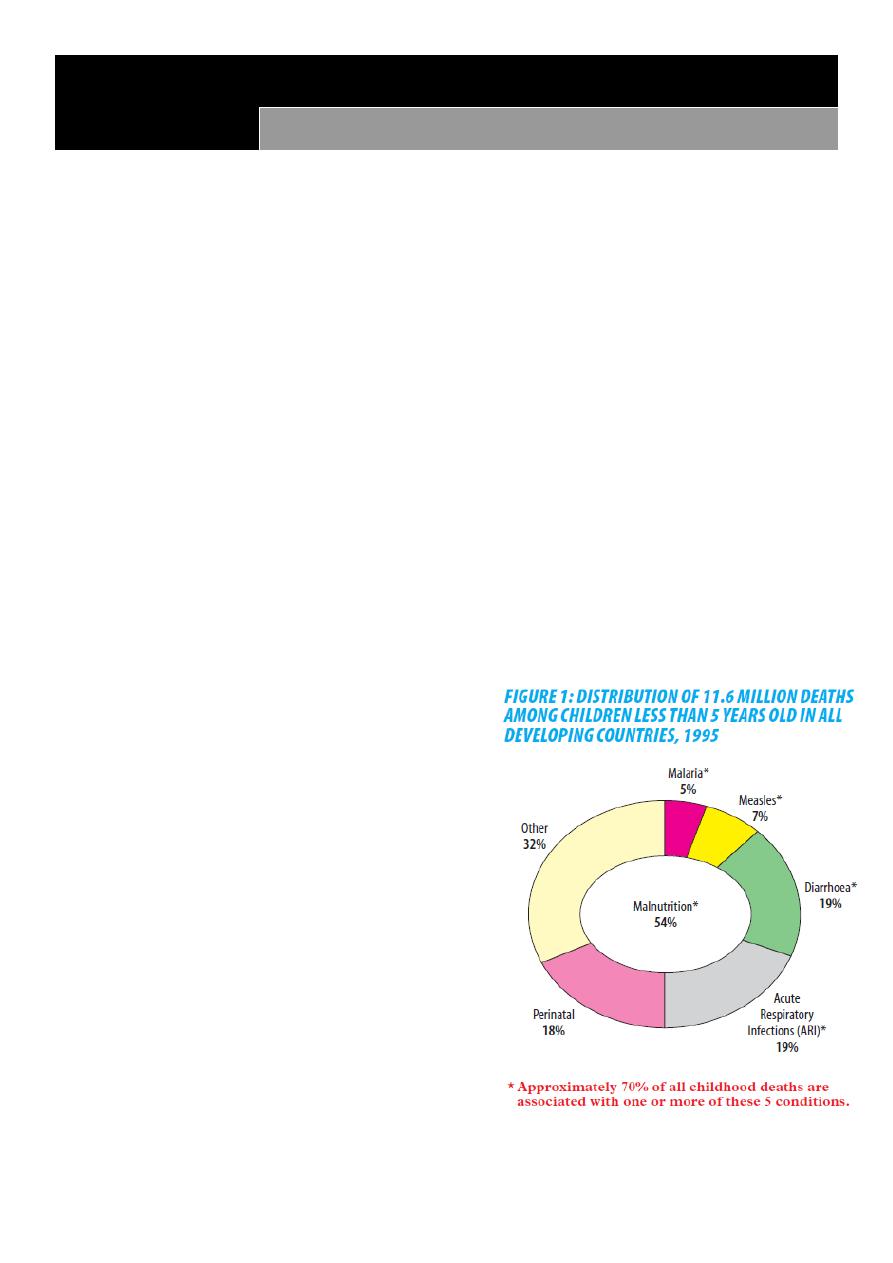
Altogether more than 10 million children die each year in developing countries before they
reach their fifth birthday.
Seven in ten of these deaths are due to
acute respiratory infections (mostly pneumonia),
diarrhea,
measles,
malaria, or
malnutrition; and often
to a combination of these conditions
Every day, millions of parents take children with
potentially fatal illnesses to first-level health
facilities such as clinics, health centers and
outpatient departments of hospitals.
In some countries, three in four episodes of
childhood illness are caused by one of these five
conditions. And most sick children present with
signs and symptoms related to more than one.
This overlap means that a single diagnosis may not be possible or appropriate, and that
treatment may be complicated by the need to combine therapy for several conditions.
41
Surveys of the management of sick children at these facilities reveal that many are not
properly assessed and treated and that their parents are poorly advised.
At this level, in most developing countries,
Diagnostic supports such as radiology and laboratory services are minimal or non-
existent;
drugs and equipment are scarce;
combined with an irregular flow of patients,
Health care providers at primary health care centers have few opportunities to practice
complicated clinical procedures.
Instead, they must often rely on history and signs and symptoms to determine a course
of management that makes the best use of available resources.
WHO and UNICEF developed a strategy known as Integrated Management of Childhood
Illness (IMCI).
The strategy combines Improved management of childhood illness with aspects of
nutrition,
immunization, and
other important disease prevention
In addition to health promotion elements.
The objectives of IMCI are to:
reduce deaths, frequency and severity of illness and disability, and
contribute to improved growth and development.
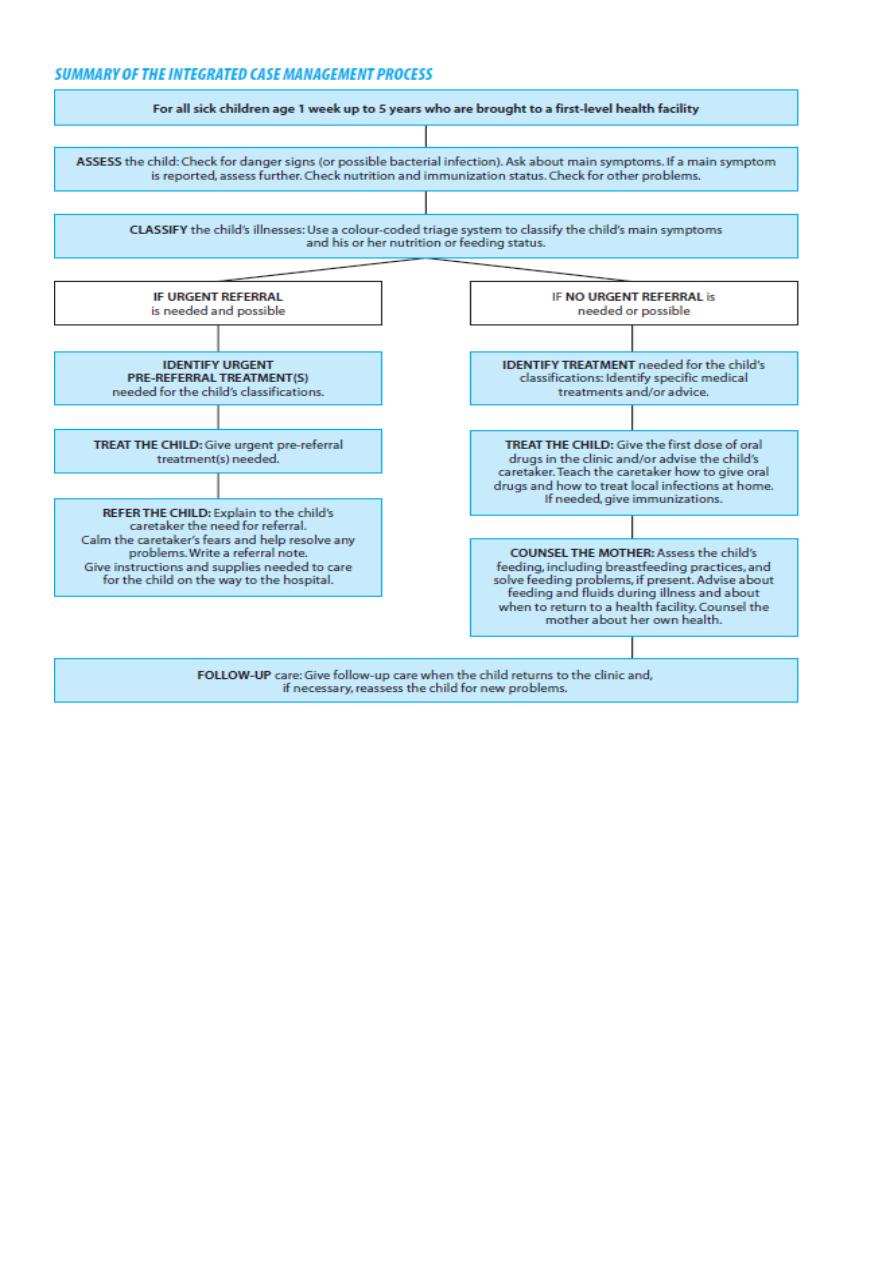
Integrated case management relies on:
Case detection using simple clinical signs and treatment.
Few clinical signs as possible are used.
The signs are based on expert clinical opinion and research results, and strike a careful
balance between sensitivity and specificity of the signs and symptoms.
Sensitivity and specificity measure the diagnostic performance of a clinical sign compared
with that of the gold standard, which by definition has a sensitivity of 100% and a specificity
of 100%.

41
Sensitivity measures the proportion or percentage of those with the disease who are
correctly identified by the sign. In other words, it measures how sensitive the sign is in
detecting the disease.
Sensitivity = true positives / [true positives + false negatives]
Specificity measures the proportion of those without the disease who are correctly called
free of the disease by using the sign.
Specificity = true negatives / [true negatives + false positives
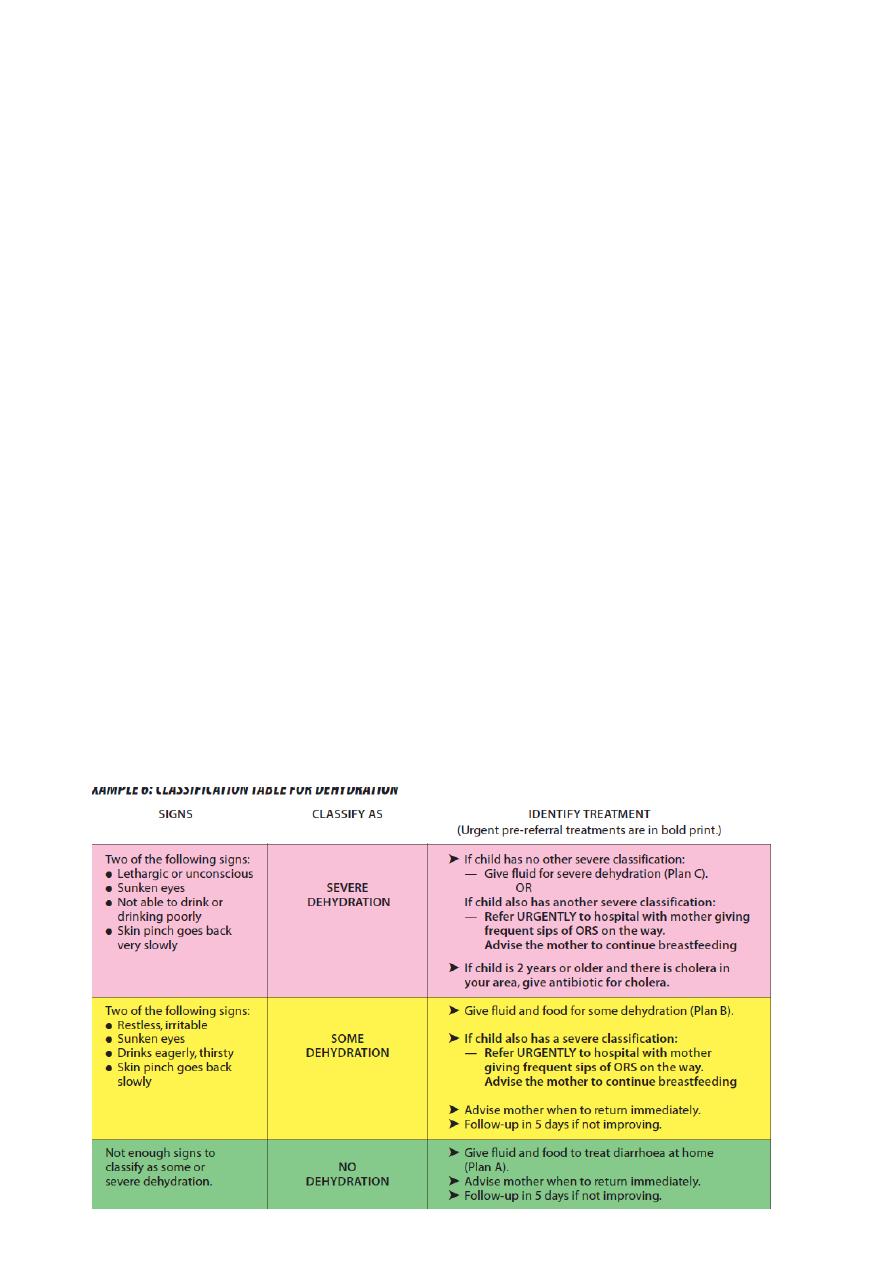
IMCI allows a health care provider to determine
If a child should be urgently referred to another health facility
Or
If the child can be treated at the first-level facility (e.g. with oral antibiotic, antimaiarial,
ORS, etc.)
Or
If the child can be safely managed at home.
The core of the IMCI strategy
The core of the IMCI strategy is focus on the most important causes of death:
Diarrhea
ARI
Malaria
Measles
Malnutrition
The complete IMCI case management process involves the following elements:
First assesses the child by
Identifying any danger signs,
Asking about the four main symptoms in all children (cough or difficult breathing,
diarrhea, fever, and ear problem), Carrying out further assessment if a main symptom
is reported, and
Reviewing the nutritional and immunization status in all children.
42
Then classifies the child's illnesses.
Each illness is classified according to whether it requires:
- urgent referral;
- specific medical treatment and advice; or
- simple advice on home management.
After classification, specific treatments are identified.
If the child has to be referred urgently to a hospital, give only essential treatment before
departure. Since most children have more than one illness.
Practical treatment instructions are carried out, including
Teach the mother how to administer oral drugs,
To increase fluid intake during diarrhea and to treat local infections at home.
The mother is advised on the signs which indicate that the child should immediately
be brought back to the clinic and when to return for routine follow-up.
Feeding is assessed and counseling of mothers on feeding problems is provided.
Follow-up instructions for various conditions are given when the child returns to the
clinic.
If necessary, reassess the child for new problems.
43
Conclusion
IMCI is a strategy combined management of illnesses of children <5 years of age and taking
care of their nutrition, immunization, and other health promotion aspects. The core elements
are: assessment, classification, treatment, giving practical instructions, feeding assessment
and counseling, and lastly giving follow up instructions.

44

45
Lec:16
Community medicine
Breast Feeding
At the end of this lecture you will be able to:
1. Identify hormones play a role in milk production.
2. State variations in breast milk composition.
3. Have a look on the composition of breast milk.
4. List reflexes played a role in Breast Feeding (BF) process.
5. Describe various steps that determine correct positioning in BF.
6. Enumerate disadvantages of Bottle Feeding
7. Enumerate benefits of BF.
8. List contraindications to BF.
9. List conditions in which BF is not contraindicated.
10. Enumerate ten steps to successful BF.
11. List common problems associated with BF, causes, prevention and treatment.
12. Indicate the time of introduction of
13. Complementary food
Define weaning and weaning period.
14. List causes of diarrhea and malnutrition associated with weaning.
15. State time of starting weaning and for how long.
16. Describe the process of weaning and type of food given.
Breast Feeding
Milk production is under control of the hormone prolactine which is secreted from the
anterior part of the pituitary gland.
Oxytocin is hormone produced by the posterior part of the pituitary gland which is
responsible for milk ejection.
The composition changes according to the need of the child & mother factors. It varies
according to the following
1) Stage of lactation : 1st week colustrum.
2
nd
week transitional milk.
there after mature milk.
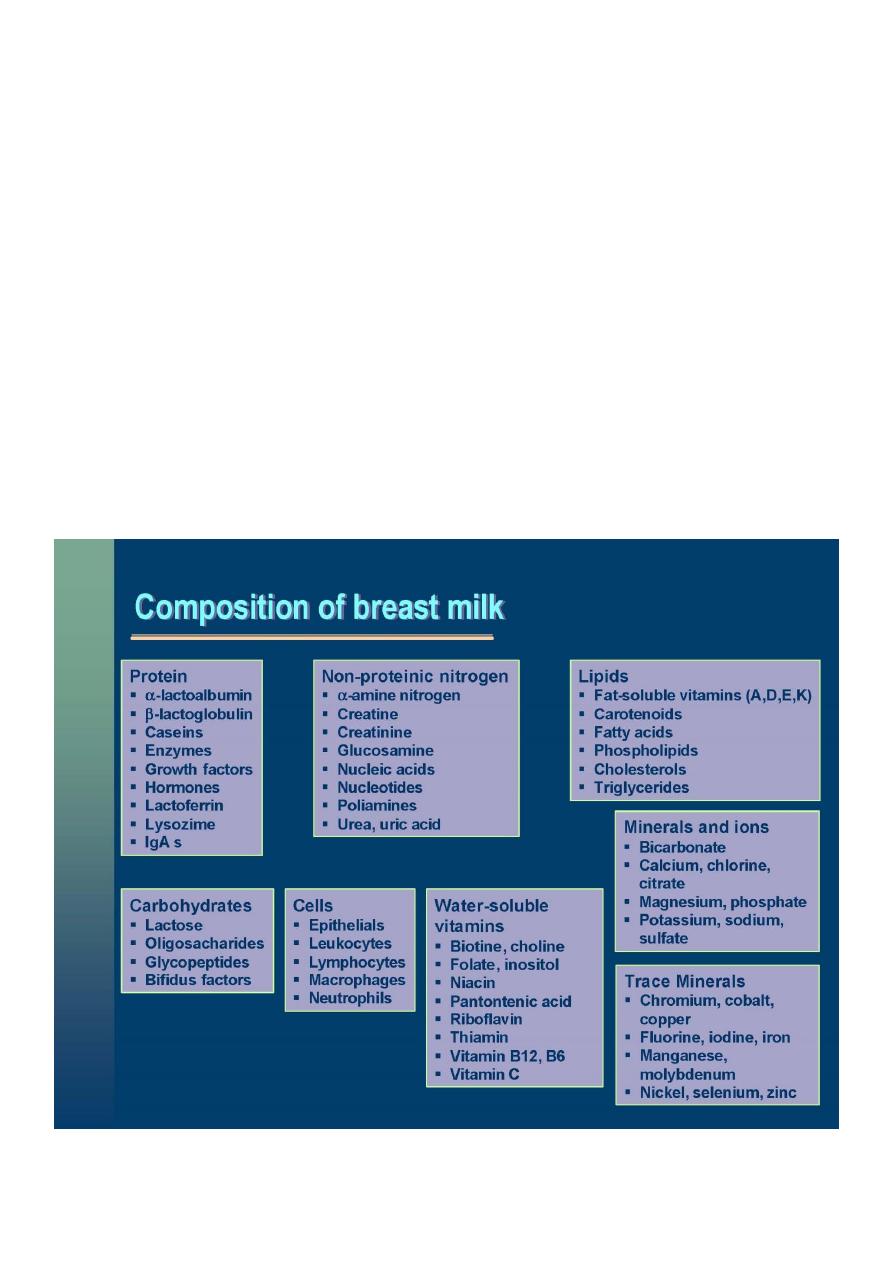
46
Fore milk Water content is more at the beginning of the feed.
Hind milk Fat content is more at the end of the feed.
2)Time of the day
Fat content is highest in the mid – day.
3) Maternal nutrition
The quality of milk will be affected by maternal under-nutrition only in its severe forms.
4) Climate
Hot climate more water is needed, mother doesn’t have to give extra-water.
Cold climate there will be an increase in fat content which will lead to higher energy
production.
5) Individual variation.

47
Breast feeding process; Reflexes
Rooting Reflex
If the cheeks or lips of the infant are stimulated (touched) he opens his mouth and turns his
face to the nipple.
Suckling Reflex
The infant suckles anything that enters his mouth and touch the roof of the mouth (palate).
This reflex is very vigorous at birth.
Swallowing Reflex
The infant swallows the milk, and coordinates this reflex with the suckling reflex.
If the reflexes are not well developed (as in a preterm baby), the breast milk can be given
by a Naso-Gastric tube.
If the baby opens his mouth widely, he will take the areola with the nipple & press on the
milk lakes so the milk is expelled. If the mouth is not opened widely, he will take only the
nipple & bite on it & no milk will be expelled. This will result in nipple cracks, which are
very painful.
Positioning in breast feeding
Correct positioning will determine the success of breast feeding. There are various steps to
correct positioning:
1- Positioning of the mother
She must breast feed in a comfortable & relaxed position because if not, she will feel tired &
end the feed quickly. The mother should sit with a straight back supported with a pillow, or
if she can’t sit straight then she can feed the baby while lying down on her back, or on her
side and the baby beside her.
2. Positioning of the infant
Head and body are in one line with a straight neck.
Infant is facing the mother.
Infant is well supported (when he is still small one hand is enough for support but later
on both hands are used).
Infant is close to the mother.
3- Attachment to the breast
Mouth should be opened widely
Chin touching the breast.
Lower lip turned outward.

48
The lower part of the areola should not be seen & the upper part should be partly visible.
4- Effective suckling
Slow deep sucks, pauses from time to time, swallowing can be seen, the mother feels
no pain.
Wrong position
This baby is not in the right position.
He is nipple feeding ,not breast feeding. If he is allowed to continue to do so ,his mother
will develop nipple cracks.
Right position
This baby is just in a right position, the mouth is widely opened.
Chin is touching the breast.
Lower lip turned outward.
The lower part of the areola is not seen & the upper part is partly visible.
Disadvantages of bottle feeding
Contamination diarrhea malnutrition. Lack of BF increases the risk of death from
diarrhea to 6.1 times and from pneumonia to 2.4 times.
High cost the mother will give diluted feed malnutrition.
Low level of vitamins , iron anemia.
Hypernatremia acidosis (in LBW infants), kidney diseases & diarrhea.
Hypercalcemia due to the high content of Ca in cow milk.
Higher content of saturated fatty acids in cow’s milk. Infants need unsaturated fatty acids
for brain development. Cow milk is deficient in lenolenic acid and cholesterol which are
needed for brain growth.
High casein content leads to indigestion which results in constipation.
Allergic conditions.
Nipple confusion & refusal of breast milk. The mechanism of suckling the breast is
different from that of sucking the bottle. The child will be confused & will abandon the
suckling mechanism preferring the sucking which is easier.
Non exclusive BF for the 1st 4months increases the risk of death from diarrhea to 3.1
times and from pneumonia to 2.4 times.

49
Benefits of breast feeding
1. High nutritional value.
2. Provides immunological protection.
3. Has anti allergic properties.
4. Provides close emotional relationship.
5. Avoids dental caries.
6. Promotes normal facial development.
7. Protects against different diseases.
8. Improves speech development.
9. Promotes greater intellectual ability.
10. Provides fertility control.
11. It is cheep ,convenient, has right temp, and sterile.
Contra –indications to BF
1. Active phase to Breast Ca.
2. Inborn errors of metabolism (PKU), (glactosemia ).
3. Breast milk Jaundice which starts after 2 weeks of life, while physiological jaundice starts
after few days.
4. Sever bilateral mistitis.
5. Beta-Streptococcal infection of the infant throat.
6. Puerperal psychosis.
There are certain conditions in which BF is not contra – indicated
1. Viral infection as HBV & HIV.
2. TB when the infant receives BCG.
3. Neonatal Jaundice.
4. Prematurity & LBW.
5. New pregnancy.
6. Congenital anomalies as in cleft palate.
7. Fetal distress & hypoxia.
8. Multiple birth.
Ten steps to successful breast feeding
Every facility providing maternity & new born care services should have the following
1. Written BF policy that is routinely communicated to all health care staff.
2. Training of all health care staff in skills necessary to implement this policy.
3. Inform all pregnants about benefits & management of BF.

51
4. Helping mothers to initiate BF within half an hour after delivery.
5. Showing mothers how to BF & maintain lactation even if they should be separated from
her baby.
6. Give new born no food or drink other then breast milk unless otherwise medically
indicated.
7. The practice of rooming in i.e. allow mothers & infants to remain together 24 hrs.
8. Encourage breast feeding on demands.
9. No artificial teats or pacifiers should be used.
10. Foster the establishment of BF support groups & refer mothers to them on discharge
from hospitals.
Problems associated with breast feeding
1- Engorged & congested breast.
Causes
infant is not in correct position imperfect emptying, leads to sustained milk and congestion.
Treatment & prevention
Early initiation of BF.
Manual evacuation.
Massage & cold sponging.
Breast emptying.
2.Milk fever
This happens when the breast is filled milk is pumped back into the circulation immune
reaction. It is self-limiting.
3.Nipple pain & cracks
Causes
Only nipple is sucked.
Incorrect positioning.
Treatment & prevention
Correct position.
Do not use Antibiotic & creams.
4. Suckle refusal
Causes
Sick infant.
Premature (<2000gm) where reflexes are not developed yet.
51
Nipple confusion.
Separation of infant from his mother for several days (psychological refusal).
5. Mastitis
Causes: blocked duct & bacterial growth leads to abscess formation
Treatment
Early treatment (i.e.) before pus accumulation:
Massage.
Express milk.
Antibiotics.
Bed rest.
Open obstructed duct.
Late treatment (i.e. after pus accumulation )
Surgical.
Antibiotics.
Note: Don't stop breast feeding use the healthy breast.
When to start complementary food
When energy and nutrients are no longer sufficient i.e. age 4-6 month.
At this age the child
has a better control of his tongue
moves jaws up and down,
starts teething,
likes to put things in his mouth,
interested in new tests,

52
has more mature digestive system.
Delayed initiation of complementary food
Does not adequately fill the energy gap.
Child stop growing or grows slowly.
Increase risk of malnutrition and micronutrients deficiency.
Weaning period
It is the transitional stage when a young child’s diet gradually changes from one of milk
alone to a diet based on what the family eats .
Weaning begins when the child is introduced to food other than milk & is completed
when the child is full accustomed to the regular family diet & this period differs from
one child to another.
During weaning the child should continue breast feeding, since breast milk is an
important source of nutrition during this period.
During this period the child may be exposed to :
1- Diarrhea
Causes
Wrong food
Contaminated food.
Bad hygiene particularly during food preparation.
Bad storage of food.
Contaminated water.
2- Malnutrition
Causes
Type of food i.e. not giving the infant enough proteins and energy in the diet.
Repeated attacks of diarrhea.
When to start weaning and for how long ?
Start at 6 months of age.
Weaning can be completed at any time. between12-24 months.

53
note:
Early weaning (2 months) is wrong. It leads to diarrhea.
Late weaning (>6 months) is also wrong. It leads to malnutrition.
How to wean ?
1. Gradually by using tea spoon one time and use mashed food.
2. Initially give one meal /day & watch adaptation of the child. If there is no vomiting or
diarrhea give another meal & so on.
3. Then increase the quantity & frequency.
4. Give about 2-4 additional meals two months later.
5. Add solid food at the age of 7 months & the meals should reach 5-6 /day.
What to give to the baby?
This depends on
The traditional food usually given to the child.
What is available.
Time available to mother (preparations feeding).
Note :
1. Start with fruit juices, rice soup, vegetable soup up to the age of 6 month then add white
meat (chicken) then red meat when the child is adapting so ending up with multimix.
2. Eggs should not be given before the end of the first year (sensitivity ,contamination).
3. Honey shouldn’t be given before the end of the first year (contamination).
Conclusion
Breast feeding is important strategy for health promotion and protection of children under
fives. Since, it has many advantages against many disadvantages of bottle feeding.
