1

2

3
Part:1
Pediatric
General information
#Common CNS symptoms in pediatric:
Headache.
Abnormal body movements.
Loss of consciousness.
Mental status (ask about school performance).
Blurred vision.
Diplopia, paresthesia, numbness.
Pain.
#Abnormal body movements:
Type: describe.
Onset, duration, unilateral or bilateral.
Associated with loss of consciousness or not.
Cyanosis or not.
Aggravating and reliving factors.
Differentiate it from: breath holding attack and pseudo-epilepsy.
#Loss of consciousness:
Any fit + loss of consciousness = generalized epilepsy until proven otherwise.
Focal abnormal movement + loss of consciousness = partial epilepsy.
#No loss of consciousness:
Rigor: symptom precede the elevation of body temperature (increase muscle
contraction increase energy production increase temperature) due to any
cause like: Any Abscess, Any Sepsis, Brucellosis, Malaria.
Shivering: when you hold part of body movement stops (in fit not stop).
#Sequence of typical generalized seizure:
Aura.
Loss of consciousness.
Tonic phase.
Clonic phase.
Postictal phase (headache, confusion, amnesia, sleep)
#Headache:
Onset and duration.
Site (uni or bilateral).
4
Aggravating and reliving factors.
Associated with fever, vomiting, visual problems.
#Migraine attack:
Onset and timing.
Number of attacks per month.
Aggravating and reliving factors.
Medications.
Eating contraindicated substances.
#Other symptoms:
Diplopia: due to increased intracranial pressure for any cause.
Unilateral numbness: one limb (one hand or one leg).
Bilateral numbness: two limbs (two hands or two legs or one hand + one leg).
Symmetrical numbness: two upper limbs or two lower limbs.
Asymmetrical numbness: one hand and one leg contralaterally or ipsilaterally.
Hemiplegia: half asymmetrical.
Monoplegia: one limb.
Tetraplegia: all limbs.
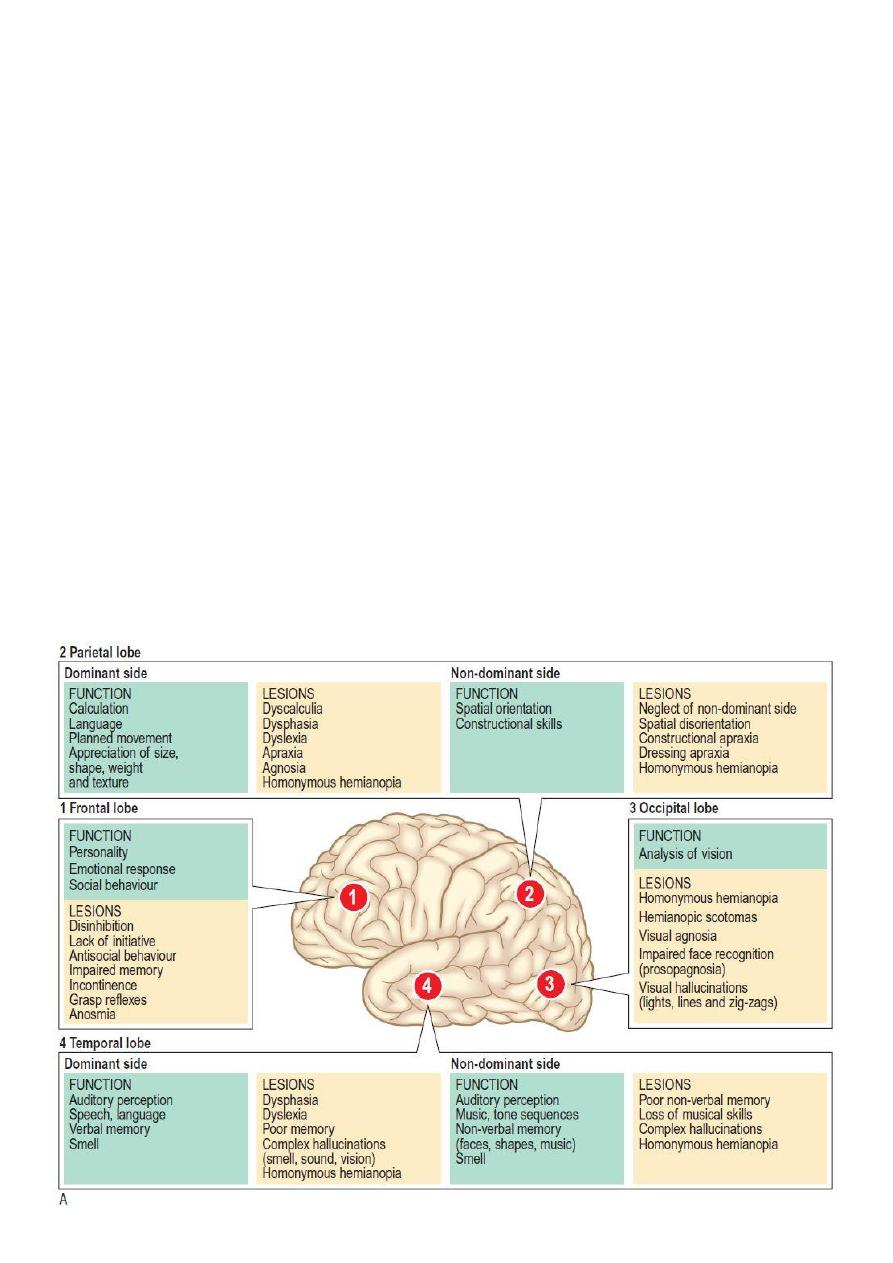
#Higher cerebral functions:

5
#Neurological exam:
Bulk of muscle of both legs: atrophy (neuropathy), hypertrophy (tumor),
pseudohypertrophy (fat deposition).
Shape of muscle.
Deforming.
Contracture.
Movement abnormality: waddling gait, stamping gait, …
Tremor: fine or course (intention tremor).
Absence of bone.
Absence of some muscles.
Joint swelling.
Examine the tone (passive movement) and power (active movement).
Reflexes: deep (knee jerk, ankle jerk) superficial (planter)
Clonus: when there is Hyperreflexia ankle and knee sustained vibration.
#Notes:
Demyelinating disease affecting both sexes at age of 20-40 years.
Multiple sclerosis is disease of white matter.
Seizure is disease of cerebral cortex.
Intention tremor is cerebellar symptom.
Causes of cataract: idiopathic, retinoblastoma, congenital rubella, galactocemia.
Bell's palsy: is benign disease due to viral infection.
Werdnig hoffman syndrome: tongue fasciculation, hypotonia, recurrent chest
infection, death after one year.
Rombergs
sign in peripheral neuropathy, B12 deficiency, tertiary syphilis.
Chicken pox may lead to cerebellitis.
Truncal ataxia is sign of vermis lesion.
Most common cause of abnormal gait is drug poisoning.
In case of bilateral lower motor neuron lesion there will be no movement (no gait).
History of CNS divided into:
o Acute: in case of meningitis, encephalitis to differentiate between them in
meningitis consciousness is present while it is absent in encephalitis.
o Subacute: in case of T.B., meningitis, sarcoidosis, leukemia, brain tumor.
o Chronic: could be progressive or non-progressive in cerebral palsy.
level of consciousness :
Seizure
Anxious (air hunger)
Irritable
"normal"
Lethargic
Delirium
Semi conscious
Coma

6
#Cerebellum signs:
Ataxia = drunken gait.
Hypotonia.
Nystagmus: vertical, horizontal, rotary // abnormal rhythmical oscillatory movement
of the eye.
Dysdidokinesia: inability of the cooperative child to perform rapid alternating
movement (pronation and supination) of the one hand over the fixed and extended
other hand.
Dysartheria (slurred speech).
Dysmetria: over shooting of finger-nose.
Intension tremor.
In-coordination.
#Cerebellum examination:
Assessment of slurred speech and dysartheria.
Dysdidokinesia ( حركة الخبا
ز
): impament of ability to make movements exhibiting a
rapid change of motion that is caused by cerebellar dysfunction.
Overshooting (dysmetria): ask child to catch something you hold (toy).
Intention tremor: detected during hand shaking.
Dysmetria: finger-nose test.
Gait: ataxia.
Co-ordination: heel-shin test (abnormal when they are unable to keep foot on shin).
#Reflexes examination:
Knee reflex appropriate exposure, tap the tendon, see the contraction of
quadriceps.
Ankle reflex appropriate exposure, tap the tendon, see the contraction of calf
muscles.
Babinski reflex one of the reflexes occur in infants, responses when body receives
certain stimulus, after sole of foot firmly stroked big toe upward and others fan
out normal in children up to 2 years and disappear as child gets older, may
disappear as early as 12 months.

7
Part:2
Pediatric
Seizure
Seizures and Epilepsy in Children
#Define the following: seizure, fit, convulsion, epilepsy.
Seizure is abnormal electrical discharge from the brain could be motor or sensory or both.
Fit=convulsion is motor seizure means there is tonic with or without clonic face.
Epilepsy is recurrent seizures.
#What is a Seizure?
Seizures are sudden events that cause temporary changes in physical movement, sensation,
behavior or consciousness. They are caused by abnormal electrical and chemical changes in
the brain.
There are many different types of seizures. Some last for only a few seconds, while others
may last a few minutes. The specific type of seizure a person has depends on where in the
brain the seizure starts, how the seizure spreads and how much (and what part) of the
brain is involved. Seizures might include:
Loss of consciousness
Convulsions (whole body shaking)
Confusion
Brief periods of staring
A sudden feeling of fear or panic
Uncontrolled shaking of an arm or leg
Flexing, stiffening, jerking, or twitching of the upper body
Nodding of the head
#What is Epilepsy?
The term epilepsy is used to describe seizures that occur repeatedly over time without an
acute illness (like fever) or an acute brain injury. Sometimes, the cause of the recurring
seizures is known (symptomatic epilepsy), and sometimes it is not (idiopathic epilepsy).
A doctor would likely diagnose a child with epilepsy if the following were true:
The child has had one or more unprovoked seizures.
The doctor thinks the child is likely to have a seizure again
The child's seizures are not directly caused by another medical condition, like
diabetes, a severe infection or an acute brain injury.
#Other Disorders That Can Look Like Seizures:
Some children experience sudden episodes that might masquerade or imitate seizures, but
are really not. Examples include:

8
Breath holding
Fainting(syncope)
Facial or body twitching (myoclonus)
Sleep disorders (night terrors, sleepwalking, and cataplexy)
They may occur just once or may recur over a limited time period. Again, although these
episodes may resemble epilepsy, they are not, and they require quite different diagnostic
tests and treatment.
#Notes:
o Fit: generalized tonic clonic convulsion.
o Tonic: spastic / Clonic: movement.
o Convulsion can occur in neonate due to electrolyte disturbance like hypoglycemia,
hypocalcaemia.
o Fit in neonate is different from that in adult, in neonate it is not always pathological,
partial convulsion may be due to electrolyte disturbance, generalized convulsion
always pathological.
o Timing of convulsion is important because it cause anoxia to the brain (no O2 reaching
the brain) so the time of fit determine the extent of injury to baby's brain.
o Febrile convulsion is benign, it occur in the beginning of fever not in the peak of fever.
o Note baby at early time of fever and give him anti-pyretic to avoid febrile convulsion.
o Baby at convulsion may bite his tongue, so put the baby at semi-position + extension to
avoid aspiration.
o Witness is important in giving right history.
#At emergency room give:
IV line.
Give O2: if the baby still having convulsion, to avoid brain anoxia.
Semi-position, extension.
Give diazepam (short acting) lorazepam 0.3 mg/ Kg.
If fit continue give him another dose of diazepam or lorazepam after 5 min and
continue giving O2.
If there is response, give baby drug at maintenance dose (Phenobarbiton 7 mg/Kg as
infusion) and do investigations.
If there is no response after 5 min also give diazepam 0.3 mg/Kg, after 5 min if there
is no response give another dose.
Give loading dose of phenobarbitone 15 mg/Kg if there is no response occur give 7
mg/Kg.
If generalized tonic clonic convulsion continued after giving these drugs give baby
glucose.
9
Part:3
Pediatric
Cranial nerves
#Examination of the cranial nerves
Start by general exam for example: the baby is conscious alert (small child) or oriented
(older child), normal posture or lying supine or in the lab of his/her mother, no sequent, no
nystagmus, no fascial asymmetry, no deformity.
#Olfactory nerve (I):
Function: Smell.
Anatomy: It starts as small nerves in the upper part of the nasal cavity passes upward
through the cribriform palate, then these small nerves converge together to form the
olfactory nerve which pass to the frontal lobe (area of olfaction), and has no nucleus.
Examination:
1-Exam each nostril separately
2-You should confirm that the nostril is patent (Rhinitis (increased secretion), foreign
body obstructing the nostril interfere with smell)
3-Bring familial odors as apple or tea or others in tubes specific for smell examination
4-Never use irritant smell because its sensed by the ophthalmic division of the V
cranial nerve not olfactory nerve.
Causes of Anosmia or parasomia:
1-Rhinitis
2-Foregin body
3-Subfrontal tumor
4-Fracture to the base of the skull or fracture in the nose.
5-Aging (don’t mention in pediatrics!)
11
#Optic nerve (II):
Function: Vision
Anatomy: It starts from the optic disc then form the optic nerve passes posteriorly
and form optic chiasma with contralateral optic nerve, from optic chiasma optic
tracts emerge (right and left) passes posteriorly to enter into the lateral geniculate
nucleus from the later optic radiation(right and left) emerge which ends into the
primary visual cortex in the occipital lobe.
Examination: It has five components to be examined:
1-Visual acuity:
Above 4 months you can use Fixation and follow test, this done by holding an
interesting toy about one meter in front of the baby, once baby fixes his vision to it,
you start to move it in an arc, if the baby follow it, consider that this baby has normal
vision.
Below 4 months, the baby can follow faces and light only.
Above 7 years (cooperative child), we can use Snellen chart
Sometimes Allen’s chart (pics of animals with different sizes) can be used below 7
years.
2-Visual field (in cooperative child):
One meter distance between doctor and baby then the doctor closes one eye by his
hand and the child asked to close the eye opposite to the doctor eye, then the doctor
start to test upper, lower and right and left fields of each eye separately by
comparing with his eye considering that the doctor has normal visual fields.
3-Color vision: (in cooperative and old child):
This can be tested by using Ishihara test, which consist of book containing different
figures with different colors, and the child is asked about these figures (considering
that the child knowing these figures e.g. numbers, pictures etc.)
4-Fundoscopy:
Right hand fundoscopy right hand and right eye.
Left hand fundoscopy left hand and left eye.
In small child this can be done only under general anesthesia.
In old cooperative child you can do it easily.
Purpose is to examine the optic disc for papilledema.
Causes of papilledema: high intracranial pressure, hemangioma, mass, hemorrhage.
5-Pupillary reflex:
Optic nerve form the sensory (afferent) part of this reflex, while the motor (efferent)
part is oculomotor (will be discussed next)
Abnormalities in optic nerve function occurs due to:
1-Optic neuritis
2-Brain tumor
3-Retinoblastoma
4-Chronic papilledema (chronic increase in intracranial pressure)
5-Pituitary tumors (mainly in adults, don’t mention in pediatrics)
11
#Oculomotor, trochlear and abducent (III, IV, and VI):
Function: Eye movement, Accommodation and pupillary reflex.
Anatomy: 3rd and 4th CN originates from the midbrain, while 6th CN originates from
the pons.
Examination: These nerves should be examined simultaneously, their examination
consist of three components:
1-Eyeball movement:
One meter between the child and examiner:
1-In small child move an interesting toy in H shape pattern and look at the child if he
follow the toy by his eyes, in the same time you should look for sequent and
nystagmus with each movement.
2-In older cooperative child you can move your finger or any object in H shape
pattern and asking him/her to follow, in every movement you should look for
sequent and nystagmus and ask about diplopia.
2-Accommodation:
1-In small child, move an interesting toy toward the nose, normally there will be
ptosis, conversion and meiosis of both eyes.
2-In older child, you can move your finger or any other object same as above.
3-Pupillary reflex:
Afferent: optic nerve
Efferent: Oculomotor nerve
This test has two parts:
1-Direct: By using light torch, come out of the visual field and direct the light toward
the pupil, normally the pupil size will decrease
2-Indirect (consensual): the same maneuver but this time you put a barrier between
the two eyes, then direct the torch toward one eye and look at the other eye for
pupil constriction (normal consensual reflex).
Abnormalities and interpretations of pupillary reflex:
If the direct reflex was negative, put barrier and direct the light torch toward the eye
again (which had negative direct reflex), and look for the contralateral eye if there is
pupil constriction (consensual reflex +) means that the optic nerve of the eye
examined first is intact, but the lesion is in the oculomotor nerve of that side, but if
the consensual reflex is also negative, means that the lesion in the optic nerve of that
eye!
Notes:
Types of squint: diversion squint and conversion squint.
Diplopia: as patient looks downward like step down a ladder.
Dilated pupil atropine // no reaction cataract or blindness.
3th cranial nerve lesion lead to upward diversion squint + ptosis + lack of
accommodation (mydriasis) + lacrimation also affected.
12
#Trigeminal nerve (V):
Function: motor, sensory, reflexes.
1-Motor: supply the muscles of mastication by the motor fibers of the mandibular
division which includes:
a-Masseter muscle, temporalis muscle: closing the mouth (clenching the mouth)
b-Lateral ptrygoid muscles: open the mouth and moving the lower jaw from side to
side (lesion in the nerve causes deviation of the jaw toward it).
2-Sensory: Supply the skin of the face by the three division as follow:
a-Ophthalmic; supply the skin above the imaginary line that runs from the middle of
cranium downward to the lateral angle of the eye.
b-Maxillary; supply the skin below the imaginary line as described above and above
an imaginary line from anterior third of the lateral part of the cranium to the angle of
the mouth.
c-Mandibular: supply the skin below the imaginary line as described in b.
3-Reflexes:
a-Corneal reflex:
Afferent: Ophthalmic division of trigeminal.
Efferent: Branch from fascial nerve causes blinking of the eye.
Two ways of examination:
1-Blowing on the child eye (usually not done due to risk of transmit infection to child
as respiratory infection) its positive when the child blink his eyes.
2-By using cotton, bring it out of the field of the child and touch rapidly the
corneoscleral junction, positive when the child blink his eye(also not done due to risk
of corneal ulceration)
b-Jaw jerk:
Afferent: 5th CN mandibular division.
Efferent; 5th CN mandibular division.
Ask the child to slightly open his mouth, put your index finger on the the chin and by
taping it by the hummer, you will notice slight or no upward movement of the jaw
normally, while brisk upward movement seen in upper motor neuron lesion.
Anatomy: Its nucleus in the pons.
#Facial nerve (VII):
Function: motor supply for fascial muscles and sensation of taste of the anterior two
thirds of the tongue.
Anatomy: nucleus in the pons.
Examination: In fascial nerve you should examine 3 components:
1-Motor: fascial muscles (4 muscles which are; frontalis, orbicularis oculi, cheek
muscles and orbicularis oris) and this done as follow:
a-Ask the child to look upward while fixing his neck in normal anatomical position,
check for forehead wrinkles bilaterally
b-Ask the child to close his eyes as much as he can till the eyebrow is buried, then try
to open his eyes by your hands to check for resistance.
13
c-Ask the child to blow against closed mouth, also check the resistance by pushing his
cheeks with your fingers
d-Ask the child to smile, look for the angle of the mouth if they are normal or there is
mouth deviation.
If there is a lesion in the right fascial nerve, the mouth will be deviated toward the
normal side.
All muscles affected in upper motor neuron lesion, while only cheek muscles and
orbicularis oris muscles are affected in lower motor neuron lesion, because the upper
two muscles supplied by nerve fibers that come from the upper half of fascial
nucleus, and the lower two muscles supplied by nerve fibers that originate from the
lower half of fascial nucleus, the upper half has innervation from both cerebral
hemispheres therefore when the fibers come from one hemisphere affected, the
branched from the other side will take its place, while lower half of the nucleus take
innervation only from the ipsilateral hemisphere, therefore when its fibers damaged
nothing take its place!
2-Sensory: it takes taste sensation of the anterior two thirds of the tongue by its
sensory branch, chorda tympani.
To examine this typically the tongue should be pulled by forceps out of the mouth,
and then put drops of specific taste on its specific are of sensation (sweet on the
anterior part of the tongue, salty and sour on the lateral side and biter on the
posterior part of the tongue)
#Note: Ramzi Hunt syndrome, its herpes zoster of the sensory part of the fascial
nerve of part of the external auditory canal.
Note:
o Glabellar reflex: elicited by repetitive tapping on the glabella (area on the
forehead between the eyes) normally person blinks in response to several tapes
then no response, if persistent cerebral palsy (abnormal) Myerson's sign.
o Facial nerve palsy:
Upper motor neuron lesion: only lower part affected (toward lesion).
Lower motor neuron lesion: Bell's palsy, all sites of face, no wrinkling, deviation of
mouth toward same side.
#Vestibulcohlear nerve (VIII):
Function: Hearing and balance
Anatomy: Pons
Examination: You should examine two component in this nerve:
1-Hearing:
a-Audiometery; it’s a device that needs cooperative child > 5 years
b-Tunic fork; used in children > 5 years, also needs cooperative child.
c-Distraction test; could be used in babies > 4 months, this can be done by two
examiners one stand infront of the child having an interesting toy in his hand and the
other examiner stand behind the baby, when the child fixes his vision to the toy in
14
front of him/her, the examiners behind will produce a sound, if the child turn his
head toward him, means his hearing is ok.
2-Balance:
a-Nystagmus: there are 3 types, transverse, vertical and arc movement.
You can examine for it by two methods:
1-Water caloric test:
a-warm water (44C and above) introduced in the external auditory canal, head will
turn to the ipsilateral side, both eyes will turn toward contralateral side with
horizontal nystagmus toward the ipsilateral ear.
b-Cold water (30 C or below) introduced in the external auditory canal, head will turn
to the contralateral side, both eyes will turn toward the ipsilateral side with
horizontal nystagmus toward the contralateral ear.
2-Hallpike test; Check Macleods for further information
b-Ataxia: Incoordination of body movement.
#Glossopharyngeal and vagus nerves (IX and X):
Function: supply muscles of swallowing, laryngeal muscles (voice production), taste
and general sensation of the posterior two third of the tongue.
Anatomy: nucleus in the medulla oblongata
Glossopharyngeal; mainly sensory, while Vagus mainly motor.
Examination: You should examine these nerves together and start as follow:
1-The Uvula, should be central, if there is lesion in one side the uvula should deviated
to the normal side. Ask the baby to say Ahh to demonstrate the uvula clearly.
2-Gag reflex; by touching the posterior wall of the pharynx by tongue depressor
(afferent by glossopharyngeal), this will cause contration of the pharyngeal muscles
(efferent by vagus nerve), this reflex induces sense of vomiting.
#Accessory nerve (IX):
Function: pure motor for the sternocleidomastoid muscle and trapezius muscle.
Anatomy: its nucleus found In the medulla oblongata (cranial root).
Examination: Can be examined as follow:
1-Ask the baby to elevate or shrug his shoulder, and push against his shoulders by
your hands.
2-If the child is small, move an interesting toy in front of him from side to side to
check for sternocleidomastoid muscles
3-If the child is old and cooperative ask him to look to the side, the push his jaw by
your hand and ask him to push against your hand.

15
#Hypoglossal nerve (XII):
Function: pure motor for the muscles of the tongue
Anatomy: nucleus in the medulla
Examination: (you need cooperative child):
1-Examine the tongue in resting and look for:
a-Wasting
b-Fasciculation (fibrillation when seen on EMG, but in tongue examination we can
use both words)
2-Exmine the tongue after asking the baby to protrude his tongue out of the mouth
and look for
a-Weakness
b-Deviation (deviation is toward the abnormal side)
3-Then ask the baby to close his mouth and push his cheeks by his tongue.
#Baby during feeding uses 9 cranial nerves:
Eye to eye contact with mother by optic nerve (indirectly related).
Eye movement by 3rd, 4th and 6th cranial nerves (indirectly related).
Muscles of mastication by V CN (directly related).
Facial muscles (sucking muscles) by VII CN (directly related).
Muscles of deglutition by IX and X CNs (directly related).
Swallowing (tongue) by XII CN (directly related).
#Causes of Cranial nerves disorders:
Infection like meningitis or encephalitis.
Infarction.
Hemorrhage.
Trauma.
Tumor.
Demyelination.
Note: 10, 9, 7 cranial nerves lesion deviation toward side of lesion, the other cranial
nerves lesions deviation to the opposite of the lesion.
Note: upper motor neuron for all cranial nerves is from the origin of the nerve till the
nucleus and lower motor neuron is from the nucleus till the end of the nerve.

16

17
Part:4
Pediatric
Milestone
#Neonates (below 30 days):
Gross motor: Asymmetrical movement of the four limbs
Fine motor: Fixation of the eyes to the mother up to 90 degree
(Clinical note: because fixation of the baby eyes to the roof of the room may signify
seizure!)
Speech: Crying signify normal speech.
#Two months:
Gross motor: Same as above + head control to start to develop and complete at 4
months
Fine motor: Fixation of the baby eyes to the mother > 90 degree.
Social: Smiles responsively, and if absent may be needed to be evaluated again at 4
months, and if it is absent at 4 months it signify developmental problem.
#Four months:
Rolling over (This is more complex than walking and occurs due to axial muscles
development, when this occur the baby definitely will walk, even if delayed).
Laughs.
Sits with support.
#Six months:
Sits alone
Feed self
Hold bottle
Babbles
At this time, we can do a test known as , to check for hearing and this done
by two persons one will stand in front of the baby with a toy and the other stand
behind the baby with a toy that produce sound, if the baby looks to the person in the
back means that his hearing is normal otherwise the baby may have deafness.
#6- 9 months:
Pincer grasp
Waves bye-bye
Says Dada, Mama
#7- 11 months:
Stands

18
#8- 12 months:
Walks
#9-2.5 – 3 years:
Draws a line
Ride a tricycle
Run
Comprehensive talking ( answering your questions)
Climbing stairs
Draws a straight line
#10- 4 years:
Copies circle and may be +
#11- 5 years:
Copies a square
#12- 6 years:
Copies a triangle
#General note:
Once a child can copy square and triangle then he is ready to learn in the school.
Vision is tested by Allen’s test before 4 years, after 5 years by Snellen chart
Walking can be delayed up to 1.5 year after that is abnormal unless the child is
obese
At 2 months if no head control and no smiling this indicate significant problem
At 8 months if the baby can’t sit without support, or no palmar grasp this indicate
Significant problem
After 8 months, the child should respond to own name.
Up to 1.5 years if no pincer grasp or no walking, indicate significant problem.
Sitting with support means that the child uses his hands to maintain his sitting
position.
With the development of gross motor skills, the infant is first able to control his or
her posture, then proximal musculature, and lastly distal musculature.
Stranger anxiety develops between 9 and 18 months of age, when infants normally
become insecure about separation from the primary caregiver.
