Genetic of cancer
Cancer is not a single disease but a diverse group of conditions that all share in common an increase in cell numbers within particular tissues. Cancers can either be benign (where the cancer fails to spread to other tissues and is, in most cases, non-life threatening) or malignant (where the cancer is invasive and spreads to other tissues within the body). Cancers can arise from practically any tissue in the body but are most commonly found to occur in epithelia—the sheets of cells that form the upper layer of the skin and that line the walls of cavities and tubes within the body. Cancers that arise from epithelia are called carcinomas and these tumors are responsible for more than 80% of all cancer-related deaths in the Western world.Genetic Changes and Cancer
Cancer is a genetic disease—that is, cancer is caused by certain changes to genes that control the way our cells function, especially how they grow and divide. These changes include mutations in the DNA that makes up our genes. Genetic changes that increase cancer risk can be inherited from our parents if the changes are present in germ cells, which are the reproductive cells of the body (eggs and sperm). Such changes, called germline changes, are found in every cell of the offspring. Cancer-causing genetic changes can also be acquired during one’s lifetime, as the result of errors that occur as cells divide during a person’s lifetime or exposure to substances, such as certain chemicals in tobacco smoke, and radiation, such as ultraviolet rays from the sun, that damage DNA.Genetic changes that occur after conception are called somatic (or acquired) changes. They can arise at any time during a person’s life. The number of cells in the body that carry such changes depends on when the changes occur during a person’s lifetime. In general, cancer cells have more genetic changes than normal cells. But each person’s cancer has a unique combination of genetic alterations. Some of these changes may be the result of cancer, rather than the cause. As the cancer continues to grow, additional changes will occur. Even within the same tumor, cancer cells may have different genetic changes.
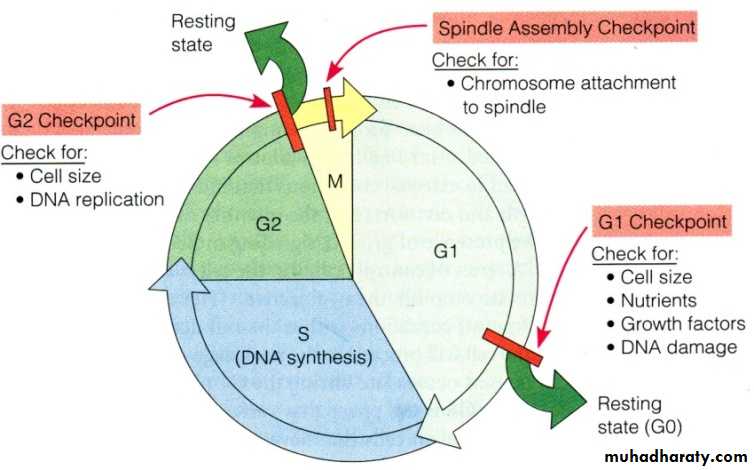
Check Points in the Cell Cycle
The cell cycle is a highly regulated process with many proteins including proto-oncogenes, tumor suppressor genes among others to regulate the cycle from one stage to the next. There are 3 checkpoints that take place in the cell cycle to prevent the cell from progressing to the next stage when it is not allowed. These checkpoints include; G1, G2 and a spindle checkpoint in Mitosis. The check point in G1 checks the DNA for any damaged bases and prevents the coping of the DNA if these bases are not fixed. The check point then allows for proper mechanisms to go through and fix those mutations in the genome. When these damaged bases are fixed the cell can then progress onto the S phase where the DNA actually replicates. In the G2 checkpoint, DNA is checked for unreplicated or damaged DNA. This checkpoint also checks for breaks in the DNA and allows for the repairment of those breaks. If these breaks are not repaired and the cell proceeds to mitosis then the broken portion of the chromosomes will not separate properly since it is not physically attached to the centromere and will not pulled by the spindles to its respective side. This checkpoint inhibits the progression of mitosis until DNA replication is completed. Arrest in the cell cycle is caused in the G1 and G2 phase by the P53 protein (which is a tumor suppressor gene). P53which is a transcription factor that then stimulates the expression of P21. P21 is a Cyclin-Kinase inhibitor that binds to and inhibits all Cdk-Cyclin complexes. This causes arrest in G1 and G2 phase. If the damage to the genome is extensive and cannot be repaired, P 53 can also activate genes that code of apoptosis, or cell death. The spindle assembly checkpoint checks for whether the prerequisites have been met for chromosomes segregation, and therefore determines whether the chromosome segregation should take place orbe delayed.
Hereditary Cancer Syndromes
Inherited genetic mutations play a major role in about 5 to 10 percent of all cancers. Researchers have associated mutations in specific genes with more than 50 hereditary cancer syndromes, which are disorders that may predispose individuals to developing certain cancers.Genetic tests can tell whether a person from a family that shows signs of such a syndrome has one of these mutations. These tests can also show whether family members without obvious disease have inherited the same mutation as a family member who carries a cancer-associated mutation. Many experts recommend that genetic testing for cancer risk be considered when someone has a personal or family history that suggests an inherited cancer risk condition, as long as the test results can be adequately interpreted (that is, they can clearly tell whether a specific genetic change is present or absent) and when the results provide information that will help guide a person’s future medical care.
Cancers that are not caused by inherited genetic mutations can sometimes appear to “run in families.” For example, a shared environment or lifestyle, such as tobacco use, can cause similar cancers to develop among family members. However, certain patterns in a family—such as the types of cancer that develop, other non-cancer conditions that are seen, and the ages at which cancer develops—may suggest the presence of a hereditary cancer syndrome. Even if a cancer-predisposing mutation is present in a family, not everyone who inherits the mutation will necessarily develop cancer. Several factors influence the outcome in a given person with the mutation, including the pattern of inheritance of the cancer syndrome.Here are examples of genes that can play a role in hereditary cancer syndromes.
The most commonly mutated gene in all cancers is TP53, which produces a protein that suppresses the growth of tumors. In addition, germline mutations in this gene can cause Li-Fraumeni syndrome, a rare, inherited disorder that leads to a higher risk of developing certain cancers.
Inherited mutations in the BRCA1 and BRCA2 genes are associated with hereditary breast and ovarian cancer syndrome, which is a disorder marked by an increased lifetime risk of breast and ovarian cancers in women. Several other cancers have been associated with this syndrome, including pancreatic and prostate cancers, as well as male breast cancer.
Another gene that produces a tumor suppressor protein is PTEN. Mutations in this gene are associated with Cowden syndrome, an inherited disorder that increases the risk of breast, thyroid, endometrial, and other types of cancer.
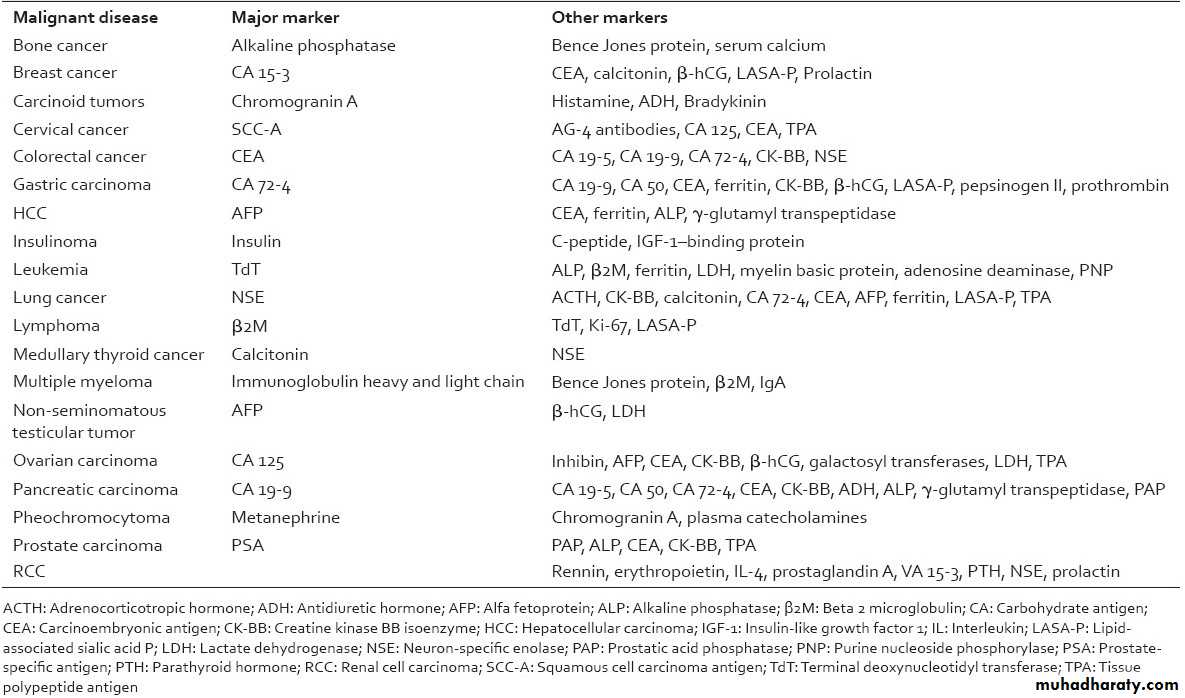
Tumor markers
A tumor marker is a substance that is produced by the body in response to cancer, or is produced by the cancer itself. Some of these markers are specific to one cancer, while others are seen in several types of cancer. These markers are generally used to evaluate the patient's response to treatment or to monitor for recurrence