MULTIPLE FETAL PREGNANCY
Contents:
A. Incidence and epidemiology.
B. Etiology of multiple fetus.
C. Types of twins:-
1. Determination of zygosity.
2. Risk of zygosity:
a) Risk of fetuses.
b) Maternal complications.
c) Problem specific to monochorionic twins.
D. Management of twins:-
1. Antenatal.
2. In labor.
MULTIPLE PREGNANCIES:-
•
consists of two or more fetuses.
•
TWINS make up the vast majority (97-98%) of multiple gestations.
•
Pregnancies with three or more fetuses are referred to as ‘higher multiples’.
Incidence and epidemiology:-
•
Rate of twins and higher-order multiple births increase by infertility therapy.
•
Increase neonatal morbidity and mortality rates.
•
Increase maternal complication with multiple gestations at least two fold.
•
Frequency of twins:-
a) Monozygotic: 1:250 (independent).
b) Dizygotic: 1:90 white USA, & 1:20 African.
c) * Depend on race, hereditary, age, parity and fertility drugs:
-
Hereditary: mother important than father.
-
Age: peak at 37 years of age.
-
Parity: increase more than six times.
-
Race: more in Caucasians & negroes.
-
Iatrogenic: drugs for ovulation induction
Etiology of multiple fetuses:-
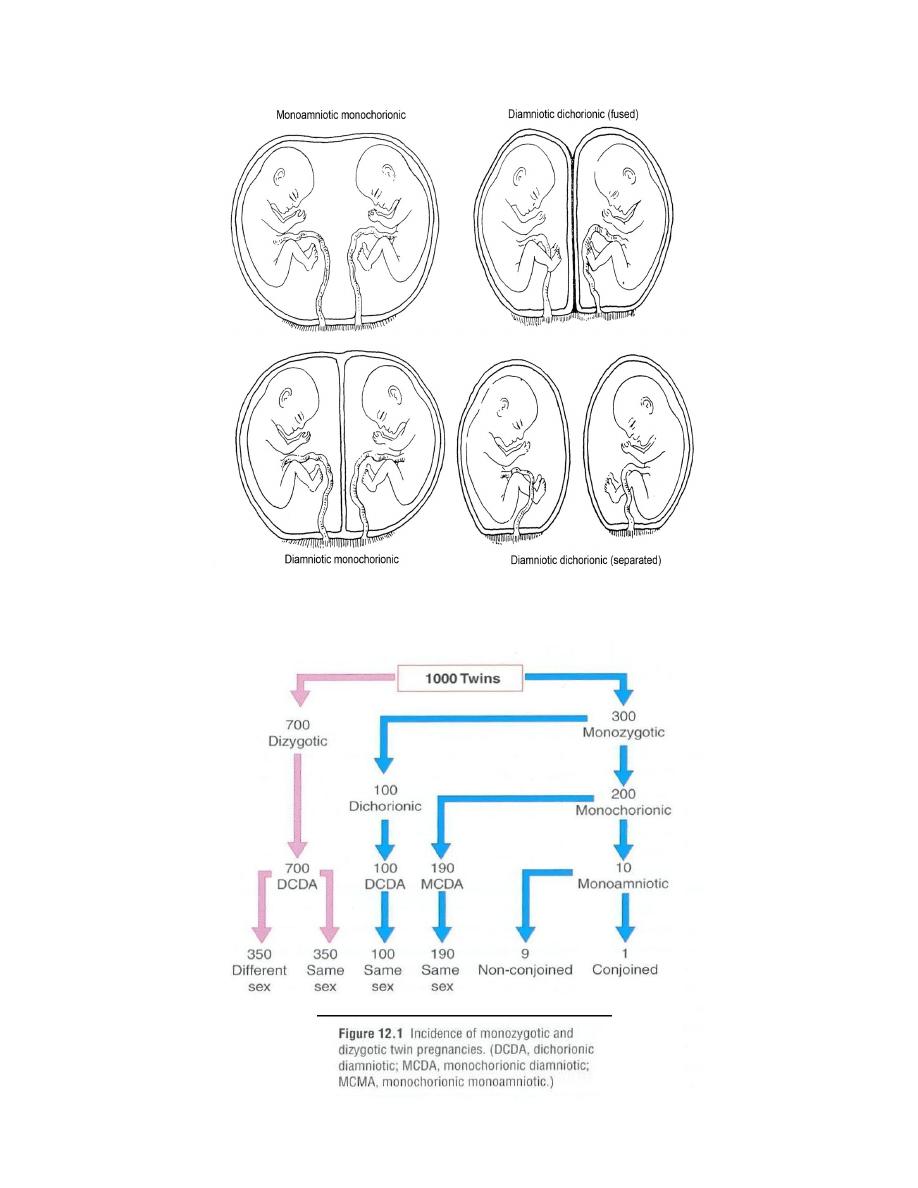
1. Dizygotic: It is a fertilization of two separate ovum.
2. Monozygotic = Identical twins: It is a single fertilized ovum that subsequently
divides into two similar structures.
Divisions:-
•
First 72 hr: two embryos, diamniotic, dichorionic and two placenta or single fused
placenta.
•
4-8 days: two embryos, diamniotic , monochorionic.
•
About 9-12 days after fertilization: two embryos, monoamniotic and monochorionic.
•
Divisions after 12 days: cleavage is incomplete and conjoined twins result.
Diagnosis of Multiple Fetuses:
1. History.
2. Clinical Examination.
3. Investigations.
A. History:-
1. Family history.
2. Advanced age.
3. High parity.
4. Large maternal size.
5. Medication.
B. Clinical Examination:-
1. Exaggerated pregnancy symptoms.
2. Late in first trimester by Doppler à two fetal hearts.
3. Uterine palpation can feel two fetal heads or multiple fetal parts.
4. Uterine size is larger than expected for the gestational age determined from
menstrual data.
•
Deferential diagnosis for large for date:-
1. Multiple fetuses.
2. Inaccurate menstrual history.
3. Hydramnios.
4. Hydatidiform mole.
5. Elevation of the uterus by distended bladder.
6. Uterine myomas.
7. A closely attached adnexal mass.
8. Fetal macrosomia (late in pregnancy).
C. Investigations:-
1. Ultrasonograghic examination.
à separated gestational sacs in early pregnancy.
2. Radiological.
3. Biochemical tests.
a) chorionic gonadotropin in plasma and in urine.
b) alpha fetoprotein level (alone is not diagnostic).
Complications of Multiple Gestation:-
A. Maternal:-
1. Anemia, Hydramnios, Preeclampsia, Preterm labour, Postpartum
hemorrhage, Cesarean delivery.
B. Fetal:-
1. Malpresentation, Placenta previa, Abruptio placentae, Premature rupture of
the membranes, Prematurity, Umbilical cord prolapsed, Intrauterine growth
restriction, Congenital anomalies.

Risk of Multiple Fetal Pregnancy:-
A. Abortion:-
•
Increase spontaneous abortion more
than three times.
B. Malformation:-
•
Congenital malformation > single
C. Low birth weight:-
1. growth restriction (estimated fetal weight less than 10th percentile for
singleton gestation).
2. preterm.
3. discordance (difference in estimated fetal weight of greater than 20%-25%
between twin A and twin B).
D. Decrease duration of gestation:-
1. 57% of twins à at 35 weeks.
2. 92% of triplets à at 32 weeks.
3. all quadruplets à at 29–30 weeks
E. Preterm birth:-
1. It is the most common complication of multiple pregnancies effecting long
term out come.
2. prophylactic use of Tocolytics , Bed rest , Cerclage.
3. fetal fibronectin (at 24-28 weeks if high associated with increase risk of
preterm before 32 weeks of gestation).
F. Intrauterine fetal demise of one twin (late pregnancy), Vanishing twin (early
pregnancy).
Maternal Complication:
1. Acute fatty liver.
2. Anemia.
3. Abnormal placentation.
4. Amniotic fluid volume abnormalities.
5. Preeclampsia.
6. Operative vaginal delivery and C-section.
7. Premature rupture of membrane.
8. Postpartum hemorrhage.
9. Umbilical cord prolapse.
Problems Specific to Monochorionic twins:-
"Twin-Twin transfusion syndrome":-
•
15% of monochorionic develops.
•
Early onset often is associated with poor prognosis.
•
Twin-Twin transfusion can be acute or chronic.
•
The net effect of blood flow imbalance result:
-
donor:- small, hypoperfused, anemic.
-
recipient:- large, hyperperfused.

Problems for Monoamnionicity:
•
Rare < 1% .
•
Mortality 20-50%.
•
Cord entanglement.
•
Perinatal mortality.
•
Preterm Delivery.
•
Growth restriction.
•
Congenital anomalies.
•
Conjoined twins à Siamese twins:-
-
Anterior (thoracopagus).
-
Posterior (pygopagus).
-
Cephalic (craniopagus).
-
Caudal (ischopagus).
Management:
•
Antenatal.
•
In Labor.
DIAGNOSIS OF MULTIPLE PREGNANCY:-
•
+ve family history mainly on maternal side.
•
+ve history of ovulation induction.
•
Exaggerated symptoms of pregnancy.
•
Marked edema of lower limb.
•
Discrepancy between date and uterine size.
•
Palpation of many fetal parts.
•
Auscultation of two fetal heart beats at two different sites with a difference of 10
beats
•
USS:-
-
Two sacs by 5 weeks by TV USS.
-
Two embryos by 7 weeks by TV USS.
"Antenatal Care"
A. AIM:-
1. Prolongation of gestation age, increase fetal weight.
2. Improve PNM and morbidity.
3. Decrease incidence of maternal complications.
B. Follow Up:-
1. Every two weeks.
2. Iron and folic acid to avoid anemia.
3. Assess cervical length and competency.
C. Fetal Surveillance:-
1. Monthly USS.from 24 weeks to assess fetal growth and weight.
2. A discordinate weight difference of >25% is abnormal (IUGR).
3. Weekly CTG from 36 weeks.
D. Determination of zygosity:-
1. Very important as most of the complications occur in monochorionic
monozygotic twins.

2. During pregnancy by USS:-
a) Very accurate in the first trimester, two sacs, presence of thick chorion
between amniotic memb.
b) Less accurate in the second trimester the chorion become thin and fuse
with the amniotic memb.
c) Different sex indicates dizygotic twins.
d) Separate placentas indicates dizygotic twins
"Antenatal Management"
•
Early diagnosis (mainly by ultrasound).
•
Adequate nutrition:-
-
Caloric consumption increased by 300 Kcal per day.
-
Iron 60-100 mg per day.
-
Folic acid 1mg per day.
•
Frequent prenatal visit:-
observe maternal and fetal complications:-
-
Frequent ultra sound à fetal growth, congenital anomalies, amniotic fluid.
-
Doppler.
-
BPP.
•
Routine antenatal care for all women involves screening for hypertension and
gestational diabetes.
•
These conditions occur more frequently in twin pregnancies and there is also a
higher risk of other problems (such as antepartum haemorrhage and
thromboembolic disease).
INTRAUTERINE DEATH OF ONE TWIN:
•
Early in pregnancy: usually no risk.
•
In 2nd or 3rd trimester:
-
Increase risk of DIC.
-
Increase risk of thrombosis in the a live one.
-
The risk is much higher in monochorionic than in dichorionic twins.
-
The a life baby should be delivered by 32-34 weeks in monochorionic twins.
HIGHER MULTIPLE GESTATION:
•
Spontaneous triplets 1:8000 births.
•
Spontaneous quadruplets 1:700,000 births.
•
The main risk is sever prematurity .
•
CS is the usual and safe mode of delivary.
•
High PNMR of 50-100 / 1000 births
•
Presentation:-
-
Cephalic - Cephalic 42%
-
Cephalic - Breech 27%
-
Cephalic - Transverse 18%
-
Breech - Breech 5%
-
Other 8%

MONITORING OF FETAL GROWTH & WELL-BEING:-
•
Monitoring for fetal growth and well-being in twins is principally by ultrasound scan.
•
Each assessment should include fetal measurement, fetal activity, fetal lies and
amniotic fluid volumes.
•
In monochorionic twins, features of TTTS should be sought, including discordaces
between fetal size, fetal activity, amniotic fluid volumes.
•
Doppler assessment of the fetal circulations and cardiotocography (CTG).
Threatened preterm labour:-
•
Antenatal strategies in those identified as at high risk may include screening for
bacterial vaginosis (treatment may eliminate a co-factor for spontaneous preterm
labour), screening for group B Streptococcus (GBS; intrapartum antibiotics reduce
neonatal infection), maternal steroid therapy to enhance fetal lung maturation.
•
Once preterm is diagnosed, neonatal unit staff must be promptly involved.
"Intrapartum Management":-
A. In Labor Management:-
1. Trained obstetrical attendant.
2. Available blood.
3. Good access I.V live.
4. CTG monitoring.
5. Anesthetist à ER C-S.
6. Pediatrician for each fetus.
7. Mode of delivery depend on presentation.
B. Preparation:-
1. A twin CTG machine should be used for fetal monitoring and a portable
ultrasound machine should be available during delivery.
2. A standard oxytocin solution for augmentation should be prepared, run
through an intravenous giving-set and clearly labelled ‘for augmentation’, for
use for delivery of the second twin, if required.
3. A second high-dose oxytocin infusion should also be available for the
management of postpartum hemorrhage.
4. It is essential that two neonatal resuscitation trolleys, and two pediatricians
are available and that the special care baby unit and anesthetist are informed
well in advance of the delivery.
C. Twin Delivery:-
•
Analgesia during labour.Epidural analgesia is recommended.
•
Fetal well-being in labour.
-
Fetal heart rate monitoring should be continuous throughout labour.
-
An abnormal fetal heart rate pattern in twin I may be assessed using fetal
scalp sampling, as for a singleton pregnancy.
-
However, a non-reassuring pattern in twin 2 will usually necessitate delivery by
Caesarean section.
-
The condition of twin 1, as acute complications such as cord prolapse and
placental separation are well recognized.

-
Delivery of the first twin is undertaken in the usual manner and thereafter the
majority of second twins will be delivered within 15 minutes.
-
After the delivery of the first twin, abdominal palpitation should be performed to
assess the lie of the second twin.
-
It is helpful to use ultrasound for confirmation, which is also useful for checking
the fetal heart rate.
-
If the lie is longitudinal with a cephalic presentation, one should wait until the
head is descending and then perform amniotomy with a contraction.
-
If contractions do not ensue within 5-15minutes after delivery of the first twin,
an oxytocin infusion should be started, out let forceps and vacuum extraction
can be used.
-
IF second twin transverse or oblique presentation, we can perform external
cephalic version or breech extraction with or without internal podalic version.
-
Continue oxytocin drip &give ergometrine to avoid risk of PPH,handle both
cords deliver them by controlled cord traction method.
•
Delivery of vertex-non-vertex:-
-
Non-vertex first twin
-
When twin 1 presentation as a breech, clinicians usually recommend delivery
by elective Caesarean section.
-
Other factors include dwindling experience of breech delivery and the rarely
seen phenomenon of ‘locked twins’.
•
Internal podalic version;-
-
superior or posterior. If the back is inferior or if the limbs are not imnuediately
palpable, ultrasound may help to show the operator where they would be
found. This will rninirnize the unwanted experience
