1
Lec-1 Surgery
د.زيد
Head injury
Introduction:
Traumatic brain injury remain the leading cause of death and long term disability in people
younger than 40 years .
EPIDEMIOLOGY:
Traumatic brain injury will surpass many diseases as the major cause of death and disability
by the year 2020.
it is the third leading cause of death preceded by cardio-cerebral vascular disease and
cancer.
mortality rate range from 6-39 per 100.000.
it acounts for 3.4% of patients attending emergency department.
classification:
i.mechanistic:
1.closed
2.penetrating
3.crush
4.blast
II.clinical:(according to glascow coma scale)
3-8:severe
8-13:moderate
14-15:mild
2
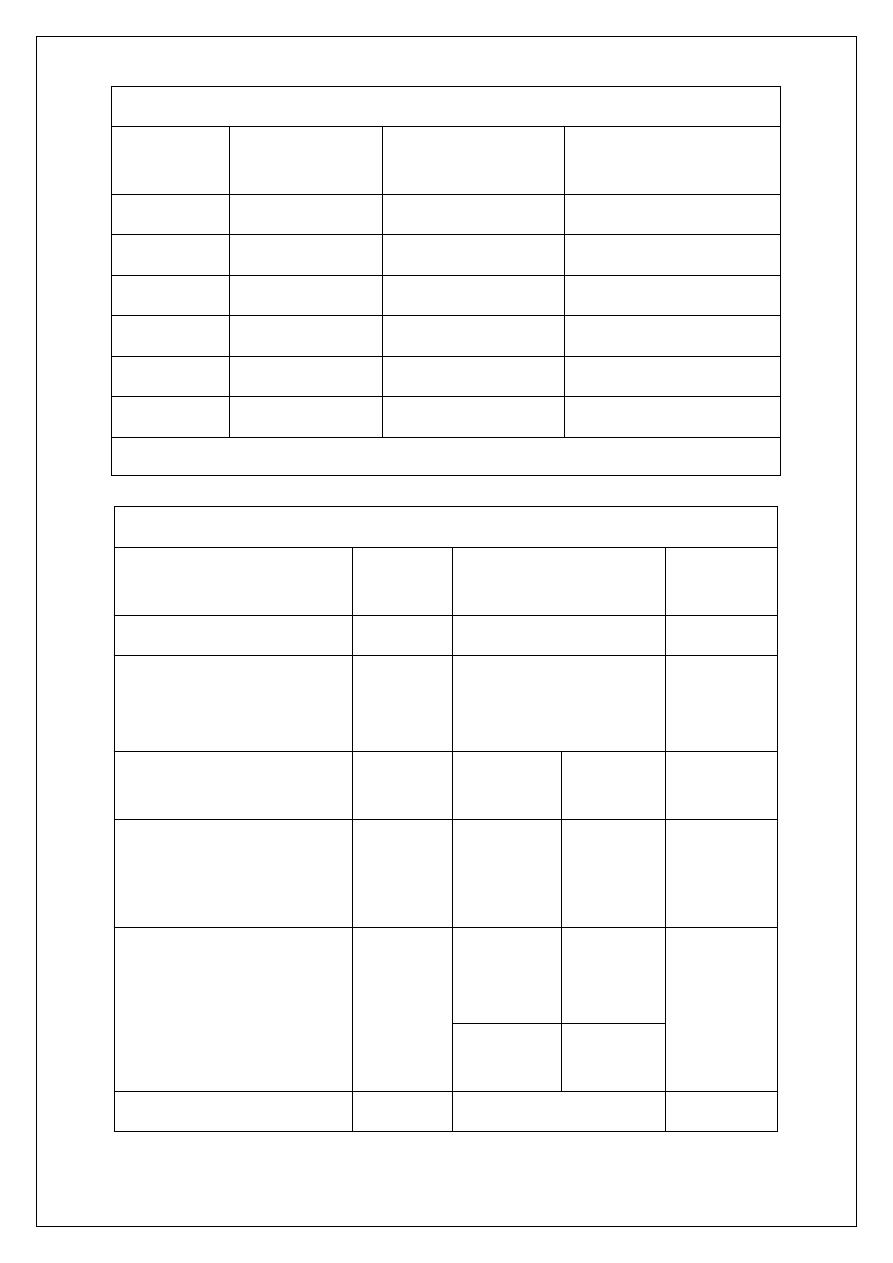
Glascow coma scale(age >4 year)
Best motor
Best verbal
Best eye
opening
points
obeys
6
Localizes pain
oriented
5
Withdraws to pain
confused
spontaneous
4
Flexion(decorticate)
Inappropriate
To speech
3
Extension(decerebrate)
Incomprehensible
To pain
2
None
None
None
1
Glascow coma scale(age <4 year))
Best motor
Best verbal
Best eye
opening
points
obeys
6
Localizes
pain
Smile,oriented to
sound,follow
object,interact
5
Withdraws
to pain
interactio
n
crying
spontane
ous
4
Flexion
(decorticat
e)
inappropr
iate
consolable
To
speech
3
Extension
(decerebra
te)
moaning
Inconsiste
ntly
consolable
To pain
2
restless
inconsolab
le
None
None
None
1
3
III.ADMINISTRATIVE:
ICD9 and icd10
mechanistic causes of head injuries:
i.contact injuries:
1.linear skull fracture
2.depressed skull fracture
3.basilar skull fracture
4.epidural hematoma
5.coup contusion
6.countercoup contusion
ii.head motion(inertial):
1.translation
2.rotation
3.angular
classification of head injury according to the site of injury:
i.scalp injury
ii.skull injury
iii.brain injury
scalp injury:
1.laceration(wound)
2.hematoma
1.scalp laceration:
.most common type of injury.
.caused by sharp or blunt or blast injury.
.may give rise to severe haemorrhage if not controlled and cause shock in peadiatric group.
.it may overlie any type of fracture.
4
.wound healing is rapid but infection may occure.
.management:cleaning,suturing and dressing.
scalp hematoma:
.it may be sub galeal or sub pericranial.
.always associated with skull fracture in infants.
.the soft fluctuant center may like depressed fracture on palpation.
resolution of hematoma occure within few weeks.
.mangement:
1.observation.
2.avoid aspiration.
3.correction of anemia if occure.
skull fractures classification:
1.LINEAR FRACTURE.
2.DEPRESSED FRACTURE.
3.DIASTATIC FRACTURE.
4.PING PONG FRACTURE.
LINEAR FRACTURE:
.MAY BE CLOSED OR OPENED
.OCCURE AS ARESULT OF BLUNT TRAUMA
.REQUIRE NO SPECIFIC MANAGEMENT,ONLY 24 HOURS OBSERVATION
.MAY REQUIRE CT SCAN OF BRAIN ESPECIALLY IF OCCURE OVER SQUAMOUS TEMPORAL
BONE LEADING TO EPIDURAL HEMATOMA.
DEPRESSED FRACTURE:
. MAY BE CLOSED OR OPENED(COMPOUND).
5
.OCCURE AS ARESULT OF SHARP TRAUMA.
CLOSED DEPRESSED FRACTURE:
.RARE IN ADULTS.
.RARELY CAUSE BRAIN COMPRESSION.
.REQUIRE CT SCAN OF BRAIN.
.USUALLY CONSERVATIVE MANAGEMENT IS ENOUGH.
INDICATION FOR ELIVATION:
A.COSMETIC PURPOSES.
B.MASS EFFECT.
C.LARGE DEPRESSED PART WITH POSSIBILITY OF DURAL TEAR.
D.PREVENTION OF SECONDARY INFECTION.
COMPOUND DEPRESSED FRACTURE:
IT CAN CAUSE PROFUSE BLEEDING,CSF LEAK AND BRAIN HERNIATION THROUGH FRACTURE
SIDE.
IT IS AN INDICATION FOR SURGERY IN ORDER TO PREVENT INFECTION.
GOAL OF SURGERY:
A.REMOVAL OF FOREIGN BODIES.
B.REMOVAL OF NECROTIC TISSUES AND BONE CHIPS.
C.CLOSURE OF DURA IN WATER-TIGHT FASHION.
D.PREVENTION OF INFECTION.
COMPLICATION:
A.BRAIN PROLAPSE THROUGH DURAL TEAR LEADING TO ISCHEMIA.
B.INFECTION (OSTEOMYLITIS OR MENINGITIS).
C.EPILIPSY(EARLY OR LATE)
D.COSMETIC DEFORMITY.
E.SEVERE BLEEDING FROM ONE OF VENOUS SINUSES.
6
DIASTATIC FRACTURE:
IT IS ASEPARATED CRANIAL SUTURE.
.EITHER INVOLVE CORONAL OR LAMBDOID SUTURE.
.COMMON UNDER 3 YEARS OLD,RARELY IN ELDER AGE GROUP EXCEPT AS PART OF MORE
EXTENSIVE SKULL FRACTURE.
PING PONG FRACTURE:
IT IS ASMOOTH CONCAVE DEPRESSION DUE TO BLUNT TRAUMA TO CRANIAL VAULTAND
LOOK SIMILAR TO ADENT IN A”PING PONG”BALL.
IT IS USUALLY OCCURE IN CHILDREN.
.IT NEED NO TREATMENT IF IT IS LESS THAN 3CM IN DIAMETER BUT IT MAY NEED SURGICAL
INTERVENTION IF IT IS MORE THAN 5CM.
basilar skull fracture:
.relatively frequent.
.can be diagnosed both radiologically and some time clinically(by palpation).
.associated with csf fistula but usually seals off few days later.
.aetiology:is due to indirect violence on the vault producing deformation of skull with
compression of skull at one area and giving way or break of skull at other area,with the
base of skull being most vulnerable.
types of skull fracture:
a.anterior fossa basal fracture:
.may open into the frontal or ethmoidal air sinuses or run across the cribriform plate.
.clinical picture:
a.periorbital hematoma(racoon eye).
b.epistaxis
7
c.subconjunctival hematoma.
d.csf rhinorrhea
c.nasal tip parasthesia due to injury of first branch of trigeminal nerves.
b.middle fossa fracture:
it involve petrous temporal bone.
clinical picture:
1.csf otorrhea.
2.battle sign:bluish ciscoloration over mastoid bone.
3.haemotympanum
4.vii and viii cranial nerves palsies.
posterior fossa basal fracture:
1.swelling or bluish discoloration of suboccipital area.
2.9th,10th,11th cranial nerves at the jagular foramen.
3.retraction of head and stiffnes due to upper cervical nerves irritation.
4.management:
a.observation.
b.prophylactic antibiotics.
c.treatment of associated injuries.
indication of surgery:
1.persistance of csf leak more than two weeks.
2.presence of fracture involving frontal or ethmoidal sinuses.
3.occurrence of meningitIS
III.BRAIN INJURIES:
TYPES:
I.PRIMARY BRAIN INJURY:
8
OCCURE AT THE TIME OF INSULT{E.G.CONTUSION AND LACERATION} AND IS IRREVERSIBLE.
II.SECONDARY BRAIN INJURY:
OCCURE AT ANY TIME AFTER TIME OF INSULT AND OFTEN IS PREVENTABLE AND ITS
CAUSES ARE:
A.HYPOXIA(DECREASE SPO2)
B.HYPOTENSION(SYSTOLIC BLOOD PRESSURE LESS THAN 90 mmhg)
C.RAISED I.C.P.(MOR THAN 20 MMHG)
D.LOW CEREBRAL PERFUSION PRESSURE(CCP LESS THAN 65 MMHG)
E.PYREXIA
F.SEIZURE
G.METABOLIC CHANGES
I.PRIMARY BRAIN INJURY:
A. CEREBRAL CONCUSSION
B. DIFFUSE AXONAL INJURY
C.BRAIN STEM AND HEMISPHERIC CONTUSION
A.CEREBRAL CONCUSSION:
.IT IS THE MILDEST FORM OF BRAIN INJURY.
.DUE TO ROTATIONAL ACCELERATION OF HEAD IN THE ABSENCE OF SIGNIFICANT
MECHANICAL CONTACT.
.CLASSICALLY;TRANSIENT LOSS OF CONCIOUSNESS FOLLOWED BY RAPID RETURN TO
NORMAL STATE OF ALERTNESS.
.RECENT STUDY SHOWS THE CAUSE IS DUE TO DIFFUSE CEREBRAL HEMISPHERE
INVOLVEMENT AND BRAIN STEM LESION IS LESS COMMON.
IMAGING SHOWS SIGN OF CYTOTOXIC BRAIN EDEMA DESPITE NORMAL CT SCAN AND GCS
15.
CLINICALLY:IRRITABILITY,AMNESIA,LETHARGY,COGNITIVE
DISFUNCTION;BRADYCARDIA,HYPOTENSION AND SWEATING.
9
B.DIFFUSE AXONAL INJURY:
.it is one of most important pathological substrate producing prolonged traumatic
coma(more than 6 hours) not attritutable to mass lesion .
.caused by angular rotational acceleration leading to mechanical shearing at the grey_
white matter interface.
.it may lead to death.
c.cerebral contusion and laceration:
these are areas of bruising and swelling with intact pia_arachnoid,localized or generalized
edema and haemorrhage due to damage of small blood vessels.
.are typically surface lesion
(frontal and temporal) but occure at deeper structure of brain.
.clinical picture:different periods of unconciousness and focal neurological deficit.
.radiologically: punctate haemorrhage through brain parynchyma called ”salt on pepper”
appearance.
.can resolve compeletly from weaks to months.
.laceration differ from contusion in involvement of pia_arachnoid interface.
ii.secondary brain injury:
a.brain oedema(cerebral swelling)
b.intracranial haemorrhage.
c.infection.
d.seizure
e.hydrocephalus
f.ischemia
g.cerebral herniation
h.csf rhinorrhea
11
a.brain oedema:
.massive swelling of all or part of brain due to increased water content of brain(cerebral
oedema).
.it is vasogenic oedema or cytotoxic or both.
.osmotic oedema also can occure.
b. intracranial haemorrhage:
1.extradural haematoma
2.subdural haematoma:acute and chronic
3.intracerebral haematoma
4.subarachnoid haemorrhage
1.extradural haematoma:
.2% of traumatic head injury.
it is acollection of blood between skull and dura.
.usually caused by trivial trauma
.occure in young age group(rare below 2year and more than 60).
.source of bleeding:
-middle meningeal artery which is disrupted by tempo-parietal fracture.
-middle meningeal vein.
-dural venous sinuses.
.clinical presentation:
breif post traumatic loss of conciousness
followed by “lucid interval” for several hours
then,obtundatio,contralateral hemiparesis,ipsilateralpupillary dilatation.
deterioration usually occure sover few hours but may takes days.
radiologically;it is biconvex or lens shape.
11
it is aneurosurgical emergency evacuated by “craniotomy”
subdural haematomas:
it is acollection of blood between dura and the arachnoid and is formed by venous or rarely
arterial, blood dissects between the dura and arachnoid.
three types of sdh according to yime:
a.acute(<3 days)
b.subacute(3days-3weeks)
c.chronic(>3 weeks)
a.acute sdh:
.it is usually due to severe trauma and thus associated with poor outcome.
.sources of bleeding:
1.related to contusion or laceration
2.related to rupture of bridging veins or superficial cortical veins or dural venous sinuses.
clinically;same as that of extradural haematoma but there is persistant loss of conciousness
with no lucid interval.
radiologically;concave in shape because it takes the shape brain paranchyma.
acute subdural haematoma are rapidly evolving lesion and early evacuation is mandatory
by “craniotomy”.
c.chronic sdh :
.commonly occure in elderly people, chronic alcoholic.
.cerebral atrophy appear to be an important factor.
.caused by rupture of bridging veins after amild trauma.
.the patient present with progressive neurological deficit more than 3 weeks after trauma.
.radiologically;hypodense concave shape.
.it should be evacuated if it cause mass effect by drilling “burr holes” over the collection
and washing it using warm normal saline.
3.intra cerebral haematoma:
12
.it defined as haematomas 2 cm or larger not in contact wih the surface of brain.
.occure due to rupture of intrinsic blood vessels at time of injury or due to coalesence of
contusions.
.radiologically;hyperdense mass surrounded by perifocal oedema and sometime midline
shift.
.large haematomas should be evacuated by “craniotomy” while small haematomas can be
managed conservativly.
4.subarachnoid haemorrhage:
.it is ableeding into subarachnoi space occure in fatal head injury.
.usually managed conservativly.
c.cns infection:
it is caused by penetration of dura by trauma.
presentation:
1.meningitis
2.brain abscess
3.subdural empyemas
d.seizure:
1.immediate: at time of insult
2.early: <than 7 days
3.late: > than 7 days
e. hydrocephalus:
1.acutely due to obstruction of cef flow by blood in the ventricles.
2.delayed non obstructive type due to impaired csf resorption following traumatic
subarachnoid haemorrhage.
f.cerebral ischemia:
13
can be found in 90% of patient who survive for several hours after injury and is significantly
associated with hypoxia such as cardiac arrest,status epilipticus or raised i.c.p.
g.cerebral herniation:
1.subfalcine
2.uncal
3.tentorial
4.tonsilar
h.csf rhinorrhea:
.caused by a piece of brain tissue or bone into the dural tear prevent its healing.
management of head injury:
i.pre hospital management:
rapid removal of victim to emergency department is critical to improve the chance of
survival by preventing secondary injuries (by paramedical personnel,police man,fire service
and helicopter)
guidelines include:
1.avoid hypoxia(<90) and hypotension(<90)
2.assesment of glascow coma scale:
.it used as arelible indicator of severity and prognosis.
.obtain after securing of airway,breathin and circulation.
.obtain before using sedative or paralytic drugs.
3.pupil assesment(size and reflex):
.important in diagnosis and prognosis.
.note evidence of orbital trauma
.asses after resuscitation and stabilization
4.airway, breathing and circulation:
.using mouth gauge or endotracheal tube with umbo bag.
.monitoring of blood pressure and isotonic fluid replacement.
14
5.frequent assesment of clincal condition for any deterioration.
ii.hospital management:
1.primary survey:
a.airway
b.breathing
c.circulation
d.disability:
.asses glascow coma score
.pupillary size and response
.lateralizing sign and sign of cord injury
e.exposure:
.adequate exposure for compelet examination
.prevent hypothermia
2.secondary survey:
a.history:
.cause,mechanism and circumstances of injury
.presenc and period of loss of conciousness
.presence of headache and vomiting
.presence of seizure
.presence of post traumatic amnesia
.medical, surgical and drug history
b.examination:
.vital sign
.scalp: for any swellin or wound
.skull:for fracture
.level of conciousness by g.c.s.
15
.pupil size and response:
.lateralizing sign like hemiparesis
.signs of skull base fracture
.full neurological examination
.thorough examination of the patien for other injuries
c.indication of hospital admission:
.any loss or depression of conciousness
.persistant haedache and vomiting
.focal neurological deficit
.seizure
.those who are difficult to be assesed(intoxication or under alcohol effect)
.concomitant disease as coagulopathy
d.investigation:
1.skull x-ray:
for skull fracture or foreign body
2.cervical x-ray:
to exclude fracture or dislocation
3.ct scan of brain(indication):
high risk factors:
.failure to reach g.c.s. of 15 within 2 hours
.suspected open skull fracture
.any sign of skull base fracture
.> than 2 episode of vomiting
.age > than 65
moderate risk factors:
.amnesia before impact longer than 30 minute
.dangerous mechanism of injury
16
4.mri of brain and cerebral angiography
e.decision:
i.conservative(control of i.c.p.):
.i.c.p. should be controlled below 20 mmhg
.mannitol is osmotic diuretic and rapidly decrease i.c.p. and increase cerebral blood flow by
volume expansion and decreased blood viscosity.
.exclusion of haematoma is essential before use of mannitol.
ii.surgical intervention:
.is indicated for evacuation of haematoma as life saving.
complication of head injury:
a.neurological deficit:
this need physiotherapy,speech andoccupational therapy.
b.post traumatic seizure
c.csf fistula
d.post concussion syndrome:
headache,dizziness,impaired short memory,conccentration.easy fatigability and depression.
e.c s f fistula.
f.neuroendocrine and metabolic disorder.
glascow coma score:
good recovery 5
moderate disability 4
severe disability 3
vegetative state 2
dead 1
