1
Fifth stage
Pediatric
Lec. 3
.د
اوس
22/3/2017
Faltering growth (failure to thrive)
•
refers to not only failure of growth(suboptimal weight gain) but also impairment of
other aspects of a child’s well being. It is common in infancy
•
Other definition:: mild failure to thrive being a fall across two centile lines and severe
being a fall across three centile lines.
•
A single observation of weight is difficult to interpret unless markedly discrepant
from the head circumference or length, although the further the weight is below the
2nd centile, the more likely the child is ‘failing to thrive’. A weight below the 0.4th
centile should always trigger an evaluation
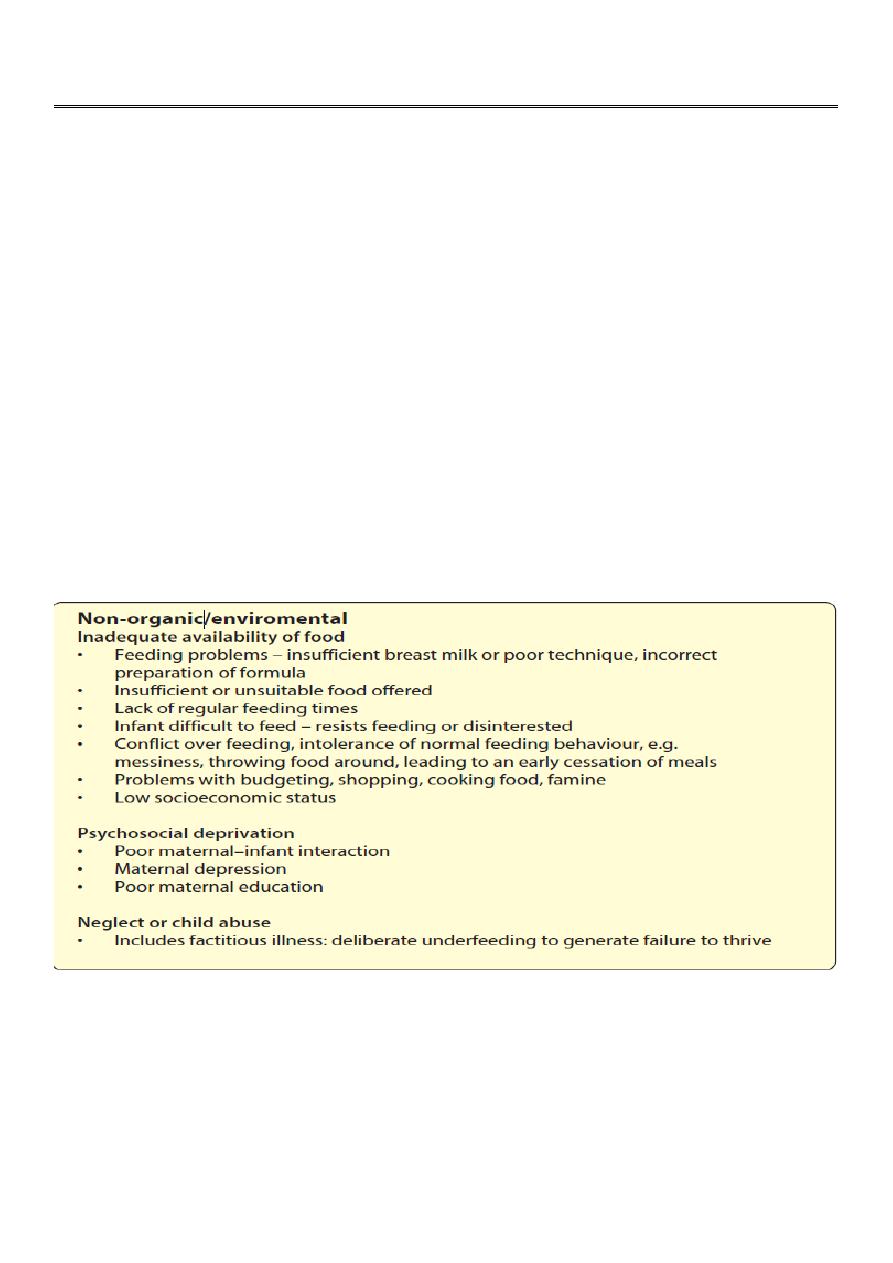
Clearly this can be organic or non-organic
2
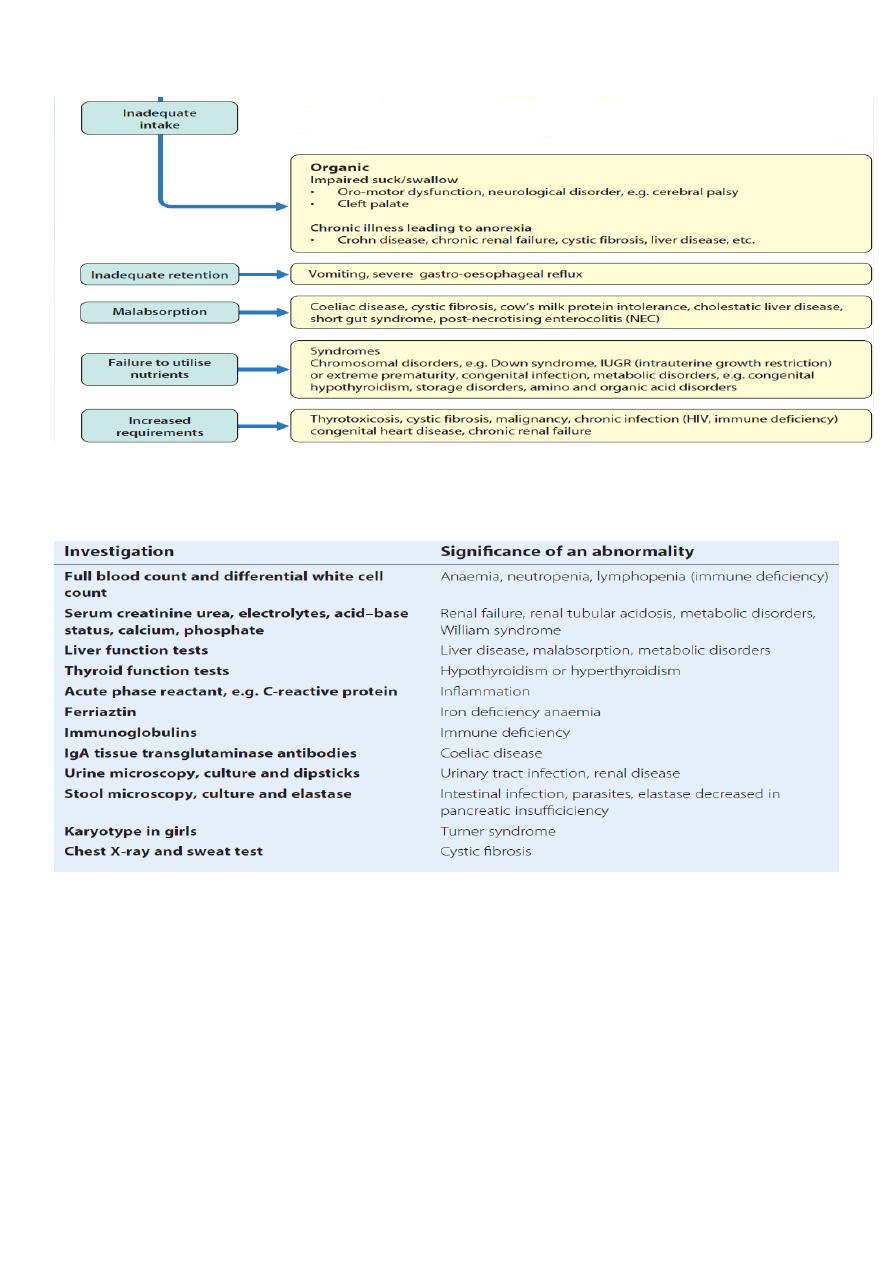
Organic causes of faltering growth
Investigations
Management
•
The management of most non-organic failure to thrive is multidisciplinary and is
carried out in primary care.
•
A pediatric dietician may be helpful in assessing the quantity and composition of food
intake, and recommending strategies for increasing energy intake and a speech and
language therapist has specialist skills with feeding disorders. Input from a clinical
psychologist and from social services may also be appropriate. Nursery placement
may be helpful in alleviating stress at home and assist with feeding.
3
•
Hospital admission is usually only necessary in children under 6 months with severe
failure to thrive, requiring active refeeding. While hospital admission may offer the
opportunity to observe and improve the mother’s method and skill in feeding, In
extreme cases, hospital admission can be used to demonstrate that the child will gain
weight when fed appropriately.
Malnutrition
•
Malnutrition is a global problem that varies from under nutrition to over nutrition. It
has been defined as failure of the body to obtain the appropriate amount of proteins,
energy, vitamins and other nutrients it needs to maintain healthy tissue and organ
function
•
Worldwide, malnutrition is common and is responsible directly or indirectly for about
a third of all deaths of children under 5 years of age
Consequences Of malnutrition
The multisystem consequences of undernutrition include:
1- Growth failure
2- Impaired gastrointestinal function
3- Immunodeficiency
4- Respiratory dysfunction
5- Myocardial dysfunction
4
6- Increased operative morbidity/mortality
7- Delayed wound healing
8-Impaired intellectual development
9-Altered behavior
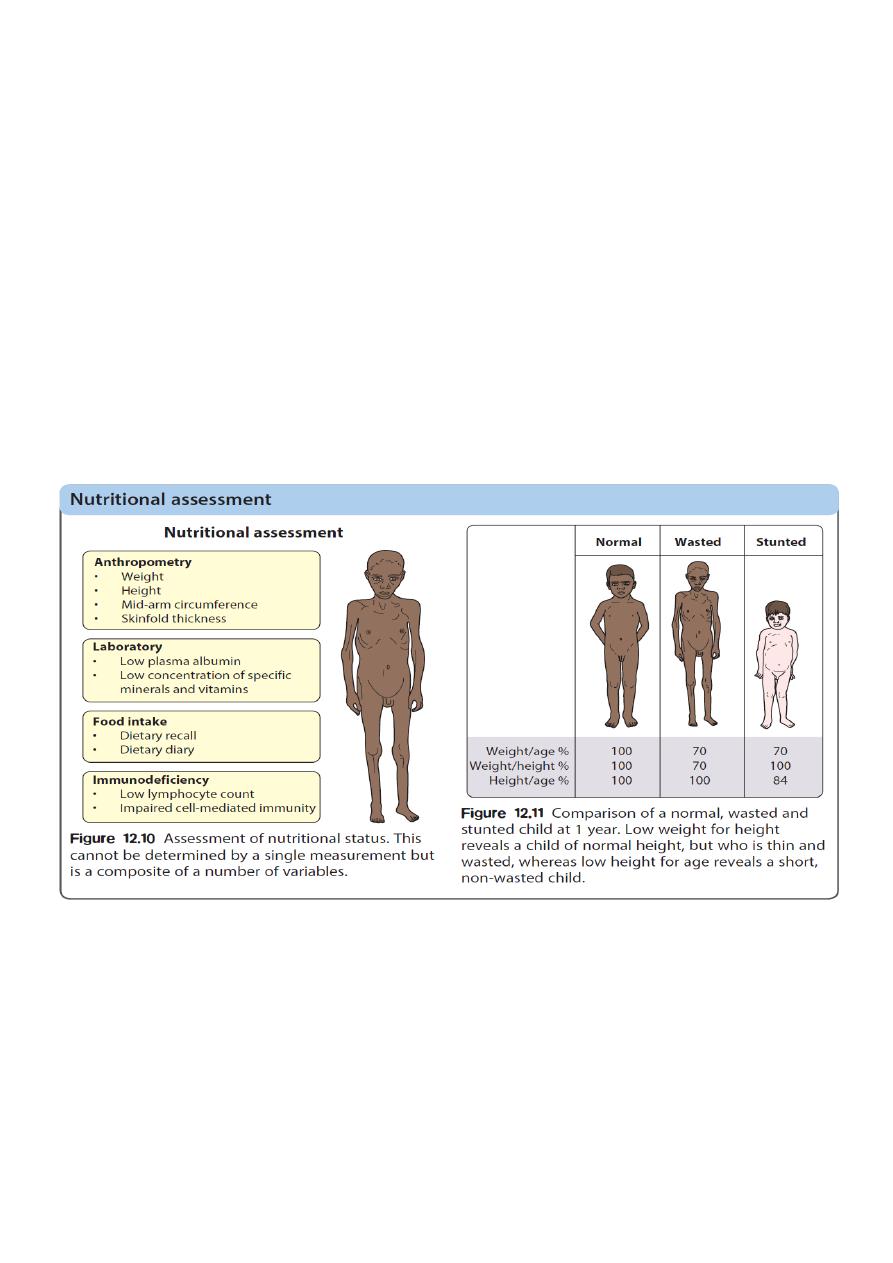
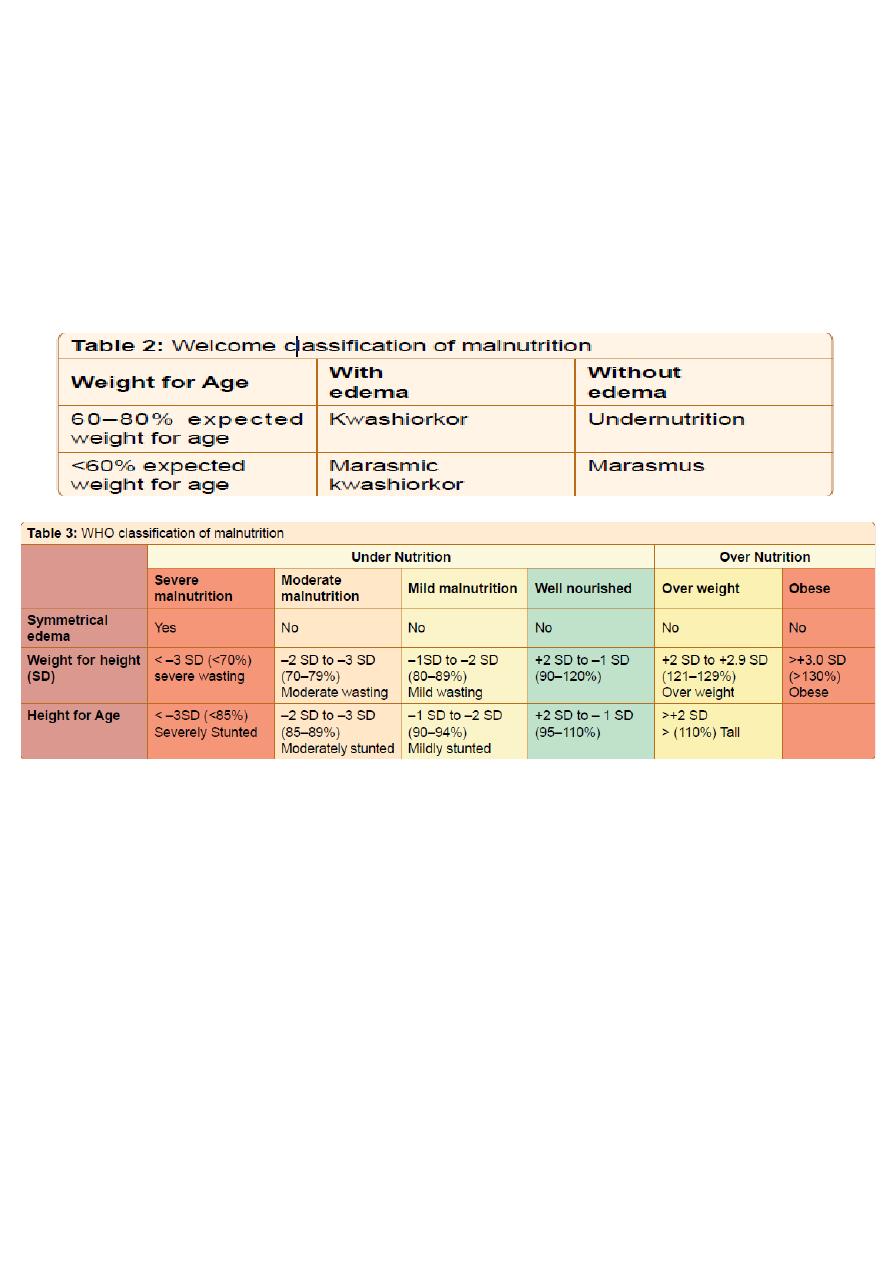
CLASSIFICATION OF MALNUTRITION
Marasmus
•
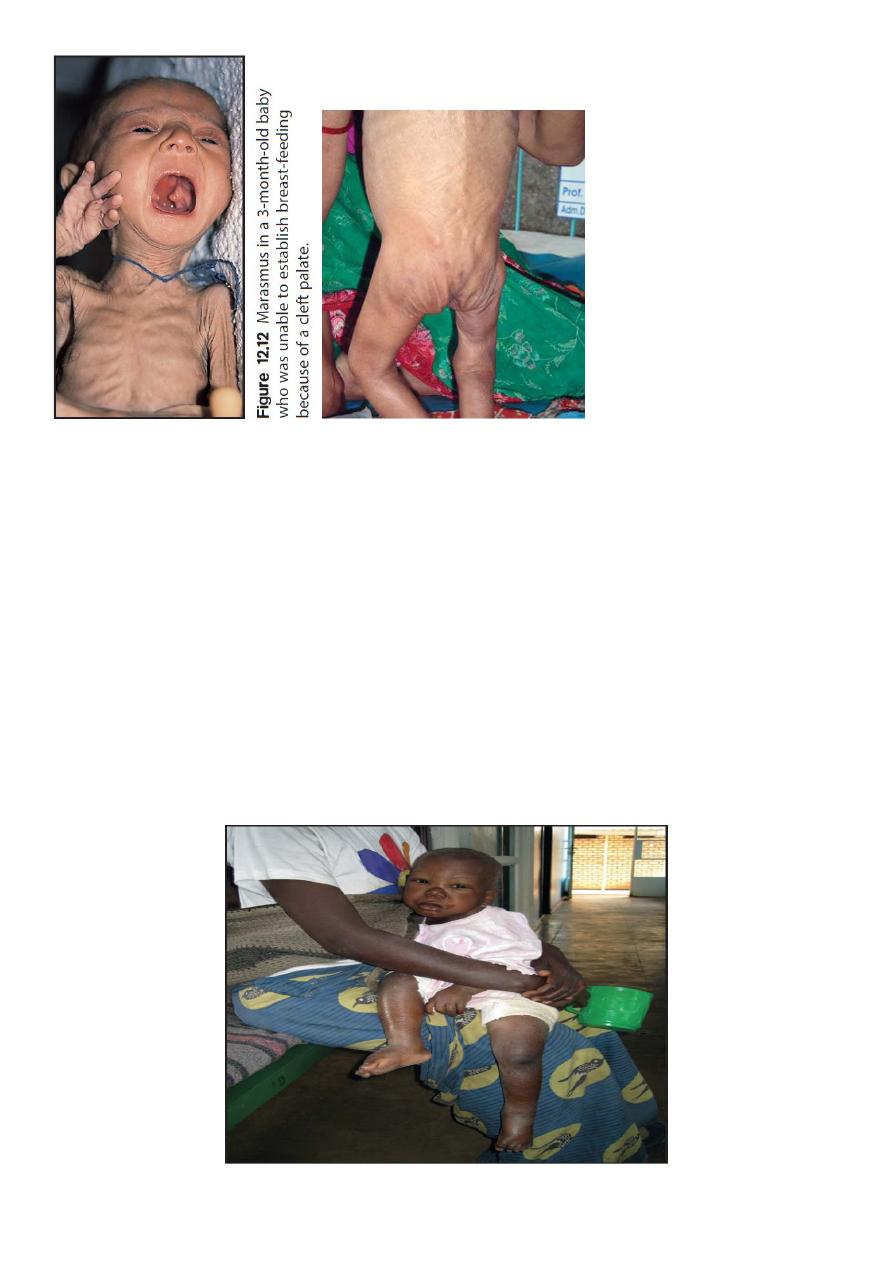
Severe protein-energy malnutrition in children usually leads to marasmus, with a
weight for height more than −3 standard deviations below the median,
corresponding to <70% weight for height, and a wasted, wizened appearance (Fig.
12.12). Oedema is not present. Skinfold thickness and mid-arm circumference are
markedly reduced, and affected children are often withdrawn and apathetic
5
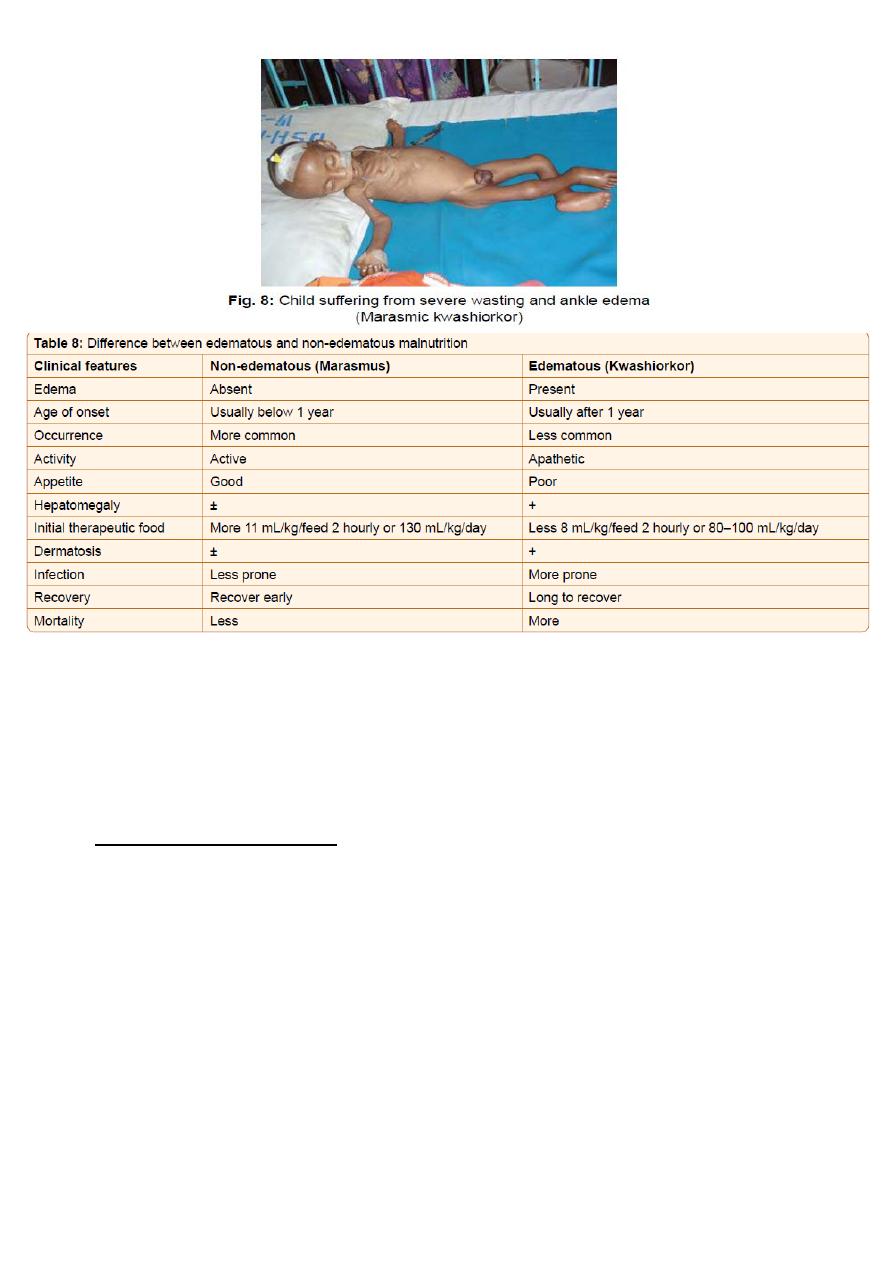
Kwashiorkor
•
Kwashiorkor is another manifestation of severe protein malnutrition in which there is
generalised oedema as well as severe wasting.Because of the oedema, the weight
may not be as severely reduced. In addition, there may be:
•
a ‘flaky-paint’ skin rash with hyperkeratosis (thickened skin) and desquamation
•
a distended abdomen and enlarged liver (usually due to fatty infiltration)
•
angular stomatitis
•
hair which is sparse and depigmented
•
diarrhoea, hypothermia, bradycardia and hypotension
•
low plasma albumin, potassium, glucose and magnesium.
6
Management
•
Severe acute malnutrition has a high mortality; about 30% in children require hospital
care. In addition to protein and energy deficiency, there is electrolyte and mineral
deficiency (potassium, zinc, magnesium) as well as micronutrient and vitamin
deficiency (vitamin A).
•
Acute management includes:
1. Hypoglycaemia – common; correct urgently, particularly if coma or severely ill.
2. Hypothermia – wrap, especially at night.
3. Dehydration – correct, but avoid being overzealous with intravenous fluids, as
may lead to heart failure.
4. Electrolytes – correct deficiencies, especially potassium
5. Infection – give antibiotics; fever and other sign may be absent. Treat oral candida
if present.
6. Micronutrients – give vitamin A and other vitamins
7. Initiate feeding – small volumes, frequently, including through the night.
7
•
Children with no appetite or medical complications need hospital care. Otherwise care
can be community based. Although protein deficient, diet is initially low in protein as
high protein feeds are not tolerated. Too rapid feeding may result in diarrhoea.
Specialised feeds are widely available. Initially Formula 75 (75 kcal/100 ml),
subsequently Formula 100 (100 kcal/100 ml) or Ready-to-Use Therapeutic Food
(RUTF).
•
During recovery phase, growth is monitored
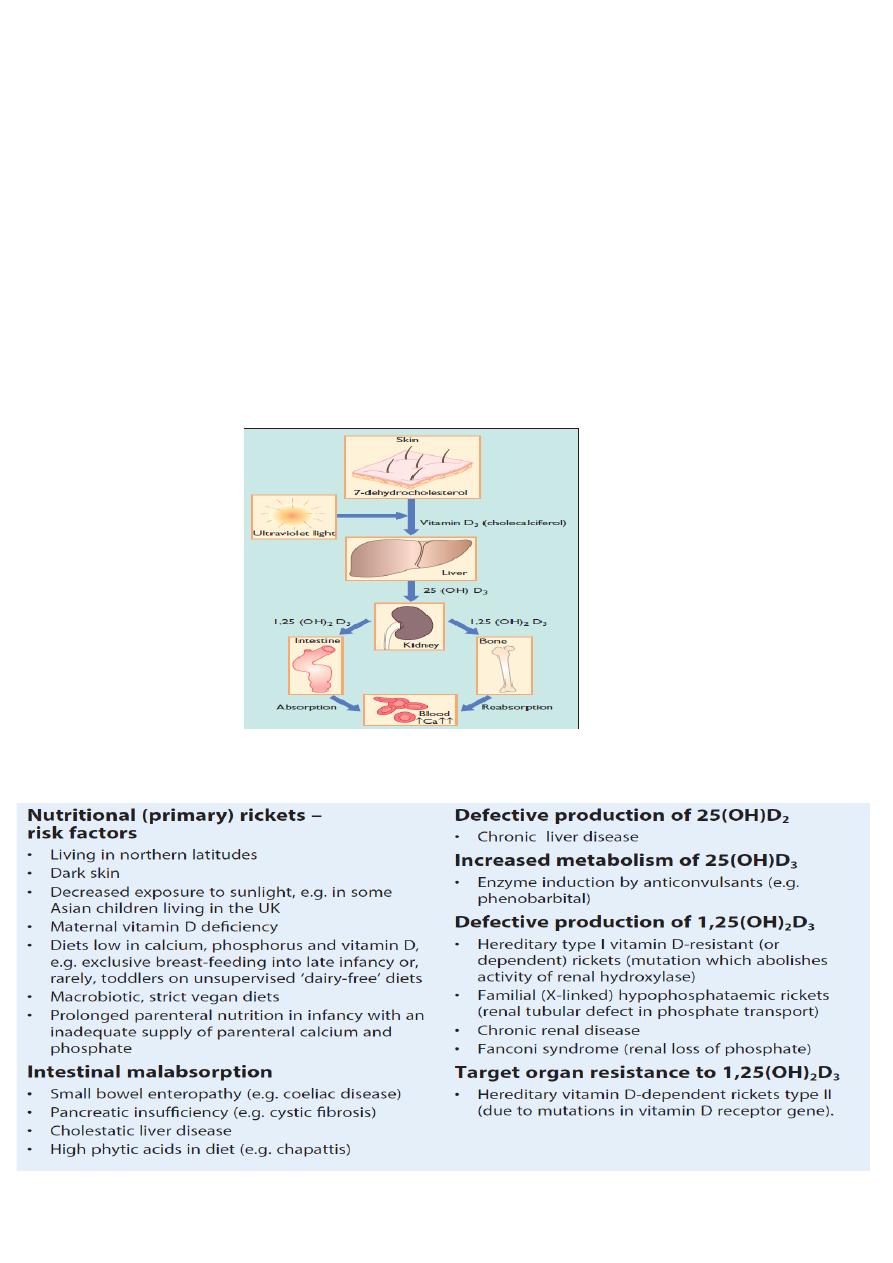
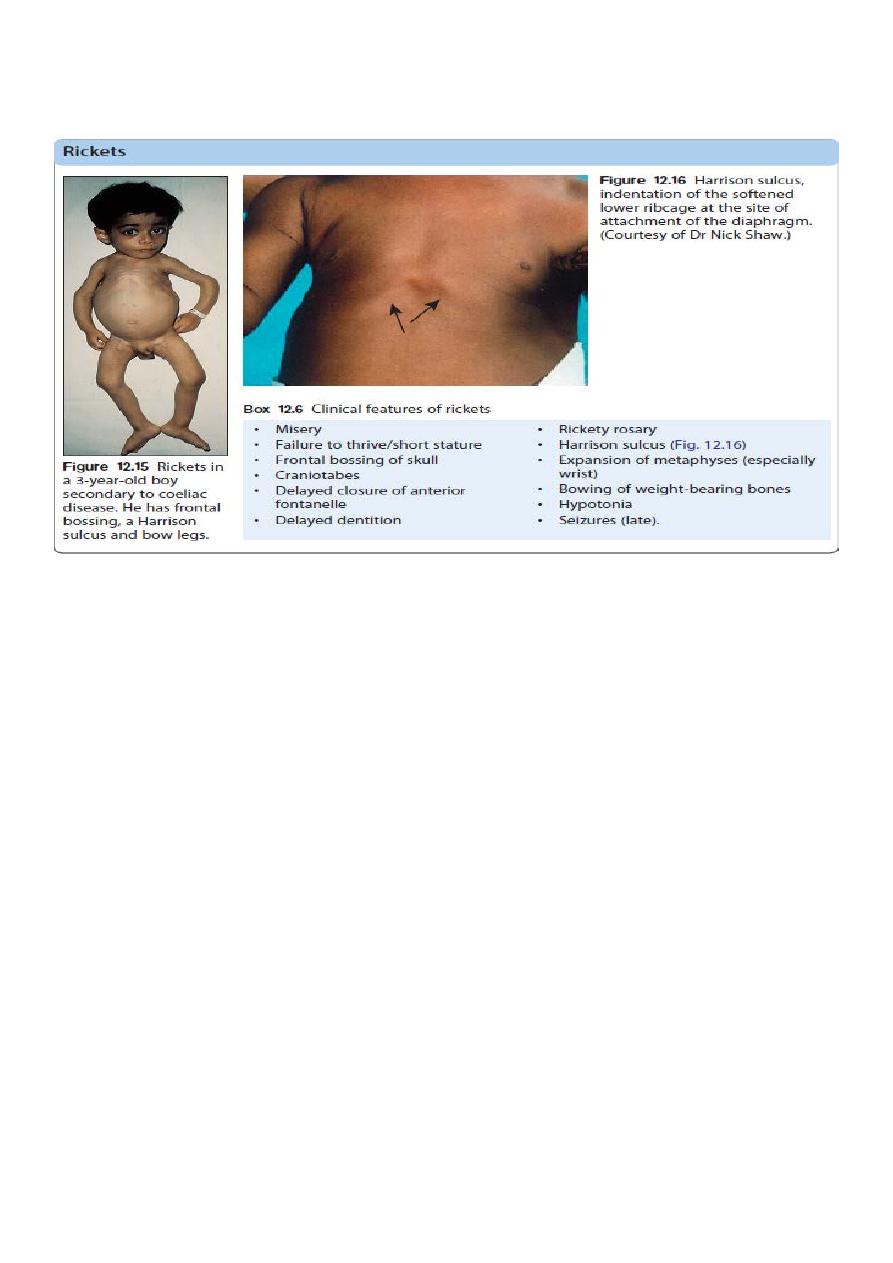
Rickets
Rickets signifies a failure in mineralisation of the growing bone or osteoid tissue. Failure of
mature bone to mineralise is osteomalacia.
Aetiology
8
Diagnosis
1. Dietary history for vitamin and calcium intake
2. Blood tests – serum calcium is low or normal phosphorus low, plasma alkaline
phosphatase activity greatly increased, 25-hydroxyvitamin D may be low and
parathyroid hormone elevated.
3. X-ray of the wrist joint – shows cupping and fraying of the metaphyses and a widened
epiphyseal plate.
Management
Nutritional rickets is managed by advice about a balanced diet, correction of predisposing
risk factors and by the daily administration of vitamin D3 (cholecalciferol). If compliance is
an issue, a single oral high dose of vitamin D3(600000iu) can be given, followed by the daily
maintenance dose. Healing occurs in 2–4 weeks and can be monitored from the lowering of
alkaline phosphatase, increasing vitamin D levels and healing on X-rays, but complete
reversal of bony deformities may take years
