
1
Fifth stage
Pediatric
Lec. 2
.د
ايمان
9
1 /4/2017
Specific poisoning
Acetaminophen(paracetamol)
• Normally metabolized by liver; saturation of normal pathways leads to breakdown of
acetaminophen by p450 to NAPQI (N-acetyl-p-benzoquinone imine )which combined
with hepatic cell causes hepatic necrosis.
• In therapeutic doses it is known to have very few adverse events.
The maximum daily dose of acetaminophen is 4 g in adults and 90 mg/kg in children. A
single ingestion of 7.5 g in an adult or more than 200 mg/kg in a child is a potentially toxic
dose but smaller doses may also cause liver damage.
Clinical manifestations:
● Stage I (0-24 hrs)
➢ Early symptoms
Mild (Nausea, vomiting, malaise and diaphoresis).
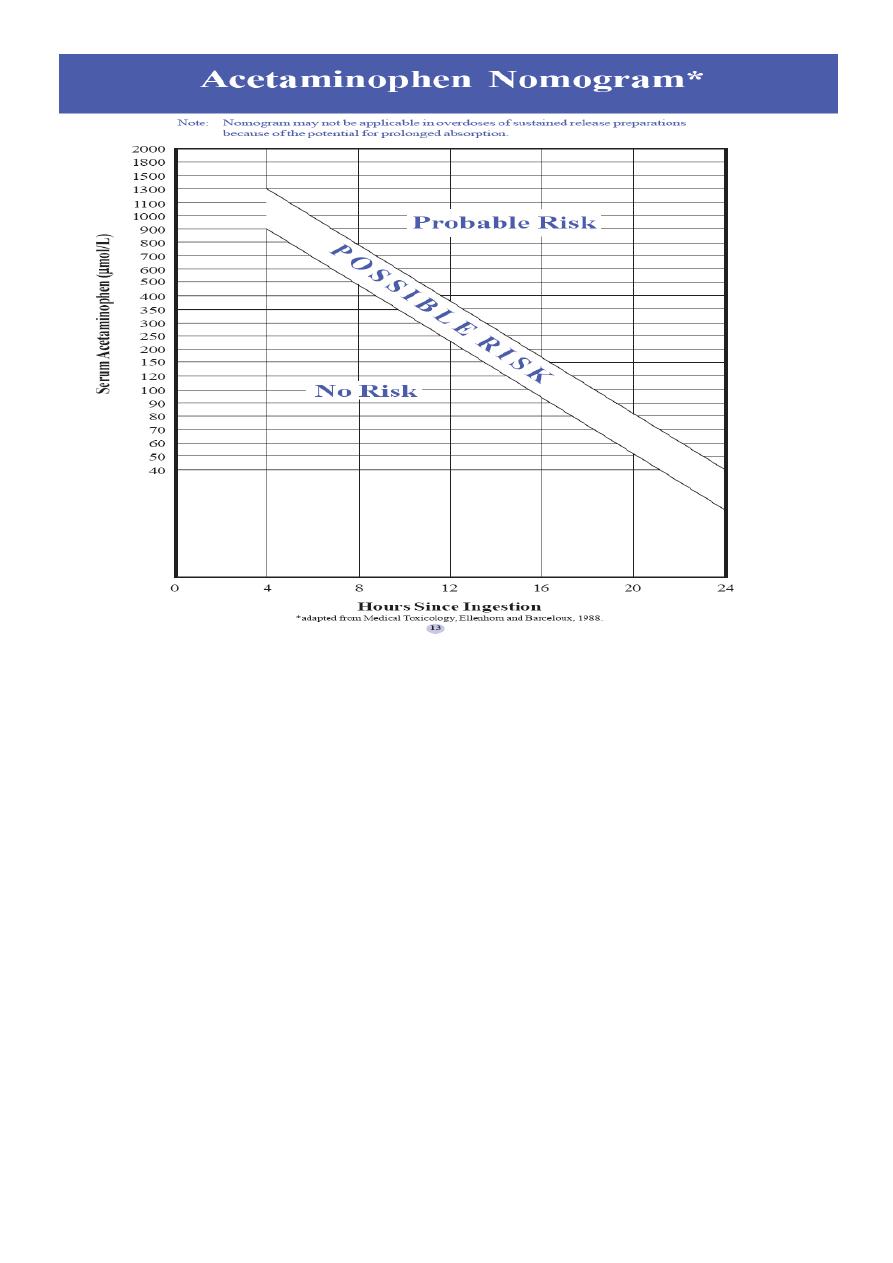
Serum acetaminophen level 4 hrs post ingestion
PLOT ON SPECIFIC NOMOGRAM.
No need to repeat levels
If > 900 µmol/L ---> Possible risk
➢ Normal bilirubin Transaminases and PT
Serum level 4h or more after ingestion can help predict hepatotoxicity
2
• Stage II:
› 24-48 hrs after ingestion.
▪ Better, less symptoms.
▪ Elevated bilirubin, transaminases and PT
• Stage III
› ( 2- 4 days) after ingestion:
▪ Hepatic dysfunction
▪ (Rarely hepatic failure)
▪ Peak elevations in:
• Bilirubin
• Transaminases may reach > 1000 IU/L
• Prolonged PT

3
• Stage IV
› (7-8 days)
▪ Depending on the extent of damage: Clinical improvement
LFTs returning to normal or…..
Death
Probable toxicity should be treated with:
N-acetylcysteine oral (effective as many as 24 hours after a toxic ingestion).
i.v administration NAC is recommended for selected pt.
Most pediatric patients can be treated with activated charcoal alone.
GIT decontamination limited to patients with recent (within 60 min) and potentially life-
threatening toxicity.
Iron Poisoning
Five Stages but variable
• Stage 1: 30 min to 6 hr after ingestion
▪ GIT stage: within several hrs of ingestion:
▪ V/D, Hematochezia and abdominal pain
▪ significant volume losses leading to potential hypovolemic shock.
▪ Patients who do not develop GI symptoms within 6 hr of ingestion are unlikely
to develop serious toxicity
Toxic doses occur at 10-20mg/Kg of elemental iron.
• Stage 2: Quiescent stage: 4-48hrs
▪ Clinical improvement of GIT
▪ signs of hypoperfusion, including tachycardia, pallor, and fatigue Decreased
U.O.P.

4
• Stage 3: Circulatory collapse : 48-96 hrs
▪ Metabolic acidosis, hypotension, Shock
▪ Coagulopathy
▪ Multi Organ Failure
• Stage 4:
▪ Hepatic failure: 96 hrs
▪ Liver transplant can save lives
• Stage 5: Bowel obstruction 2-6 wks Due to scarring
Management
1. Gastric decontamination:
WBI remains the decontamination strategy of choice
No activated charcoal to be used!!!
2. Secure good IV
3. Get initial then 4hrs Iron levels and TIBC
4. Chelate with Deferoxamine if levels> 500mg/dL
Hydrocarbons
Hydrocarbons (HC) are composed of large number of organic compounds made up of
carbon and hydrogen atoms.
e.g kerosene,benzene
They cause damage to lung and nervous system.
Ingestion is rarely more than 10 ml but as little as 2 ml entering in to the tracheobronchial
tree can cause severe chemical pneumonitis.
Pathophysiology:
Hydrocarbon aspiration primarily affects the CNS and respiratory systems. Volatile
hydrocarbons are highly lipid soluble. They enter the circulation through the lungs and
rapidly diffuse throughout the body and into the CNS .

5
Kerosene ingestion:
Clinical Presentation
Respiratory :
• Choking, gagging, and coughing usually begins immediately or within 2–5 min of
the aspiration, and persists.
• There may be oral pain.
• Vomiting is common.
• Signs of significant exposure are continued cough, tachypnea, increased
respiratory effort, rib cage retractions, grunting, wheezes, and rales on chest
auscultation.
Radiographic findings :
• often occur before the development of physical findings. They may be seen
within 20 minutes or as late as 24 hours after aspiration. CXR abnormalities
typically peak between 2-8 hr after aspiration.
• CXR findings include perihilar, basal, or lobar densities. Occasionally,
pneumatoceles develop after several days and may take weeks to resolve.
CVS : Cardiac arrhythmia may occur after inhalation.
GIT : local irritation to the pharynx, esophagus, stomach, and small intestine, with edema
and mucosal ulceration which may lead to hematemesis .
CNS : HC ingestion or inhalation may have direct CNS effects as headache, ataxia, dizziness,
blurred vision, weakness, stupor, seizures & coma or 2ry to hypoxia like CNS depression,
including drowsiness, tremors, or convulsions.
Hematologic : Leukocytosis (with fever) occurs early in the clinical course . Hemolysis,
hemoglobinuria, and consumptive coagulopathy also may occur with significant ingestion .
Treatment:
• Do not induce vomiting !!!!!
• Do not attempt gastric lavage !!!!!!
• Bronchospasm treated with selective beta 2 agonists.
• If gastric lavage is to be performed, the patient should be intubated with a cuffed
ETT to protect the airway from further aspiration.

6
• Activated charcoal also is not useful because it does not bind the common
hydrocarbons.
▪ Corticosteroid should be avoided.
▪ Antibiotcs given if bacterial pneumonia occurs.
▪ Treatment is usually supportive, attention to respiratory and CNS symptoms.
▪ Observe in ER for 6-8 hrs if no symptoms discharge.
Organophosphorus
• Insecticides
• Inhibition of Cholinesterase enzymes all over.
▪ Muscarinic symptoms are DUMBBELS, which stands for diarrhea/defecation,
urination, miosis, bronchorrhea/bronchospasm, bradycardia, emesis,
lacrimation, and salivation.
▪ Nicotinic signs and symptoms include muscle weakness, fasciculations,
tremors, hypoventilation (diaphragm paralysis)
▪ CVS hypertension, tachycardia, and dysrhythmias.
▪ Severe manifestations include coma, seizures, shock, arrhythmias, and
respiratory failure
Diagnosis
:
from hx & physical examination.
blood Cholinesterase levels < 50% indicates poisoning.
Atropine as test dose
Management:
A….B….C….. Stabilization
Wash hair and body with soap & water
Consider Gastric lavage if within 1hr
Atropine sulphate I.V. till pupils are normal size.
Remember…Atropine has no effect on muscle paralysis must support breathing
USE Cholinestrase reactivator such as Pralidoxime

7
Tricyclic Antidepressants
e.g amitriptyline
Anticholinergic effects cause most of the following presenting symptoms:
Dry mouth
Flushed skin
Blurred vision
Urinary retention
Constipation
Dizziness
Emesis
Physical Signs of TCA toxicity include the following:
Anticholinergic effects
Altered mental status (agitation, confusion, lethargy)
Resting sinus tachycardia
Dry mucous membranes
Mydriasis
Fever
Cardiac effects
Hypertension (early and transient, should not be treated)
Tachycardia
Orthostasis and hypotension
Arrhythmia/ECG changes
CNS effects
Coma
Seizure
Myoclonic twitches/tremor
Hyperreflexia
Pulmonary effects - Hypoventilation resulting from CNS depression
GIT effects - Decreased or absent bowel sounds

8
Lab Studies:
Rapid bedside glucose level determination
Serum pH, electrolytes, calcium, Urine toxicology screening
The single most important test to guide therapy and prognosis remains the 12-lead surface
ECG. Important ECG changes include the following:
1. Prolongation of the QRS complex
2. Prolongation of the QT interval
3. Tachycardia and arrhythmia
Medical Care:
Careful attention to ABC, and neurologic parameters are of most importance because of
the risk of rapid deterioration in patients. Decontamination strategies should be used
carefully in selected patients(usually charcoal)
Sodium bicarbonate given in doses to achieve PH level 7.45-7.55 to treat and prevent
dysrhythmias
Lidocain is used to treat dysrhythmias that are unresponsive to serum alkalization
Lomotil (enterostop®)
Antidiarrheal agent containing both diphenoxylate and atropine.
Both agents are absorbed by the GIT and absorption may be delayed in overdose due to
inhibitory effects on smooth muscle motility.
Diphenoxylate is an opioid
Patients manifest signs and symptoms of opiate toxicity(respiratory depression, altered
mental status, and miosis).
Respond well to naloxone and supportive care.
Current recommendations are for a minimum of 24 hour observation.

9
Common Antidotes
1. Organophosphate : atropine+pralidoxime
2. Anticholinergic drugs : physostigmine
3. Acetaminophen : N-acetylcystiene
4. Methemoglobinemia : methylene blue+vitamin C
5. Narcotics (opiates) : naloxone
6. Benzodiazepines (valium) : flumazenil
7. Iron : deferoxamine (desferal)
8. Cyanide : amylnitrate
9. Arsenic, mercury,other metals : BAL
10. Lead : DMSA-EDTA
11. Methanol : ethanol
12. Acute dystonic reaction : diphenhydramine
