Internal Medicine: 4
th
Stage TUCOM Dr.Hassan
DISEASES OF THE ESOPHAGUS
Learning objectives:
1. Review the functional anatomy and physiology of esophagus.
2. Understand the concept of Gastro-esophageal reflux disease (GERD).
3. List the factors that associated with development of GERD.
4. Explain the clinical features of GERD.
5. List the important investigations and it’s indications in patients with GERD.
6. Review the treatment of GERD.
7. List the complications of GERD.
8. List other causes of esophagitis.
9. List the motility disorders of esophagus.
10.Describe the definition, pathogenesis, and clinical presentation of achalasia.
11.Outline the important investigations of achalasia.
12.review the treatment of achalasia.
13.List the types of esophageal carcinoma.
14.Recognized the epidemiology of esophageal carcinoma.
15.Understand the difference between squamous cell carcinoma and adenocarcinoma
of esophagus.
16.Known the clinical features of esophageal carcinoma.
17.List the important investigations of esophageal carcinoma.
18.Outline the treatment of esophageal carcinoma.
Esophagus:
• This muscular tube extends 25 cm from the cricoid cartilage to the cardiac orifice of
the stomach. It has an upper and a lower sphincter. it is lined by stratified squamous
epithelium. The muscle layers of the upper esophagus are striated skeletal muscle,
while the muscles of lower part are smooth. A peristaltic swallowing wave propels the
food bolus into the stomach.
GASTRO-ESOPHAGEAL REFLUX DISEASE:
• Gastro-esophageal reflux disease (GERD) develops when the esophageal mucosa is
exposed to gastric contents for prolonged periods of time, resulting in symptoms and,
in a proportion of cases, esophagitis.
• Gastro-esophageal reflux resulting in heartburn affects approximately 30% of the
general population.
Factors associated with the development of (GERD):
1. Obesity and dietary factors.
2. Defective oesophageal clearance.
3. Abnormal lower esophageal sphincter:
1. Reduced tone.
Page of
1
105
Internal Medicine: 4
th
Stage TUCOM Dr.Hassan
2. Inappropriate relaxation.
4. Hiatus hernia.
5. Delayed gastric emptying.
6. Increased intraabdominal pressure.
Hiatus hernia:
• Hiatus hernia: An anatomical abnormality in which part of the stomach protrudes up
through the diaphragm into the chest.
• Causes reflux because the pressure gradient between the abdominal and thoracic
cavities, which normally pinches the hiatus, is lost. In addition, the oblique angle
between the cardia and esophagus disappears. Many patients who have large hiatus
hernias develop reflux symptoms.
Types of hiatus hernia:
1. Sliding.
2. Rolling or paraesophageal.
Clinical features of GERD:
• Major symptoms; are heartburn and regurgitation, often provoked by bending,
straining or lying down.
• Waterbrash; which is salivation due to reflex salivary gland stimulation as acid enters
the gullet.
• Others develop odynophagia or dysphagia. A few present with atypical chest pain
which may be severe, can mimic angina and is probably due to reflux-induced
esophageal spasm.
Complications:
1. Esophagitis: A range of endoscopic findings, from mild redness to severe, bleeding
ulceration with stricture formation.
2. Barrett's esophagus: ('columnar lined oesophagus'-CLO) is a pre-malignant
glandular metaplasia of the lower esophagus, in which the normal squamous lining
is replaced by columnar mucosa of intestinal metaplasia. CLO is the major risk
factor for esophageal adenocarcinoma. Diagnosis of this condition requires
multiple biopsies from suspected area to detect intestinal metaplasia and/or
dysplasia. Neither potent acid suppression nor antireflux surgery will stop
progression or induce regression of CLO. Esophagectomy is widely recommended
for those with high grade dysplasia.
3. Anaemia; Iron deficiency anaemia occurs as a consequence of chronic, insidious
blood loss from long-standing esophagitis.
4. Benign esophageal stricture; Fibrous strictures develop as a consequence of long-
standing esophagitis.
Page of
2
105
Internal Medicine: 4
th
Stage TUCOM Dr.Hassan
5. Gastric volvulus; Occasionally a massive intra-thoracic hiatus hernia may twist
upon itself.
Investigations:
• Young patients who present with typical symptoms of gastro-esophageal reflux,
without worrying features such as dysphagia, weight loss or anaemia, can be treated
empirically without investigation.
• Is advisable if patients over 55 year old, if symptoms are atypical or if a complication
is suspected or if there is no response to empirical treatment.
• Investigations include:
1. Endoscopy is the investigation of choice. This is performed to exclude other upper
gastrointestinal diseases which can mimic gastro-esophageal reflux, and to identify
complications.
2. Twenty-four-hour pH monitoring is indicated if, despite endoscopy, the diagnosis is
unclear or surgical intervention is under consideration.
1) A slim catheter with a terminal radiotelemetry pH-sensitive probe above the
gastro-esophageal junction.
2) episodes of pain are noted and related to pH. A pH of less than 4 for more than
6-7% of the study time is diagnostic of reflux disease.
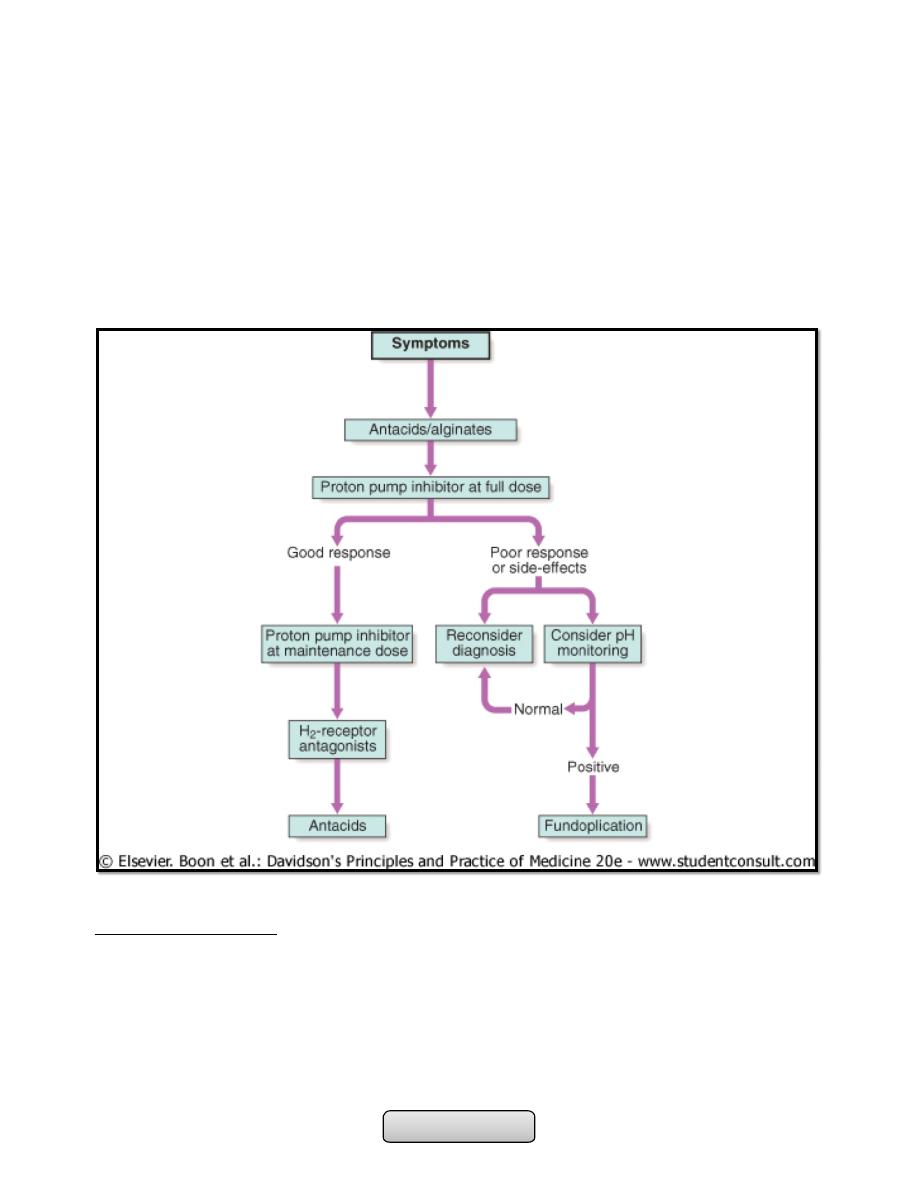
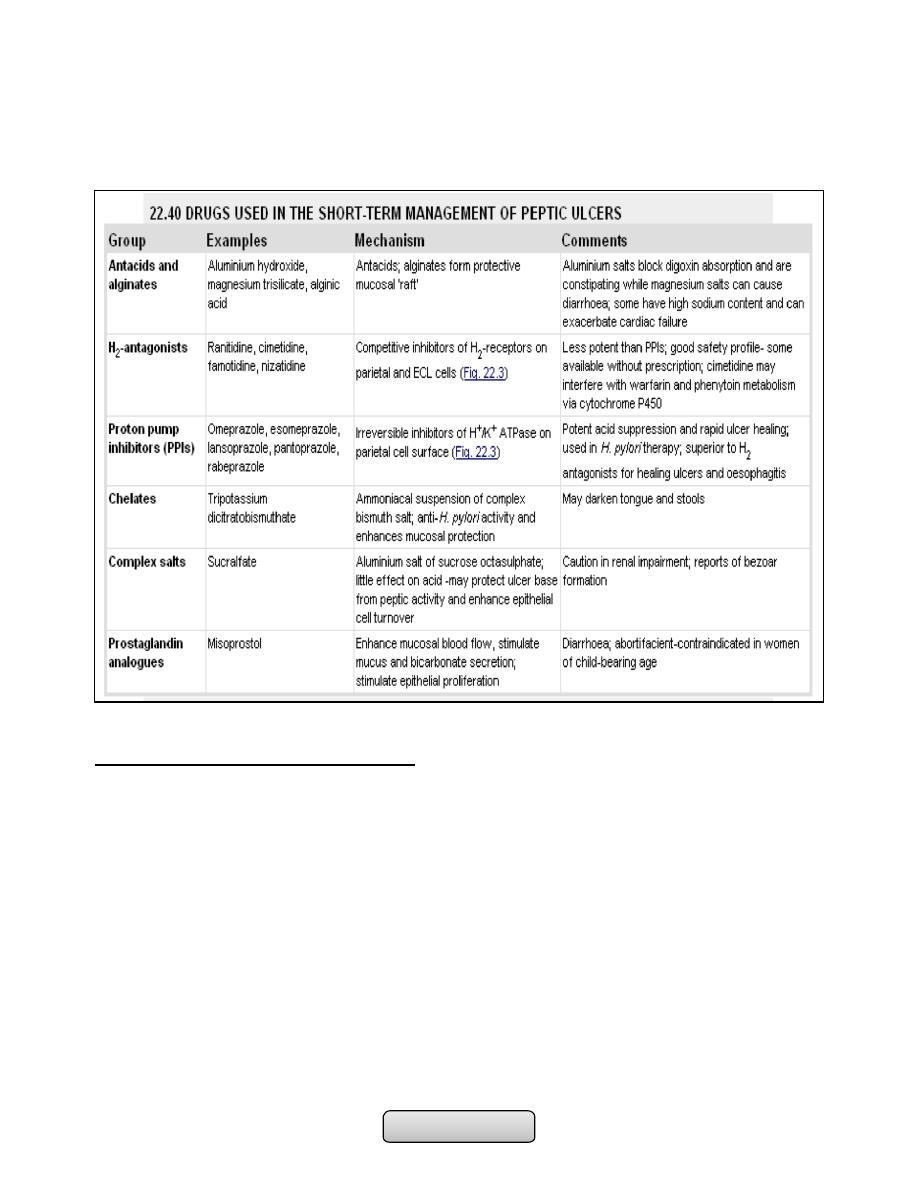
Management:
1. Lifestyle advice; including weight loss, avoidance of dietary items which the
patient finds worsen symptoms, elevation of the bed head in those who experience
nocturnal symptoms, avoidance of late meals and giving up smoking.
2. Antacids and alginates; also provide symptomatic benefit.
3. H
2
-receptor antagonist drugs; also help symptoms without healing esophagitis.
4. Proton pump inhibitors; are the treatment of choice for severe symptoms and for
complicated reflux disease.
5. Anti-reflux surgery; Patients who fail to respond to medical therapy, those who are
unwilling to take long-term proton pump inhibitors and those whose major
symptom is severe regurgitation.
OTHER CAUSES OF ESOPHAGITIS:
1. Infection; Esophageal candidiasis, Herpes simplex virus, Cytomegalovirus
(CMV) ,and HIV infection .
2. Corrosives; Strong household bleach or battery acid .
3. Drugs; Tetracyclines, potassium preparations, nonsteroidal anti-inflammatory
drugs, iron sulfate, and the bisphosphonate alendronate.
• Candida esophagitis is often associated with oral thrush and tends to present with
dysphagia and only mild pain on swallowing. It has a characteristic appearance on
Page of
3
105
Internal Medicine: 4
th
Stage TUCOM Dr.Hassan
endoscopy, and esophageal brushings and biopsies demonstrate fungal hyphae.
Treatment with oral fluconazole is generally very effective.
• Herpes simplex virus causes multiple esophageal ulcers and presents clinically with
severe odynophagia. Acyclovir is the treatment of choice for herpes esophagitis.
• Cytomegalovirus (CMV) also causes esophageal ulceration and odynophagia. Endoscopy
usually demonstrates a single large ulcer in the distal esophagus, and biopsies often
detect viral inclusions that confirm the diagnosis. Both ganciclovir and foscarnet are
effective treatments for CMV esophagitis.
MOTILITY DISORDERS:
1. PHARYNGEAL POUCH; Incoordination of swallowing within the pharynx leads to
herniation through the cricopharyngeus muscle and formation of a pouch.
2. DIFFUSE ESOPHAGEAL SPASM
3. ACHALASIA OF THE OESOPHAGUS
4. SECONDARY CAUSES ; systemic sclerosis, Dermatomyositis, rheumatoid arthritis and
myasthenia gravis.
Page of
4
105
Internal Medicine: 4
th
Stage TUCOM Dr.Hassan
PHARYNGEAL POUCH:
• Most patients are elderly and have no symptoms, although regurgitation, halitosis and
dysphagia can occur. Some notice gurgling in the throat after swallowing. A barium
swallow demonstrates the pouch and reveals incoordination of swallowing, often with
pulmonary aspiration. Endoscopy may be hazardous since the instrument may enter
and perforate the pouch. Surgical myotomy and resection of the pouch are indicated
in symptomatic patients.
Diffuse esophageal spasm:
• Episodic chest pain which may mimic angina, but is sometimes accompanied by
transient dysphagia. Some cases occur in response to gastro-esophageal reflux.
Treatment is based upon the use of proton pump inhibitor drugs when gastro-
esophageal reflux is present. Oral or sublingual nitrates or nifedipine may relieve
attacks.
ACHALASIA OF THE OESOPHAGUS:
Pathophysiology;
Achalasia is characterised by:
• A hypertonic lower esophageal sphincter: which fails to relax in response to the
swallowing wave.
• Failure of propagated esophageal contraction: leading to progressive dilatation of the
gullet.
Cause;
1. Is unknown.
2. Abnormal nitric oxide synthesis within the lower esophageal sphincter.
3. Degeneration of ganglion cells within the sphincter and the body of the esophagus
occurs.
4. Loss of the dorsal vagal nuclei within the brain stem.
5. Chagas disease.
Barium swallow findings:
• Tapered narrowing of the lower esophagus, esophageal body is dilated, aperistaltic
and food-filled.
Clinical features:
• Usually develops in middle life;
• Dysphagia develops slowly, and is initially intermittent, it is worse for solids and is
eased by drinking liquids, and by standing and moving around after eating.
• Episodes of severe chest pain due to esophageal spasm('vigorous achalasia').
• Nocturnal pulmonary aspiration develops.
• Predisposes to squamous carcinoma of the esophagus.
Investigations:
• Chest X-ray; widening of the mediastinum, aspiration pneumonia.
Page of
5
105
Internal Medicine: 4
th
Stage TUCOM Dr.Hassan
• A barium swallow; tapered narrowing of the lower esophagus, esophageal body is
dilated, aperistaltic and food-filled.
• Endoscopy; must always be carried out, carcinoma of the cardia can mimic the
presentation and radiological and manometric features of achalasia ('pseudo-
achalasia').
• Manometry; confirms the high-pressure, non-relaxing lower esophageal sphincter with
poor contractility of the esophageal body.
Management:
• Endoscopic Forceful pneumatic dilatation improves symptoms in 80% of patients.
Some patients require more than one dilatation, injection of botulinum toxin into the
lower esophageal sphincter.
• Surgical myotomy ('Heller's operation') with anti-reflux procedure. Proton pump
inhibitor therapy is also often necessary. Because it may be complicated by gastro-
esophageal reflux.
OESOPHAGEAL STRICTURE:
CAUSES;
1. Gastro-esophageal reflux disease
2. Webs and rings
3. Carcinoma of the esophagus or cardia
4. Extrinsic compression from bronchial carcinoma
5. Corrosive ingestion
6. Post-operative scarring following esophageal resection
7. Post-radiotherapy
8. Following long-term nasogastric intubation
CARCINOMA OF THE ESOPHAGUS:
1. Squamous cell carcinoma; rare in Western, common in Iran, parts of Africa and China,
mostly in upper 2 third of the esophagus.
• AETIOLOGICAL FACTORS;
-
Smoking.
-
Alcohol excess.
-
Chewing betel nuts or tobacco.
-
Coeliac disease.
-
Achalasia of the esophagus.
-
Post-cricoid web.
-
Post-caustic stricture.
-
Tylosis (familial hyperkeratosis of palms and soles).
2. Adenocarcinoma; In Western populations, in the lower third of the esophagus, from
Barrett's esophagus or from the cardia of the stomach.
Page of
6
105
Internal Medicine: 4
th
Stage TUCOM Dr.Hassan
Clinical features:
• Progressive, painless dysphagia for solid foods.
• In late stages weight loss is often extreme.
• Chest pain or hoarseness suggests mediastinal invasion.
• Fistulation between the esophagus and the trachea or bronchial tree; pneumonia and
pleural effusion.
• Metastatic spread is common.
Investigations:
• Endoscopy; The investigation of choice, with cytology and biopsy.
• Barium swallow ; site and length of the stricture .
• Thoracic and abdominal CT
• Endoscopic ultrasound (EUS)
Management:
1. Esophageal resection; overall 5-year survival rate is 6-9%. 70% of patients have
extensive disease at presentation.
2. Neoadjuvant (pre-operative) chemotherapy with agents such as cisplatin and 5-
fluorouracil.
3. Radiotherapy; squamous carcinomas are radiosensitive.
4. Palliative treatment;
-
Relief of dysphagia and pain, laser therapy.
-
Insertion of stents.
-
Radiotherapy to shrink tumour size.
-
Nutritional support.
-
Analgesia.
………………………………………………………………………………………….
UPPER GASTROINTESTINAL HAEMORRHAGE
Learning objectives:
1. Identify upper gastrointestinal haemorrhage.
2. Recognize the causes of upper gastrointestinal haemorrhage.
3. Clarify the management steps of patient with upper gastrointestinal haemorrhage.
4. Outline the prognostic factors in patient with upper gastrointestinal haemorrhage.
5. Identify the concept of occult gastrointestinal bleeding.
Upper gastrointestinal haemorrhage:
• Upper GI bleeding; Bleeding from GIT proximal to ligament of Teritz (band of C.T
connect the distal part of duodenum to the diaphragm).
• Is the most common gastrointestinal emergency.
Page of
7
105
Internal Medicine: 4
th
Stage TUCOM Dr.Hassan
Clinical assessment;
1. Haematemesis; may be red with clots when bleeding is profuse, or black ('coffee
grounds') when less severe.
2. Melaena; is the term used to describe the passage of black-tarry, loose, sticky,
foul-smelling stools that containing altered blood, caused by oxidation of the iron
in hemoglobin during its passage through the colon. As little as 100 mL of blood in
the stomach can produce melena.
3. Hematochezia; The passage of bright red blood or maroon stools per rectum. Is
commonly associated with lower gastrointestinal bleeding, but may also occur
from a brisk upper GI bleed.
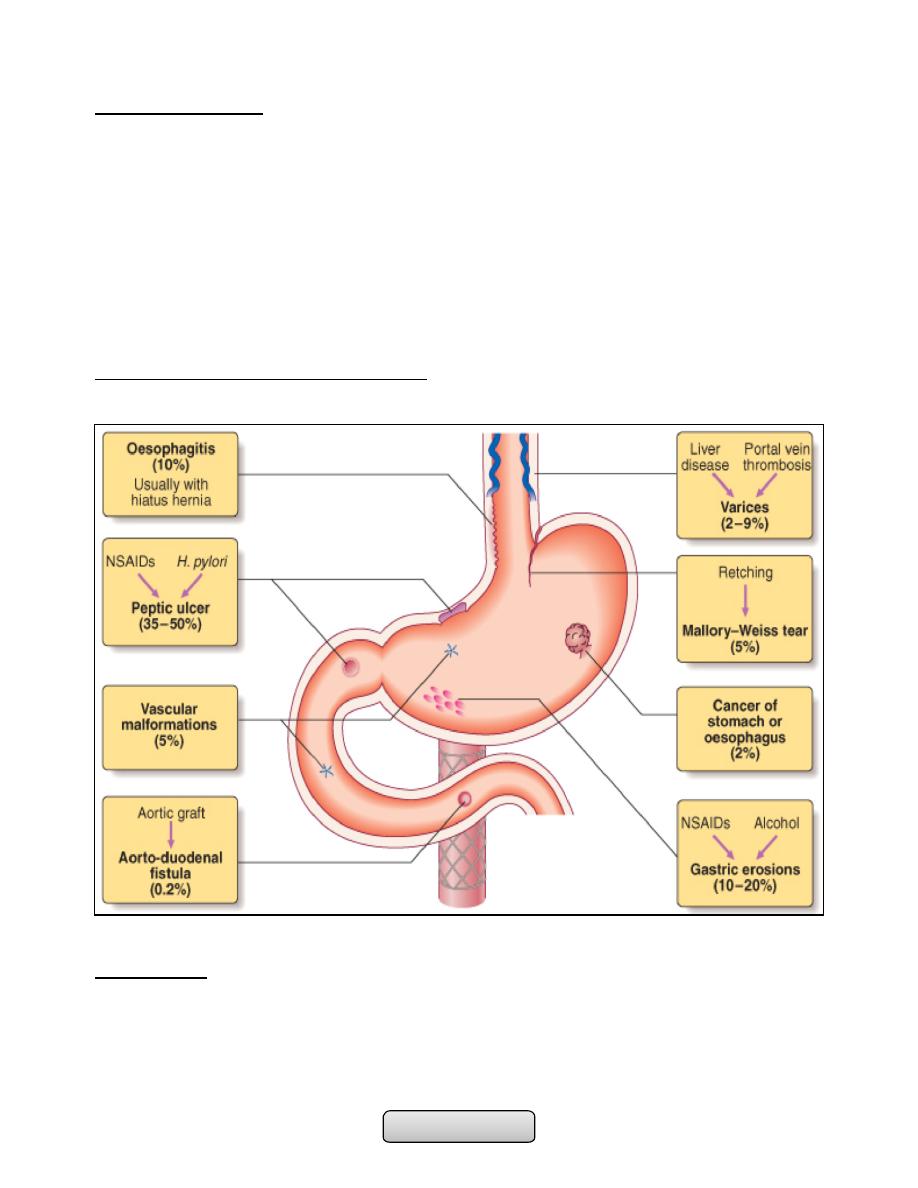
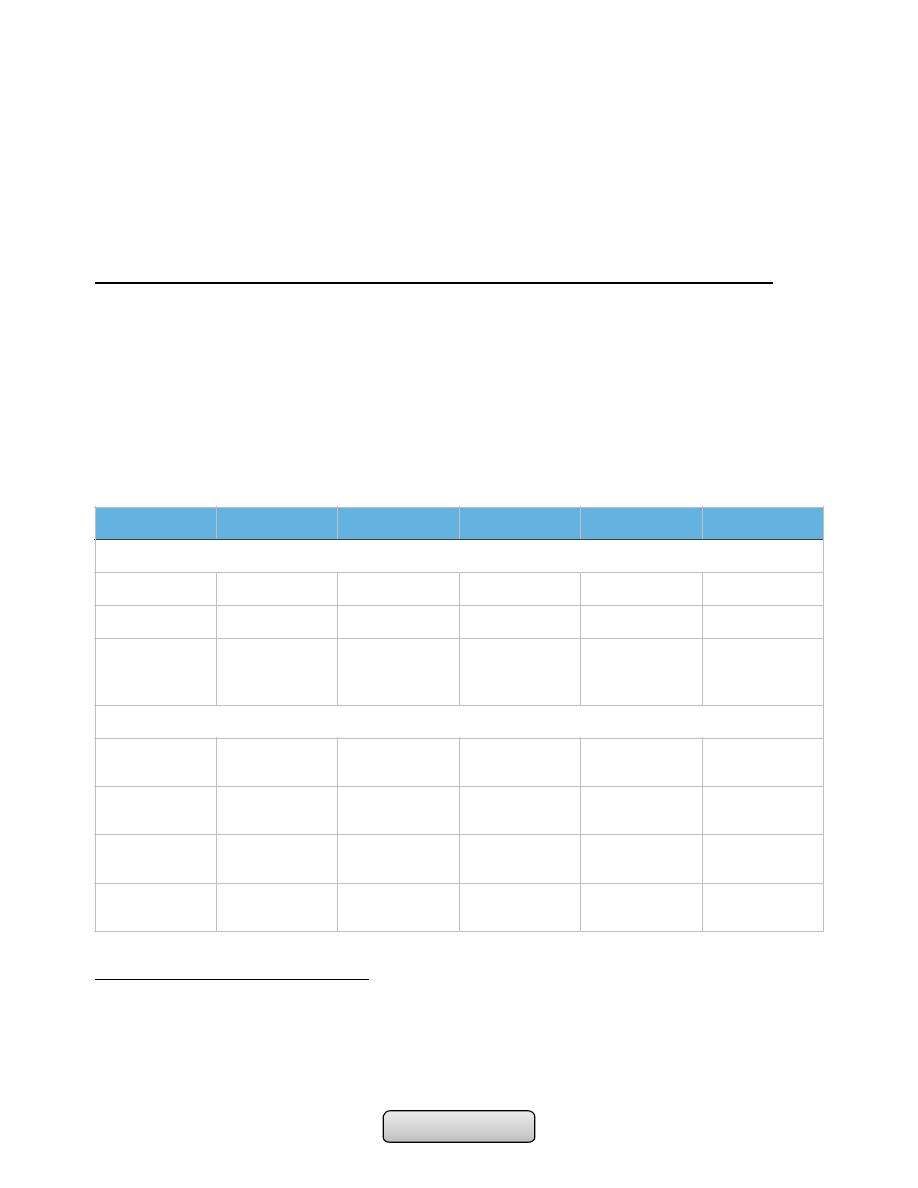
Causes of acute upper GI haemorrhage:
Management:
A. Intravenous access; Using two or at least one large-bore cannula. should be
placed in proximal large vein e. g. in antecubital fossa.
B. Initial clinical assessment;
1. Define circulatory status;
Page of
8
105

Internal Medicine: 4
th
Stage TUCOM Dr.Hassan
a) Systolic blood pressure drops changes positions from supine to standing
(postural hypotension); indicates lost at least 800 mL (15%) of circulating
blood volume.
b) Hypotension: tachycardia, tachypnea, and mental status; indicates that
1500 mL (30%) loss of circulating blood volume.
2. Severe bleeding ; causes tachycardia with hypotension and oliguria. The patient
is cold and sweating, and may be agitated.
3. Seek evidence of chronic liver disease; Jaundice, cutaneous stigmata,
hepatosplenomegaly and ascites may be present in decompensated liver
cirrhosis.
4. Define comorbidity; The presence of cardiorespiratory, cerebrovascular or renal
disease is important.
C. Blood tests;
1. Blood group, Rhesus and cross-matching of at least 2 units of blood; 4 units if
Systolic blood pressure drops below 100 mmHg and 6 units for active variceal
bleeding.
2. Full blood count; Chronic bleeding leads to anemia, but HB concentration may
be normal after acute bleeding.
3. Urea and electrolytes; renal failure, absorbed products of luminal blood well
be increase urea.
4. Liver function tests;
5. Prothrombin time;
D. Resuscitation; Intravenous crystalloid fluids (0.9% NS) or colloid such as (gelofusin
or Hartman's solution) are given, Blood is transfused when the patient is shocked
or HB less than 100 g per liter. NS should be avoided in patient with liver disease.
(CVP) monitoring is useful in severe bleeding.
E. Oxygen; by facemask to all patients in shock.
F. Endoscopy; after adequate resuscitation:
1. Diagnosis.
2. Endoscopic stigmata of recent haemorrhage: Spurting hemorrhage, visible
vessel or adherent clot.
a) Major stigmata of recent haemorrhage and endoscopic treatment:
(1) Active arterial spurting from a gastric ulcer. An endoscopic clip is about
to be placed on the bleeding vessel. When associated with shock, 80% of
cases will continue to bleed or rebleed.
(2) 'Visible vessel' (arrow). In reality, this is a pseudoaneurysm of the feeding
artery seen here in a pre-pyloric peptic ulcer. It carries a 50% chance of
rebleeding.
(3) Haemostasis is achieved after endoscopic clipping of the bleeding vessel
in the duodenum.
3. Endoscopic therapy.
Page of
9
105
Internal Medicine: 4
th
Stage TUCOM Dr.Hassan
G. Monitoring; hourly pulse, blood pressure and urine output measurements.
H. Surgical operation; urgent operation:
1. Endoscopic hemostasis fails to stop active bleeding.
2. Rebleeding; on one occasion in an elderly or frail patient, or twice in younger,
fitter patients.
I. Prognosis; The mortality rate is depend on Rockall score for risk stratification
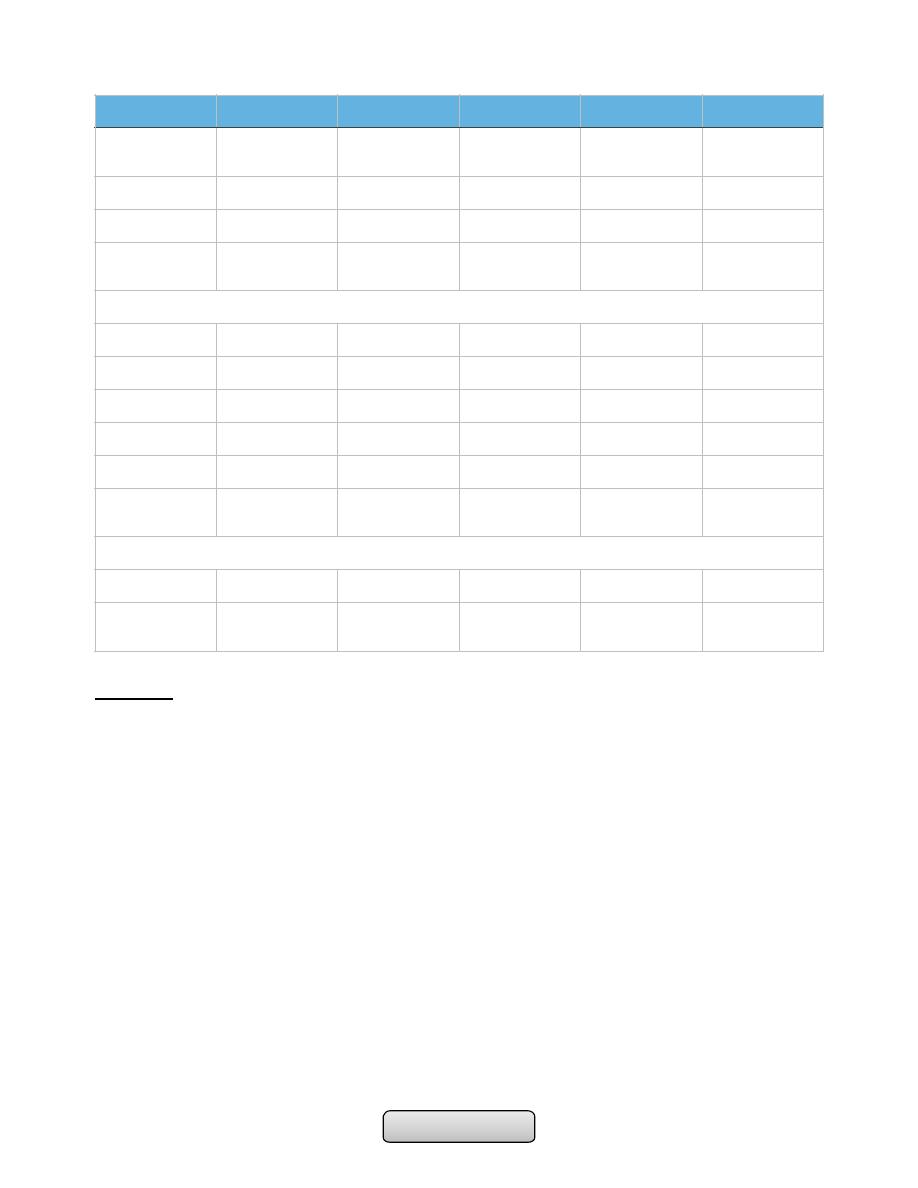
Rockall score for risk stratification in acute upper gastrointestinal haemorrhage:
1. Malignancy and varices have the worst prognosis.
2. These features are associated with a high risk of rebleeding. Rebleeding (fresh
haematemesis or melaena associated with shock or a fall of haemoglobin > 20 g/L
over 24 hours) is associated with a 10-fold increased risk of death.
3. An initial score can be calculated, endoscopic findings can be added later and a final
score then obtained, ranging from 0 to 11.
-
A score < 3 is associated with a good prognosis.
-
While a total score > 8 carries a high risk of mortality.
Occult gastrointestinal bleeding:
• 'Occult' means that blood or its breakdown products are present in the stool but
cannot be seen by the naked eye.
• It may reach 200 ml per day.
Variable
Score 0
Score 1
Score 2
Score 3
Score
Calculate on admission
1- Age
< 60
60-79
> 80
2- Shock
No shock
Pulse > 100
SBP < 100
3- Comorbidity
Nil major
CCF, IHD,
major
comorbidity
Renal/liver
failure
Metastatic
cancer
Calculate after endoscopy
4- Diagnosis
Mallory-Weiss
tear or normal
All other
diagnoses
GI malignancy1
5- Evidence of
bleeding
None
Blood in
stomach
Adherent clot
Visible or
spurting vessel2
Final score
(range 0-11)
Page of
10
105
Internal Medicine: 4
th
Stage TUCOM Dr.Hassan
• Cause iron deficiency anemia (IDA). Clinically suspected when a patient presents with
unexplained IDA.
• Any cause of GI bleeding m. b. responsible but the most important is colorectal
cancer.
• Investigations; IDA, faecal occult blood (FOB) test (Guaiac test), positive FOB test
necessitates upper and lower endoscopy.
………………………………………………………………………………………..
PEPTIC ULCER DISEASE
Learning objectives:
1. Review the functional anatomy and physiology of stomach and duodenum.
2. List the factors that responsible for normal mucosal defense mechanism against
ulcer formation.
3. Understand the concept of peptic ulcer disease (PUD).
4. Review the prevalence of PUD.
5. Explaine the pathophysiology and aetiology of PUD.
6. Clarify the pathological changes of PUD.
7. Recognize the clinical features of PUD.
8. Outline the important investigations of PUD.
9. Review the treatment of PUD.
10.List the complications of PUD.
Peptic Ulcer Disease:
Functional anatomy and physiology of stomach and duodenum;
• Stomach; The stomach acts as a 'hopper', retaining and grinding food, then actively
propelling it into the upper small bowel.
• It’s divided into four regions; the cardia, the fundus, the body, and the antrum: which
end by pyloric channal.
• The gastric rugae (or gastric folds) provide the stomach to increased surface when the
food in it.
• The mucosa, is formed by a layer of columnar epithelium, with numerous
invaginations of the surface epithelium into the lamina propria, which are
called gastric pits
• The muscularis mucosae, a thin layer of smooth muscle, forms the border between
the mucosa and submucosa.
• The submucosa, immediately deep to the mucosa, provides a dense connective tissue
in which lymphocytes, plasma cells, arterioles, venules, lymphatics, and the
myenteric plexus are contained.
Page of
11
105
Internal Medicine: 4
th
Stage TUCOM Dr.Hassan
• The third tissue layer, the muscularis propria, is a combination of an inner oblique, a
middle circular, and an outer longitudinal smooth muscle layer.
• The serosa, a thin, transparent continuation of the visceral peritoneum.
Gastric glands:
the gastric pits branched into four or five gastric glands made up of highly specialized
epithelial cells.
1. Parietal (Oxyntic) cells, which secrete both acid and intrinsic factor. Acid is
secreted in response to the activity of the hydrogen-potassium ATPase ('proton
pump') .
2. Chief cells, which secrete pepsinogen .
3. Enterochromaffin-like (ECL) cells, which secrete histamine .
4. G cells, which secrete gastrin .
5. D cells, which secrete somatostatin.
6. Mucus, secreting cells.
The duodenum:
• The most proximal portion of the small intestine, forms a C-shaped loop around the
head of the pancreas and is in continuity with the pylorus proximally and the jejunum
distally.
• Angular changes in course divide the duodenum into four portions. The first part of
the duodenum is the duodenal bulb or cap.
• The submucosal Brunner's glands that produce bicarbonate-rich secretions involved in
acid neutralization.
The mucosal defense system:
1. The first line of defense is a mucus-bicarbonate layer.
2. The next line of defense is the epithelial cells, intracellular tight junctions, cells
migration, and cell proliferation and renewal.
3. Prostaglandins are important in maintaining mucosal blood flow.
PEPTIC ULCER DISEASE:
• Peptic ulcer: refers to an ulcer in the lower oesophagus, stomach or duodenum, in the
jejunum after surgical anastomosis to the stomach or, rarely, in the ileum adjacent to a
Meckel's diverticulum, which penetrate the muscularis mucosae.
• Erosions; do not penetrate it.
• Ulcer may be acute or chronic, but acute ulcer show no evidence of fibrosis.
Gastric and duodenal ulcer:
• The prevalence of peptic ulcer is decreasing in Western communities as a result of
widespread use of H. pylori eradication therapy.
Page of
12
105
Internal Medicine: 4
th
Stage TUCOM Dr.Hassan
• It remains high in developing countries.
• Male to female ratio for duodenal ulcer varies from 5:1 to 2:1, whilst that for gastric
ulcer is 2:1 or less.
Pathophysiology and aetiology of PUD:
I. H. pylori infection;
A. The prevalence of H. pylori infection in developed world approxim. 50% of those
over the age of 50 yrs while 90% of the adult population in developing world are
infected.
B. The vast majority of colonized people remain healthy and asymptomatic.
C. 90% of duodenal ulcer patients and 70% of gastric ulcer patients are infected with
H. pylori.
D. H. pylori: Is Gram-negative, spiral and has multiple flagella at one end which make
it motile, allowing it to burrow and live deep beneath the mucus layer closely
adherent to the epithelial surface.
E. Production of the enzyme urease, this produces ammonia from urea and raises the
pH around the bacterium. It spread by person-to-person contact via gastric
refluxate or vomit.
F. H. pylori exclusively colonises gastric-type epithelium, in duodenum in assoctation
of gastric metaplasia. In most people H. pylori causes antral gastritis --depletion
of somatostatin (from D cells)---hypergastrinaemia --- increase acid production.
G. The majority of patients remains asyptomatic, but in some patients this effect is
exaggerated, leading to duodenal ulceration. The role of H. pylori in the
pathogenesis of gastric ulcer is less clear but it probably acts by reducing gastric
mucosal resistance to attack from acid and pepsin. In approximately 1% of infected
people, H. pylori causes a pangastritis leading to gastric atrophy and
hypochlorhydria ---gastric cancer.
H. The end result of H pylori infection:
1. Gastritis.
2. PUD.
3. Gastric MALToma.
4. Gastric cancer.
II. NSAIDs;
A. NSAIDs induce ulcer by reducing mucosal resist.– decr. Prostagl.– mucos. Injury.
B. RISK FACTORS FOR NSAID-INDUCED ULCERS:
1. Age > 60 years.
2. Past history of peptic ulcer.
3. Past history of adverse event with NSAIDs.
4. Concomitant corticosteroid use.
5. High-dose or multiple NSAIDs.
Page of
13
105
Internal Medicine: 4
th
Stage TUCOM Dr.Hassan
6. Individual NSAID-highest with azapropazone, piroxicam, ketoprofen; lower with
ibuprofen.
III. Zollinger-Ellison syndrome (ZES);
A. Gastrin-secreting tumors, accounts for 0.1% of causes of PUD.
B. Should be considered in patients with ulcers in unusual sites (e.g., distal
duodenum or jejunum); multiple, recurrent, or complicated duodenal ulcers; or
ulcers associated with chronic diarrhea.
IV. Smoking;
A. Increased risk of GU and, to a lesser extent DU, more complications and less
healing.
Pathology of PUD:
• Duodenal Ulcers mostly in the first portion of duodenum (>95%), Ulcers are sharply
demarcated, the base of the ulcer often consists of a zone of eosinophilic necrosis
with surrounding fibrosis. Malignant DUs are extremely rare.
• GUs can represent a malignancy, benign GUs are histologically similar to DUs.
Clinical features:
• The most common characteristics of abdominal pain suggestive of PUD:
-
Chronic recurrent abdominal pain with a history of spontaneous relapse and
remission lasting for decades.
-
Localisation to the epigastrium.
-
Relationship to food.
-
Episodic occurrence.
• Epigastric pain described as a burning or gnawing discomfort, hunger pain, relieved by
antacids or food, awakes the patient from sleep ,associated with weight gain.
• Vomiting occurs in about 40%; persistent daily vomiting suggests gastric outlet
obstruction.
• In some patients --silent ulcer; anaemia from chronic undetected blood loss.
• Complications; haematemesis, or acute perforation.
• The pain pattern in GU patients may be different from that in DU patients, where
discomfort may actually be precipitated by food. Nausea and weight loss occur more
commonly in GU patients.
Investigations of PUD:
1. Endoscopy: is the preferred investigation. Gastric ulcers must always be biopsied.
2. Barium studies: DU appears as a well-demarcated crater, most often seen in the
bulb. Benign GU also appears as a discrete crater with radiating mucosal folds
originating from the ulcer margin. Ulcers >3 cm in size or associ. with a mass are
more often malignant.
3. Tests for Detection of H. pylori infection.
Page of
14
105
Internal Medicine: 4
th
Stage TUCOM Dr.Hassan
Management:
The aims of management are to relieve symptoms, induce healing and prevent
recurrence.
1. H. pylori eradication.
2. General measures.
3. Short-term management.
4. Maintenance treatment.
5. Surgical treatment.
Regimens for H. Pylori eradication;
• First-line therapy is a proton pump inhibitor (12-hourly), clarithromycin 500 mg 12-
hourly, and amoxicillin 1 g 12-hourly or metronidazole 400 mg 12-hourly, for 10 days.
• Second-line therapy is a proton pump inhibitor (12-hourly), bismuth 120 mg 6-hourly,
metronidazole 400 mg 12-hourly, and tetracycline 500 mg 6-hourly, for 10 days.
• General measures; Cigarette smoking, aspirin and NSAIDs should be avoided
• Short-term management; after H pylori eradication ,followed by continuous acid
suppre. drugs ( H2 RB or PPI) for 4-6 wks.
• Maintenance treatment; GU need 8-12 wks to complete healing, with repeated
endoscopy and biopsy.
• Surgical treatment;
-
Emergency; Perforation, Haemorrhage.
-
Elective; Complications, e.g. gastric outflow obstruction. Recurrent ulcer following
gastric surgery.
Refractory ulcer:
• A GU that fails to heal after 12 weeks or DU after 8 weeks of therapy should be
considered refractory.
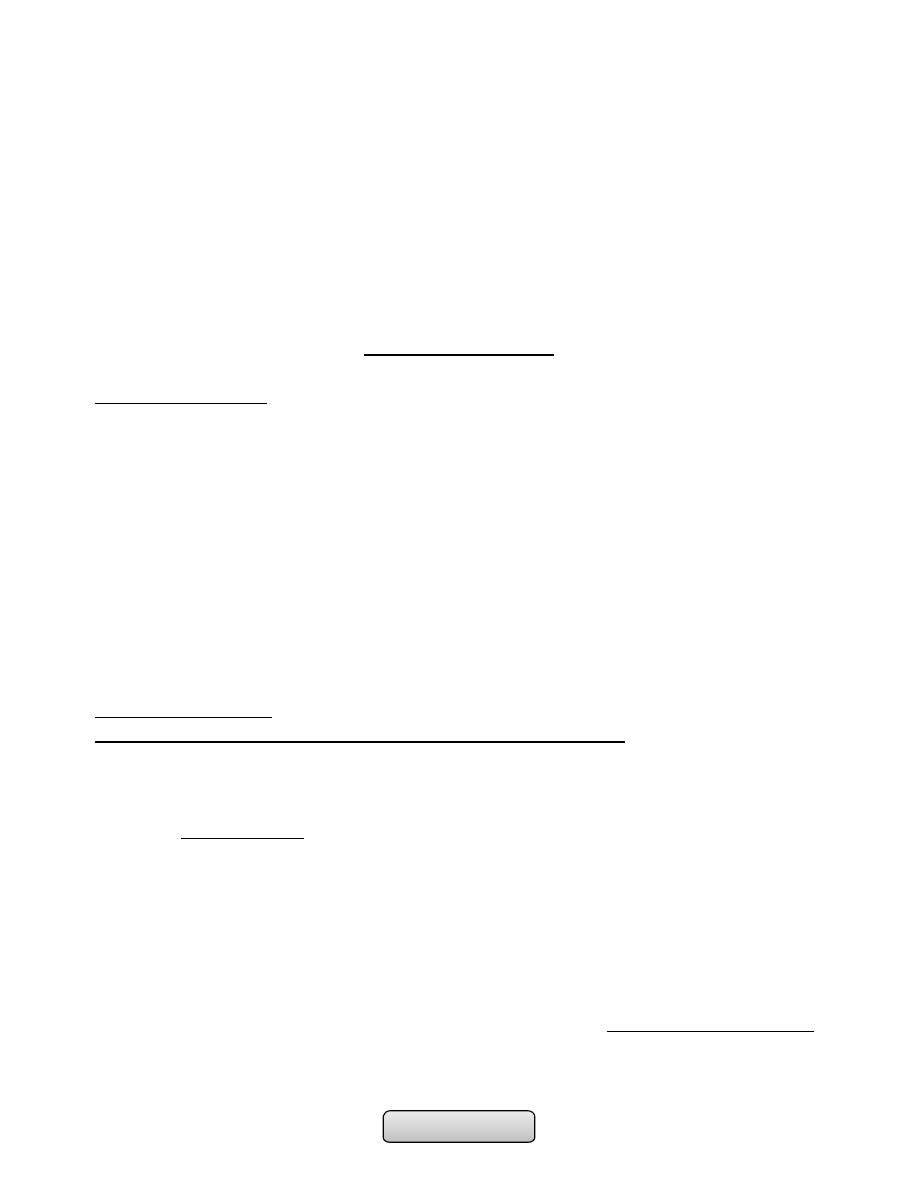
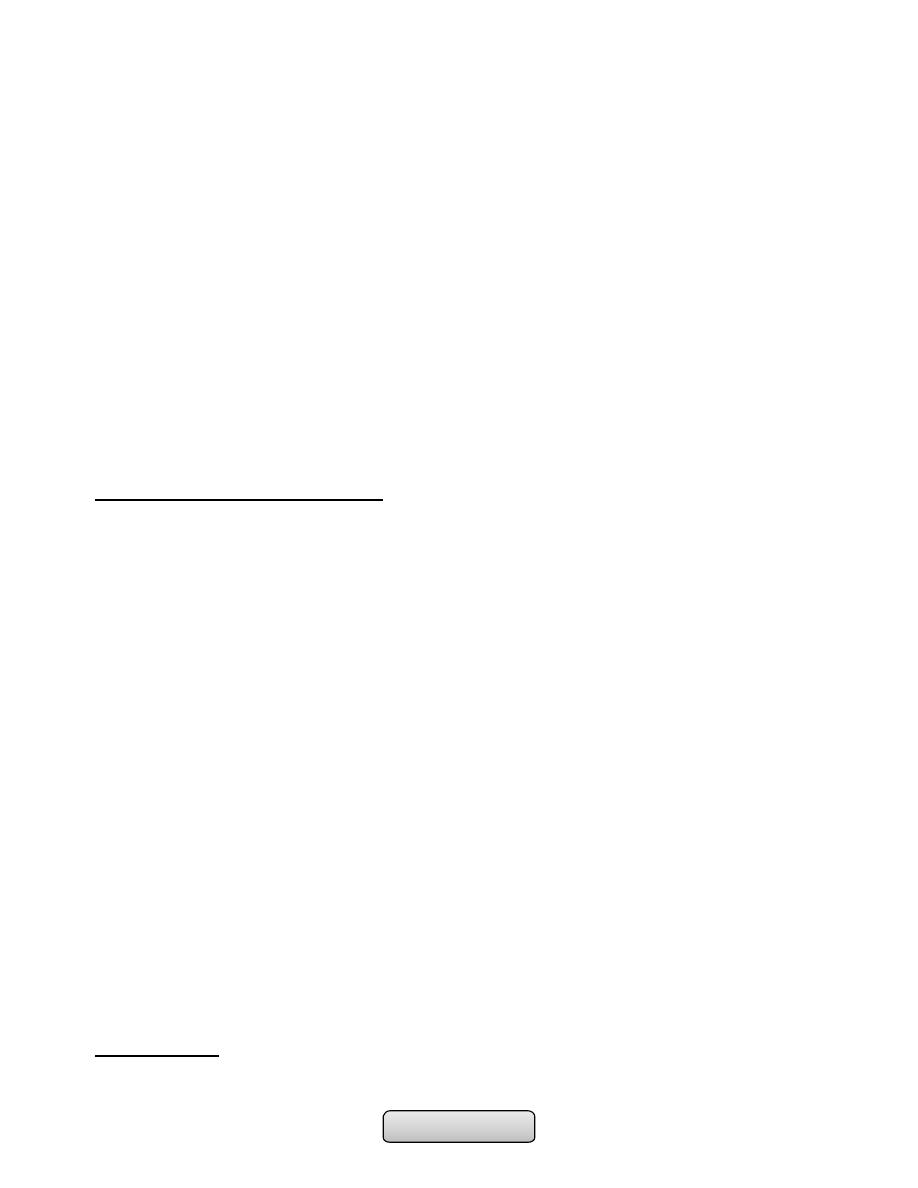
Test
Advantages
Disadvantages
NON-INVASIVE
Serology
Rapid kits available
Lacks sensiti and specif
Urea breath tests
High sensitivi and specifi
expensive
Faecal antigen test
Cheap, accurate
Acceptability
INVASIVE (ANTRAL BIOPSY)
Histology
Sensitivity and specificity
False negatives occur
Rapid urease tests
Cheap, quick, specifi.
Lack sensitivity
Microbiological culture
Gold standard'
Slow and laborious
Page of
15
105
Internal Medicine: 4
th
Stage TUCOM Dr.Hassan
• Common causes; poor compliance , persistent H. pylori infection, NSAID use,
cigarette smoking , GU malignancy and ZES.
Complications of peptic ulcer disease:
A. Complications of gastric resection or vagotomy:
1. Dumping.
2. Bile reflux gastritis.
3. Diarrhoea and maldigestion.
4. Weight loss.
5. Anaemia.
6. Metabolic bone disease.
7. Gastric cancer.
B. Complications of PUD it self:
1. Perforation.
2. Bleeding.
3. Gastric outlet obstruction
…………………………………………………………………………………………………..
Page of
16
105
Internal Medicine: 4
th
Stage TUCOM Dr.Hassan
TUMOURS OF THE STOMACH
Learning objectives:
1. Classify the gastric tumours.
2. Review the prevalence of gastric tumours.
3. Describe the pathophysiology, causes and risk factors of gastric tumours.
4. Explain the pathology of gastric tumours.
5. Clarify the clinical features of gastric tumours.
6. Understand the important investigations and staging of gastric tumours.
7. Explain the treatment of gastric tumours.
TUMOURS OF THE STOMACH:
1. GASTRIC CARCINOMA.
2. GASTRIC LYMPHOMA.
3. OTHER TUMOURS OF THE STOMACH; Gastrointestinal stromal cell tumours (GIST), a
variety of polyps, and gastric carcinoid tumours.
GASTRIC CARCINOMA:
• The incidence of gastric cancer in the UK has fallen markedly in recent years, It is
extremely common in China, Japan and parts of South America.
• Japanese migrants to the USA have much lower incidence in second-generation
migrants, confirming the importance of environmental factors.
• It is more common in men, after 50 years of age.
Aetiology;
1. H. pylori infection; is associated with chronic atrophic gastritis -- hypo- or
achlorhydria --- gastric cancer.
2. Diets; rich in salted, smoked or pickled foods and the consumption of nitrites and
nitrates may increase cancer risk. Diets lacking fresh fruit and vegetables as well
as vitamins C and A.
3. Smoking.
4. Alcohol.
5. Autoimmune gastritis (pernicious anaemia).
6. Adenomatous gastric polyps.
7. Previous partial gastrectomy (> 20 years).
8. Ménétrier's disease: It is a rare condition the gastric pits are elongated and
tortuous, with replacement of the parietal and chief cells by mucus-secreting
cells. As a result, the mucosal folds of the body and fundus are greatly enlarged.
Total gastrectomy specimen cut open to show giant gastric rugae and excessive
mucous secretion.
9. Hereditary diffuse gastric cancer families (HDC-1 mutations).
10.Familial adenomatous polyposis (FAP).
Page of
17
105
Internal Medicine: 4
th
Stage TUCOM Dr.Hassan
Pathology;
• Microscopically; All tumours are adenocarcinomas arising from mucus-secreting cells:
-
either 'intestinal', arising from areas of intestinal metaplasia, more common.
-
or 'diffuse', arising from normal gastric mucosa, poorly differentiated and occur in
younger patients.
• Macroscopically; Classified as polypoid, ulcerating, fungating or diffuse a scirrhous
cancer (linitis plastica):
-
Early gastric cancer; Is defined as cancer confined to the mucosa or submucosa,
regardless of lymph node involvement often recognized in Japan due to
widespread screening.
-
Advanced gastric cancer; Over 80% of patients in the Westren present at this
stage.
• Location; 50% in the antrum, 20-30% occur in the gastric body, 20% in the cardia, or
diffuse submucosal infiltration (uncommon).
Clinical features:
• Which depend on the location, size, and growth pattern of gastric cancer.
• Early gastric cancer is usually asymptomatic.
1. Dyspepsia.
2. Dysphagia.
3. Weight loss.
4. GI bleeding; Anaemia from occult bleeding, haematemesis, and melaena.
5. Palpable epigastric mass.
6. Pylorus/cardia obstruction.
7. Perforation.
8. Metastatic spread;
1. To the supraclavicular lymph nodes (Troisier's sign).
2. To umbilicus ('Sister Joseph's nodule').
3. To ovaries (Krukenberg tumour).
4. To the perirectal pouch (Blumer shelf).
5. Liver ---Jaundice.
6. Bone --- Bone pain.
7. Peritoneum --- Ascitis.
9. Paraneoplastic syndromes;
1. Thrombophlebitis (Trousseau's sign).
2. Acanthosis nigricans (pigmented dermal lesions).
3. Membranous nephropathy.
4. Microangiopathic hemolytic anemia.
5. Leser-Trélat sign (seborrheic keratosis).
6. Dermatomyositis.
Page of
18
105

Internal Medicine: 4
th
Stage TUCOM Dr.Hassan
Diagnosis and staging:
• Upper GI endoscopy; Is the investigation of choice in;
-
Dyspeptic patient with 'alarm features‘
-
New onset of dyspepsia in patient >55 years
-
Dyspepsia & family h/o gastric carcinoma
• Barium meal; is a poor alternative.
• CT abdomen; show evidence of intra-abdominal spread or liver metastases.
• Laparoscopy; is required to determine whether the tumour is resectable.
Management:
1. Surgery; cure can be achieved in 90% of patients with early gastric cancer by total
gastrectomy with lymphadenectomy, which is the operation of choice.
2. Unresectable tumours; for advanced cancer:
1. Chemotherapy; using FAM (5-fluorouracil, doxorubicin and mitomycin C) or ECF
(epirubicin, cisplatin and 5-fluorouracil).
2. Endoscopic laser ablation for dysphagia or recurrent bleeding.
3. Carcinomas at the cardia; endoscopic dilatation, laser therapy or insertion of
expandable metallic stents.
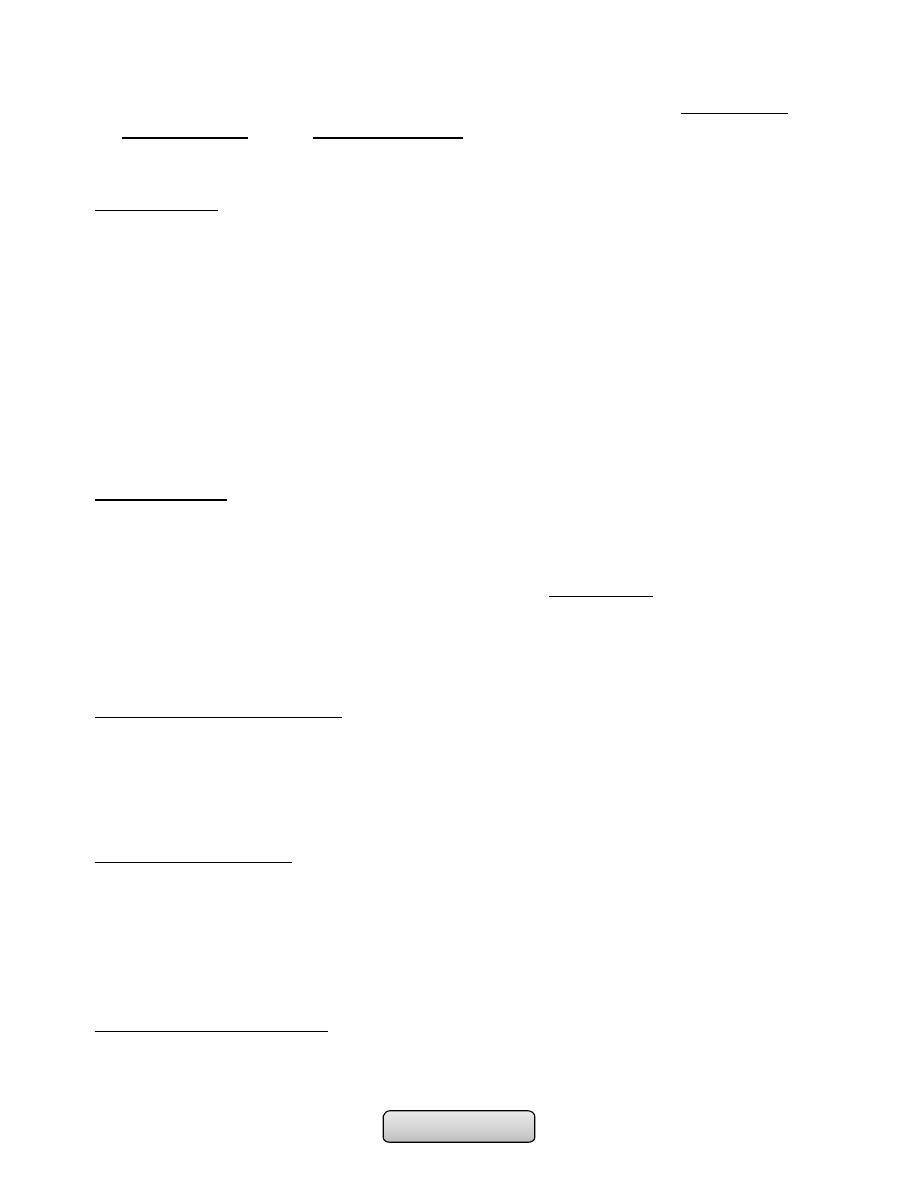
TNM staging of gastric cancer
T
Tis
Intaepithelial tumour
T1
Tumour invades submucosa
T2
Tumour invades muscularis
propria
T3
Tumour penetrates serosa
T4
Tumour invades adjacent
structures
N
N0
No regional lymph node
metastases
N1
Metastasis in 1 to 2 regional
lymph nodes
N2
Metastasis in 3 to 6 regional
lymph nodes
N3
Metastasis in 7 or more regional
lymph nodes
M
M0
No distant metastasis
M1
Distant metastasis
Page of
19
105
Internal Medicine: 4
th
Stage TUCOM Dr.Hassan
Prognosis:
• Remains very poor, with the exception of early gastric cancer. So endoscopic screening
of patients with new-onset dyspepsia in those over the age of 55years, or those with
'alarm' features, are essential.
GASTRIC LYMPHOMA:
• Primary gastric lymphoma accounts for less than 5% of all gastric malignancies.
• The stomach is the most common site for extranodal non-Hodgkin's lymphoma (NHL).
• Lymphoid tissue is not found in the normal stomach but lymphoid aggregates develop
in the presence of H. pylori infection.
• There are 2 types of gastric lymphoma;
1) Gastric mucosa associated lymphoid tissue lymphoma (MALToma); It is low-
grade lymphoma, H. pylori infection is closely associated.
2) Extranodal manifestation of high grade NHL.
• Clinical presentation; is similar to that of gastric cancer.
• Endoscopically; the tumour appears as a polypoid or ulcerating mass.
• Treatment;
-
Low-grade MALTomas consists of H. pylori eradication and close observation.
-
High-grade B-cell lymphomas are treated by a combination of chemotherapy,
surgery and radiotherapy.
• Prognosis; Depends on the type and stage of lymphoma at the time of diagnosis.
..............................................................................................................
FUNCTIONAL (NON-ULCER) DYSPEPSIA
Learning objectives:
1. Define functional dyspepsia.
2. List the causes of functional dyspepsia.
3. Review the clinical features of functional dyspepsia.
4. List the important investigations of functional dyspepsia.
5. Outline the management of functional dyspepsia.
FUNCTIONAL (NON-ULCER )DYSPEPSIA:
• Dyspepsia; is a collective symptoms thought to be originate from the upper
gastrointestinal tract, that may include pain or discomfort, bloating, feeling of
fullness with very little intake of food , feeling of early satiety, nausea, loss of
appetite or heartburn.
• Functional dyspepsia; chronic dyspepsia (more than 3 months) in the absence of
organic disease.
Page of
20
105
Internal Medicine: 4
th
Stage TUCOM Dr.Hassan
Aetiology;
• The pathophysiology of functional dyspepsia is unclear but probably due to mucosal,
motility, psychiatric disorders or H. pylori infection.
Clinical features;
• Usually young (< 40 years) women.
• Abdominal pain associated with a variable 'dyspeptic' symptoms( nausea and bloating
after meals).
• Morning symptoms are characteristic.
• A drug history, pregnancy, and alcohol misuse should be ruled out.
Examination;
• Usually negative apart from inappropriate tenderness on abdominal palpation, no
weight loss, patients may be anxious.
• Symptoms may appear disproportionate to clinical well-being.
Investigations;
1. Endoscopy is necessary to exclude mucosal disease.
2. Testing for H. pylori infection.
3. Ultrasound scan may detect gall stones.
Management;
• Explanation of symptoms and reassurance that the risk of cancer is very low in
absence of alarm features.
• Possible psychological factors should be explored.
• Give dietary advice; stop smoking, take regular meals, limit spicy, acidic and fatty
foods may be helpful.
• Review medications that may aggravating symptoms.
Drug treatment;
1. Antacids and alginates are sometimes helpful.
2. Prokinetic drugs such as metoclopramide or domperidone -- if nausea, vomiting or
bloating is prominent.
3. H
2
-receptor antagonists or PPI -- if night pain or heartburn is troublesome.
4. The role of H. pylori eradication remains controversial. Indicated in those who are
positive results. (Testing and treating for H. pylori) used as a role.
5. Low-dose amitriptyline is sometimes of value.
6. Some patients need behavioral or other formal psychotherapy.
………………………………………………………………………………………….
Page of
21
105

Internal Medicine: 4
th
Stage TUCOM Dr.Hassan
INFLAMMATORY BOWEL DISEASE
Inflammatory bowel disease (IBD):
• IBD refers to two ulcerative colitis and Crohn's disease which have relapsing and
remitting course, usually extending over years, precipitated by a complex interaction
of environmental, genetic, and immunoregulatory factors.
• The diseases have many similarities and it is sometimes impossible to differentiate
between them.
• A crucial distinction is that ulcerative colitis only involves the colon, while Crohn's
disease can involve any part of the gastrointestinal tract from mouth to anus.
• In developing world Crohn's disease appears to be very rare, but ulcerative colitis
becoming more common.
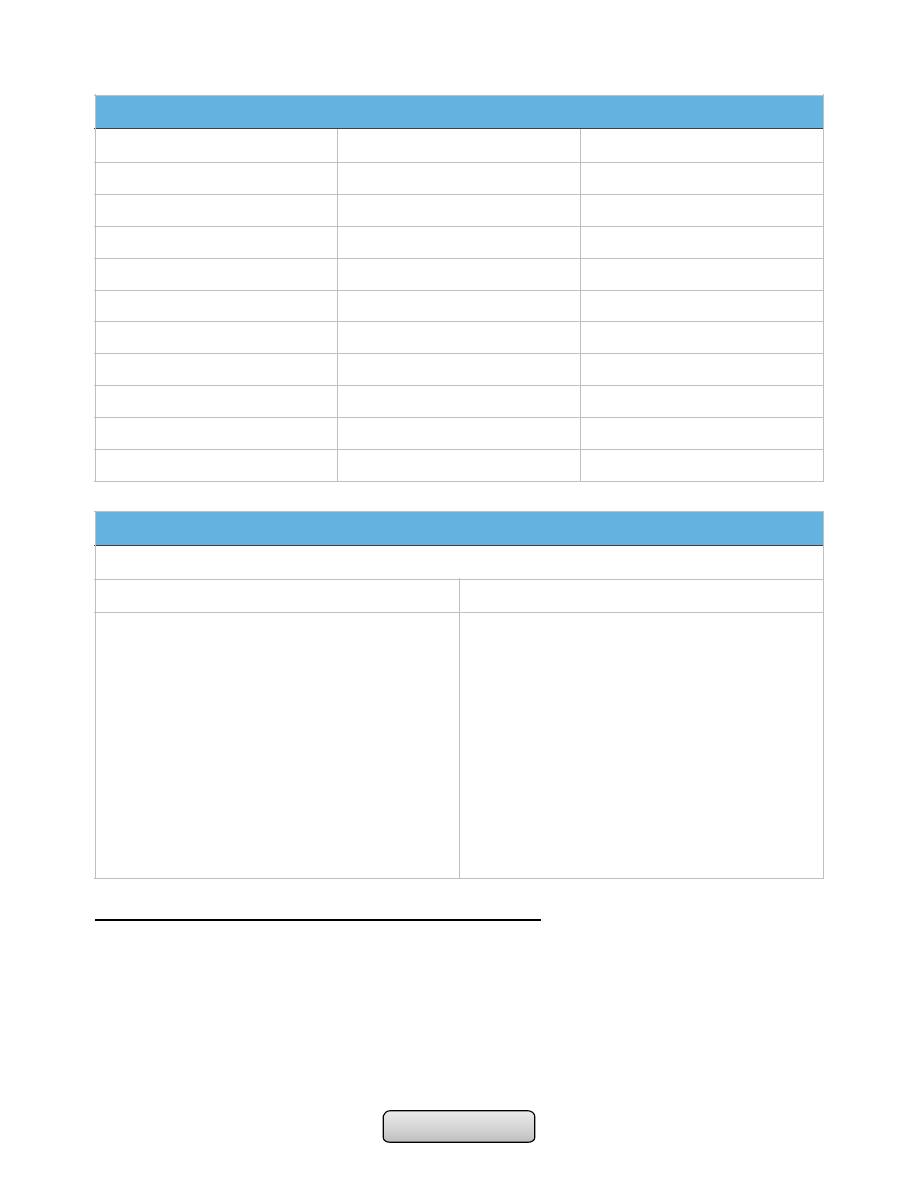
Comparison of ulcerative colitis and Crohn's disease
Ulcerative colitis
Crohn's disease
Age group
Any
Any
Gender
M = F
M = F
Ethnic group
Any
Any; more common in Ashkenazi Jews
Genetic factors
HLA-DR103 associated with
severe disease
CARD 15/NOD-2 mutations predispose
Risk factors
More common in non smokers.
Appendicectomy protects
More common in smokers
Anatomical distribution
Colon only; begins at anorectal
margin with variable proximal
extension
Confluent lesion
Any part of gastrointestinal tract; perianal
disease common; patchy
distribution-'skip lesions'
Extraintestinal
Common
Common
Presentation
Bloody diarrhoea
Variable; pain, diarrhoea, weight loss all
common
Histology
Inflammation limited to mucosa;
crypt distortion, cryptitis, crypt
abscesses, loss of goblet cells
Submucosal or transmural inflammation
common; deep fissuring ulcers, fistulas;
patchy changes; granulomas
Management
5-ASA; corticosteroids;
azathioprine; colectomy is curative
Corticosteroids; azathioprine;
methotrexate; biologic therapy (anti-
TNF); nutritional therapy; surgery for
complications, is not curative
Page of
22
105
Internal Medicine: 4
th
Stage TUCOM Dr.Hassan
Ulcerative colitis;
• Inflammation invariably involves the rectum (proctitis) but can spread to involve the
sigmoid colon (proctosigmoiditis) or the whole colon (pancolitis). Inflammation is
confluent and is more severe distally.
• In long-standing pancolitis the bowel can become shortened and 'pseudopolyps'
develop which are normal or hypertrophied residual mucosa within areas of atrophy.
• Both acute and chronic inflammatory cells infiltrate the lamina propria and the crypts
('cryptitis'). Crypt abscesses are typical.
Crohn's disease;
• The most common site involved is the terminal ileum and right side of colon.
• The entire wall of the bowel is oedematous and thickened, and there are deep ulcers
which often appear as linear fissures; thus the mucosa between them is described as
'cobblestone'.
• initiate abscesses or fistulas involving the bowel, bladder, uterus, vagina and skin of
the perineum.
• Crohn's disease has a patchy distribution and the inflammatory process is interrupted
by islands of normal mucosa.
Clinical features:
Ulcerative colitis:
• The major symptom is bloody diarrhoea. The first attack is usually the most severe
and thereafter the disease is followed by relapses and remissions. Emotional stress,
intercurrent infection, gastroenteritis, antibiotics or NSAID therapy may all provoke a
relapse.
• Proctitis or Proctosigmoiditis causes rectal bleeding and mucus discharge, sometimes
accompanied by tenesmus. Constitutional symptoms do not occur.
• Extensive colitis causes bloody diarrhoea with passage of mucus. In severe cases
anorexia, malaise, weight loss and abdominal pain occur, and the patient is toxic with
fever, tachycardia and signs of peritoneal inflammation.
• Factors considered for disease severity assessment in ulcerative colitis
Crohn's disease:
• The major symptoms are abdominal pain, diarrhea and weight loss.
• Ileal Crohn's disease may cause subacute or even acute intestinal obstruction or
watery diarrhea.
• Crohn's colitis presents in an identical manner to ulcerative colitis, but rectal sparing
and the presence of perianal disease are features which favour a diagnosis of Crohn's
disease.
• Many patients present with symptoms of both small bowel and colonic disease
• Few have isolated perianal disease, vomiting from jejunal strictures or severe oral
ulceration.
Page of
23
105
Internal Medicine: 4
th
Stage TUCOM Dr.Hassan
Differential diagnosis of small bowel Crohn's disease:
• Other causes of right iliac fossa mass
-
Caecal carcinoma
-
Appendix abscess
• Infection (tuberculosis, Yersinia, actinomycosis)
• Mesenteric adenitis
• Pelvic inflammatory disease
• Lymphoma
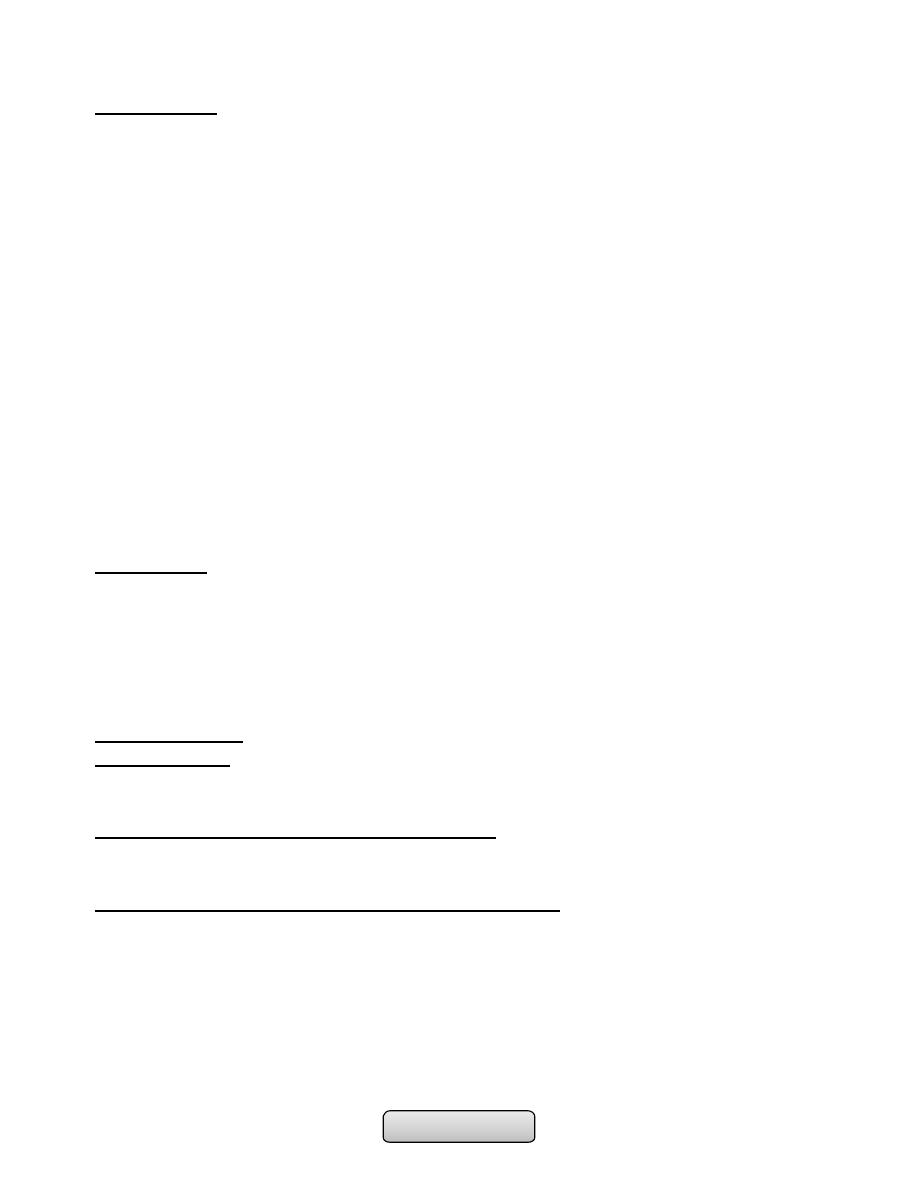
Factors considered for disease severity assessment in ulcerative colitis
Mild
Severe
Daily bowel frequency
< 4
> 6
Blood in stools
+/-
+++
Stool volume
< 200 g/24 hrs
> 400 g/24 hrs
Pulse
< 90 bpm
> 90 bpm
Temperature
Normal
> 37.8°C, 2 days out of 4
Sigmoidoscopy
Normal
Blood in lumen
Abdominal X-ray
Normal
Dilated bowel
Haemoglobin
Normal
< 100 g/L (< 10 g/dL)
ESR
Normal
> 30 mm/hr
Serum albumin
> 35 g/L (> 3.5 g/dL)
< 30 g/L (< 3 g/dL)
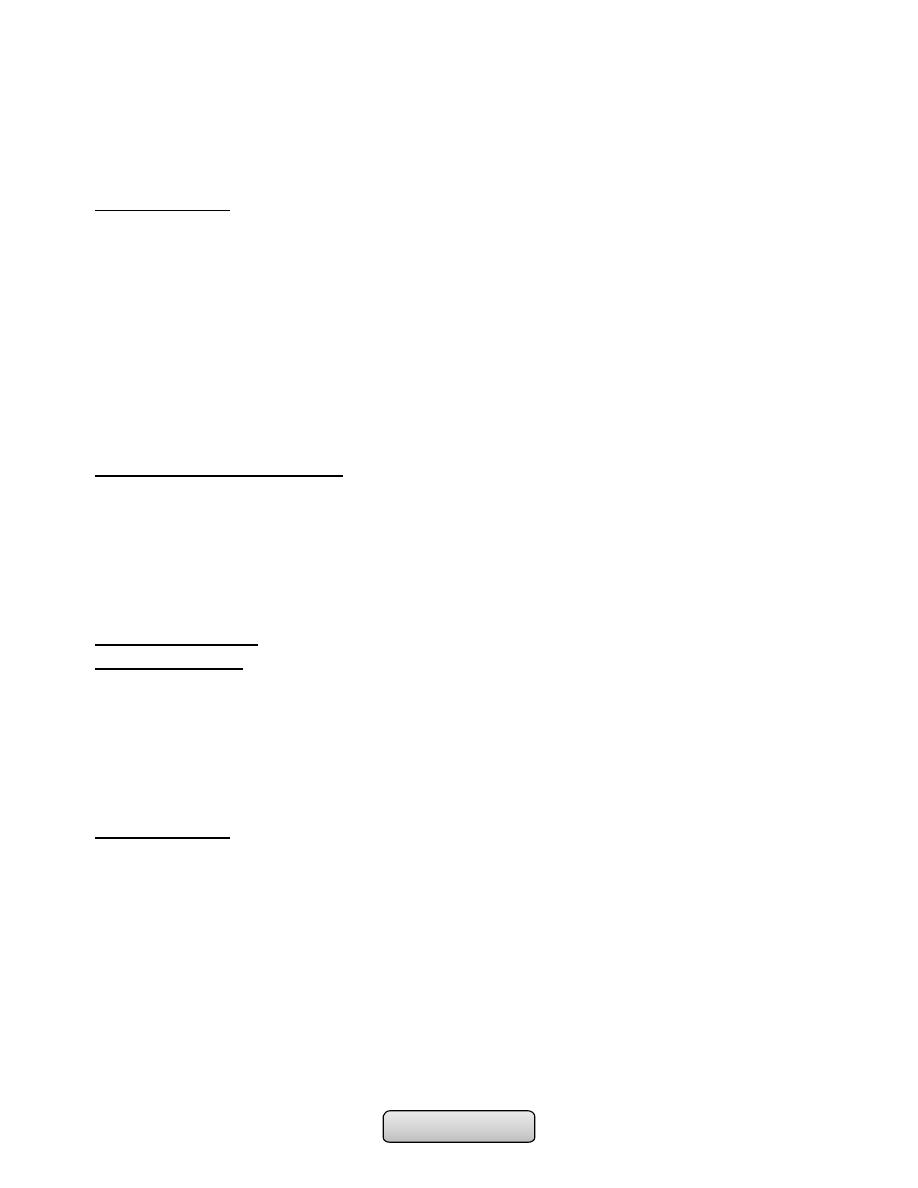
Differential diagnosis
Conditions which can mimic ulcerative or Crohn's colitis
Infective
Non-infective
• Bacterial:
-
Salmonella
-
Shigella
-
Campylobacter jejuni
-
E. coli O157
-
Gonococcal proctitis
-
Pseudomembranous colitis
-
Chlamydia proctitis
• Viral:
-
Herpes simplex proctitis
-
Cytomegalovirus
• Protozoal:
-
Amoebiasis
• Vascular:
-
Ischemic colitis
-
Radiation colitis
• Idiopathic:
-
Collagenous colitis, Behçet's disease
• Drugs: NSAIDs
• Neoplastic:
-
Colonic carcinoma
• Other:
-
Diverticulitis
Page of
24
105
Internal Medicine: 4
th
Stage TUCOM Dr.Hassan
Complications:
1. Life-threatening colonic inflammation;
• This can occur in both ulcerative colitis and Crohn's disease. In the most extreme
cases the colon dilates (toxic megacolon) and bacterial toxins pass freely across the
diseased mucosa into the portal then systemic circulation.
• An abdominal X-ray should be taken daily because when the transverse colon is
dilated to more than 6 cm there is a high risk of colonic perforation, although this
complication can also occur in the absence of toxic megacolon.
2. Haemorrhage; is due to erosion of a major artery is rare but can occur in both
conditions.
3. Fistulas; These are specific to Crohn's disease. Enteroenteric, Enterovesical,
Enterovaginal fistula and Fistulation from the bowel may also cause perianal or
ischiorectal abscesses, fissures and fistulas.
4. Cancer; The risk of colon cancer is increased in patients with long-standing,
extensive, active colitis of more than 8 years' duration.
Page of
25
105
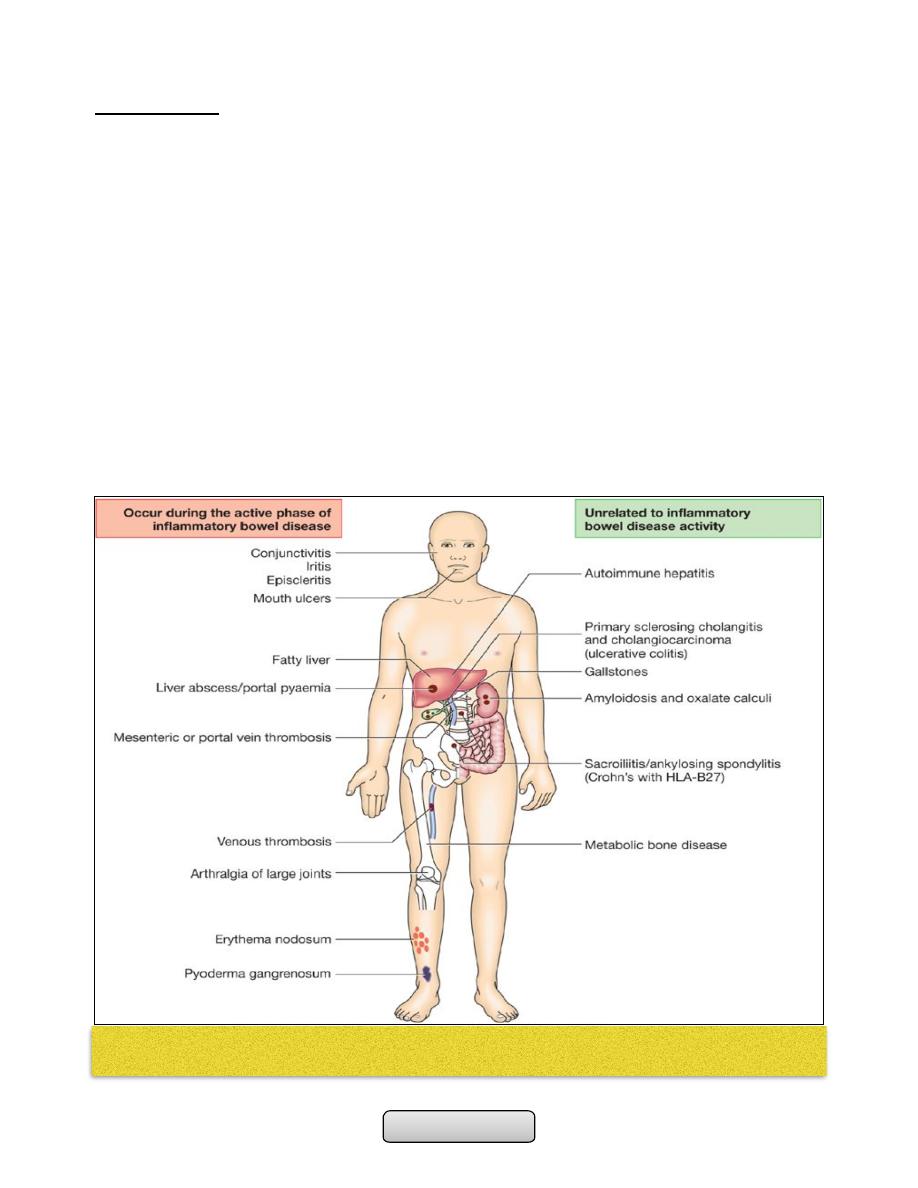
Extraintestinal complications are common in IBD and may dominate the clinical
Internal Medicine: 4
th
Stage TUCOM Dr.Hassan
Investigations:
1. General; Full blood count may show anaemia resulting from bleeding or malabsorption
of iron, folic acid or vitamin B
12
.
2. Endoscopy;
• Sigmoidoscopy with biopsy is an essential investigation in all patients who present
with diarrhoea, which show loss of vascular pattern, granularity, friability and
ulceration.
• Colonoscopy may show active inflammation with pseudopolyps or a complicating
carcinoma. Biopsies should be taken to confirm the diagnosis and define disease
extent, and also to seek dysplasia in patients with long-standing colitis.
3. Radiology;
• Barium enema is a less sensitive investigation than colonoscopy in patients with colitis
and is now little used.
• Contrast studies of the small bowel can be helpful in the investigation of Crohn's
disease; affected areas are narrowed and ulcerated, and multiple strictures are
common.
• MRI scans provide comparable information without radiation exposure or risking small
bowel obstruction and are useful in delineating pelvic or perineal involvement.
Management:
The key aims of treatment are to:
• Treat acute attacks
• Prevent relapses
• Detect carcinoma at an early stage
• Select patients for surgery.
Ulcerative colitis:
Active proctitis;
• Mesalazine enemas or suppositories combined with oral mesalazine are effective first-
line therapy.
Active left-sided or extensive ulcerative colitis;
• high-dose aminosalicylates combined with topical aminosalicylate and corticosteroids
are effective. Oral prednisolone 40 mg daily is indicated for more active disease.
Severe ulcerative colitis or fulminant ulcerative colitis:
• Intravenous fluids.
• Transfusion if Hb < 100 g/L.
• I.v. methylprednisolone (60 mg daily) or hydrocortisone (400 mg daily).
• Topical and oral aminosalicylates are also used.
• Antibiotics for proven infection.
• Nutritional support.
• Subcutaneous heparin for prophylaxis of venous thromboembolism.
Page of
26
105
Internal Medicine: 4
th
Stage TUCOM Dr.Hassan
• Avoidance of opiates and antidiarrhoeal agents.
• Consider intravenous ciclosporin or infliximab in stable patients not responding to 3-5
days of corticosteroids.
Crohn's disease:
• Patients with active colitis or ileocolitis:
-
Are initially treated in a similar manner to those with active ulcerative colitis.
-
Aminosalicylates and corticosteroids are both effective and usually induce
remission in active ileocolitis and colitis.
• Patients with isolated ileal disease; Should be treated with;
-
Corticosteroids
-
Aminosalicylates
-
Anti-TNF antibodies; infliximab
-
Oral metronidazole
Fistulas and perianal disease;
• Metronidazole and/or ciprofloxacin are first-line therapies.
• Thiopurines are used in chronic disease.
• Infliximab and adalimumab heal enterocutaneous fistulas and perianal disease in
many patients.
• Surgical intervention:.
Surgical treatment:
Ulcerative colitis:
• Impaired quality of life: Loss of occupation or education
• Failure of medical therapy
• Fulminant colitis
• Disease complications unresponsive to medical therapy: nArthritis or Pyoderma
gangrenosum
• Colon cancer or severe dysplasia
Crohn's disease:
• Similar to those for ulcerative colitis.
• Fistulas, abscesses and perianal disease.
• Small or large bowel obstruction.
……………………………………………………………………………………………..
Page of
27
105
Internal Medicine: 4
th
Stage TUCOM Dr.Hassan
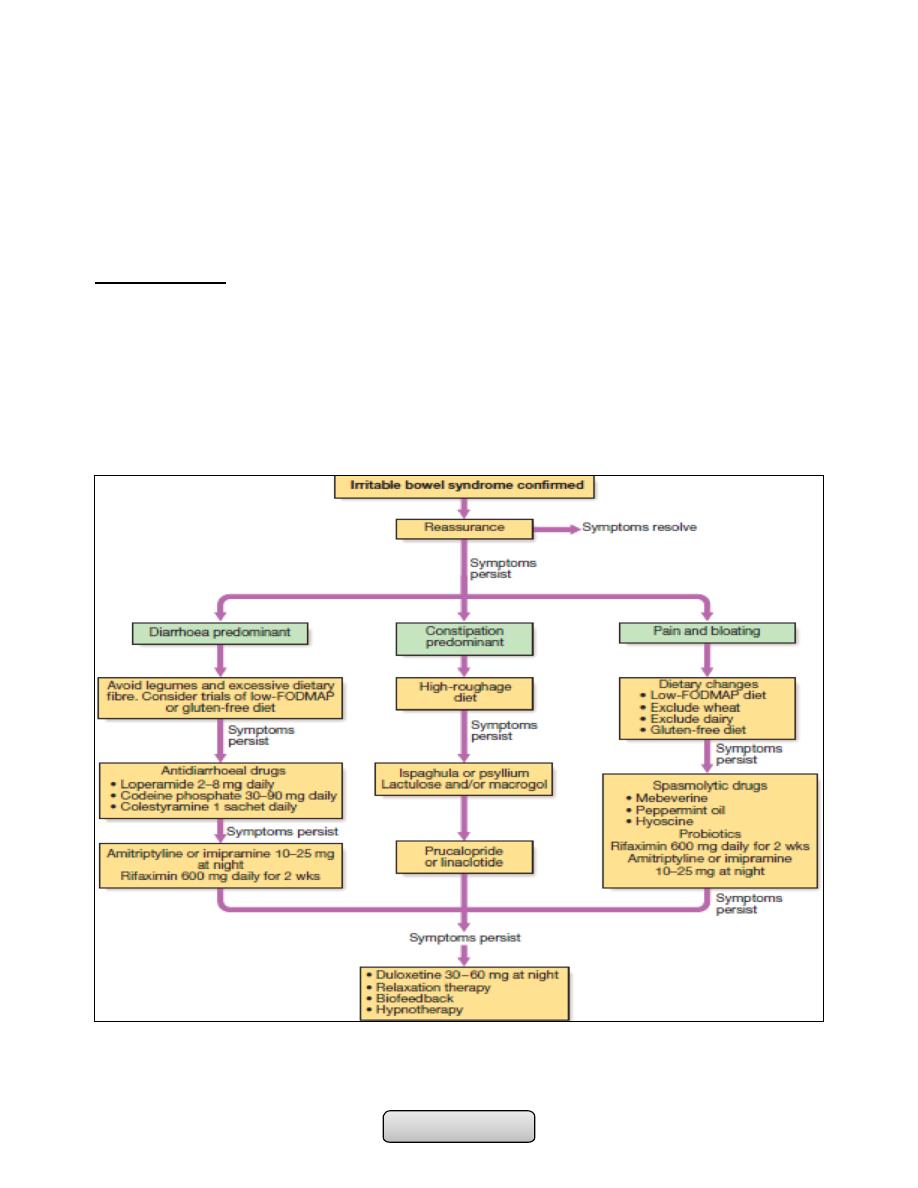
IRRITABLE BOWEL SYNDROME
Irritable bowel syndrome (IBS);
• Is a functional bowel disorder characterized by recurrent abdominal pain or
discomfort and altered bowel habits in the absence of structural abnormalities.
• diagnosis of the disorder is based on clinical presentation
• About 10–15% of the population are affected. Young women are affected 2–3 times
more often than men.
Pathophysiology;
The cause of IBS is incompletely understood but the following factors are thought to play
an important role;
1. Behavioural and psychosocial factors;
• Most patients do not have psychological problems but some patients have an anxiety
or depression.
2. Physiological factors;
• Relatively excessive release of 5-HT in diarrhoea-predominant IBS (D-IBS) and relative
deficiency with constipation-predominant IBS (C-IBS).
• Immune activation with raised numbers of mucosal mast cells.
3. Luminal factors;
• Alterations in intestinal bacterial contents (the gut microbiota) with small intestinal
bacterial overgrowth.
• Dietary factors are also important. Some patients have chemical food intolerances
(not allergy) to poorly absorbed, short-chain carbohydrates (lactose, fructose and
sorbitol, among others), collectively known as FODMAPs (fermentable oligo-, di- and
monosaccharides, and polyols). Their fermentation in the colon leads to bloating,
pain, wind and altered bowel habit.
• Noncoeliac gluten sensitivity (negative coeliac serology and normal duodenal biopsies)
seems to be present in some IBS patients
Clinical features;
• The most common presentation is that of recurrent abdominal discomfort (Rome III
criteria). This is usually colicky or cramping in nature, felt in the lower abdomen and
relieved by defecation. Associated with abdominal bloating worsens throughout the
day.
• There is an alteration of bowel habits, patients classify as having predominantly
constipation or predominantly diarrhoea.
Diagnosis;
• Based on Rome criteria combined with the absence of alarm symptoms, with normal
investigation results (Full blood count, with or without sigmoidoscopy).
Page of
28
105
Internal Medicine: 4
th
Stage TUCOM Dr.Hassan
Rome Ill criteria for diagnosis of irritable bowel syndrome:
• Recurrent abdominal pain or discomfort at least 3 days/mth in the last 3 months,
associated with two or more of the following:
-
Improvement with defecation.
-
Onset associated with a change in frequency of stool.
-
Onset associated with a change in form (appearance) of stool
Alarm features:
-
Age > 50 yrs; male gender
-
Family history of colon cancer.
-
Weight loss.
-
Anaemia.
-
Nocturnal symptoms.
-
Rectal bleeding.
………………………………………………………………………………………………
Page of
29
105
Internal Medicine: 4
th
Stage TUCOM Dr.Hassan
COLORECTAL CANCER
COLORECTAL CANCER:
• Colorectal cancer is the second most common internal malignancy and the second
leading cause of cancer deaths in Western countries (Lung is the first). But it is
relatively rare in the developing world. Why?
• It becomes increasingly common over the age of 50.
Aetiology:
Both genetic and environmental factors are important in colorectal carcinogenesis:
I. Genetic factors:
A. Accumulation of multiple genetic mutations.
B. Hereditary syndromes (autosomal dominant inheritance):
1. Nonpolyposis syndrome (Lynch syndrome).
2. Familial adenomatous polyposis (FAP).
II. Environmental factors;
A. Dietary factors are believed to be most important:
1. Increased risk:
a) Red meat.
b) Saturated animal fat.
2. Decreased risk.
a) Dietary fibre.
b) Fruit and Vegetables.
c) Calcium.
d) Folic acid.
e) Omega-3 fatty acids.
B. Non-dietary risk factors in colorectal cancer:
1. Medical conditions:
2. Colorectal adenomas.
3. Long-standing extensive ulcerative colitis or Crohn's colitis.
4. Ureterosigmoidostomy.
5. Acromegaly.
6. Pelvic radiotherapy.
C. Others:
1. Obesity and sedentary lifestyle.
2. Smoking.
3. Alcohol (weak association).
4. Cholecystectomy (effect of bile acids in right colon).
5. Type 2 diabetes (hyperinsulinaemia).
6. Streptococcus Bovis Bacteremia in individuals who develop endocarditis may
have a possible risk.
Page of
30
105
Internal Medicine: 4
th
Stage TUCOM Dr.Hassan
Risk factors for malignant change in colonic polyps:
1. Large size (> 2 cm)
2. Multiple polyps
3. Dysplastic polyp
Pathology:
• Most tumours arise from malignant transformation of a benign adenomatous polyp.
• Over 65% occur in the rectosigmoid
• Macroscopically, the majority of cancers are either polypoid and 'fungating', or
annular and constricting.
• Spread occurs through the bowel wall.
• Rectal cancers may invade the pelvic viscera and side walls.
• Lymphatic invasion is common at presentation, as is spread through both portal and
systemic circulations to reach the liver and, less commonly, the lungs.
Clinical features:
• Symptoms vary depending on the site of the carcinoma
• In tumours of the left colon, fresh rectal bleeding is common and obstruction occurs
early.
• Tumours of the right colon present with anaemia from occult bleeding, or altered
bowel habit, but obstruction is a late feature.
• Colicky lower abdominal pain is present in two-thirds of patients and rectal bleeding
occurs in 50%.
• A minority present with features of either obstruction or perforation, leading to
peritonitis, localized abscess or fistula formation.
• 10 and 20% of all patients present solely with iron deficiency anaemia or weight loss.
On examination:
• Signs of anaemia
• Low rectal tumours may be palpable on digital examination.
• If disease has spread to the abdomen, there may be a palpable mass, ascites, bowel
obstruction or hepatomegaly.
• Metastatic spread to the pelvic region may become evident as bladder dysfunction,
sciatic nerve pain, and vaginal discharge or bleeding.
• Lesions that have spread to the lung or bone marrow can remain silent until very
advanced disease is present.
Investigations:
• Double-contrast air-barium enema revealing tumor as filling defect or stricture with
apple-core appearance. If the test is positive colonoscopy should be undergo.
Page of
31
105

Internal Medicine: 4
th
Stage TUCOM Dr.Hassan
• Colonoscopy is the investigation of choice because it is more sensitive and specific
than barium enema. lesions can be biopsied and polyps removed.
• CT colography ('virtual colonoscopy') is a sensitive non-invasive technique for
diagnosing tumors and polyps greater than 1 cm that can be used if colonoscopy is
incomplete or high-risk.
• CT is valuable for detecting hepatic metastases and the extent of tumor spread.
• A proportion of patients have raised serum carcinoembryonic antigen (CEA)
concentrations but this is variable and so of little use in diagnosis. Measurements of
CEA are valuable, however, during follow-up and can help to detect early recurrence.
Management:
• Surgery;
-
The tumour is removed, along with adequate resection margins and pericolic
lymph nodes.
-
Post-operatively, patients should undergo colonoscopy after 6-12 months and
periodically thereafter to search for local recurrence
-
Two-thirds of patients have lymph node or distant spread (Dukes stage C) at
presentation and are, therefore, beyond cure with surgery alone.
• Adjuvant therapy;
-
5-fluorouracil and folinic acid (to reduce toxicity) for 6 months improves both
disease-free and overall survival in patients with Dukes C colon cancer by around
4-13%.
• Radiotherapy;
-
Pre-operative radiotherapy can be given to patients with large, fixed rectal
cancers to 'down-stage' the tumour, making it resectable and reducing local
recurrence.
-
Dukes C and some Dukes B rectal cancers are given post-operative radiotherapy to
reduce the risk of local recurrence if operative resection margins are involved.
• Palliative treatment:
-
Surgical resection to treat obstruction, bleeding or pain.
-
Palliative chemotherapy with 5-fluorouracil and folinic acid improves survival.
-
Pelvic radiotherapy is sometimes useful for distressing rectal symptoms such as
pain, bleeding or severe tenesmus
-
Endoscopic laser therapy or insertion of an expandable metal stent can be used to
relieve obstruction.
Prevention and screening:
1. Chemoprevention; The most promising agents at present are aspirin, calcium and folic
acid.
2. Secondary prevention (screening):
Page of
32
105
Internal Medicine: 4
th
Stage TUCOM Dr.Hassan
• Faecal occult blood (FOB) testing; In the USA, annual FOB screening is recommended
after the age of 50 years.
• Flexible sigmoidoscopy ; In the USA every 5 years in all persons over the age of 50.
• Colonoscopy; Remains the gold standard but requires expertise, is expensive and
carries risks; many countries lack the resources to offer this form of screening. In the
USA every 10 yr.
• Screening by molecular genetic analysis is an exciting prospect but is not yet
available.
• Faecal occult blood test (Guaiac test): In the presence of heme and a hydrogen
peroxide developer guaiac acid is oxidized producing a blue color.
……………………………………………………………………………………………
ACUTE AND CHRONIC HEPATITIS
Acute hepatitis:
• Hepatitis; is clinicopathologic conditions due to liver damage by viral, toxic,
metabolic, pharmacologic, or immune-mediated attack.
• Acute hepatitis; inflammation of liver lasting less than 6 months.
• Fate: Either complete resolution or rapid progression to fulminant hepatitis and acute
liver failure or slowly progress to chronic hepatitis.
Causes of Acute Hepatitis:
1. Viral Hepatitis; Hepatitis A virus, Hepatitis B virus Hepatitis C virus, Hepatitis D
virus ("delta agent") and Hepatitis E virus.
Other: Epstein-Barr virus Cytomegalovirus.
2. Alcohol.
3. Toxins; Amanita phalloides mushroom poisoning and Herbal preparations.
4. Drugs; Acetaminophen, Isoniazid, Halothane Phenytoin, Ketoconazole.
5. Other; Autoimmune hepatitis, Wilson's disease.
Acute Viral Hepatitis:
• This is a common cause of jaundice.
Page of
33
105
Internal Medicine: 4
th
Stage TUCOM Dr.Hassan
Serology:
• Hepatitis A:
-
Anti-HAV of IgM type, indicating a primary immune response, is already present in
the blood at the onset of the clinical illness and is diagnostic of an acute HAV
infection.
• Hepatitis B:
-
Acute infection the hepatitis B surface antigen (HBs Ag) is a reliable marker of HBV
infection
-
Anti-HBs Ab usually appears after about 3-6 months and persists for many years or
perhaps permanently
-
The hepatitis B core antigen (HBc Ag) is not found in the blood, but antibody to it
(anti-HBc) appears early in the illness and rapidly reaches a high titre which then
subsides gradually but persists. Anti-HBc is initially of IgM type while IgG antibody
appearing later.
-
The hepatitis B e antigen (Hbe Ag) appears only transiently at the onset of the
illness and is followed by the production of antibody (anti-HBe). The Hbe Ag
reflects active replication of the virus in the liver.
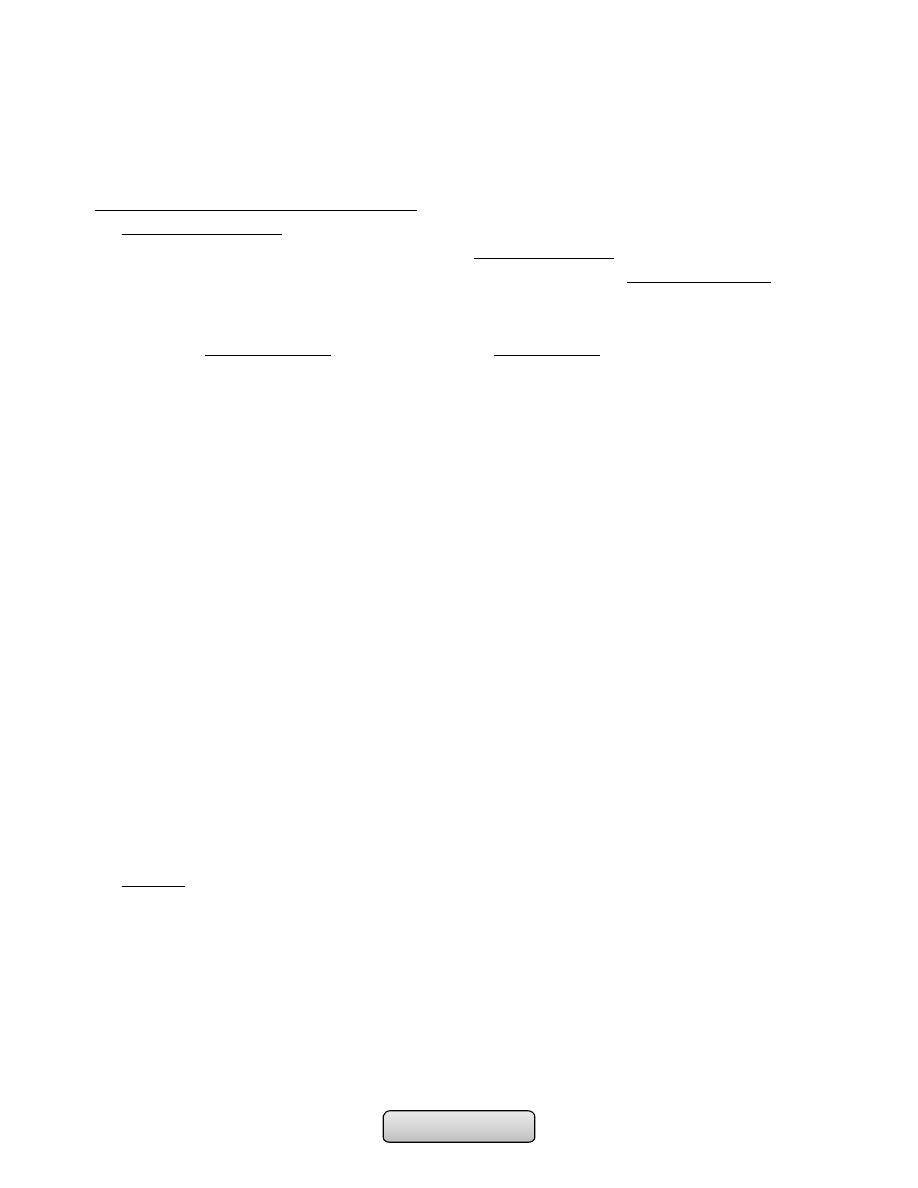
Hepatitis A
Hepatitis B
Hepatitis C
Hepatitis D
Hepatitis E
Group
Enterovirus
picornavirus
Hepadna
Flavivirus
Incomplete
virus
Calicivirus
Nucleic acid
RNA
DNA
RNA
RNA
RNA
Size (diameter) 27 nm
42 nm
30-38 nm
35 nm
27 nm
Incubation
(weeks)
2-4
4-20
2-26
6-9
3-8
Spread
Faeces
Yes
No
No
No
Yes
Blood
Uncommon
Yes
Yes
Yes
No
Saliva
Yes
Yes
Yes
?
?
Sexual
Uncommon
Yes
Uncommon
Yes
?
Vertical
No
Yes
Uncommon
Yes
No
Chronic
infection
No
Yes
Yes
Yes
No
Prevention
Active
Vaccine
Vaccine
No
Prevented by
No
Passive
Immune serum
globulin
Hyperimmune
serum globulin
No
Hepatitis B
vaccination
No
Page of
34
105
Internal Medicine: 4
th
Stage TUCOM Dr.Hassan
-
The persistence of HBs Ag for longer than 6 months indicates chronic infection.
-
Chronic HBV infection is marked by the presence of HBs Ag and anti-HBc (IgG) in
the blood.
-
HBV-DNA can be measured by polymerase chain reaction (PCR) in the blood. Viral
loads are usually in excess of 105 copies/ml in the presence of active viral
replication.
• Hepatitis D:
-
HDV contains a single antigen to which infected individuals make an antibody
(anti-HDV) initially IgM and later IgG.
• Hepatitis C:
-
Eighty per cent of individuals exposed to the virus will become chronically infected
-
hepatitis C RNA can be identified in the blood as early as 2-4 weeks after
infection.
-
Active infection is confirmed by the presence of serum hepatitis C RNA in anyone
who is antibody positive.
Clinical features of viral hepatitis:
1. Prodromal phase;
• Which last for several days and characterized by malaise, fatigue, anorexia, nausea,
vomiting, myalgia, headache, and mild fever.
• Arthritis and urticaria (serum sickness) due to immune complex deposition, may be
present in 5 to 10% of cases of acute hepatitis B and C.
• Taste and smell alteration.
2. Icteric phase;
• Jaundice appear after few days to 2 weeks.
• Dark urine and pale stools.
• Improvement in the patient's well-being.
• Splenomegaly is found in about one-fifth of patients.
• Anicteric phase; Symptoms without jaundice.
• Laboratory;
-
Aminotransferases (ALT & AST) serum levels rise to greater than 20- 100 fold
normal.
-
An elevated serum bilirubin (>2.5 to 3.0 mg/dL) or higher than 20 mg/dL.
-
Serum alkaline phosphatase when it rise to more three times of normal levels
indicate cholestatic hepatitis.
-
Prolongation of the prothrombin time in sever hepatitis.
-
Serological tests confirm the aetiology of the infection.
3. Recovery phase; Gradual resolution of symptoms and laboratory values.
Complications:
1. Cholestatic hepatitis.
Page of
35
105
Internal Medicine: 4
th
Stage TUCOM Dr.Hassan
2. Acute liver failure.
3. Chronic hepatitis.
4. Aplastic anemia.
5. Relapsing hepatitis.
Management:
1. Supportive treatment;
• Rest.
• Maintenance of hydration and adequate dietary intake.
• Alcohol should be avoided.
• Hospitalization if severe nausea and vomiting or deterioration of liver function.
• Drugs such as sedatives and narcotics should be avoided.
• Elective surgery should be avoided.
• Acute hepatitis C; α-interferon may decrease the risk of chronicity.
• Vitamin K indicated if prolonged cholestasis.
2. Liver transplantation;
• Very rarely indicated, when the patient developed acute liver failure.
Chronic Hepatitis:
• Defined as a hepatic inflammatory process lasting more than 6 months.
Causes of Chronic Hepatitis;
1. Viral Hepatitis; B, C and Hepatitis B with superimposed hepatitis D.
2. Alcoholic hepatitis.
3. Nonalcoholic steatohepatitis.
4. Drugs and Toxins; Methyldopa, Nitrofurantoin, Amiodarone, Captopril,
Propylthiouracil.
5. Autoimmune
6. Genetic and Metabolic Disorders; Wilson's disease, and α
1
-Antitrypsin deficiency.
Classification:
A. Initial classification; which depend on histopathology only;
1. Chronic persistent hepatitis; inflammatory activity confined to portal areas --
good prognosis.
2. Chronic lobular hepatitis; inflammatory activity and necrosis scattered
throughout the lobule -- good prognosis.
3. Chronic active hepatitis; inflammation that spilled into the adjacent lobule
associated with necrosis and fibrosis, which progress to cirrhosis and liver
failure.
B. Recent classification; which depend on;
1. Etiologic agent
Page of
36
105
Internal Medicine: 4
th
Stage TUCOM Dr.Hassan
2. Grade of injury (numbers and location of inflammatory cells)
3. Stage of disease (degree and location of fibrosis)
Chronic hepatitis B:
• Route of transmission and risk of chronic infection
• Horizontal transmission (10%); Injection drug use, infected unscreened blood
products, tattoos/acupuncture needles, sexual.
• Vertical transmission (90%); From HBs Ag positive mother.
Clinical features:
• Asymptomatic, fatigue, jaundice, malaise and anorexia, may progress to liver failure.
• Extrahepatic features; Arthralgias and arthritis, glomerulonephritis, and vasculitis ,
due to immune complexes deposition.
Invx;
• Aminotransferases elevated. HBs Ag +ve, HBe Ag +ve, and anti-HBc IgG Ab +ve.
Treatment:
• Indication for treatment; High viral load, elevated serum transaminases and/or
histological evidence of inflammation.
-
Alfa-interferon or longer-acting pegylated interferons; that augmenting immune
response.
-
Lamivudine; Nucleoside analogue which inhibits DNA polymerase and suppresses
HBV-DNA levels.
-
Adefovir; Nucleotide analogue which inhibits HBV-DNA polymerase.
• Liver transplantation.
Chronic Hepatitis D;
• Chronic hepatitis B plus D has similar clinical and laboratory features to those seen in
chronic hepatitis B alone– but more severe chronic hepatitis or cirrhosis.
• Preventing hepatitis B effectively prevents hepatitis D.
• Anti-HDV IgG titer is high.
Chronic Hepatitis C:
• 75% will become chronically infected.
Clinical features;
• Similar to chronic hepatitis B, fatigue common, but jaundice is rare.
• Extrahepatic features; Essential mixed cryoglobulinemia , Sjögren's syndrome, lichen
planus, and porphyria cutanea tarda.
• Progress to cirrhosis and hepatocellular carcinoma.
Page of
37
105
Internal Medicine: 4
th
Stage TUCOM Dr.Hassan
Invx;
• Presence of serum hepatitis C RNA in anyone who is antibody-positive.
• Liver histology degree of liver fibrosis
Treatment;
• Pegylated α-interferon together with oral ribavirin, a synthetic nucleotide analogue.
• Liver transplantation:
Alcoholic hepatitis:
• Alcohol is one of the most common causes of chronic liver disease (ALD) worldwide
• A unit of alcohol contains 8 g of ethanol. Consumption of more than 80 g/day, for
more than 5 years, is required to confer significant risk of advanced liver disease
Risk factors for ALD are:
• Drinking pattern; liver damage is more likely to occur in continuous rather than
intermittent or ‘binge’ drinkers, Gender; more in women, Genetics, Nutrition; more
in obese
Pathophysiology;
• 80% of alcohol is metabolised to acetaldehyde that activate the immune system,
contributing to cell injury. 20% of alcohol is metabolised by Cytochrome CYP2E1 lead
to hepatotoxicity from low doses of paracetamol.
C/F;
• Jaundice, malnutrition, hepatomegaly or features of portal hypertension (e.g.
ascites,encephalopathy)
Investigations;
• AST elevated to higher degree than ALT , GGT also elevated, increase s. bilirubin,
macrocytosis in the absence of anaemia, PT increase and albumin decrease in sever
liver dysfunction, liver biopsy to show extent of liver damage
Management;
• Cessation of alcohol consumption
• Good nutrition is very important
• Corticosteroids have a value in the treatment of severe alcoholic hepatitis
• Pentoxifylline, which has a weak anti-TNF action, may be beneficial in severe
alcoholic hepatitis.
• Liver transplantation have a good prognosis if the patient remains abstinent from
alcohol.
Page of
38
105
Internal Medicine: 4
th
Stage TUCOM Dr.Hassan
Non-alcoholic steatohepatitis:
• Most common in persons who are overweight, diabetes, and hyperlipidemia.
Clinical features;
Asymptomatic; As abnormal LFTs.
Complication;
Cirrhosis, variceal haemorrhage or hepatocellular carcinoma.
U/S; liver will appear bright.
Liver biopsy; fat deposition is usually macrovesicular, neutrophil infiltration and fibrosis.
Treatment;
• Weight reduction
• Vitamin E (as an antioxidant)
• Lipid-lowering agents, particularly gemfibrozil.
• Drugs that improve insulin resistance like metformin.
Autoimmune hepatitis:
• Is a liver disease of unknown aetiology
• Association with other autoimmune diseases
• Hypergammaglobulinaemia and autoantibodies
• Young women
• Insidious, with fatigue, anorexia, jaundice, fever, arthralgia, and vitiligo.
• Spider naevi ,hepatosplenomegaly, 'cushingoid' face with acne, hirsutism and pink
cutaneous striae.
Investigations;
• Antinuclear antibodies, anti-smooth muscle antibody and antimicrosomal antibodies
(anti-LKM) are positive. Increase IgG level.
Treatment;
• With corticosteroids, Azathioprine for maintenance.
GENETIC AND METABOLIC HEPATITIS:
• Wilson's disease and α
1
-antitrypsin deficiency
• Before the age of 35 years
• Family history of liver disease
Wilson's disease:
• Wilson's disease is a rare, autosomal recessive disorder of copper metabolism that is
caused by a variety of mutations in the gene ATP7B on chromosome 13. Total body
copper is increased, with excess copper deposited in, and causing damage to, several
organs.
• Hepatic disease occurs predominantly in childhood and early adolescence.
Page of
39
105
Internal Medicine: 4
th
Stage TUCOM Dr.Hassan
• Neurological damage causes basal ganglion syndromes and dementia which tends to
present in later adolescence.
• Others include renal tubular damage and osteoporosis.
• Kayser-Fleischer rings the most important single clinical clue to the diagnosis and can
be seen in 60% of adults.
• Diagnosis and treatment:
-
Low serum caeruloplasmin is the best single laboratory clue to the diagnosis. high
free serum copper concentration. high urine copper excretion of greater than 0.6
µmol/24 hrs and a very high hepatic copper content
-
The copper-binding agent penicillamine is the drug of choice.
Alpha
1
-antitrypsin deficiency:
• Alpha
1
-antitrypsin (α
1
-AT) is a serine protease inhibitor (Pi) produced by the liver. It’s
gen located on chromosome 14. which described as medium (M), slow (S), and very
slow (Z). Homozygous individuals (PiZZ) have low plasma α
1
-AT concentrations, these
forms cannot be secreted into the blood by liver cells because it is polymerised within
the endoplasmic reticulum of the hepatocyte, that leads to hepatic and pulmonary
disease.
• Liver disease includes chronic hepatitis and cirrhosis in adults, and in the long term
hepatocellular carcinoma. Lung disease including emphysema in adult life.
• Diagnosis and treatment:
-
Diagnosis is made from the low plasma α1-AT concentration and the PiZZ genotype.
-
No specific treatment is available; Life style modification: correct obesity, stop
smoking and alcohol. Treat the complicatios of CLD. Liver tansplantation if end
stage liver dis.
…………………………………………………………………………………………….
LIVER CIRRHOSIS & ITS COMPLICATIONS
Liver Cirrhosis:
• Liver cirrhosis; Is the irreversible fibrous scarring and hepatocellular regeneration that
leads to loss of normal hepatic lobular architecture.
• Small (<3 mm; micronodular cirrhosis):
-
A typical feature of alcoholic cirrhosis.
• Large (>3 mm; macronodular cirrhosis):
-
Is more commonly seen as a sequelae to chronic active hepatitis.
Causes:
1. Alcohol.
2. Chronic viral hepatitis B, D or C.
3. Non-alcoholic fatty liver disease.
Page of
40
105
Internal Medicine: 4
th
Stage TUCOM Dr.Hassan
4. Immune:
1) Primary sclerosing cholangitis.
2) Autoimmune liver disease
5. Biliary
1) Primary biliary cirrhosis.
2) Cystic fibrosis
6. Genetic
1) Haemochromatosis.
2) α
1
-antitrypsin deficiency.
3) Wilson's disease
7. Cryptogenic (unknown).
Primary biliary cirrhosis (PBC):
• PBC Is a chronic, progressive cholestatic liver disease of unknown cause which
predominantly affects middle-aged women.
Clinical features;
• lethargy, arthralgia, pruritus, jaundice. Bone pain or fractures due to osteomalacia
(fat-soluble vitamin malabsorption). Scratch marks, Xanthelasma, later on patients
develops portal hypertension and liver failure.
Investigations;
• LFTs show a pattern of cholestasis. Antimitochondrial antibody is diagnostic. Liver
biopsy shows a granuloma formation of the portal tracts, leading to progressive
damage and eventually loss of the small and middle-sized bile ducts.
Management;
• Ursodeoxycholic acid (UDCA) improves bile flow, improves LFTs and reduces apoptosis
of the biliary epithelium. Liver transplantation should be considered.
Primary sclerosing cholangitis:
• Is a cholestatic liver disease caused by diffuse inflammation and fibrosis that can
involve the entire biliary tree and leads to the gradual obliteration of intrahepatic
and extrahepatic bile ducts, and ultimately biliary cirrhosis, portal hypertension and
hepatic failure. Cholangiocarcinoma develops in about 10-30% of patients during the
course of the disease.
• ERCP is usually diagnostic and may reveal multiple irregular stricturing and dilation.
• Histological appearances characteristic are periductal 'onion-skin' fibrosis and
inflammation.
• Management; There is no cure for primary sclerosing cholangitis
Page of
41
105
Internal Medicine: 4
th
Stage TUCOM Dr.Hassan
Haemochromatosis:
• Is a condition in which the amount of total body iron is increased; the excess iron is
deposited in and causes damage to several organs including the liver. It may be
primary or secondary to other diseases . Iron is deposited throughout the body and
total body iron may reach 20-60 g (normally 4 g).
• Hereditary haemochromatosis (HHC): It is caused by increased absorption of dietary
iron and is inherited as an autosomal recessive gene located on chromosome 6.
• Usually presents in men aged 40 years or over with features of hepatic cirrhosis
(especially hepatomegaly), diabetes mellitus or heart failure. Arthropathy, Leaden-
grey skin pigmentation due to excess melanin occurs, especially in exposed parts,
axillae, groins and genitalia; hence the term 'bronzed diabetes'. Impotence, loss of
libido, testicular atrophy and arthritis with chondrocalcinosis secondary to calcium
pyrophosphate deposition are also common. Cardiac failure or cardiac dysrhythmia
may complicate heart muscle disease.
• Serum ferritin is greatly increased; the plasma iron is also increased, with a highly
saturated plasma iron-binding capacity. The diagnosis is confirmed by liver biopsy,
which shows heavy iron deposition and hepatic fibrosis which may have progressed to
cirrhosis.
• Treatment consists of weekly venesection of 500 ml blood (250 mg iron) until the
serum iron is normal, this may take 2 years or more.
Clinical features of liver cirrhosis:
• Hepatomegaly (although liver may also be small)
• Jaundice
• Ascites
• Circulatory changes
-
Spider telangiectasia, palmar erythema, cyanosis.
• Endocrine changes
-
Loss of libido, hair loss
-
Men: gynaecomastia, testicular atrophy, impotence
-
Women: breast atrophy, irregular menses, amenorrhea
• Hemorrhagic tendency
-
Bruises, purpura, epistaxis, menorrhagia.
• Portal hypertension
-
Splenomegaly, collateral vessels (caput medusa), variceal bleeding (oesophageal,
gastric and rectal varices), fetor hepaticus.
• Hepatic (portosystemic) encephalopathy
• Other features
-
Pigmentation, digital clubbing, duputryn's contracture, Pruritus.
Page of
42
105
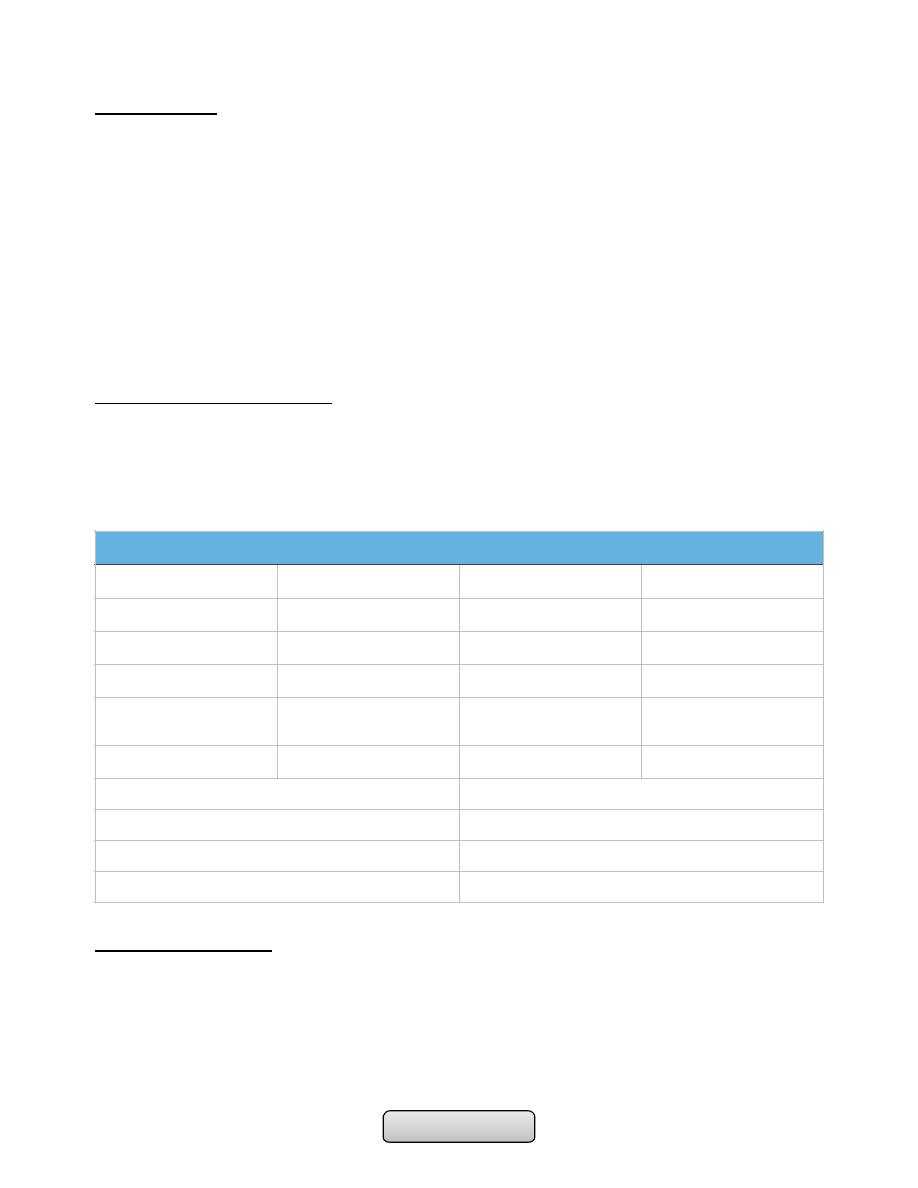
Internal Medicine: 4
th
Stage TUCOM Dr.Hassan
Investigations:
A. Laboratory Features;
• Hepatocellular dysfunction; (Hypoalbuminemia and prolonged PT),
hyperbilirubinemia, low blood urea; and elevated ammonia levels.
• Portal hypertension; Thrombocytopenia and leukopenia.
• Anemia; Hypersplenism or GI bleeding.
B. Radiologic features; includes U/S of abdomen with or without Doppler of the portal
and hepatic venous vessels. CT or MRI; which show liver atrophy with nodular surface
and features of portal hypertension.
C. liver biopsy; no need in the presence of clinical and laboratory features but may be
considered when the cause of liver disease is doubtful.
Treatment of liver cirrhosis:
• Treatment of any known cause.
• The maintenance of nutrition.
• Treatment of the complications of cirrhosis.
• Liver transplantation
Major Complications:
1. Hepatocellular dysfunction and portal hypertension, which may result in;
a) Variceal hemorrhage.
b) Ascites, which can be further complicated by spontaneous bacterial peritonitis.
c) Hepatic encephalopathy.
d) Hepatorenal syndrome.
Prognosis; Child-Pugh classification of prognosis in cirrhosis
1
2
3
Encephalopathy
None
Mild
Marked
Bilirubin (μmol/l)
< 34
34-50
> 50
Albumin (g/l)
> 35
28-35
< 28
Prothrombin time
(seconds prolonged)
< 4
4-6
> 6
Ascites
None
Mild
Marked
Child-Pugh grade
Hepatic deaths (%)
< 7 = Child's A
43
7-9 = Child's B
72
> 9 = Child's C
85
Page of
43
105
Internal Medicine: 4
th
Stage TUCOM Dr.Hassan
e) Hepatopulmonary syndrome
2. Hepatocellular carcinoma.
Portal hypertension:
• Prolonged elevation of the portal venous pressure above 12 mmHg (normally 2-5
mmHg).
• Increase in intrahepatic vascular tone -- increased resistance to portal venous flow --
an increase in portal venous pressure.
• Splenomegaly is a cardinal finding.
• Hypersplenism is common
• Caput medusae, oesophageal, gastric and rectal varices.
• Fetor hepaticus.
Variceal hemorrhage
• Occurs from oesophagogastric varices.
• Endoscopy is mandatory to determine the size ,site of varices, and source of bleeding.
To introduce some therapeutic options.
Management;
1. Restore the circulation with blood and plasma
2. Local measures:
• Banding or sclerotherapy.
• Balloon tamponade.
• Oesophageal transection.
3. Reduction of portal venous pressure:
• Drugs; Terlipressin is the drug of choice
• TIPSS (Transjugular intrahepatic portosystemic stent shunt) and shunt surgery
Prevention of recurrent bleeding:
1. Band ligation.
2. Sclerotherapy.
3. TIPSS (Transjugular intrahepatic portosystemic stent shunt).
4. Portosystemic shunt surgery.
5. Beta-adrenoceptor antagonists (β-blockers).
Ascites:
• Accumulation of excess fluid in the peritoneal cavity
• Clinically detectable when it is greater than 500 ml
• Cirrhosis is the most common cause of ascites
• A high serum-ascites albumin gradient (>1.1 g/dL) signifies portal hypertension
Page of
44
105
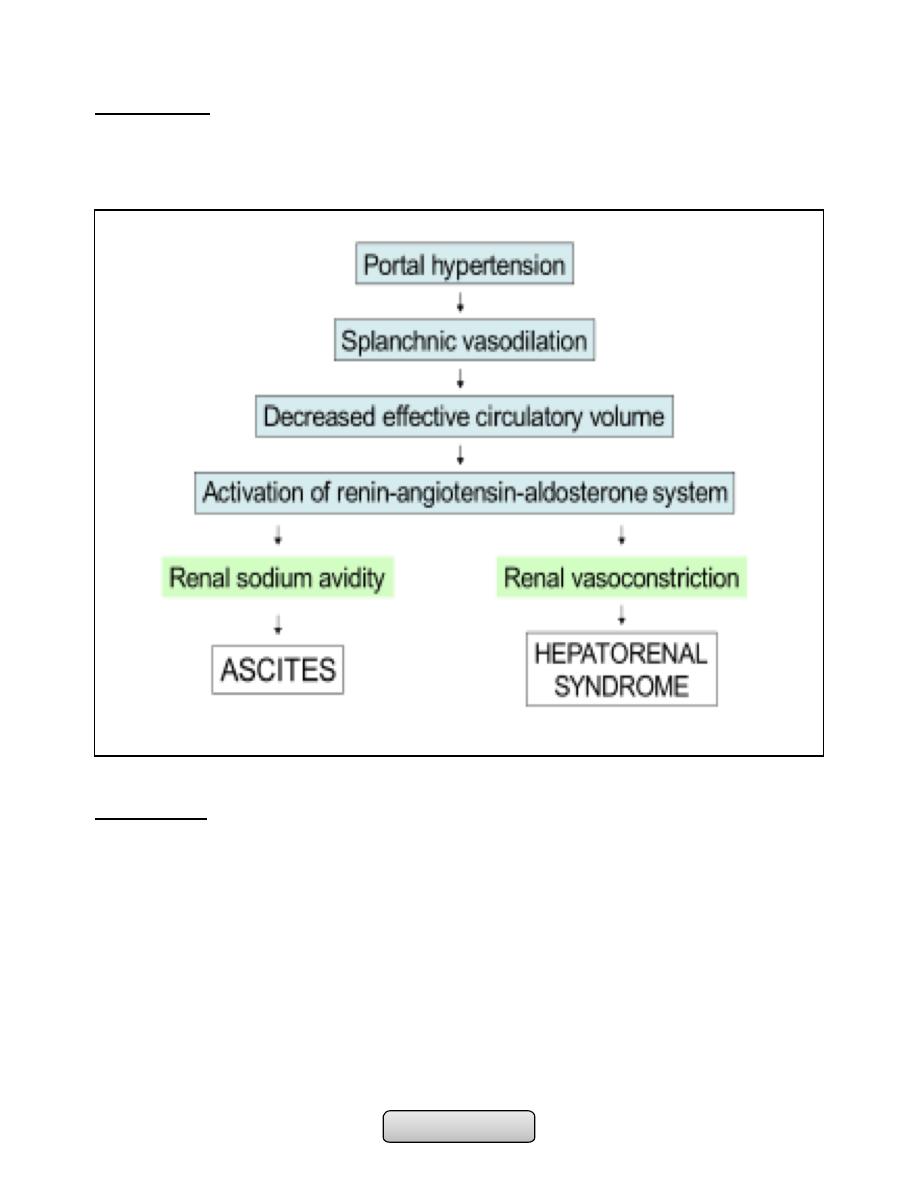
Internal Medicine: 4
th
Stage TUCOM Dr.Hassan
Pathogenesis;
• Splanchnic vasodilation (overflow theory).
• Renal sodium and water retention to normalize arterial pressure (underflow theory).
Management;
1. Sodium and water restriction; Restriction of sodium intake to 100 mmol/day (‘no
added salt diet’) is usually adequate. Drugs containing large amounts of sodium, and
those promoting sodium retention such as non-steroidal anti-inflammatory drugs
(NSAIDs), must be avoided.
2. Diuretic drugs; Spironolactone (100-400 mg/day) is the drug of choice. Some also
require powerful loop diuretics, e.g. furosemide. Patients who do not respond to
doses of 400 mg spironolactone and 160 mg furosemide are considered to have
refractory ascites.
3. Paracentesis; 3-5 litres daily is safe, provided the circulation is supported by giving
intravenous colloid such as human albumin (6-8 g per litre of ascites removed) or
another plasma expander.
Page of
45
105
Internal Medicine: 4
th
Stage TUCOM Dr.Hassan
4. Peritoneo-venous (LeVeen) shunt; Is a long tube with a non-return valve running
subcutaneously from the peritoneum to the internal jugular vein in the neck, which
allows ascitic fluid to pass directly into the systemic circulation.
5. Transjugular intrahepatic portosystemic stent shunt (TIPSS)
Spontaneous bacterial peritonitis:
• Infection of ascitic fluid. Escherichia coli is the organism most frequently found.
• Fever, abdominal pain, and tenderness may be present.
• Diagnosis is strongly suspected: ascitic neutrophil count above 250 × 10
6
/l.
• Confirmed by culture
• Rx --broad-spect. antibiotics, such as i.v cefotaxime or i.v ceftriaxone.
• Prophylactic quinolones such as norfloxacin (400 mg daily) or ciprofloxacin (250 mg)
daily.
Hepatic encephalopathy:
• A neuropsychiatric syndrome that may complicate advanced liver disease.
• Extensive portosystemic collateral formation (shunting).
• Inadequate hepatic removal of nitrogenous compound like ammonia, γ-aminobutyric
acid, and mercaptans. Which pass through portosystemic shunting to CNS, lead to
brain dysfunction and cerebral oedema .
• Examination; Disturbed consciousness, fetor hepaticus, flapping tremor (asterixis) ,
constructional apraxia hyper-reflexia and bilateral extensor plantar responses.
Clinical grading of hepatic encephalopathy
Treatment;
• Identification and treatment of precipitating factors
• Antibiotics that reduce colonic bacteria (i.e., neomycin and metronidazole).
• Nonabsorbable disaccharides (i.e., lactulose)
• Lactitol is more palatable.
• liver transplantation.
Clinical grading of hepatic encephalopathy
Clinical grade
Clinical signs
Grade 1
Poor concentration, slurred speech, disordered sleep rhythm
Grade 2
Drowsy, occasional aggressive behavior, lethargic
Grade 3
Marked confusion, gross disorientation
Grade 4
Unresponsive to voice, unconscious
Page of
46
105
Internal Medicine: 4
th
Stage TUCOM Dr.Hassan
Hepatorenal syndrome:
• Functional renal failure complicated advanced liver disease .
• Two types;
-
Type I rapidly progressive renal failure bad prognosis.
-
Type II more slowly better prognosis.
Treatment;
• Correction of plasma volume depletion
• Vasopressin
• TIPSS
• Liver transplantation
Hepatopulmonary syndrome:
• Characterised by hypoxemia, intrapulmonary vascular dilatation and chronic liver
disease with portal hypertension.
• Clinical features; Digital clubbing, cyanosis, spider naevi and a characterized by
reduction in arterial oxygen saturation on standing.
Treatment;
• No proven medical therapy exists
• Oxygen
• Liver transplantation
Hepatocellular carcinoma (HCC):
• HCC is the most common primary liver tumour, and the sixth most common cause of
cancer worldwide. Cirrhosis is present in 75– 90% of individuals with HCC and is an
important risk factor for the disease. Other causes like tobacco, aflatoxins and
autoimmune hepatitis.
• Macroscopically, the tumour usually appears as a single mass in the absence of
cirrhosis, or as a single nodule or multiple nodules in the presence of cirrhosis. It
takes its blood supply from the hepatic artery and tends to spread by invasion into the
portal vein and its radicals. Lymph node metastases are common.
Clinical features;
• Common presentation in cirrhotic patients are deterioration in their liver function,
with worsening ascites and/or jaundice or variceal haemorrhage. Associated with
weight loss, anorexia and abdominal pain.
• The second presentation is through screening of patients at risk of HCC (e.g. hepatitis
B and C, haemochromatosis, alcohol, NASH and α1-antitrypsin deficiency).
Page of
47
105
Internal Medicine: 4
th
Stage TUCOM Dr.Hassan
Investigations;
• Serum markers;
-
Alpha-fetoprotein (AFP) is produced by 60% of HCCs. AFP is used in conjunction
with ultrasound in screening.
• Imaging;
-
Ultrasound will detect focal liver lesions as small as 2–3 cm
-
Multidetector CT, following intravenous contrast, identifies HCC by its classical
hypervascular appearance.
-
MRI can be used to differentiate HCC from hyperplastic nodules in cirrhosis.
• Liver biopsy;
-
Biopsy should be avoided in patients who may be eligible for transplantation or
surgical resection because there is a small (< 2%) risk of tumour seeding along the
needle tract.
• Role of screening for HCC;
-
by ultrasound scanning and AFP measurements at 6-month intervals, is indicated in
highrisk patients, such as those with cirrhosis due to hepatitis B and C,
haemochromatosis, alcohol, NASH and α1-antitrypsin deficiency.
Management;
• Hepatic resection: This is the treatment of choice for non-cirrhotic patients.
• Liver transplantation.
• Percutaneous therapy; Percutaneous ethanol injection into the tumour under
ultrasound guidance or Radiofrequency ablation, using a single electrode inserted into
the tumour under radiological guidance
• Trans-arterial chemo-embolisation; hepatic artery embolisation with Gelfoam and
doxorubicin is more effective.
• Chemotherapy; Sorafenib
……………………………………………………………………………………………........................................
DISEASES OF THE PANCREAS
The pancreas:
• Gland with both exocrine and endocrine functions
• 15-25 cm long
• 60-100 g
• Location: retro-peritoneum, 2nd lumbar vertebral level
• Extends in an oblique, transverse position
• Parts of pancreas: head, neck, body and tail
Page of
48
105
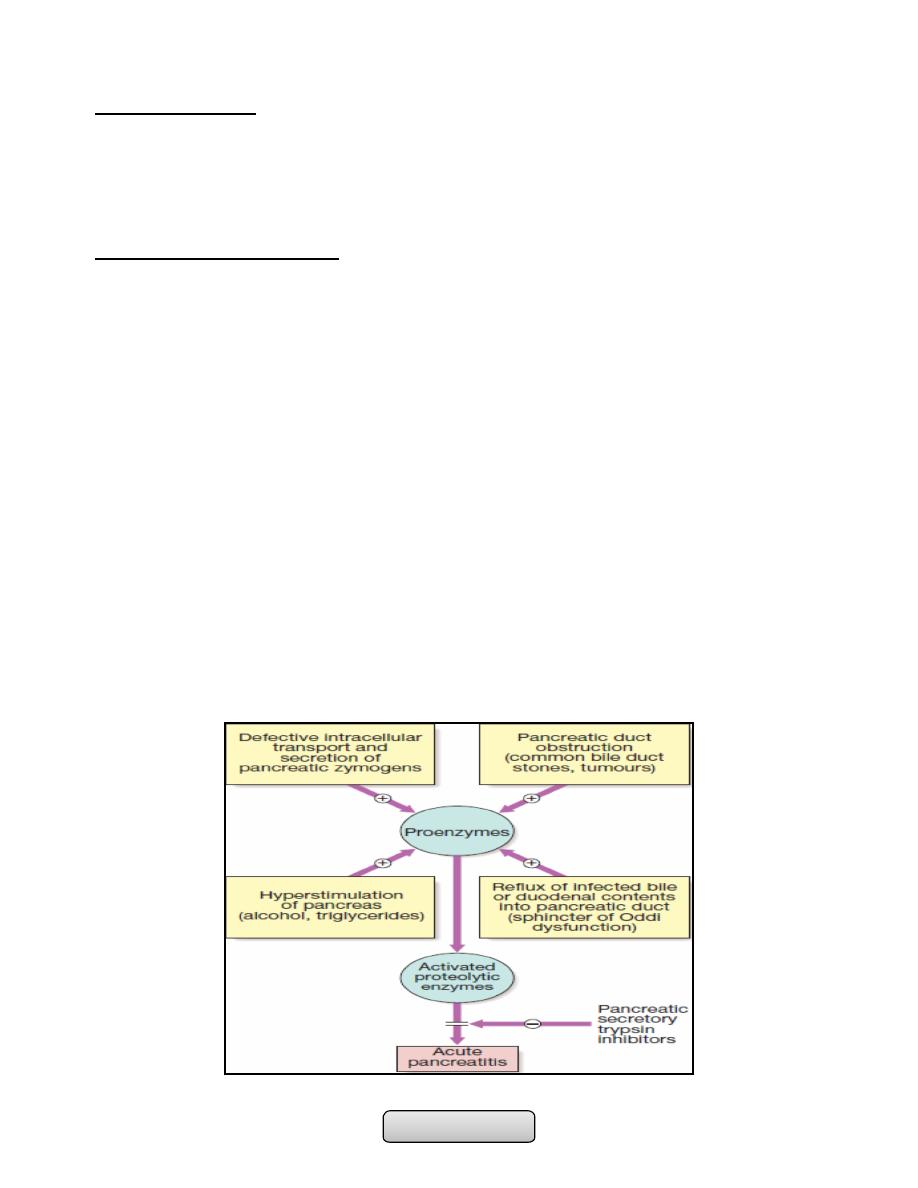
Internal Medicine: 4
th
Stage TUCOM Dr.Hassan
Acute pancreatitis:
• It is an acute inflammati0n of pancreas which may remain local or extend to
extrapancreatic tissues.
• 3% of all cases of abdominal pain admitted to hospital. 80% of cases are mild to
moderate and have good prognosis.
Causes of acute pancreatitis:
A. Common (90% of cases):
1. Gallstones.
2. Idiopathic.
3. Alcohol.
4. Post-ERCP.
B. Rare:
1. Post-surgical (abdominal, cardiopulmonary bypass).
2. Trauma.
3. Drugs (azathioprine/mercaptopurine, thiazide diuretics, sodium valproate).
4. Metabolic (hypercalcaemia, hypertriglyceridaemia).
5. Pancreas divisum (p. 894).
6. Sphincter of Oddi dysfunction.
7. Infection (mumps, Coxsackie virus).
8. Hereditary.
9. Renal failure.
10.Organ transplantation (kidney, liver).
11.Severe hypothermia.
12.Petrochemical exposure.
Page of
49
105
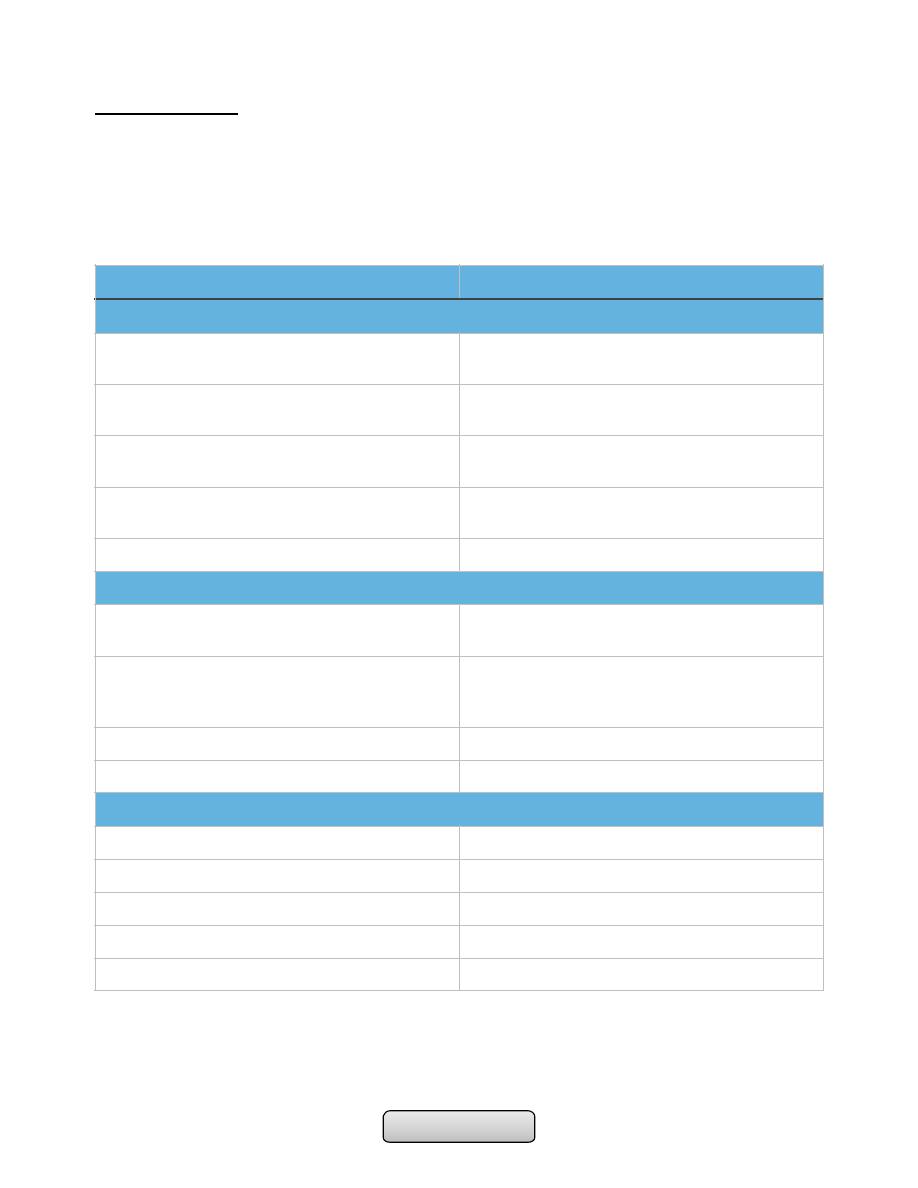
Internal Medicine: 4
th
Stage TUCOM Dr.Hassan
Clinical features:
• Acute, severe, constant upper abdominal pain, radiates to the back associated with
nausea and vomiting. There is epigastric tenderness, but no guarding.
• Discoloration of the flanks (Grey Turner’s sign) or the periumbilical region (Cullen’s
sign) is a feature of severe pancreatitis with haemorrhage.
• Various complications may occur.
complication
Cause
Systemic
Systemic inflammatory response syndrome
(SIRS)
Increased vascular permeability from cytokine,
platelet aggregating factor and kinin release
Hypoxia
Acute respiratory distress syndrome (ARDS)
due to microthrombi in pulmonary vessels
Hyperglycaemia
Disruption of islets of Langerhans with altered
insulin/glucagon release
Hypocalcaemia
Sequestration of calcium in fat necrosis, fall in
ionised calcium
Reduced serum albumin concentration
Increased capillary permeability
Pancreatic
Necrosis
Non-viable pancreatic tissue and peripancreatic
tissue death; frequently infected
Abscess
Circumscribed collection of pus close to the
pancreas and containing little or no pancreatic
necrotic tissue
Pseudocyst
Disruption of pancreatic ducts
Pancreatic ascites or pleural effusion
Disruption of pancreatic ducts
Gastrolntestinal
Upper gastrointestinal bleeding
Gastric or duodenal erosions
Variceal haemorrhage
Splenic or portal vein thrombosis
Erosion into colon
Duodenal obstruction
Compression by pancreatic mass
Obstructive jaundice
Compression of common bile duct
Page of
50
105
Internal Medicine: 4
th
Stage TUCOM Dr.Hassan
Investigations:
• Raised serum amylase or lipase concentrations. A persistently elevated serum amylase
concentration suggests pseudocyst formation. Peritoneal amylase concentrations are
massively elevated in pancreatic ascites.
• Ultrasound scanning can confirm the diagnosis (pancreatic swollen), also to show
gallstones, biliary obstruction or pseudocyst formation.
• CT for evidence of pancreatic swelling, pancreatic necrosis, abscess or pseudocyst.
Management:
• Opiate analgesics should be given to treat pain
• Hypovolaemia should be corrected using normal saline or other crystalloids.
• Admission to intensive care unit in sever cases.
• Oxygen should be given to hypoxic patients.
• Hyperglycaemia should be corrected using insulin.
• Hypocalcaemia need correction by intravenous calcium injection if tetany occurs.
• Nasogastric aspiration if paralytic ileus is present
• Prophylaxis of thromboembolism with subcutaneous low-molecular-weight heparin
• Prophylactic, broad-spectrum intravenous antibiotics, such as imipenem or
cefuroxime, to prevent infection
• Urgent ERCP to diagnose and treat choledocholithiasis.
• Treatment of complications like necrosectomy and drainage of pancreatic abscess or
pancreatic pseudocysts
Chronic pancreatitis:
• Is a chronic inflammatory disease characterized by fibrosis and destruction pancreatic
tissue resulting in permanent endocrine and exocrine pancreatic dysfunction.
• Around 80% of cases in Western countries result from alcohol misuse. Other causes are
listed in the table.
Glasgow criteria for prognosis in acute pancreatitis*
-
Age > 55 yrs.
-
PO2 < 8 kPa (60 mmHg).
-
White blood cell count (WBC) > 15 x 109/L.
-
Albumin < 32 g.lL (3.2 g’dL).
-
Serum calcium < 2 mmoUL (8 mg/dL) (corrected).
-
Glucose > 10 mmol/L (180 mg/dL).
-
Urea > 16 mmoL’L (45 mg’dL) (after rehydration).
-
Alanine aminotransferase (ALT) > 200 U/L.
-
Lactate dehydrogenase (LDH) > 600 U/L.
*Severity and prognosis worsen as the numter of these factors increases. More than three implies severe
disease.
Page of
51
105
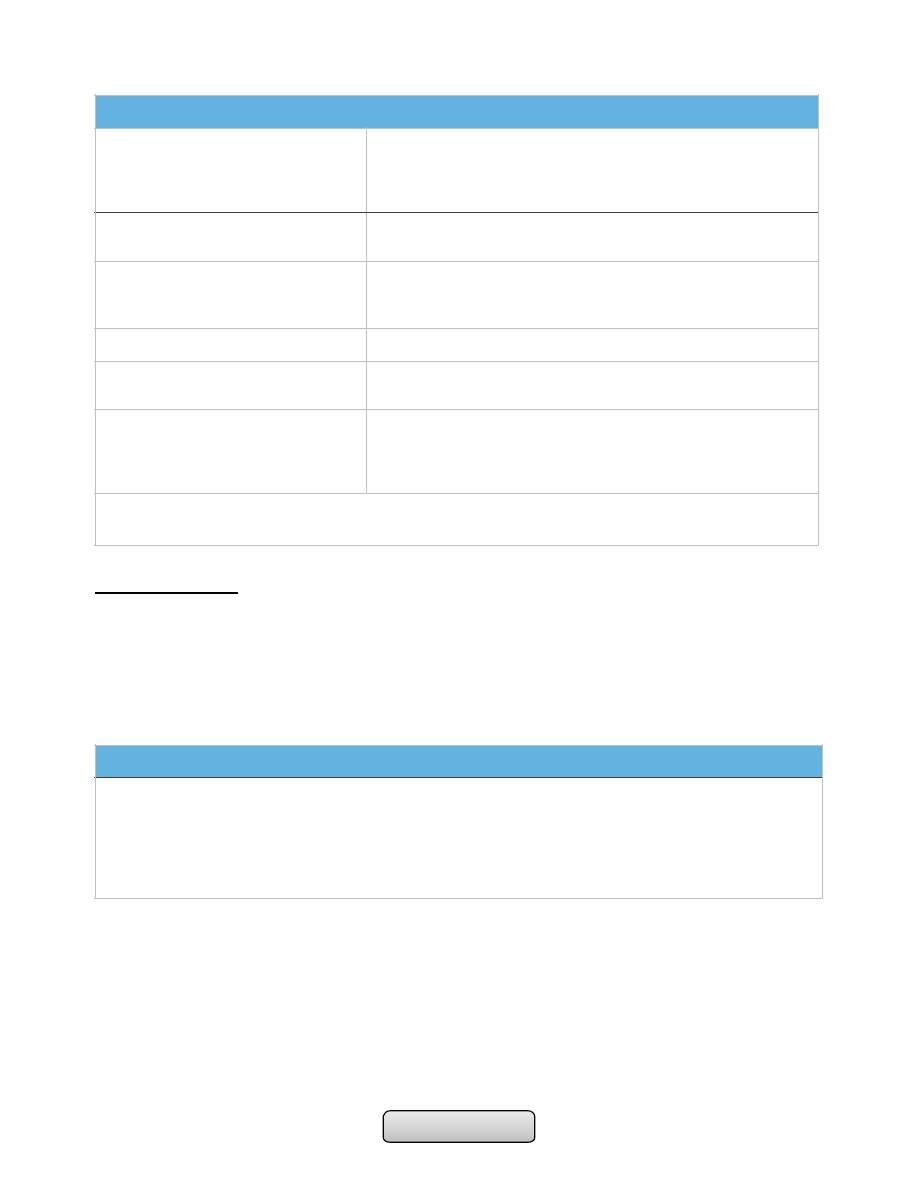
Internal Medicine: 4
th
Stage TUCOM Dr.Hassan
Clinical features:
• Chronic upper abdominal pain, radiated to the back, relieved by leaning forwards,
drinking alcohol or opiate analgesics.
• Weight loss, anorexia, steatorrhoea or diabetes.
• Malnourished patient, skin pigmentation over the abdomen and back is common and
results from chronic use of a hot water bottle (erythema ab igne).
Causes of chronic pancreatitis*
Toxic - metabolic
-
A|coho|
-
Hypercalcaemia
-
Tobacco
-
Chronic renal failure
Idiopathic
-
Tropical
-
Early/|ate - onset types
Genetic
-
Hereditary pancreatitis (cationic trypsinogen mutation)
-
SPINK-1 mutation
-
Cystic fibrosis
Autoimmune
Isolated or as part of multi-organ problem
Recurrent and severe acute
pancreatitis
-
Recurrent acute
-
Post-necrotic pancreatitis
Obstructive
-
Ductal adenocarcinoma
-
Pancreas divisum
-
lntraductal papillary mucinous neoplasia
-
Sphincter of Oddi stenosis
* These can be memorised by the mnemonic ‘T|GARO'. Gallstones do not cause chronic
pancreatrtis but may be observed as an incidental finding.
Complications of chronic pancreatitis
-
Pseudocysts and pancreatic ascites, which occur in both acute and chronic pancreatitis
-
Obstructive jaundice due to benign stricture of the common bile duct as it passes through the diseased
pancreas
-
Duodenal stenosis
-
Portal or splenic vein thrombosis leading to segmental portal hypertension and gastric varices
-
Peptic ulcer
Page of
52
105
Internal Medicine: 4
th
Stage TUCOM Dr.Hassan
Management:
Alcohol avoidance
Pain relief; NSAIDs, opiate but with the risk of addiction and oral pancreatic enzyme
supplements.
Coeliac plexus neurolysis sometimes produces long-lasting pain relief
Total pancreatectomy (diabetes, which may be
difficult to control, with a high risk of hypoglycaemia)
Malabsorption treated by dietary fat restriction, oral pancreatic enzyme supplements and
PPI.
Management of complications
Autoimmune pancreatitis (AIP) responds to corticosteroids.
Pancreatic carcinoma:
90% of pancreatic neoplasms are adenocarcinomas
which arise from the pancreatic ducts.
Men are affected twice as often as women.
The disease is associated with
1. increasing age
2. smoking
3. chronic pancreatitis
4. genetic predisposition (hereditary pancreatitis, MEN, hereditary non-polyposis
colon cancer (HNPCC) and familial atypical mole multiple melanoma syndrome
(FAMMM).
Investigations in chronic pancreatitis
Tests to establish the diagnosis
-
Ultrasound
-
CT (may show atrophy, calcification or ductal dilatation)
-
Abdominal X-ray (may show calcification)
-
MRCP
-
Endoscopic ultrasound
Tests of pancreatic function
-
Collection of pure pancreatic juice after secretin injection (gold standard but invasive and seldom used)
-
Pancreolauryl test (see Box 22.12, p. 851)
-
Faecal pancreatic elastase
Tests of anatomy prior to surgery
-
MRCP
Page of
53
105
Internal Medicine: 4
th
Stage TUCOM Dr.Hassan
Management:
• Alcohol avoidance
• Pain relief; NSAIDs, opiate but with the risk of addiction and oral pancreatic enzyme
supplements.
• Coeliac plexus neurolysis sometimes produces long-lasting pain relief
• Total pancreatectomy (diabetes, which may be
• difficult to control, with a high risk of hypoglycaemia)
• Malabsorption treated by dietary fat restriction, oral pancreatic enzyme supplements
and PPI.
• Management of complications
• Autoimmune pancreatitis (AIP) responds to corticosteroids.
Pancreatic carcinoma:
• 90% of pancreatic neoplasms are adenocarcinomas
• which arise from the pancreatic ducts.
• Men are affected twice as often as women.
• The disease is associated with:
-
Increasing age
-
Smoking
-
Chronic pancreatitis
-
Genetic predisposition (hereditary pancreatitis, MEN, hereditary non-polyposis
colon cancer (HNPCC) and familial atypical mole multiple melanoma syndrome
(FAMMM).
Clinical features:
• Asymptomatic
• Central abdominal pain, weight loss and obstructive jaundice
• Few patients present with diarrhoea, vomiting from duodenal obstruction, diabetes
mellitus, recurrent venous thrombosis, acute pancreatitis or depression.
Investigations:
• ultrasound
• contrast-enhanced CT
• EUS or laparoscopy
• MRCP and ERCP
Management:
• Surgical resection is the only method of cure, but the 5-year is 12%.
• In the majority of patients, the treatment is palliative.
• Chemotherapy
• Pain relief
Page of
54
105

Internal Medicine: 4
th
Stage TUCOM Dr.Hassan
• Jaundice can be relieved by choledochojejunostomy or stenting which preferable in
the elderly and those with very advanced disease
………………………………………………………………………………………............................................
Respiratory
…………………………………………………………………………………………..........................................
UPPER RESPIRATORY TRACT INFECTIONS
RESPIRATORY INFECTIONS CAUSED BY VIRUSES:
Influenza:
•
What do you know about Influenza viruses?
•
Influenza is an acute respiratory illness caused by infection with influenza viruses.
•
The illness affects the upper and/or lower respiratory tract and is often
accompanied by systemic signs and symptoms such as fever, headache, myalgia, and
weakness. Outbreaks of illness occur nearly every winter.
•
Such outbreaks result in significant morbidity and mortality in the general
population.
•
Influenza viruses are RNA viruses in the family Orthomyxoviridae that can affect
birds and mammals including humans. They have surface projections are molecules
of hemagglutinin and neuraminidase.
•
There are three types of influenza:
-
Influenza A; Responsible for regular outbreaks and pandemic. Influenza A viruses
also infect domestic animals (pigs, horses, chickens, ducks) and some wild birds.
-
Influenza B; Often causes sporadic outbreaks of illness, it is human pathogen only.
-
Influenza C; Seldom causes disease symptoms, human pathogen only.
Clinical syndrome
Usual cause
Epidemic influenza
Influenza A and B
Sore throat
Adenoviruses
Common cold (coryza)
Rhinoviruses
Croup
Parainfluenza 1, 2, 3
Bronchitis
Rhinoviruses, adenoviruses
Bronchiolitis
Respiratory syncytial virus
Pneumonia
Influenza A and B, chickenpox
Page of
55
105
Internal Medicine: 4
th
Stage TUCOM Dr.Hassan
Genes of Influenza A:
• Sheathed in a lipid bilayer (derived from the plasma membrane of its host cell).
Studded in the lipid bilayer are two integral membrane proteins: hemagglutinin ("H")
and neuraminidase ("N"). Within the lipid bilayer are matrix protein and 8
pieces of RNA.
• The HA gene. It encodes the hemagglutinin. 3 distinct hemagglutinins (H1, H2, and H3)
are found in human infections; 13 others have been found in animal flu viruses.
• The NA gene. It encodes the neuraminidase. 2 different neuraminidases (N1 and N2)
have been found in human viruses; 7 others in other animals.
Antigenic change in influenza viruses can occur:
• gradually (antigenic drift), which is the minor mutation of the surface glycoproteins,
namely hemagglutinin (H) and neuraminidase (N), that leads to seasonal epidemics that
occur in winter every year.
• or suddenly (antigenic shift ), which is a major change to the virus structure to create
an absolutely new subtype of influenza virus, that associated with pandemics and
enables a flu strain to jump from one animal species to another.
What events will lead to an influenza pandemic?
• Antigenic evolution of an influenza virus to which humans have little or no immunity, so
it easy spread among susceptible humans.
• The hemagglutinin of the 1918 flu virus was H1, its neuraminidase was N1, so it is
designated as an H1N1 "subtype".
• The data suggest that flu pandemics occur when the virus acquires a new hemagglutinin
and/or neuraminidase.
The Bird Flu;
• In October 2003, an epidemic of influenza in chickens began sweeping through several
countries (Vietnam, Thailand, Japan, China, South Korea, Cambodia).
• The virus is H5N1.
• The H5 molecule is common among bird influenza viruses but has not been seen on flu
viruses that cause human epidemics. However, sporadic human cases of H5N1 (with an
alarmingly-high fatality rate) have been occurring ever since.
The Swine Flu of 2009;
• A new H1N1 flu began infecting humans in North America in April 2009 and has now
spread throughout much of the world.
• The amino acid sequence of its H1 molecules closely resemble those found in the 1918
flu virus, so that enabled the virus to jump so successfully from pigs to humans.
Page of
56
105
Internal Medicine: 4
th
Stage TUCOM Dr.Hassan
Clinical features:
• Epidemics of influenza A occur almost exclusively during the winter months.
• An abrupt illness affects the upper (cough, sore throat, substernal discomfort) and/or
lower respiratory tract (dyspnea, wheezes, rhonchi, scattered rales or signs of
consolidation) accompanied by systemic signs and symptoms such as headache, fever
(temperatures of 38°–41°C), chills, diaphoresis, myalgia, arthralgias, weakness, and
malaise.
• Most patients have largely recovered in 1 week.
When might microbiological investigations be appropriate?
• Diagnosis usually made on clinical ground, but microbiological investigations may be
appropriate for immunocompromized patient, unusual clinical presentation or serious
systemic illness.
• This done by; antigenic detection with immunofluorescence and PCR, these methods
are preferable to culture and serology.
What are the complications of influenza?
• Tracheitis, bronchitis, bronchiolitis and bronchopneumonia. Secondary bacterial
invasion by Strep. pneumoniae, H. influenzae and Staph. aureus may occur.
• Toxic cardiomyopathy may cause sudden death (rare).
• Encephalitis, demyelinating encephalopathy and peripheral neuropathy are also rare
complications.
What preventative measures are available for influenza?
• Flu Vaccines; inactivated component of influenza virus, which reviewed each year by
WHO to ensure a closed match to influenza strains. The protection is 70- 80% when viral
strain is matched.
• Annual Immunization is recommended for;
-
Patient over 65 year
-
Chronic respiratory diseases
-
Chronic heart diseases
-
Chronic renal diseases
-
Chronic liver diseases
-
Immunosuppression
What antiviral treatment of influenza?
Amantadine and Rimantadine;
• These drugs inhibit the matrix protein needed to get viral RNA into the cytosol. They
work against A strains only, and resistance to the drugs evolves quickly.
Page of
57
105
Internal Medicine: 4
th
Stage TUCOM Dr.Hassan
Zanamivir (Relenza®) and Oseltamivir (Tamiflu®);
• These drugs block the neuraminidase and thus inhibit the release and spread of fresh
virions. Spraying zanamivir into the nose or inhaling it shortens the duration of disease
symptoms by one to three days. Unfortunately, by the 2008-2009 flu season, all H1N1
strains circulating in the U.S. had become resistant to Tamiflu.
…………………………………………………………………………………………..
PNEUMONIA
PNEUMONIA:
• Acute inflammation of lung parenchyma.
• Inflammatory infiltrate in alveoli (consolidation).
CLASSIFICATION:
1. Aetiology.
2. Morphological classification: Bronchopneumonia vs. lobar pneumonia(which may be
segmental, lobar or multilobar).
-
Lobar pneumonia; is a radiological and pathological term referring to homogeneous
consolidation of one or more lung lobes, often with associated pleural inflammation.
-
Bronchopneumonia; refers to more patchy alveolar consolidation associated with
bronchial and bronchiolar inflammation often affecting both lower lobes.
3. Community acquired vs hospital acquired (nosocomial) infection.
4. The patient's immune status.
Pathology of lobar pneumonia:
4 pathological phases;
1. Congestion; 1-2 days. Pulmonary capillaries dilated and serous fluid leaks out
capillaries into the alveoli. The patient is feverish with SOB and cough.
2. Red hepatization; 2-4 days. That is means the lung look like ‘red liver‘. The affected
lobe is solid as the alveoli are full RBCs, neutrophils and fibrinous exudate instead of
air, there is no gas exchange in this lobe. The patient becomes breathless and
hypoxic. The cough is blood stained or rusty sputum.
3. Grey hepatization; 4-8 days. The affected part look like ‘grey liver‘. The alveoli are
full of neutrophils and dense fibrous strands. The patient cough up of purulent sputum
and remain breathless.
4. Resolution; Begins after 8-10 days (without antibiotics). Monocytes clear the
inflammatory debris and normal air filled lung architecture is restored. Improvement
of patient's condition.
Page of
58
105
Internal Medicine: 4
th
Stage TUCOM Dr.Hassan
COMMUNITY-ACQUIRED PNEUMONIA (CAP):
• The incidence varies with age, being much higher in the very young and the elderly
• Most patients may be safely managed at home, but hospital admission is necessary in
20-40% of patients (5-10% of whom require intensive care)
• CAP is usually spread by droplet infection and most cases occur in previously healthy
individuals.
Factors that predispose to pneumonia:
1. Cigarette smoking
2. Upper respiratory tract infections
3. Alcohol
4. Corticosteroid therapy
5. Old age
6. Recent influenza infection
7. Pre-existing lung disease
8. HIV
9. Indoor air pollution.
Organisms causing community-acquired pneumonia:
Bacteria:
• Streptococcus pneumoniae
• Mycoplasma pneumoniae
• Legionella pneumophila
• Chlamydia pneumoniae
• Haemophilus influenzae
• Staphylococcus aureus
• Chlamydia psittaci
• Coxiella burnetii (Q fever, ‘querry’ fever)
• Klebsiella pneumoniae (Freidländer’s bacillus)
• Actinomyces israelii
Viruses:
• Influenza, parainfluenza
• Measles
• Herpes simplex
• Varicella
• Adenovirus
• Cytomegalovirus (CMV)
• Coronavirus (Urbani SARS-associated coronavirus
Page of
59
105
Internal Medicine: 4
th
Stage TUCOM Dr.Hassan
Microorganisms & clinical features of CAP:
Common organisms:
1. Streptococcus pneumoniae;
• The most common cause of classic or typical pneumonia.
• Most common in winter. All age groups but particularly young to middle-aged.
• Rapid onset of Systemic features such as fever, rigors, shivering tachycardia and
malaise predominate and delirium may be present.
• Pulmonary symptoms include tachypnea, cough, which at first is painful and dry, but
later accompanied by the mucopurulent or rust-coloured sputum, or occasionally
hemoptysis.
• Pleuritic chest pain may be a presenting feature.
• Herpes labialis and rusty sputum.
2. Mycoplasma pneumoniae;
• Children and young adults. Common in autumn. Epidemics occur every 3-4 years. After
(2–3 weeks) incubation period, fever and constitutional symptoms develop along with
headache and cough, but pleuritic pain is uncommon. Rare complications include
haemolytic anaemia, Stevens-Johnson syndrome, erythema nodosum, myocarditis,
pericarditis, meningoencephalitis, Guillain-Barré syndrome.
• Grown on artificial media takes upwards of 2 weeks.
3. Chlamydia pneumoniae;
• Young to middle-aged, large-scale epidemics, or sporadic, often mild, self-limiting
disease. Headaches and a longer duration of symptoms before hospital admission.
• The pneumonia resembles that of Mycoplasma pneumonia in that patients often have
prominent antecedent upper respiratory tract symptoms, fever, nonproductive cough,
mild to moderate illness, minimal findings on chest auscultation, and small segmental
infiltrates on chest x-ray.
• Usually diagnosed on serology.
4. Legionella pneumophila;
• Middle to old age, recent foreign travel, local epidemics around point source, e.g.
cooling tower.
• A variety of features are said to be more common such as nonproductive cough,
headache, confusion, malaise, myalgia, high fever and diarrhoea.
Laboratory results include hyponatraemia, elevated liver enzymes, hypoalbuminaemia
and elevated creatine kinase. Chest X-ray appearances may be slow to resolve.
Uncommon organisms;
1. Haemophilus influenzae;
• H. influenzae, an exclusively human pathogen, is spread by airborne droplets, its
gram-negative coccobacillus.
• Clinically indistinguishable from other types of bacterial pneumonia (e.g.
pneumococcal pneumonia).
• Often underlying lung disease (COPD, bronchiectasis).
Page of
60
105
Internal Medicine: 4
th
Stage TUCOM Dr.Hassan
2. Staphylococcus aureus;
• Coexistent debilitating illness and often preceded by influenza. Radiographic features
include multilobar shadowing, cavitation, pneumatoceles and abscesses.
• Dissemination to other organs may cause osteomyelitis, endocarditis or brain
abscesses. Mortality up to 30%.
3. Klebsiella pneumonia;
• More common in aged men, malnutrition and alcoholics. Upper lobe involvement
typical. Low platelet count and leucopenia.
Atypical pneumonia;
• It is an old term used to describe pneumonias where symptoms were more systemic
(headache, malaise, diarrhea) than pulmonary (cough, sputum, SOB). Atypical
pneumonia was most often caused by pathogens such as Mycoplasma, Chlamydia,
Legionella. as well as viral pneumonia.
• Currently, it is recognized that symptoms do not reliably predict the infecting
organism and that bacteria in atypical group commonly cause pneumonia.
Investigations:
The main objectives of investigations:
1. to obtain radiological confirmation of the diagnosis
2. to exclude other conditions that may mimic pneumonia
3. to obtain a microbiological diagnosis
4. to assess the severity of pneumonia
5. to identify the development of complications.
Radiological examination:
• In lobar pneumonia, a homogeneous opacity localized to the affected lobe or segment
usually appears within 12-18 hours from the onset of the illness.
• If a complication such as parapneumonic effusion, intrapulmonary abscess formation,
or empyema is suspected.
• Clinical-radiographic dissociation is seen often in patients with Mycoplasma
pneumoniae or viral pneumonia.
• Lateral radiographs are especially important in showing infiltrates, which may be
obscured by the heart on posteroanterior projections.
Microbiological investigations (CAP):
Many cases of CAP can be managed successfully without identification of the organism:
A. All patients:
• Sputum-direct smear by Gram and Ziehl-Neelsen stains.
• Culture and antimicrobial sensitivity testing. Blood culture-frequently positive in
pneumococcal pneumonia.
Page of
61
105
Internal Medicine: 4
th
Stage TUCOM Dr.Hassan
• Serology-acute and convalescent titers to diagnose Mycoplasma, Chlamydia,
Legionella and viral infections. Pneumococcal antigen detection in serum.
B. Severe community-acquired pneumonia; The above tests plus consider:
• Tracheal aspirate, induced sputum, bronchoalveolar lavage, protected brush specimen
or percutaneous needle aspiration. Direct fluorescent antibody stain for Legionella
and viruses.
• Serology- Legionella antigen in urine. Pneumococcal antigen in sputum and blood.
Immediate IgM for Mycoplasma.
• Cold agglutinins-positive in 50% of patients with Mycoplasma.
Assessment of disease severity:
DIFFERENTIAL DIAGNOSIS OF PNEUMONIA:
1. Pulmonary infarction
2. Pulmonary/pleural TB
3. Pulmonary oedema (can be unilateral)
4. Pulmonary eosinophilia
5. Malignancy: bronchoalveolar cell carcinoma
6. Rare disorders: cryptogenic organising pneumonia/bronchiolitis obliterans
organising pneumonia (COP/BOOP).
Assessment of gas exchange;
• Pulse oximetry provides a simple non-invasive method
• An arterial blood gas should be sampled in those with SaO
2
< 92% or with features of
severe pneumonia
General blood tests;
• white cell count my be very high (> 20 × 10
9
/l) or low (< 4 × 10
9
/l) seen in severe
pneumonia. urea and electrolytes and liver function tests. C-reactive protein (CRP) is
typically elevated.
Management:
• Rest and avoid smoking.
Oxygen;
should be administered to all patients with tachypnoea, hypoxaemia, hypotension or
acidosis. The aim of maintaining the PaO
2
≥ 8 kPa (60 mmHg) or SaO
2
≥ 92%. High
concentrations (> 35%), preferably humidified.
Page of
62
105
Internal Medicine: 4
th
Stage TUCOM Dr.Hassan
Fluid balance;
Intravenous fluids should be considered in those with severe illness, elderly patients and
those whose systemic features include vomiting.
Antibiotic treatment;
• The choice of antibiotic is guided by clinical context, severity assessment, local
knowledge of antibiotic resistance patterns, and at times epidemiological
information.
• Uncomplicated CAP; 7-10-day course is adequate:
-
Amoxicillin 500 mg 8-hourly orally
-
If patient is allergic to penicillin
-
Clarithromycin 500 mg 12-hourly orally or
-
Erythromycin 500 mg 6-hourly orally
-
If Staphylococcus is cultured or suspected
-
Flucloxacillin 1-2 g 6-hourly i.v. plus
-
Clarithromycin 500 mg 12-hourly i.v.
-
If Mycoplasma or Legionella is suspected
-
Clarithromycin 500 mg 12-hourly orally or i.v. or
-
Erythromycin 500 mg 6-hourly orally or i.v. plus
-
Rifampicin 600 mg 12-hourly i.v. in severe cases
•
Severe CAP: for 10–14 days:
-
Clarithromycin 500 mg 12-hourly i.v. or
-
Erythromycin 500 mg 6-hourly i.v. plus
-
Co-amoxiclav 1.2 g 8-hourly i.v. or
-
Ceftriaxone 1-2 g daily i.v. or
-
Cefuroxime 1.5 g 8-hourly i.v. or
-
Amoxicillin 1 g 6-hourly i.v. plus flucloxacillin 2 g 6-hourly i.v.
Treatment of pleural pain;
• Relieve pleural pain in order to allow the patient to breathe normally and cough
efficiently. Mild analgesics such as paracetamol are rarely adequate; however, opiates
must be used with extreme caution in patients with poor respiratory function.
Complications:
• Para-pneumonic effusion-common
• Empyema
• Retention of sputum causing lobar collapse
• Development of thromboembolic disease
• Pneumothorax-particularly with Staph. aureus
• Suppurative pneumonia/lung abscess-see below
• ARDS, renal failure, multi-organ failure
• Ectopic abscess formation (Staph. aureus).
Page of
63
105
Internal Medicine: 4
th
Stage TUCOM Dr.Hassan
• Hepatitis, pericarditis, myocarditis, meningoencephalitis.
• Pyrexia due to drug hypersensitivity
Discharge and follow-up:
• clinically stable,
• with no more than one of the following clinical signs: temperature > 37.8°C, heart
rate > 100/min, respiratory rate > 24/min, systolic BP < 90 mmHg, SaO
2
< 90%,
inability to maintain oral intake and abnormal mental status.
HOSPITAL-ACQUIRED PNEUMONIA:
• HAP or nosocomial pneumonia refers to a new episode of pneumonia occurring at
least 2 days after admission to hospital, includes;
-
Post-operative and certain forms of aspiration pneumonia.
-
Bronchopneumonia developing in patients with chronic lung disease, general
debility or those receiving assisted ventilation.
Aetiology;
• The elderly are particularly at risk and this condition now occurs in 2-5% of all
hospital admissions.
• Different pathogenic organisms;
1. The majority Gram-negative bacteria, includes Escherichia, Pseudomonas and
Klebsiella species.
2. Staph. aureus (including multidrug-resistant-MRSA-forms) are also common.
3. Anaerobic organisms.
Clinical features;
• The clinical features and investigation of patients with hospital-acquired pneumonia
are very similar to CAP. But there may be some differences;
-
Bronchopneumonia
-
Breathlessness and central cyanosis
-
Pleural pain is uncommon
-
Chest X-ray shows mottled opacities in both lung fields, chiefly in the lower zones.
Management of HAP:
• A third-generation cephalosporin (e.g. cefotaxime) plus an aminoglycoside (e.g.
gentamicin) to cover Gram-negative bacteria, including Pseudomonas.
• A monocyclic β-lactam (e.g. aztreonam) plus flucloxacillin to cover Staph. aureus.
• Metronidazole to cover anaerobic organisms.
• Physiotherapy ,adequate oxygen therapy, fluid support and monitoring are essential.
• The mortality from hospital-acquired pneumonia is high (approximately 30%).
Page of
64
105
Internal Medicine: 4
th
Stage TUCOM Dr.Hassan
Severe acute respiratory distress syndrome (SARS):
• Corona virus, is an RNA virus
• SARS rose to prominence in late 2002 in China. followed by an international outbreak
• high fever (> 38°C), malaise and muscle aches and later a dry cough with shortness of
breath or difficulty in breathing, with history close contact within 10 days of onset of
symptoms with a person known to be a suspect SARS case is typical.
• The chest X-ray is usually indicative of pneumonia.
• A rapid diagnosis of SARS-CoV infection can be made by PCR & Serum antibodies, can
be detected by ELISA.
• There is no specific therapy of established efficacy for SARS. Its treatment remains
largely supportive, to maintain pulmonary and other organ system functions.
………………………………………………………………………………………………
INTERSTITIAL LUNG DISEASE
Interstitial Lung Disease (ILD):
• ILD is a heterogeneous group of pulmonary diseases characterized by diffuse lung
injury and inflammation that frequently progresses to irreversible fibrosis and
severely compromised gas exchange.
• classified together because of similar clinical, radiographic, physiologic, or pathologic
manifestations.
Features common to ILD:
Clinical presentation:
• Cough: usually dry, persistent and distressing
• Breathlessness: usually slowly progressive, insidious onset.
Examination findings:
• Crackles: typically bilateral and basal
• Clubbing: common in idiopathic pulmonary fibrosis
• Central cyanosis and signs of right heart failure in advanced disease
Radiology:
• Chest X-ray: typically small lung volumes with reticulonodular shadowing
• HRCT: reticulonodular shadowing in early stage and honeycomb cysts and traction
bronchiectasis in advance stage.
Pulmonary function:
• Typically restrictive ventilatory defect with reduced lung volumes and impaired gas
transfer.
Page of
65
105
Internal Medicine: 4
th
Stage TUCOM Dr.Hassan
Results of PFT in restrictive lung disease:
• Both forced expiratory volume in one second (FEV1) and forced vital capacity (FVC)
are reduced, however, the decline in FVC is more than that of FEV1, resulting in
FEV1/FVC ratio higher than 80%.
• Both total lung capacity and lung volumes are reduced.
• Reduce diffusing capacity of the lung: decrease the transfer of gas from air to the
lung by using carbon monoxide (CO), (DLCO).
The Lung Interstitium:
• The interstitial space is defined as continuum of loose connective tissue throughout
the lung. It concerns with alveolar epithelium, pulmonary capillary endothelium,
basement membrane, perivascular and perilymphatic tissues, subpleural and
interlobular septae.
• The interstitium of the lung is not normally visible radiographically; it becomes visible
only when disease (e.g. edema, fibrosis, tumor) increases its volume and attenuation.
Classification:
I. ILD of unknown causes; Sarcoidosis and idiopathic pulmonary Fibrosis (fibrosing
alveolitis).
II. ILD due to organic dusts exposure;
A. Hypersensitivity pneumonitis (extrinsic allergic alveolitis); Farmer's lung, Bird
fancier's lung, Malt worker's lung, Cheese worker's lung, Maple bark stripper's lung.
B. Byssinosis; is acute bronchiolitis due to cotton dust inhalation.
C. Inhalation ('humidifier') fever.
III. ILD due to inhalation of inorganic dusts;
A. Coal worker's pneumoconiosis; inhalation of coal dust.
B. Silicosis; inhalation of silica dust.
C. Asbestosis; due to inhalation of asbestos fibers.
D. Berylliosis; due to inhalation Beryllium.
IV. ILD due to systemic inflammatory diseases; due to connective tissue disorders;
Rheumatoid disease, systemic lupus erythematosus, systemic sclerosis.
V. ILD due to irradiation.
Idiopathic pulmonary fibrosis:
• IPF is defined as a progressive fibrosing interstitial pneumonia of unknown cause,
occurring in adults and associated with the histological or radiological pattern of usual
interstitial pneumonia (UIP). Previously known as cryptogenic fibrosing alveolitis
• There is some role of viral exposure e.g. EBV, occupational dust e.g. metal or wood,
drugs e.g. antidepressant or GERD. There is a strong association with cigarette
smoking.
Page of
66
105
Internal Medicine: 4
th
Stage TUCOM Dr.Hassan
Clinical features;
• usually patients more than 50 yrs, progressive breathlessness and a non-productive
cough.
• Arthralgia may be reported. Finger clubbing and late inspiratory crackles at lung
bases. advanced cases central cyanosis and cor pulmnale.
Investigations:
• Rheumatoid factor and antinuclear factor can be detected in 30-50% of patients. (ESR)
is elevated in most cases.
• Pulmonary function tests show a restrictive defect with reduced lung volumes and gas
transfer.
• Abnormal chest X-ray at presentation with lower zone bi-basal reticular and
reticulonodular opacities. 'honeycomb' appearance in advanced disease.
• HRCT may be diagnostic, demonstrating a patchy, predominantly peripheral,
subpleural and basal reticular pattern with subpleural cysts (honeycombing).
• BAL (bronchoalveolar lavage) and transbronchial biopsy may be used to exclude
alternative diagnoses. Not require in typical clinical features and HRCT.
Management:
• Treatment is difficult. Although the combination of prednisolone, azathioprine and N-
acetylcysteine in large studies suggest that it is mostly ineffective.
• Treat gastro-oesophageal reflux, pulmonary hypertension and supplementation of
oxygen.
• Lung transplantation should be considered in young patients with advanced disease.
• A median survival of 3 years.
Sarcoidosis:
• Sarcoidosis is a multisystemic granulomatous disorder of unknown aetiology. seen in
colder parts of Northern Europe. Characterized by non-caseating granuloma. Over 90%
of cases affect the lungs.
Berylliosis:
• Similar clinical and radiological features to sarcoidosis, charactrized by lung
granulomas and interstitial fibrosis.
• occur in persons working in aircraft, atomic energy and electronics industries.
Coal worker's pneumoconiosis:
Pulmonary fibrosis caused by prolonged inhalation of coal dust. Which divided into;
1. Simple coal worker's pneumoconiosis (SCWP); scattered discrete fibrotic lesions,
does not cause pulmonary function abnormalities or progress following cessation of
exposure.
2. Complicated pneumoconiosis; large dense masses appear mainly in the upper lobes
(also known as progressive massive fibrosis, PMF). Presented as cough, production
Page of
67
105
Internal Medicine: 4
th
Stage TUCOM Dr.Hassan
of sputum, that may be black (melanoptysis) and breathlessness. Respiratory
failure after cessation of exposure and right ventricular failure.
3. Caplan's syndrome describes the coexistence of rheumatoid arthritis and rounded
fibrotic nodules 0.5-5 cm in diameter.
Silicosis:
• Silicosis results from the inhalation of crystalline or free silica.
• Silica is highly fibrogenic and the disease is usually progressive (even when exposure
ceases).
• The clinical and radiological features are similar to those of coal worker's
pneumoconiosis, with multiple well circumscribed 3–5-mm nodular opacities,
predominantly in the mid- and upper zones
• Enlargment of the hilar glands with an 'egg-shell' pattern of calcification is
characterestic.
• Silicosis are at increased risk of tuberculosis (silicotuberculosis), lung cancer and
COPD.
Asbestosis:
• Is a diffuse interstitial fibrosis of the lungs that may or may not be associated with
pleural fibrosis due to exposure to fibrous mineral asbestos.
• Requires substantial exposure over several years
• Risk factor for carcinoma of the lung and larynx
• Exertional breathlessness and fine, late inspiratory crackles over the lower zones and
digital clubbing.
• Chest X-ray; Shows bi-basal reticular nodular shadowing and asbestos-related pleural
disease is usually present. HRCT scanning is more sensitive.
• Pulmonary function tests; Typically show a restrictive defect with decreased lung
volumes and reduced gas transfer factor.
• Asbestos bodies may be identified in sputum or BAL and confirm asbestos exposure.
Management:
• No specific treatment is available
• Prevention of occupational lung disease:
1. Limit exposure to safe level with specific respiratory protection
2. Medical screening for early evidence of disease
3. Stop smoking
4. Change the job of patient because respiratory symptoms related to occupation
5. Patient develop work related disability must be established in worker’s
compensation systems.
…………………………………………………………………………………………….
Page of
68
105
Internal Medicine: 4
th
Stage TUCOM Dr.Hassan
PNEUMOTHORAX
Pneumothorax:
• Define as; Air accumulates in the pleural space.
Classification:
A. Spontaneous:
1. Primary; Without evidence of overt lung disease. Air escapes from the lung into
the pleural space through rupture of a small subpleural emphysematous bulla
or pleural bleb, or the pulmonary end of a pleural adhesion.
2. Secondary; Underlying lung disease, most commonly COPD and TB; also seen in
asthma, lung abscess, pulmonary infarcts, bronchogenic carcinoma, all forms of
fibrotic and cystic lung disease.
B. Traumatic;
1. Iatrogenic (e.g. following thoracic surgery or biopsy).
2. Non-iatrogenic.
Clinical features;
Commonest symptoms are sudden-onset unilateral pleuritic chest pain or breathlessness:
• Small pneumothorax (<2 cm visible rim of air on chest x ray between lung margin and
chest wall and occupying <50% of the volume of hemithorax).
-
The physical examination may be normal.
• A larger pneumothorax (>2 cm visible rim of air on chest x ray between lung margin
and chest wall and occupying >50% of the volume of hemithorax) results in;
-
Decreased or absent breath sounds.
-
Resonant percussion.
Types of spontaneous pneumothorax:
1. Tension pneumothorax; It can act as a one-way valve allowing air to enter the pleural
space during inspiration but not to escape on expiration. Intrapleural pressure may
rise to well above atmospheric levels causes mediastinal displacement towards the
opposite side and cardiovascular system compromise. Clinically, rapidly progressive
breathlessness, marked tachycardia, hypotension, cyanosis and tracheal displacement
away from the side of the lesion.
2. Closed pneumothorax; Communication between the lung and pleural space seals off as
the lung deflates and does not reopen the mean pleural pressure remains negative
spontaneous reabsorption of air and re-expansion of the lung occur over a few days or
weeks, and infection is uncommon.
3. Open pneumothorax; Communication fails to seal and air continues to transfer freely
between the lung and pleural space-- a bronchopleural fistula-- transmission of
Page of
69
105
Internal Medicine: 4
th
Stage TUCOM Dr.Hassan
infection –empyema. rupture of an emphysematous bulla, tuberculous cavity or lung
abscess into the pleural space.
Investigations:
Chest X-ray;
• Shows the sharply defined edge of the deflated lung with complete translucency (no
lung markings) between this and the chest wall. Chest X-rays also show the extent of
any mediastinal displacement and give information regarding the presence or absence
of pleural fluid and underlying pulmonary disease.
CT of chest;
• Is useful in distinguishing bullae from pleural air.
Management:
• Primary pneumothorax where the lung edge is less than 2 cm from the chest wall and
the patient is not breathless normally resolves without intervention.
• Percutaneous needle aspiration (PNA) of air: is a simple and well-tolerated
alternative to intercostal tube drainage, with a 60-80% chance of avoiding the need
for a chest drain in young patients presenting with a moderate or large spontaneous
primary pneumothorax.
• Intercostal tube drainage; indicate in above patient who does not improved by PNA
and in patients with underlying chronic lung disease, however, even a small secondary
pneumothorax may cause respiratory failure.
• Need inpatient observation:
• Inserted in the 4th, 5th or 6th intercostal space in the mid-axillary line
• Supplemental oxygen as this accelerates the rate at which air is reabsorbed by the
pleura.
• Surgical pleurodesis;
• Second pneumothorax (even if ipsilateral).
• First episode of secondary pneumothorax if low respiratory reserve makes recurrence
hazardous.
• Occupational risk (e.g. flying or diving) should also undergo definitive treatment after
the first episode of a primary spontaneous pneumothorax.
• Persistent air leak and the lung fails to re-expand after appropriate pleural drainage.
……………………………………………………………………………………………
Page of
70
105
Internal Medicine: 4
th
Stage TUCOM Dr.Hassan
LUNG CANCER
Lung cancer:
The term lung cancer is used for tumors arising from the respiratory epithelium (bronchi,
bronchioles and alveoli).
Aetiology;
1. Cigarette smoking:
• active cigarette smoking is the most important risk factor. Responsible for 90% of
lung carcinomas, which related to amount of smoked and to the tar content of
cigarettes. A person who has a 40 pack year smoking history over 20 years has 60- 70
time greater risk of lung cancer than non-smoker.
• The death rate from the disease in heavy smokers is 40 times that in non-smokers.
'Passive' smoking is more difficult to quantify 5% of all lung cancer deaths.
• Pack year: is a term used to describe the number of cigarettes a person has smoked
over time. One pack year is defined as 20 manufactured cigarettes (one pack)
smoked per day for one year. Number of pack years = (number of cigarettes smoked
per day x number of years smoked)/20 (1 pack has 20 cigarettes).
• For example: a patient who has smoked 15 cigarettes a day for 40 years has a
(15x40)/20 = 30 pack year smoking history.
2. Occupational carcinogens, including:(asbestos, arsenic, beryllium, cadmium,
chromium, and petroleum products and tar).
3. Environmental carcinogens: radon (product of uranium that emitting to near
homes)
Histological classification of lung cancer:
A. Non-small cell lung cancer:
1. Squamous cell carcinoma: 35- 45%: (Arises from altered bronchial epithelium).
2. Adenocarcinoma: 15%: (Arises from glandular tissue in the airway
submucosa).
3. Large cell carcinoma: 10%.
4. Carcinoid: 1%.
5. Bronchoalveolar cell carcinoma rare.
B. Small cell lung cancer: 20%: (Derived from neuroendocrine cells).
Incidence:
• Bronchial carcinoma increased dramatically during the 20th century, more women
now die of lung cancer than breast cancer in the USA and the UK. Is the most common
cause of cancer in men. It is the leading cause of cancer mortality worldwide in both
men and women than breast cancer, colon cancer, and prostate cancer.
Page of
71
105

Internal Medicine: 4
th
Stage TUCOM Dr.Hassan
Pathology:
• When the tumour arises in a large bronchus, symptoms arise early.
• But tumours originating in a peripheral bronchus can attain a very large size without
producing symptoms.
Clinical features:
I. Local features;
A. Cough is the most common early symptom often dry but sputum may be purulent if
there is secondary infection.
1. A change in the character of the 'regular' cough of a smoker is suggestive of
lung cancer.
B. Haemoptysis is a common symptom, especially in tumours arising in central
bronchi.
1. Repeated episodes of scanty haemoptysis or blood-streaking of sputum in a
smoker are highly suggestive of lung cancer.
C. Bronchial obstruction:
1. It is a common presentation depend on the site of the obstruction, whether
the obstruction is complete or partial, the presence or absence of secondary
infection, and the extent of pre-existing lung disease; which can b presented as
pneumonia, lung abscess or lung collapse.
2. Recurrent pneumonia at the same site or pneumonia which is slow to respond
to treatment, particularly in a smoker are suggestive of lung cancer.
D. Breathlessness may reflect occlusion of a large bronchus or large pleural effusion.
E. Stridor (a harsh inspiratory noise) occurs when the lower trachea, carina or main
bronchi are narrowed by the primary tumour or by compression from malignant
enlargement of the subcarinal and paratracheal lymph nodes.
II. Features due to spread into surrounding structures:
A. Features due to spread into the mediastinum and invade or compress the
pericardium, oesophagus, superior vena cava, trachea, phrenic or left recurrent
laryngeal nerves.
1. Laryngeal or lung cancer should be considered as the cause of hoarseness
lasting more than 3 weeks in smokers, due to involvement of left recurrent
laryngeal nerves.
B. Lung cancer in the apex of the lung ('superior sulcus tumour') may cause Horner's
syndrome.
C. Features due to lymphatic spread to supraclavicular and mediastinal lymph nodes
is also frequently.
D. Lung cancer may involve the pleura either directly or by lymphatic spread and may
extend into the chest wall, invading the intercostal nerves or the brachial plexus
and causing severe pain.
Page of
72
105
Internal Medicine: 4
th
Stage TUCOM Dr.Hassan
E. Pancoast's syndrome (pain in the shoulder and inner aspect of the arm) caused by
involvement of the lower part of the brachial plexus.
III. Blood-borne metastases, such as;
A. Focal neurological defects, epileptic seizures, or personality change.
B. Jaundice, bone pain or skin nodules.
C. Lassitude, anorexia and weight loss usually indicate the presence of metastatic
spread.
IV. Non-metastatic extrapulmonary manifestations;
A. Endocrine;
1. Inappropriate antidiuretic hormone (ADH) secretion causing hyponatraemia.
2. Ectopic adrenocorticotrophic hormone (ACTH) secretion.
3. Hypercalcaemia due to secretion of parathyroid hormone (PTH)-related
peptides.
4. Carcinoid syndrome.
5. Gynaecomastia.
B. Neurological:
1. Polyneuropathy
2. Myelopathy
3. Cerebellar degeneration
4. Myasthenia (Lambert-Eaton syndrome)
C. Other:
1. Digital clubbing
2. Hypertrophic pulmonary osteoarthropathy
3. Nephrotic syndrome
4. Polymyositis and dermatomyositis
5. Eosinophilia
Examinations:
• Usually normal unless there is significant bronchial obstruction.
• General examination.
• Spread to pleura, mediastinum or supraclavicular nodes.
• Lung collapse, pneumonia, monophonic or unilateral wheeze, stridor, hoarse voice
'bovine' cough, unilateral diaphragmatic palsy, pleural rub or signs of pleural effusion,
superior vena cava syndrome, Digital clubbing (HPOA).
• Hypertrophic pulmonary osteoarthropathy (HPOA). This is a painful periostitis of the
distal tibia, fibula, radius and ulna, with local tenderness. X-rays reveal subperiosteal
new bone formation. While most frequently associated with bronchial carcinoma,
HPOA can occur with other tumours.
Page of
73
105
Internal Medicine: 4
th
Stage TUCOM Dr.Hassan
• Superior vena cava obstruction by malignancy causes congestion and swelling of the
neck and face. Conjunctival oedema, headache and dilated veins on the chest wall,
the JVP is raised, dilated but nonpulstile.
Investigations:
The main aims of investigations are to confirm the diagnosis, establish the histological
cell type and define the extent of the disease.
1. CXR: common radiological features of bronchial carcinoma;
1. Unilateral hilar enlargement.
2. Peripheral pulmonary opacity.
3. Lung, lobe or segmental collapse.
4. Pleural effusion.
5. Broadening of mediastinum, enlarged cardiac shadow, elevation of a
hemidiaphragm. Rib destruction.
2. Flexible bronchoscope; The tumour is visualized directly. Bronchial biopsies and
brush samples can be taken. It is useful for proximal lesion (near to large airway).
3. Percutaneous needle biopsy under CT or ultrasound guidance; When the lesion is
peripheral.
4. Pleural biopsy; Is indicated in all patients with pleural effusions.
5. CT of chest; characterize lung lesion, staging of cancer, identify lymph nodes
involvement, direct bronchoscope to the best area of lung sampling, and direct
percutaneous needle biopsy.
Staging of lung cancer:
A. Stages of non-small cell lung cancer:
1. Stage I: located only in the lungs and has not spread to any lymph nodes.
2. Stage II: in the lung and nearby lymph nodes.
3. Stage III: in the lung and in mediastinal lymph nodes. Stage III has two
subtypes:
4. stage IIIA if spread only to lymph nodes on the same side of the chest.
5. stage IIIB if spread to the lymph nodes on the opposite side of the chest.
6. Stage IV: advanced disease, spread to both lungs, malignant pleural effusion, or
to another part of the body, such as the liver or other organs.
B. Stages of small cell lung cancer:
1. Limited stage: cancer is found on one side of the chest, involving just one part
of the lung and nearby lymph nodes.
2. Extensive stage: cancer has spread to other regions of the chest or other parts
of the body.
Page of
74
105

Internal Medicine: 4
th
Stage TUCOM Dr.Hassan
Management:
A. Non-small cell lung cancer:
1. Responds poorly to chemotherapy.
2. Surgery can be curative for localized disease.
B. Small cell lung cancer:
1. Is responsive to chemotherapy and radiotherapy.
2. Metastasize early therefore surgery has no role in the management of this
condition.
1. Surgical treatment;
• Surgical resection carries the best hope of long-term survival, but in the majority of
cases (over 85%) surgery is not possible or is inappropriate due to extensive spread or
co-morbidity.
• Careful staging and assessment of the patient's respiratory reserve and cardiac status
are essentials to surgery.
• Contraindication to surgical resection in lung cancer:
1) Distant metastasis (M1).
2) Invasion of central mediastinal structures; heart, great vessels, trachea and
oesophagus (T4).
3) Malignant pleural effusion (T4).
4) Contralateral mediastinal nodes (N3).
5) FEV
1
< 0.8 liters.
6) Severe or unstable cardiac or other medical condition.
2. Radiotherapy;
• Can be used in selected patients with localised disease in whom comorbidity
precludes surgery.
• Treatment of complications such as superior vena caval obstruction, recurrent
haemoptysis, and pain caused by chest wall invasion or by skeletal metastatic
deposits.
• Can be used in conjunction with chemotherapy in the treatment of small-cell
carcinoma.
• Prophylactic cranial irradiation: Radiotherapy to the brain to kill off any cancer cell
that may spread to the brain, use in small-cell carcinoma.
3. Chemotherapy;Small-cell carcinoma:
• Cytotoxic drugs, sometimes in combination with radiotherapy.
• Regular cycles of therapy, including combinations of intravenous cyclophosphamide,
doxorubicin and vincristine or intravenous cisplatin and etoposide, are commonly
used.
4. Laser therapy and stenting; Palliative, occluding major airways and allow re-aeration
of collapsed lung.
5. General aspects of management; pain relief, diet, depression and anxiety.
Page of
75
105
Internal Medicine: 4
th
Stage TUCOM Dr.Hassan
Prognosis;
Overall prognosis of lung cancer is very poor.
Secondary tumours of the lung;
• Usually multiple and bilateral.
• No respiratory symptoms and the diagnosis is made by radiological examination.
• Breathlessness may occur if a considerable amount of lung tissue has been replaced by
metastatic tumour.
• Usually from breast, renal, GIT, cervix, overy or testicle or lymphangitic
carcinomatosis.
Lymphangitic carcinomatosis;
• Lymphangitic carcinomatosis (LC) refers to the diffuse infiltration and obstruction of
pulmonary parenchymal lymphatic channels by tumor, usually adenocarcinma from
breast, lung, stomach and colon. patient usual presenting complaint is breathlessness.
………………………………………………………………………………………………
Endocrine
………………………………………………………………………………………………
DIABETES MELLITUS
Diabetes mellitus:
• Is a heterogeneous group of metabolic diseases that are characterized by chronic
hyperglycemia and disturbances in carbohydrate, lipid, and protein metabolism
resulting from defects in insulin secretion and/or insulin action, which can leads to
serious complications.
• Insulin is an anabolic hormone with profound effects on the metabolism of
carbohydrate, fat and protein.
• Insulin is secreted from pancreatic β cells into the portal circulation, with a brisk
increase in response to a rise in blood glucose.
Page of
76
105
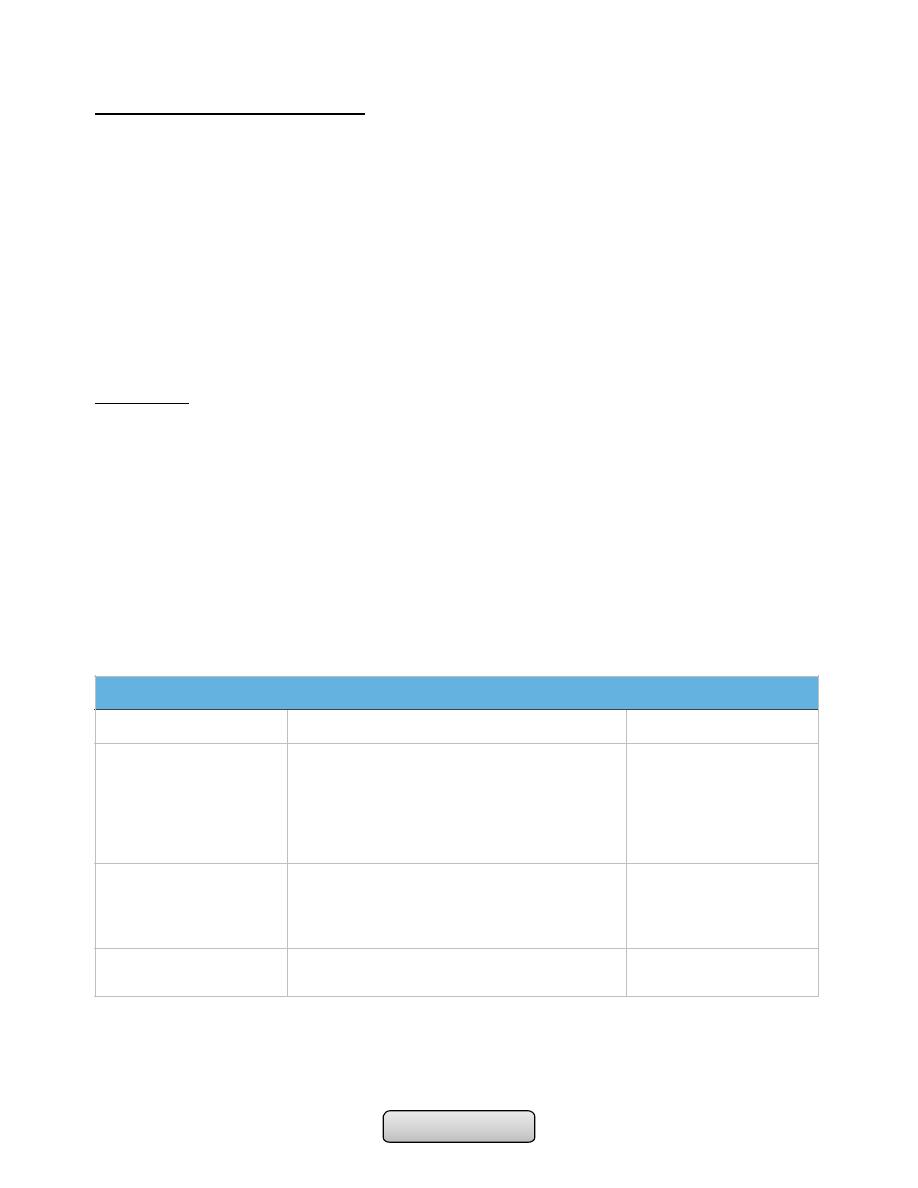
Internal Medicine: 4
th
Stage TUCOM Dr.Hassan
Endocrine function of pancreas:
• A(α) cells produce glucagon; Glucagon is a catabolic hormone. It mobilizes glucose,
fatty acids and amino acids from stores into the blood.
• B(β) cells produce insulin; Insulin is an anabolic hormone, that increases the storage
of glucose, fatty acids and amino acids in cells and tissues. Composed of 2
polypeptide chains linked by disulphide bridges. Secreted as proinsulin and
transformed to active form, insulin, by cleaveage of C peptide by protease enzymes.
• D(δ) cells produce somatostatin; Somatostatin may regulate, locally, the secretion of
the other pancreatic hormones.
• PP cells produce pancreatic polypeptide; still uncertain although the hormone may
influence gastrointestinal function and promote intra-islet homeostasis.
Physiology:
• Some characteristics of normal insulin secretion are shown in the table (next slide).
Insulin lowers blood glucose by suppressing hepatic glucose production and stimulating
glucose uptake in skeletal muscle and fat, mediated by the glucose transporter,
GLUT-4.
• Insulin stimulates lipogenesis and inhibits lipolysis, so preventing fat catabolism.
• Partial oxidation of FFAs in the liver provides energy to drive gluconeogenesis and also
produces ketone bodies (acetoacetate, which can be reduced to 3-hydroxybutyrate or
decarboxylated to acetone) which are generated in hepatocyte mitochondria.
• Insulin deficiency can lead to hyperglycemia and many metabolic derangements which
occur mainly in type 1 DM that can leads to death if not treated correctly.
Metabolic actions of insulin
Increase
Decrease
Carbohydrate
metabolism
Glucose transport (muscle, adipose tissue)
Glucose phosphorylation
Glycogen synthesis
Glycolysis
Pyruvate dehydrogenase activity
Pentose phosphate shunt
Gluconeogenesis
Glycogenolysis
Lipid metabolism
Triglyceride synthesis
Fatty acid synthesis (liver)
Lipoprotein lipase activity (adipose tissue)
Lipolysis
Lipoprotein lipase (muscle)
Ketogenesis
Fatty acid oxidation (liver)
Protein metabolism
Amino acid transport
Protein synthesis
Protein degradation
Page of
77
105
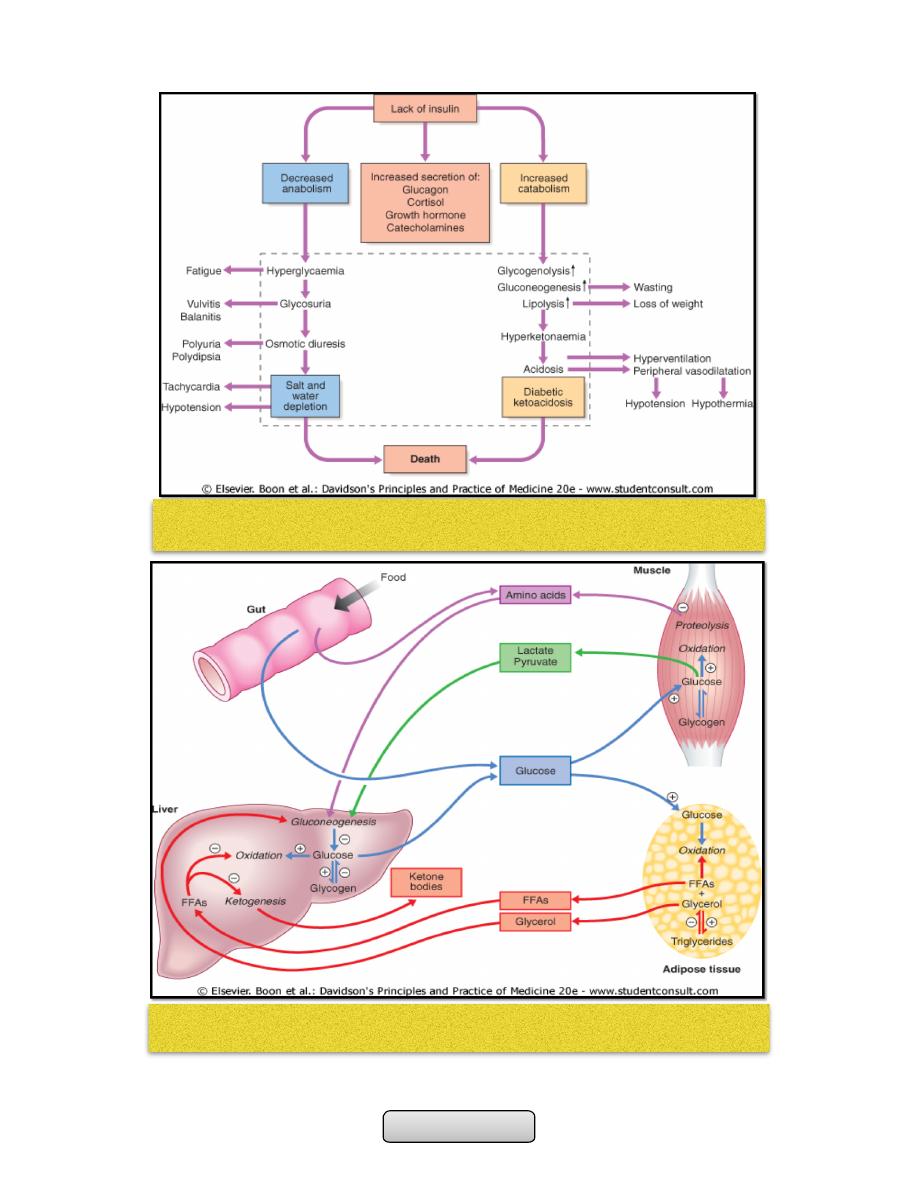
Internal Medicine: 4
th
Stage TUCOM Dr.Hassan
Page of
78
105
Insulin deficiency can lead to hyperglycemia and many metabolic derangements
which occur mainly in type 1 DM that can leads to death if not treated correctly.
Major metabolic pathways of fuel metabolism and the actions of insulin
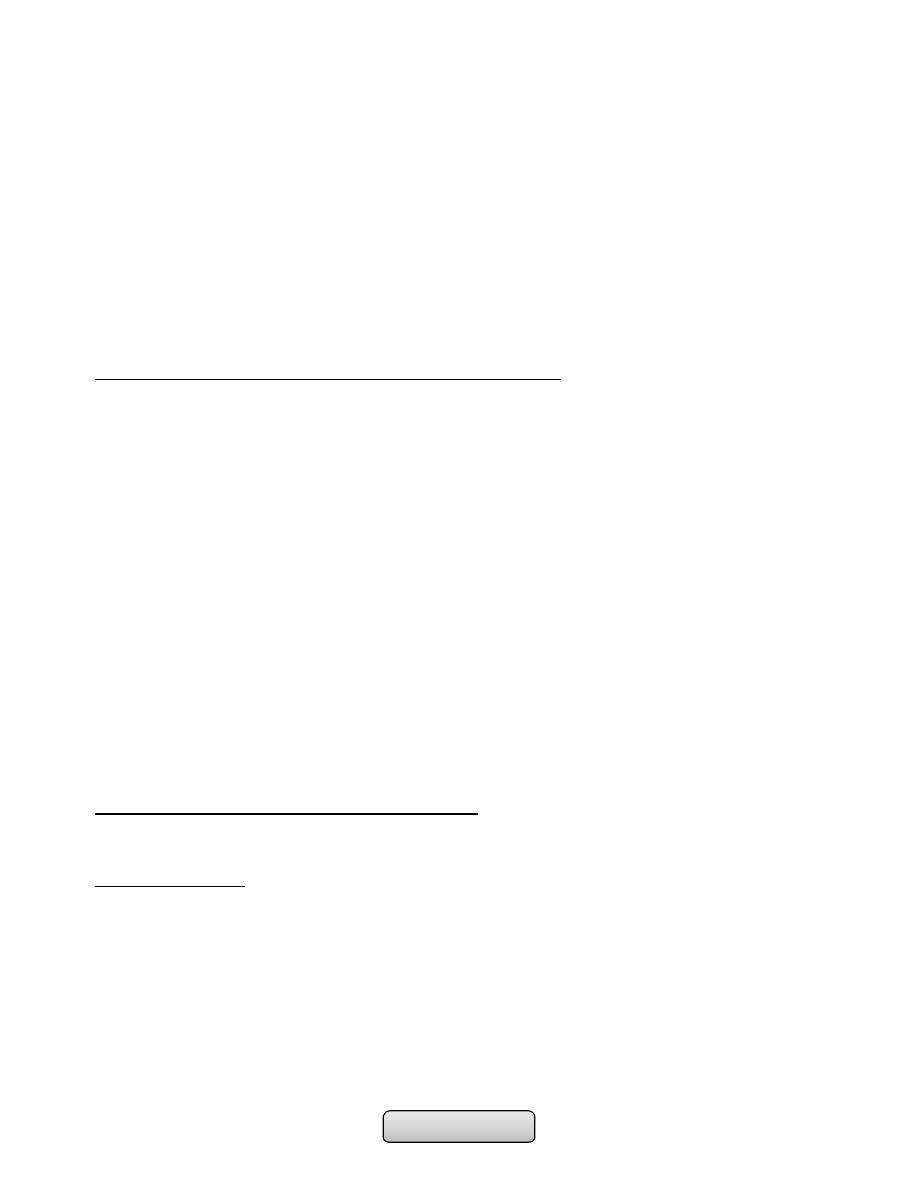
Internal Medicine: 4
th
Stage TUCOM Dr.Hassan
• A- The normal adult pancreas contains about 1 million islets which are scattered
throughout the exocrine parenchyma. Histology is shown in
• B- The core of each islet consists of β cells that produce insulin, and is surrounded by
a cortex of endocrine cells that produce other hormones including glucagon (α cells),
somatostatin (δ cells).
• C- Pro-insulin in the pancreatic β cell is cleaved to release insulin and equimolar
amounts of inert C-peptide (connecting peptide). Measurement of C-peptide can be
used to assess endogenous insulin secretory capacity.
• D- An acute first phase of insulin secretion occurs in response to an elevated blood
glucose, followed by a sustained second phase.
AETIOLOGICAL CLASSIFICATION OF DIABETES MELLITUS:
• Type 1 diabetes: Immune-mediated , Idiopathic.
• Type 2 diabetes.
• Other specific types:
-
Genetic defects of β-cell function (MODY)
-
Pancreatic disease (e.g. pancreatitis, pancreatectomy, neoplastic disease, cystic
fibrosis, haemochromatosis)
-
Excess endogenous production of hormonal antagonists to insulin (e.g. growth
hormone-acromegaly; glucocorticoids-Cushing's syndrome; glucagon-glucagonoma;
catecholamines- phaeochromocytoma; thyroid hormones-thyrotoxicosis)
-
Drug-induced (e.g. corticosteroids, thiazide diuretics, phenytoin)
-
Viral infections (e.g. congenital rubella, mumps, Coxsackie virus B)
-
Uncommon forms of immune-mediated diabetes (LADA)
-
Associated with genetic syndromes (e.g. Down's syndrome; Klinefelter's syndrome;
Turner's syndrome; DIDMOAD (Wolfram's syndrome)-diabetes insipidus, diabetes
mellitus, optic atrophy, nerve deafness; Friedreich's ataxia; myotonic dystrophy)
• Gestational diabetes.
AETIOLOGY AND PATHOGENESIS OF DIABETES:
In both of the common types of diabetes, environmental factors interact with genetic
susceptibility.
TYPE 1 DIABETES:
• It is a slowly progressive T cell-mediated autoimmune disease, destruction of the
insulin-secreting cells in the pancreatic islets takes place over many years.
Hyperglycaemia accompanied by the classical symptoms of diabetes occurs only when
70-90% of β cells have been destroyed.
• 'insulitis', infiltration of the islets with mononuclear cells containing activated
macrophages. the initial patchiness of this lesion. the striking β-cell specificity of the
destructive process, with the glucagon and other hormone-secreting cells in the islet
invariably remaining intact.
Page of
79
105
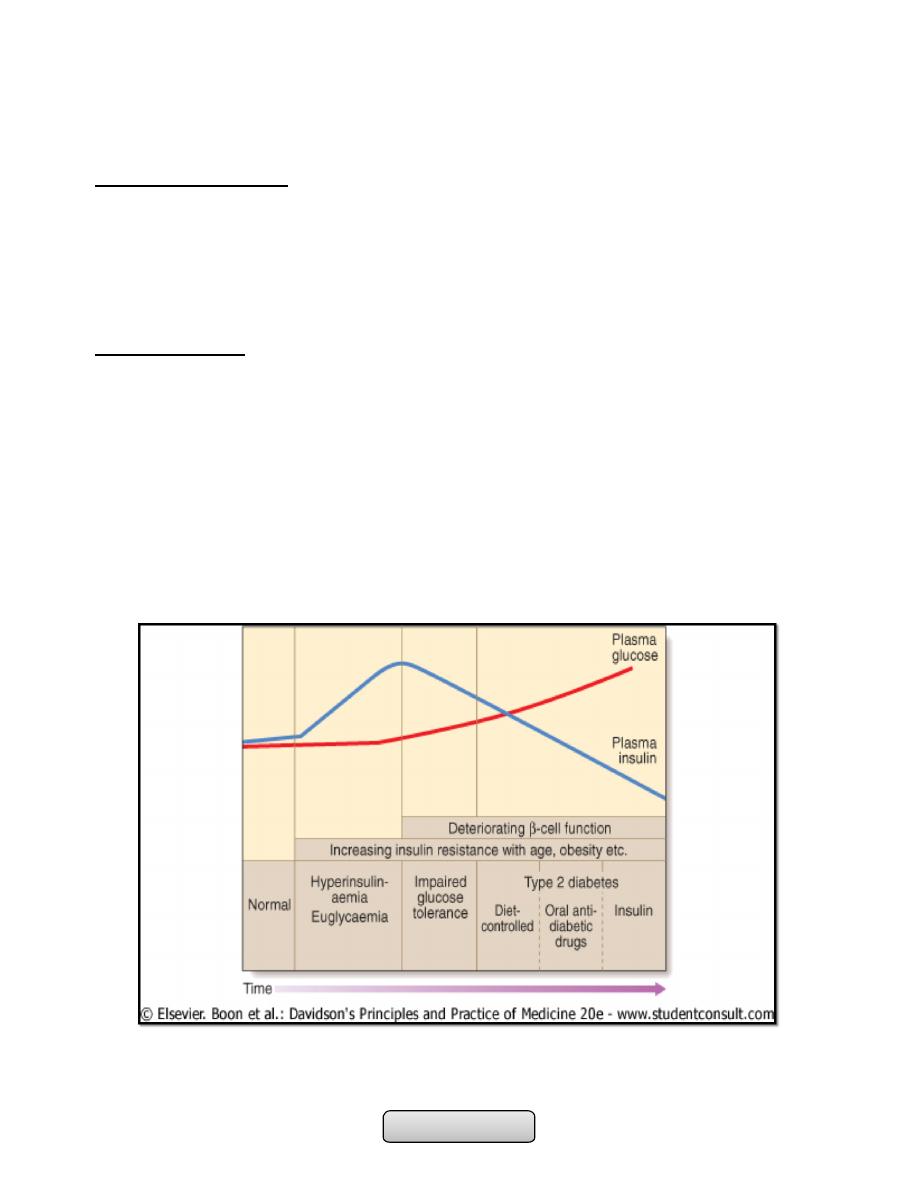
Internal Medicine: 4
th
Stage TUCOM Dr.Hassan
• Type 1 diabetes is associated with other autoimmune disorders, including thyroid
disease, coeliac disease, Addison's disease, pernicious anaemia and vitiligo.
Environmental factors;
Viral infection cause autoimmune damage to β-cells, including mumps, Coxsackie B4,
retroviruses, rubella (in utero), cytomegalovirus and Epstein-Barr virus.
Bovine serum albumin (BSA), a major constituent of cow's milk.
Various nitrosamines
Stress
TYPE 2 DIABETES:
• More complex; is a combination of resistance to the actions of insulin in liver and
muscle together with impaired pancreatic β-cell function leading to 'relative' insulin
deficiency.
• Coexisted with 'metabolic syndrome‘.
• Pathological changes; is deposition of amyloid.
• In the early stage of the disorder the response to progressive insulin resistance is an
increase in insulin secretion by the pancreatic cells, causing hyperinsulinaemia.
Eventually the β cells are unable to compensate adequately and blood glucose rises,
producing hyperglycaemia. With further β-cell failure (type 2 diabetes) glycaemic
control deteriorates and treatment requirements escalate.
Page of
80
105
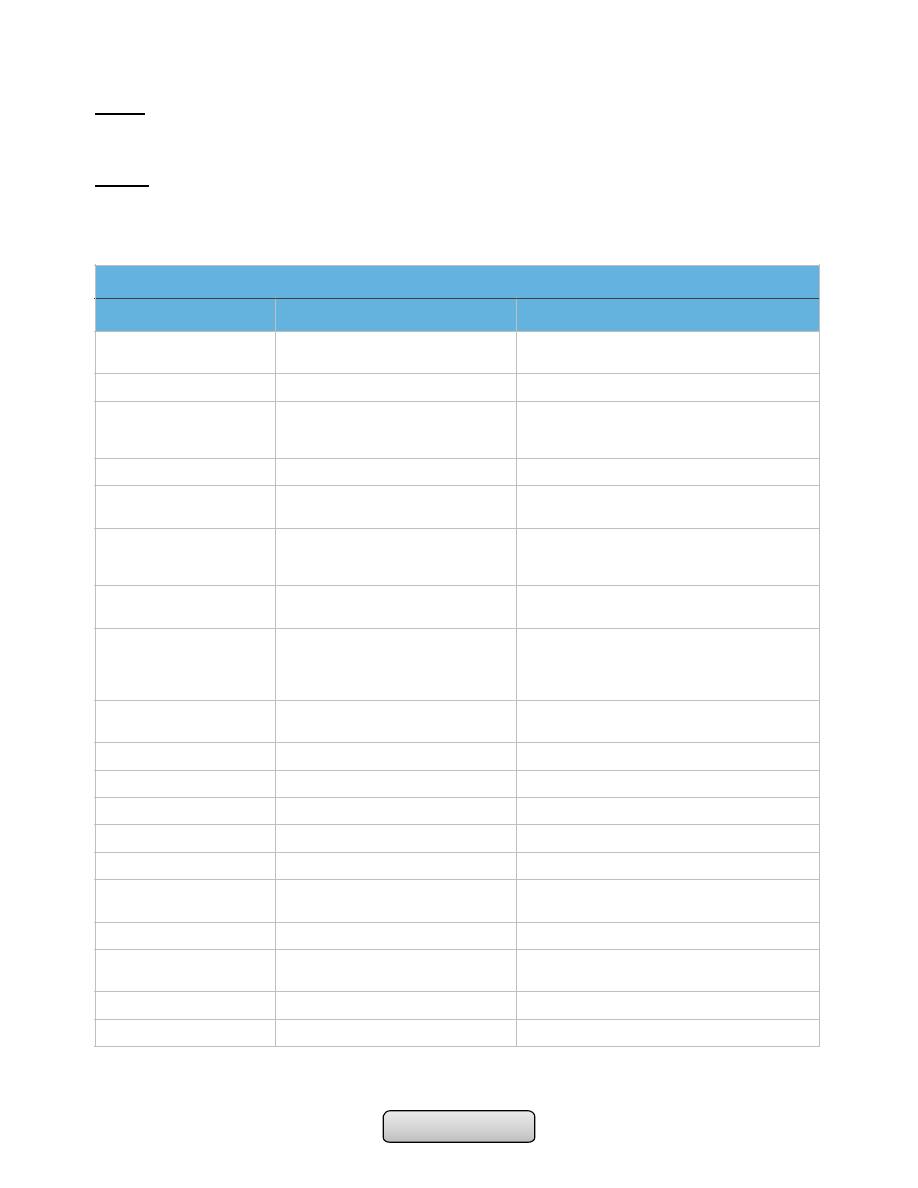
Internal Medicine: 4
th
Stage TUCOM Dr.Hassan
LADA:
Latent autoimmune diabetes of adult, is form of type 1 DM occur in middle aged
patients.
MODY:
Maturity onset diabetes of young, is a rare autosomal form of type 2 DM (less than 5% of
cases of DM) affecting young people with positive family history.
Comparison of the Two Types of Diabetes Mellitus
Type 1
Type2
Previous terminology
Insulin-dependent diabetes mellitus (IDDM),
type I, juvenile- onset diabetes
Non-insulin-dependent diabetes mellitus, type II, adult-
onset diabetes
Age of onset
Usually < 30yr
Usually > 40 yr
Genetic predisposition
Moderate; environmental factors required for
expression; 35-50% concordance in
monozygotic twins
Strong; 60-90% concordance in monozygotic twins
Family history
Uncommon
Common
Human leukocyte antigen
associations
Linkage to DQA and DQB, influenced by DRB
None known
Other associations
Autoimmune; Graves’ disease, Hashimoto's
thyroiditis, vitiligo, Addison's disease,
pernicious anemia
Metabolic syndrome
Precipitating and risk factors
Largely unknown; microbial, chemical,
dietary, other
Age, obesity (central), sedentary lifestyle, previous
gestational diabetes.
Findings at diagnosis
85-90% of patients have one or more
autoantibodies like; islet cell antibodies (ICA)
and glutamic acide decarboxylase (GAD)
antibodies
Possibly complications =25"/o (microvascular and
macrovascular) caused by significant hyperglycemia in
the preceding asymptomatic period
Endogenous insulin levels
absent
Usually present (relative deficiency), early
hyperinsulinemia
Insulin resistance
absent
present
Prolonged fast
Hyperglycemia, ketoacidosis
Euglycemia
Duration of symptoms
Weeks
Months to years
Body weight
Low
Obese
Ketonuria
Yes
No
Rapid death without treatment
with insulin
Yes
No
Autoantibodies
Yes
No
Diabetic complications at
diagnosis
No
25%
% of cases of DM
5- 15%
75- 85%
Other autoimmune disease
Common
Uncommon
Page of
81
105
Internal Medicine: 4
th
Stage TUCOM Dr.Hassan
SYMPTOMS OF HYPERGLYCAEMIA:
1. Thirst, dry mouth
2. Polyuria
3. Nocturia
4. Tiredness, fatigue
5. Recent change in weight
6. Blurring of vision
7. Pruritus vulvae, balanitis (genital candidiasis)
8. Nausea, headache
9. Hyperphagia; predilection for sweet foods
10.Mood change, irritability, difficulty in concentrating, apathy
INVESTIGATIONS:
1. URINE TESTING:
-
Glucose; By using sensitive glucose-specific dipsticks 1-2 hours after a meal since this
will detect more cases of diabetes than a fasting specimen.
-
Ketones; By using dipsticks for ketones. Ketonuria is not pathognomonic of diabetes
but, if associated with glycosuria, the diagnosis of diabetes is highly likely.
-
Protein; Dipstick testing for albumin. This will detect urinary albumin greater than
300 mg/l. Smaller amounts of urinary albumin from 30 to 300 mg/24 hours
(microalbuminuria) can be measured by special kit and these provide indicators of
the risk of developing diabetic nephropathy.
2. Blood testing:
-
Glucose; In general, venous plasma values are the most reliable for diagnostic
purposes. Glycated haemoglobin (HbA
1c
); provides an accurate and objective
measure of glycaemic control over a period of weeks to months but is not sufficiently
sensitive to make a diagnosis. HbA
1c
estimates may be erroneously diminished in
anaemia or during pregnancy, and may be difficult to interpret in uraemia or a
haemoglobinopathy. Glycated serum proteins ('fructosamine') can be measured used
in diabetic pregnancy.
-
Blood lipids; Serum lipids-total cholesterol, low-density and high-density lipoprotein
(LDL and HDL) cholesterol and triglyceride-is another important index of overall
metabolic control.
-
Oral glucose tolerance test (OGTT): Done when there is doubt about diagnosis of DM
Plasma glucose measured before, and 2 hrs after, 75 g glucose load taken orally.
Page of
82
105
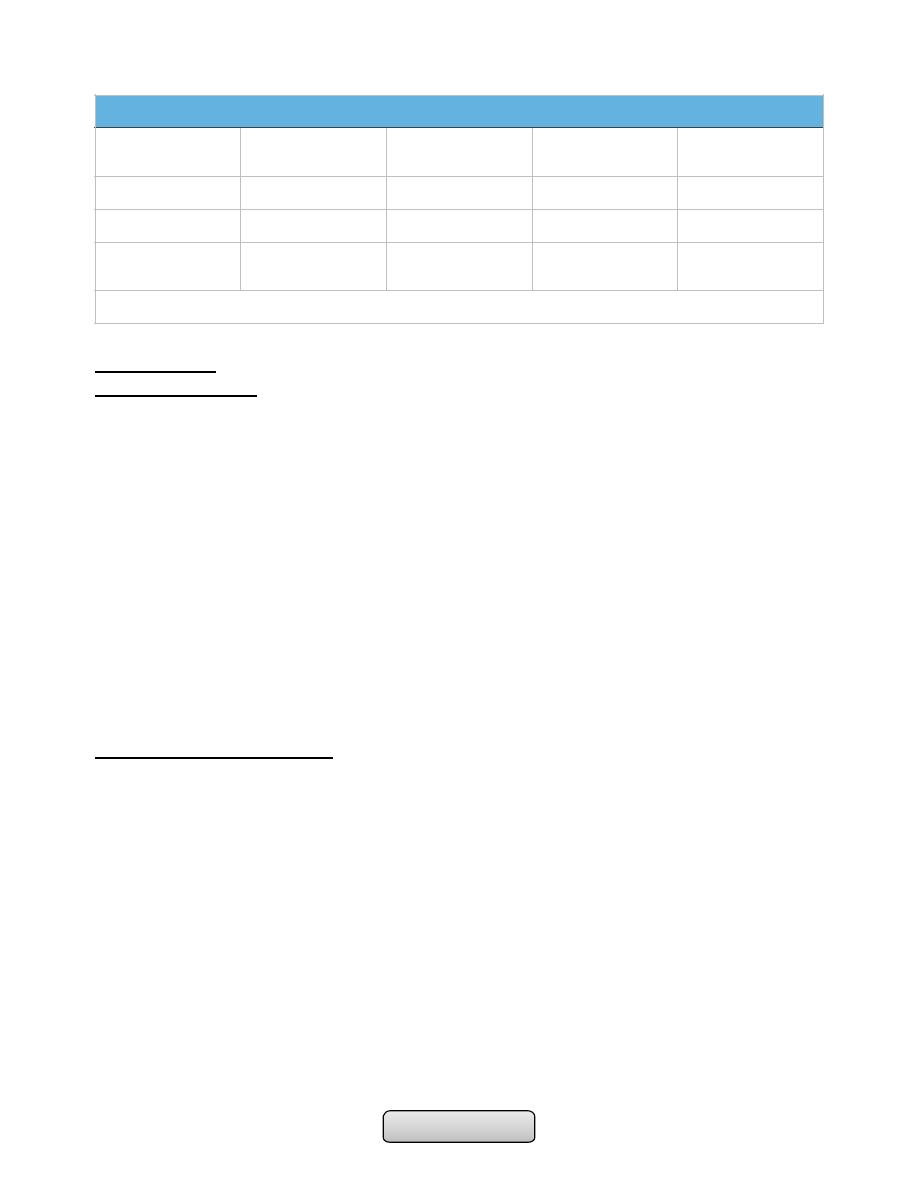
Internal Medicine: 4
th
Stage TUCOM Dr.Hassan
MANAGEMENT:
Educating patients;
• Understand their condition.
• Those requiring insulin need to learn how to measure their dose of insulin accurately
with an insulin syringe or pen device, to give their own injections and to adjust the
dose themselves on the basis of blood glucose values and other factors such as
exercise, illness and episodic hypoglycaemia.
• Familiar with the symptoms of hypoglycaemia .
• Self-assessment of glycaemic control.
• Diet= decrease saturated fat, decrease sugar intake, increase starch, moderate
protein intake.
• Smoking cessation.
• Foot care.
• Preconception advice.
• Regular exercise.
ORAL ANTI-DIABETIC DRUGS:
1. SULPHONYLUREAS;
-
Mechanism of action; The principal effect of sulphonylureas is to stimulate the
release of insulin from the pancreatic β cell.
-
Indications for use sulphonylureas are valuable in the treatment of non-obese
patients with type 2 diabetes who fail to respond to dietary measures alone.
-
The first-generation; Tolbutamide, Chlorpropamide.
-
The second-generation; gliclazide and glipizide cause few side-effects, but
glibenclamide is prone to induce severe hypoglycaemia and should be avoided in the
elderly.
-
Newer long-acting preparations such as glimepiride and a modified-release form of
gliclazide can be administered once daily with no apparent increased risk of
hypoglycaemia.
Diagnostic criteria of DM-WHO
Plasma Glucose
Normal
Impaired Fasting
Glucose
Impaired Glucose
tolerance
Diabetes Mellitus
Fasting
<11o (6.1)
>110 & <126
>126 (7.0)
2-Hour
<14o (7.8)
>140 & <200
>200 (11.1)
Random
>200 with
symptoms
Note: In asymptomatic patients, two diagnostic tests are required to confirm diabetes.
Page of
83
105

Internal Medicine: 4
th
Stage TUCOM Dr.Hassan
-
Primary treatment failures; People with type 2 diabetes who fail to respond to initial
treatment with sulphonylureas.
-
Secondary failure; (i.e. after a period of satisfactory glycaemic control).
2. BIGUANIDES; Metformin is the only biguanide available.
-
Mechanism of action; It has no hypoglycaemic effect in non-diabetic individuals, but
in diabetes, insulin sensitivity and peripheral glucose uptake are increased.
-
Indications for use; metformin is not associated with a rise in body weight and it is
therefore preferred for the obese patient. In addition, It has a synergistic with
sulphonylurea drugs, the two can be combined when either alone has proved
inadequate.
-
The main SE are diarrhea, abdominal cramps, bloating and nausea.
3. ALPHA-GLUCOSIDASE INHIBITORS;
-
They delay carbohydrate absorption in the gut by selectively inhibiting
disaccharidases. Acarbose or miglitol is available and is taken with each meal. Both
lower post-prandial blood glucose and modestly improve overall glycaemic control.
-
They can be combined with a sulphonylurea.
-
The main side-effects are flatulence, abdominal bloating and diarrhoea.
4. THIAZOLIDINEDIONES; (glitazones):
-
They work by enhancing the actions of endogenous insulin.
-
For use Rosiglitazone or Pioglitazone are usually prescribed as second-line therapy
with sulphonylureas in patients intolerant of metformin, or as third-line therapy in
combination with sulphonylurea and metformin. However, their use as monotherapy
and in combination with insulin is likely to increase.
-
Side-effects; liver dysfunction, sodium and fluid retention, must be avoided in
patients with cardiac failure.
5. MEGLITINIDES AND AMINO ACID DERIVATIVES; Repaglinide and Nateglinide:
-
These drugs are called prandial glucose regulators, directly stimulates endogenous
insulin secretion and are taken immediately before food.
-
These drugs are less likely to cause hypoglycaemia than sulphonylureas.
Drugs according to the organs:
Liver:
• Action: Decrease glucose synthesis or output.
• Drugs:
-
Metformin.
-
Thiazolidinediones.
Pancreas:
• Action: Insulin replacement.
• Drugs: Insulin.
• Or:
• Action: Increase insulin secretion.
Page of
84
105
Internal Medicine: 4
th
Stage TUCOM Dr.Hassan
• Drugs:
-
Sulphonylureas.
-
Meglitinide.
-
Amino acids derivatives.
Gut:
• Action: Delay glucose absorption.
• Drugs: Alph-glucosidase inhibitors.
Adipose tissue:
• Action: Increase peripheral glucose uptake.
• Drugs: Metformin.
• Or:
• Action: Increase glucose sensitivity.
• Drugs: Thiazolidinediones.
COMBINED ORAL ANTI-DIABETIC THERAPY AND INSULIN:
• In diabetic patients who are requiring increasing doses of a sulphonylurea or
biguanide, either alone or in combination with each other or with a thiazolidinedione,
the introduction of a single dose of an intermediate- or long-acting insulin (usually
isophane), administered at bedtime, may improve glycaemic control and delay the
development of overt pancreatic β-cell failure.
Incretin-based therapies:
• The incretin effect is the augmentation of insulin secretion seen when a glucose
stimulus is given orally rather than intravenously, and reflects the release of incretin
peptides from the gut. The incretin hormones are primarily glucagon-like peptide 1
(GLP-1) and gastric inhibitory polypeptide (GIP).
INSULIN:
Manufacture and formulation;
• Insulin was discovered in 1921, and obtained from animal sources (bovine and porcine
insulin).
• After 1980, the use of recombinant DNA technology has enabled large-scale
production of human insulin.
• Recently, rDNA and protein engineering techniques that alter the amino acid sequence
of insulin have been used to produce 'monomeric' analogues of insulin, which are more
rapidly absorbed from the site of injection (e.g. insulin lispro or aspart).
Page of
85
105
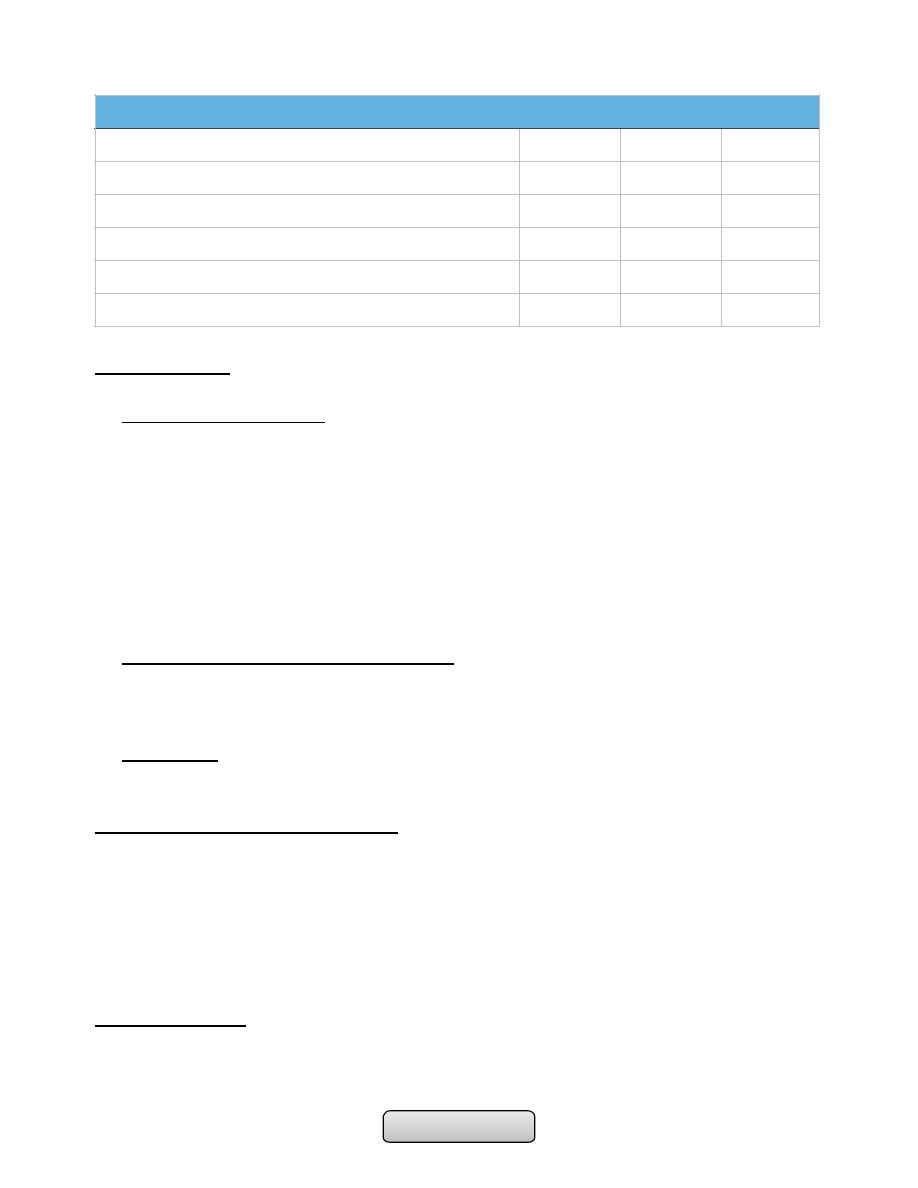
Internal Medicine: 4
th
Stage TUCOM Dr.Hassan
Insulin delivery:
The strength of insulin is 100 u/ml.
1. Subcutaneous injection;
• The most common rout, into the anterior abdominal wall, upper arms, outer thighs
and buttocks.
• Used in:
-
Type 1 DM.
-
Type 2 DM; in combination with OHA, pregnant woman, or sever illness or major
surgery require hospital admission.
-
Gestational DM.
• By using a battery-powered portable insulin pump or a disposable plastic syringe with
a fine needle (which can be reused several times), or pen device.
2. Intramuscular injection or I.V. infusion:
• Use just soluble insulin or rapidly acting insulin analogue, by using infusion pump
providing continuous intravenous infusion of insulin.
• Use in treatment of DKA or NKHDC.
3. Other rout;
• Intraperitoneal injection: in patient on peritoneal dialysis.
SIDE-EFFECTS OF INSULIN THERAPY:
Hypoglycaemia
Weight gain
Peripheral oedema (insulin treatment causes salt and water retention in the short term)
Insulin antibodies (animal insulins)
Local allergy (rare)
Lipodystrophy at injection sites
INSULIN REGIMEN:
1. Twice-daily administration of a short-acting and intermediate-acting insulin (usually
soluble and isophane insulins), given in combination before breakfast and the evening
Duration of action (in hours) of insulin preparations
Insulin
Onset
Peak
Duration
Rapid-acting (insulin analogues-lispro, aspart, glulisine)
< 0.5
0.5-2.5
3-4.5
Short-acting (soluble (regular)
0.5-1
1-4
4-8
Intermediate-acting (isophane (NPH), lente)
1-3
3-8
7-14
Long-acting (bovine ultralente)
2-4
6-12
12-30
Long-acting (insulin analogues- glargine, detemir)
1-2
None
18-24
Page of
86
105

Internal Medicine: 4
th
Stage TUCOM Dr.Hassan
meal, is the simplest regimen and is still commonly used. Individual requirements vary
considerably but usually two-thirds of the total daily requirement of insulin is given in
the morning in a ratio of 1:2, short:intermediate-acting insulins. The remaining third
is given in the evening, and doses are adjusted according to blood glucose monitoring.
2. Multiple injection regimens are popular, with short-acting insulin being taken before
each meal, and intermediate-acting insulin being injected at bedtime (basal-bolus
regimen). This type of regimen allows greater freedom of timing of meals and is of
value to individuals with variable day-to-day activities, but snacks may have to be
taken between meals to prevent hypoglycaemia.
3. Once-daily injections rarely achieve satisfactory glycaemic control and are reserved
either for some elderly patients or for those who retain substantial endogenous insulin
secretion and have a low insulin requirement.
Honey moon period;
• The pancreas of patient with type 1 DM may partially recover after the initial
diagnosis resulting in decrease insulin requirement.
COMPLICATIONS OF DM:
A. ACUTE COMPLICATIONS:
1. Hypoglycemia.
2. Diabetic Ketoacidosis.
3. Hyperosmolar Nonketotic Syndrome (HNKS).
4. Lactic Acidosis.
B. CHRONIC COMPLICATIONS:
1. Microvascular;
a) Retinopathy.
b) Neuropathy.
c) Nephropathy.
2. Macrovascular;
a) Coronary artery disease.
b) Peripheral arterial disease.
c) Cerebrovascular disease
………………………………………………………………………………………………
Page of
87
105
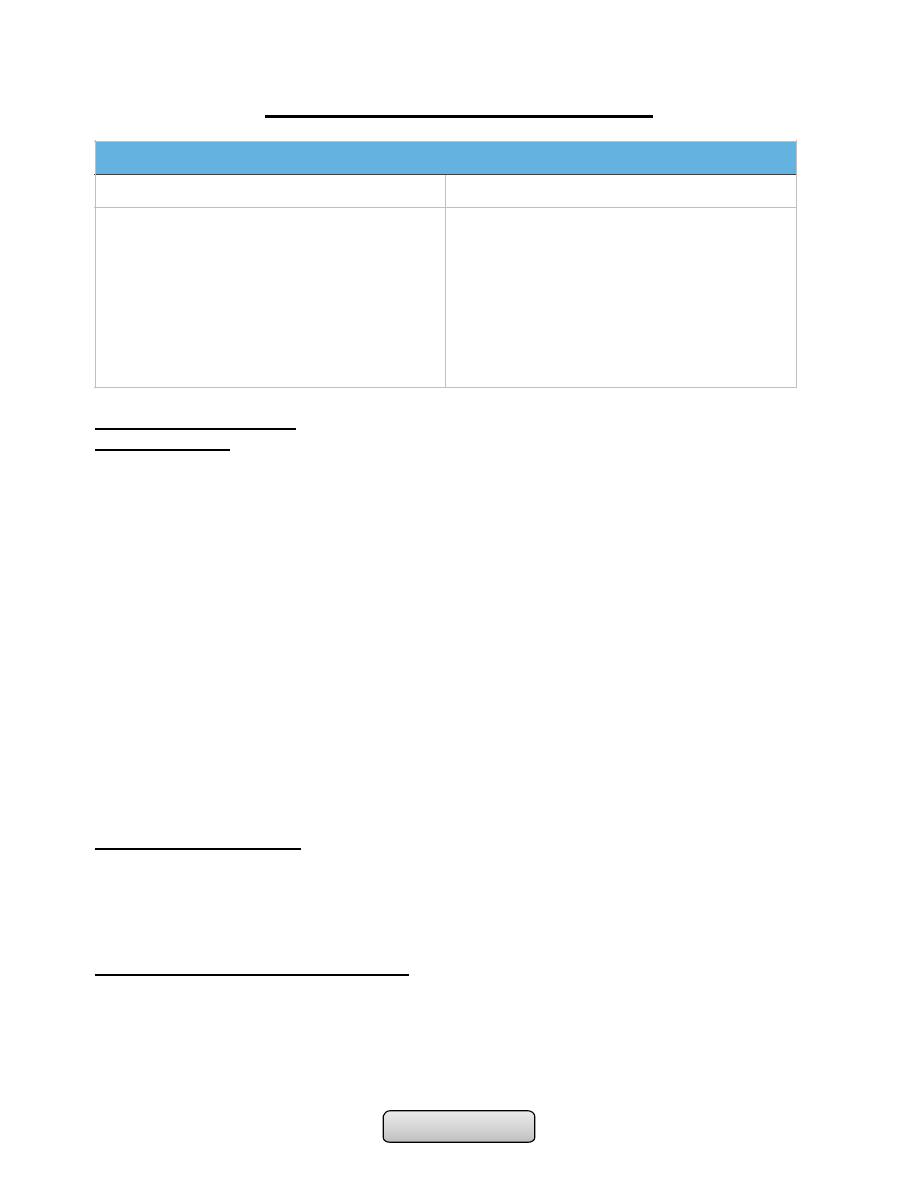
Internal Medicine: 4
th
Stage TUCOM Dr.Hassan
COMPLICATIONS OF DIABETES MELLITUS
ACUTE COMPLICATIONS:
HYPOGLYCEMIA:
• Definition:Hypoglycemia is a clinical syndrome of diverse causes in which low levels of
serum glucose can eventually lead to neuroglycopenia. Which documented by
Whipple's triad: signs and symptoms of hypoglycemia, in the presence of a low plasma
glucose concentration <45 mg/dL (2.5 mmol/L), that are relieved by restoration of
plasma glucose to normal concentrations.
• The lower limit of the fasting plasma glucose concentration is normally approximately
70 mg/dL (3.9 mmol/L) but low plasma glucose values without signs and symptoms, or
vice versa, do not constitute clinical hypoglycemia.
• As plasma glucose levels decline just below the physiologic range, glucose
counterregulatory (plasma glucose–raising) hormones are released, among these:
1.
Reduce insulin secretion
2.
Increase glucagon secretion
3.
Increase epinephrine secretion
4.
Increase cortisol and growth hormone secretion
• Glucagon is the most important in the acute response to hypoglycemia.
• In patients with type 1 diabetes of more than 5 years duration, the glucagon response
is lost. After 10 years the epinephrine response will be lost.
Causes of hypoglycemia:
1.
Hypoglycemia in diabetic patients; it is a result of treatment and not a
manifestation of the disease itself.
2.
Hypoglycemia in non-diabetic patients; it is called 'spontaneous' hypoglycemia,
which have different causes and require different investigations.
Causes of hypoglycaemia in diabetes:
1.
Missed, delayed or inadequate meal.
2.
Unexpected or unusual exercise.
3.
Alcohol.
4.
Errors in oral hypoglycaemic agent or insulin dose.
5.
Lipohypertrophy at injection sites.
COMPLICATIONS OF DIABETES MELLITUS
ACUTE COMPLICATIONS
CHRONIC COMPLICATIONS
1. Hypoglycemia.
2. Diabetic Ketoacidosis.
3. Non-ketotic Hyperosmolar Diabetic
Syndrome or Coma.
4. Lactic Acidosis
1. Microvascular;
1. Nephropathy.
2. Retinopathy.
3. Neuropathy.
2. Macrovascular;
1. Coronary artery disease.
2. Cerebrovascular disease.
3. Peripheral arterial disease
Page of
88
105
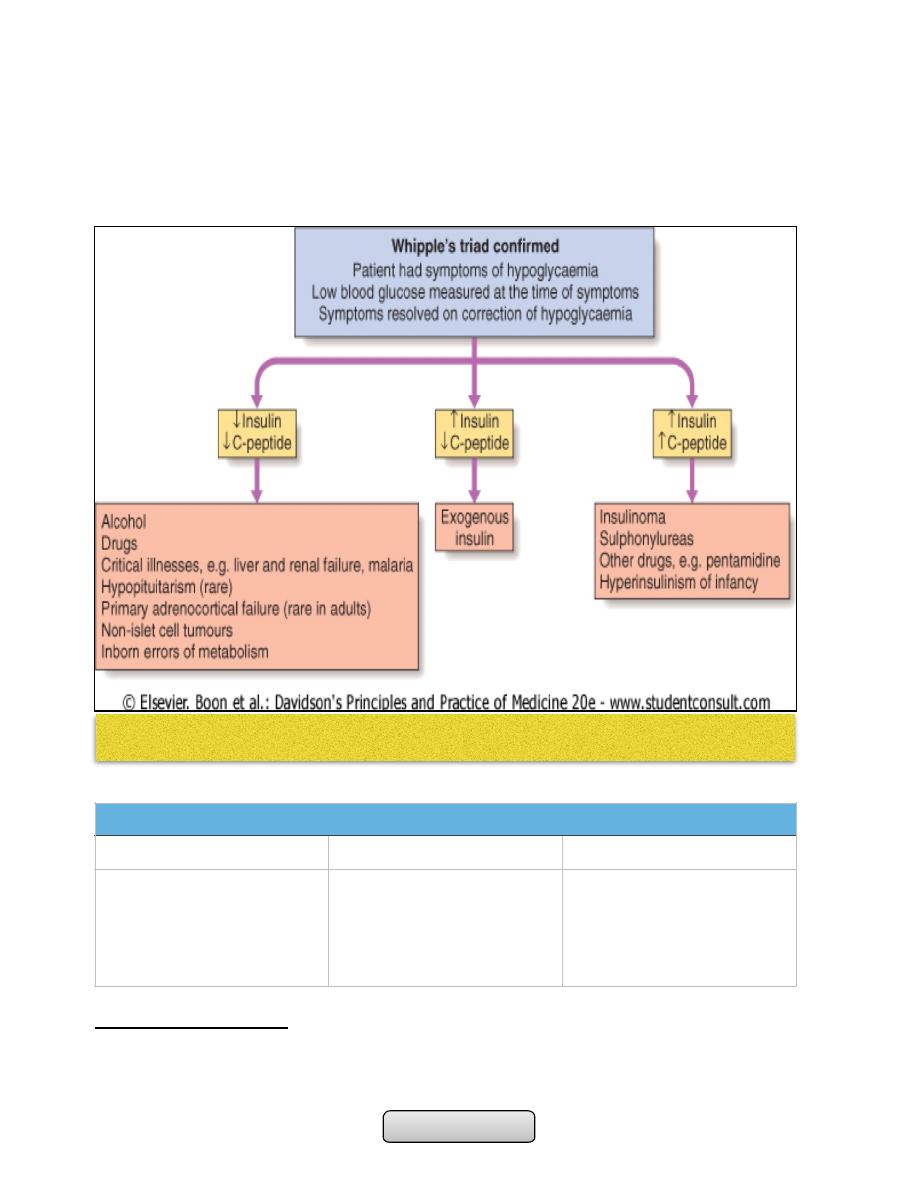
Internal Medicine: 4
th
Stage TUCOM Dr.Hassan
6.
Gastroparesis due to autonomic neuropathy.
7.
Malabsorption, e.g. coeliac disease.
8.
Unrecognised other endocrine disorder, e.g. Addison's disease.
9.
Factitious (patient induced).
10.
Breastfeeding by diabetic mother
Severe hypoglycaemia;
• Defined as any episode requiring the assistance of another person for recovery, can
result in serious morbidity and has a recognized mortality of 2-4% in insulin-treated
patients.
SIGNS AND SYMPTOMS OF HYPOGLYCEMIA
Autonomic
Neuroglycopenic
Non-specific
Sweating
Trembling
Pounding heart
Hunger
Anxiety
Confusion
Drowsiness
Speech difficulty
Inability to concentrate
Incoordination
Nausea
Tiredness
Headache
Page of
89
105
Causes of spontaneous hypoglycaemia
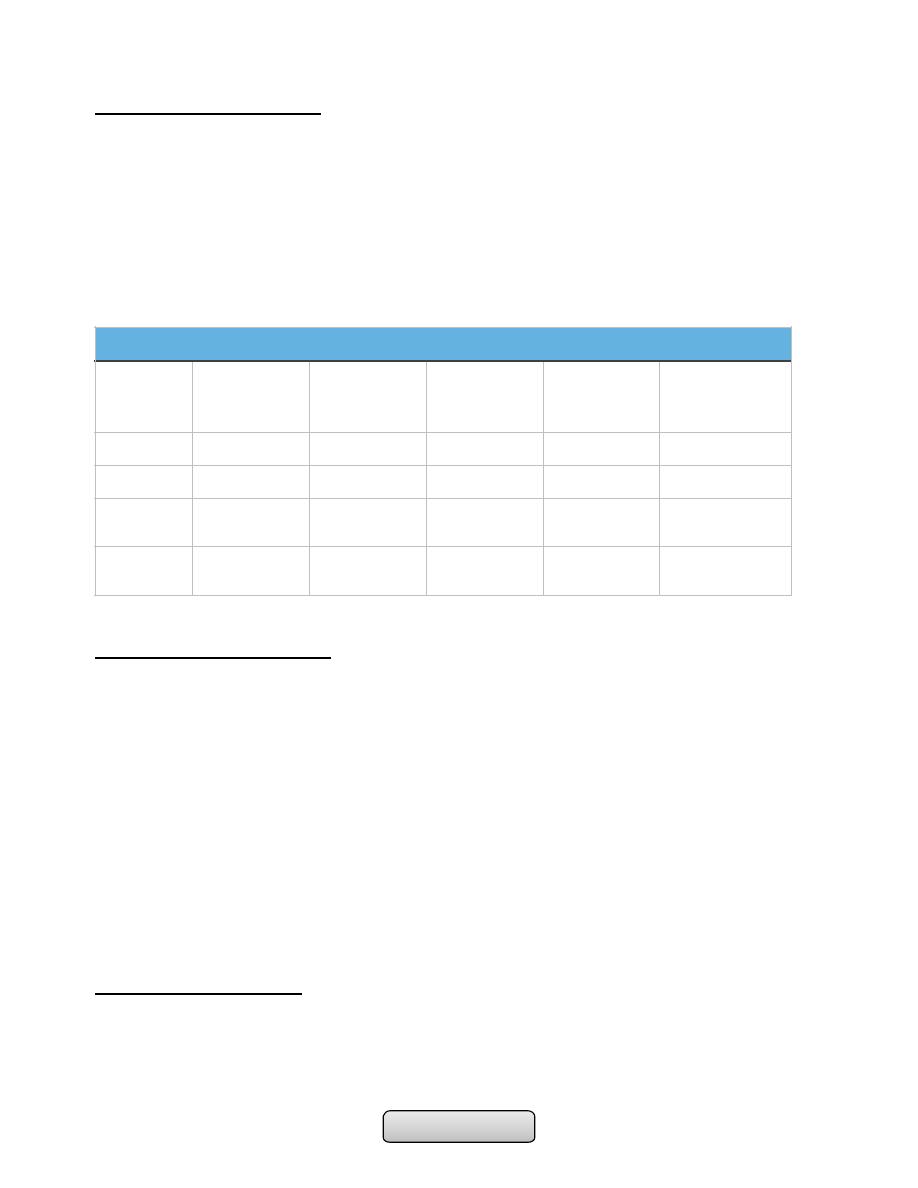
Internal Medicine: 4
th
Stage TUCOM Dr.Hassan
Diagnosis of hypoglycemia:
1.
Clinical suspicion: in patients with typical symptoms, confusion, altered level of
consciousness, seizure, or in a clinical setting in which hypoglycemia is known to
occur.
2.
Documentation of Whipple's triad.
3.
Blood sample: to confirm hypoglycaemia and for later measurement of insulin, C-
peptide, proinsulin and circulating oral hypoglycemic agents.
4.
Note: Hypoglycaemia + high insulin + high C-peptide concentrations = insulinoma
or sulphonylurea ingestion.
Treatment of hypoglycemia:
• If the patient is unable to swallow, intravenous glucose (30-50 ml of 20-50% dextrose)
or glucagon as 1 mg by intramuscular injection (but this is ineffective in patients with
depleted glycogen reserves such as liver disease).
• As soon as the patient is able to swallow, glucose should be given orally. Full recovery
may not occur immediately and reversal of cognitive impairment may not be
complete until 60 minutes after normoglycaemia is restored.
• The possibility of recurrence should be anticipated in a patient using a long- or
intermediate-acting insulin or a long-acting sulphonylurea and to prevent this a 10%
dextrose infusion, titrated to the patient's blood glucose, may be necessary.
• Causes of failure to regain consciousness after blood glucose is restored to normal:
1.
Cerebral oedema.
2.
Alcohol intoxication.
3.
Post-ictal state.
4.
Cerebral haemorrhage
DIABETIC KETOACIDOSIS:
• Ketoacidosis is a major medical emergency and remains a serious cause of morbidity,
principally in people with type 1 diabetes.
• The cardinal biochemical features of DKA are:
1.
Hyperglycemia: plasma glucose levels greater than 250 mg/dL.
Interpretation of blood results in hypoglycemic patient
Condition
Plasma
Glucose (mg/
dL)
Insulin (μU/
mL)
C-Peptide
(nmol/L)
Proinsulin
(pmol/L)
Plasma
Sulfonylurea
Level (nmol/L)
Normal
≥45
<6
<0.2
<5
-
Insulinoma
≤45
≥6
≥0.2
≥5
-
Exogenous
insulin
≤45
≥6
<0.2
<5
-
Sulfonylure
a agents
≤45
≥6
≥0.2
≥5
>0.2
Page of
90
105
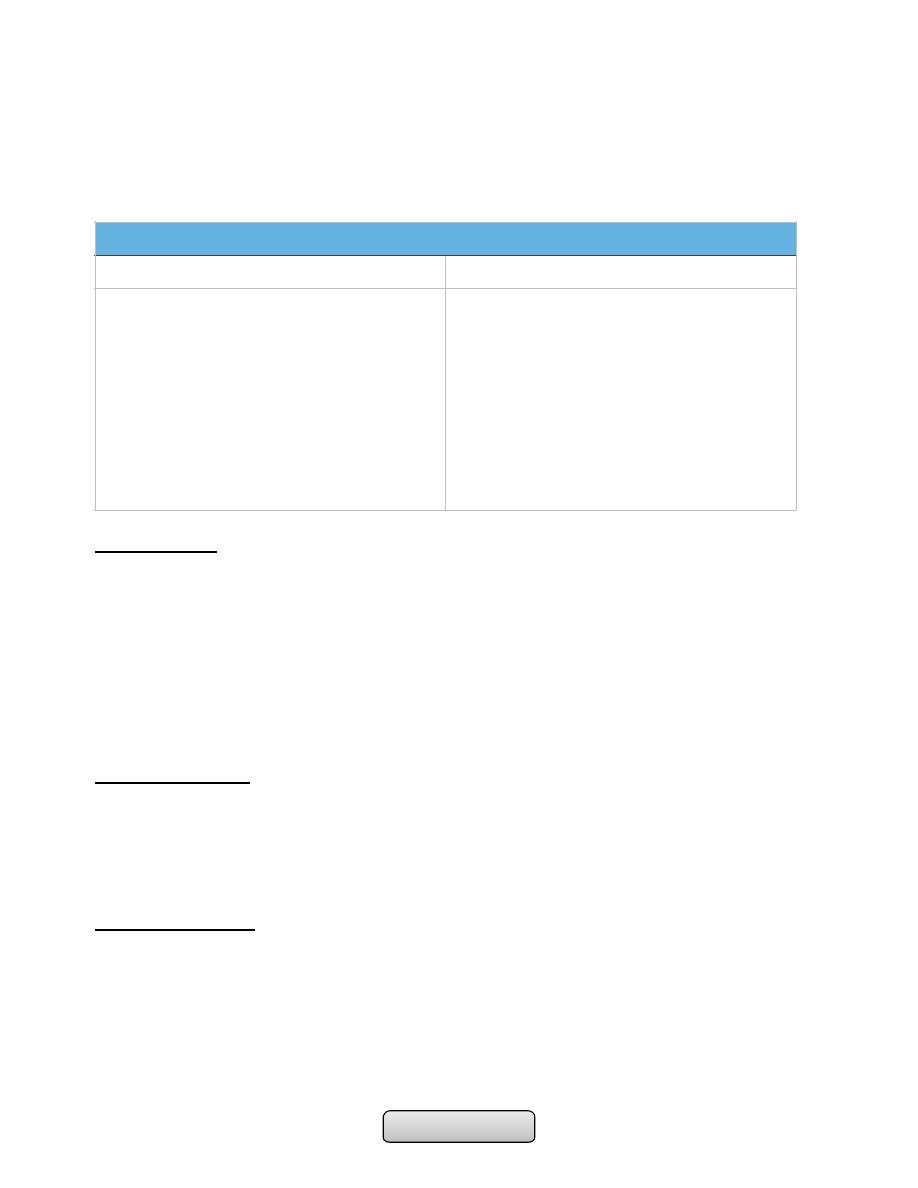
Internal Medicine: 4
th
Stage TUCOM Dr.Hassan
2.
Ketosis: moderate to severe ketonemia and moderate ketonuria (2+ to 3+ by
the nitroprusside method).
3.
Acidosis: pH less than or equal to 7.3 and/or bicarbonate less than or equal to
15 mEq/L
Investigations:
The following are important but should not delay the institution of intravenous fluid and
insulin replacement:
1.
Blood glucose, urea and electrolytes,, plasma bicarbonate.
2.
Arterial blood gases to assess the severity of acidosis.
3.
Urinalysis for ketones (a semi-quantitative guide to the plasma concentration of
acetoacetate and acetone).
4.
ECG.
5.
Infection screen: full blood count, blood and urine culture, C-reactive protein,
chest X-ray.
Treatment of DKA:
The principal components of treatment are:
1.
Fluid replacement.
2.
Administration of short-acting (soluble) insulin.
3.
Potassium replacement.
4.
Administration of antibiotics if infection is present
Fluid replacement:
• 0.9% saline (NaCl) i.v.
-
1 litre over 30 minutes
-
1 litre over 1 hr
-
1 litre over 2 hrs
-
1 litre over next 2- 4 hrs
• When blood glucose < 15 mmol/l (270 mg/dl):
-
Switch to 5% dextrose, 1 litre 8-hourly
CLINICAL FEATURES OF DIABETIC KETOACIDOSIS
Signs
Symptoms
-
Dehydration
-
Hypotension (postural or supine)
-
Cold extremities
-
Peripheral cyanosis
-
Tachycardia
-
Air hunger (Kussmaul breathing)
-
Smell of acetone
-
Hypothermia
-
Confusion, drowsiness
-
Coma
-
Polyuria
-
Thirst
-
Weight loss
-
Weakness
-
Nausea
-
Vomiting
-
Leg cramps
-
Blurred vision
-
Abdominal pain
Page of
91
105
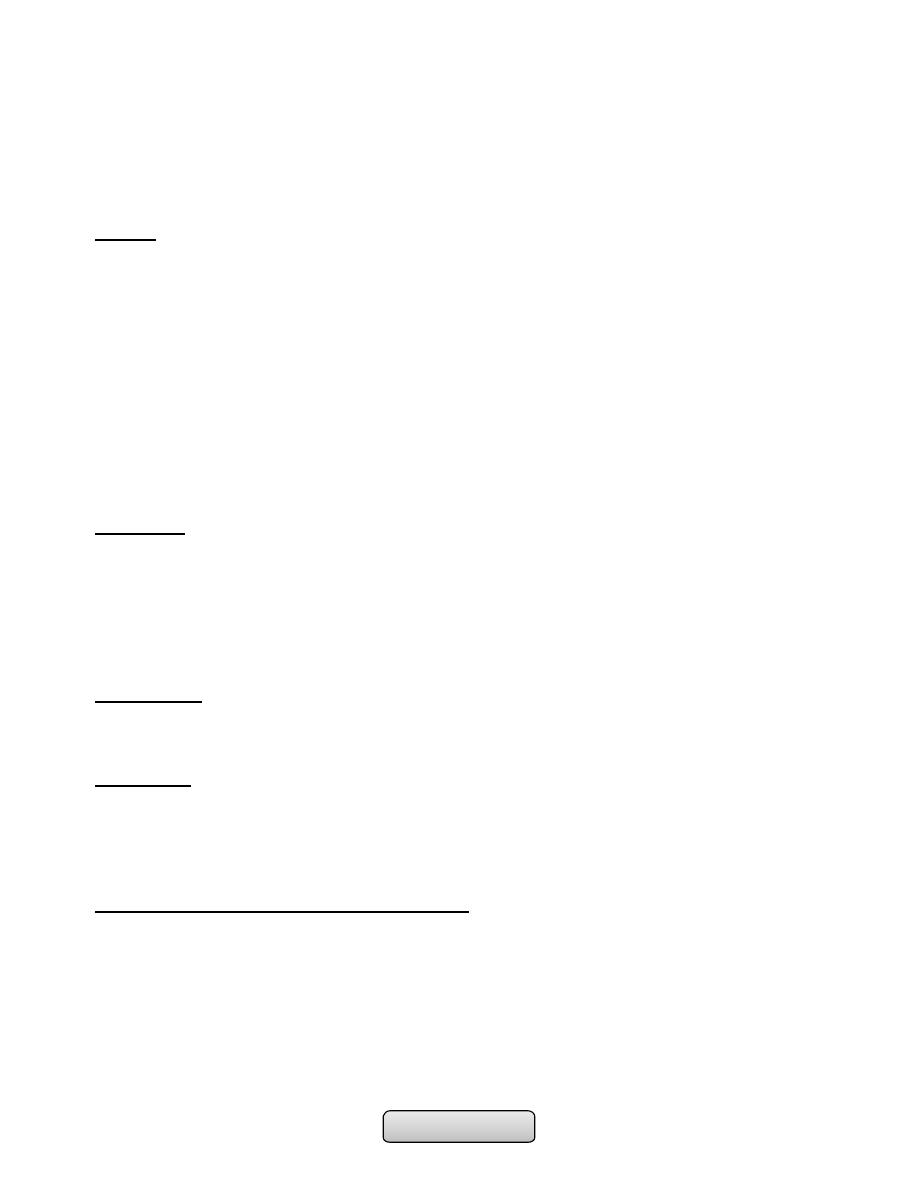
Internal Medicine: 4
th
Stage TUCOM Dr.Hassan
-
If still dehydrated, continue 0.9% saline and add 5% dextrose 1 litre per 12 hrs
• Typical requirement is 6 litres in first 24 hrs but avoid fluid overload in elderly
patients
• Subsequent fluid requirement should be based on clinical response including urine
output
Insulin:
• 50 units soluble insulin in 50 ml 0.9% saline i.v. via infusion pump
-
6 units/hr initially
-
3 units/hr when blood glucose is < 15 mmol/l (270 mg/dl)
-
2 units/hr if blood glucose declines to < 10 mmol/l (180 mg/dl)
• Intramuscular injection (loading dose of 10-20 U followed by 5 U hourly) If an I V
infusion is not possible. Or, alternatively, a fast-acting insulin analogue can be given
hourly by subcutaneous injection.
• Check blood glucose hourly initially, if no reduction in first hour, rate of insulin
infusion should be increased
• Aim for fall in blood glucose of 3-6 mmol/l (~55-110 mg/dl) per hour. If blood glucose
does not fall within 1 hour of commencing treatment, the dose of insulin should be
increased until a satisfactory response is obtained.
Potassium:
• None in first litre of i.v fluid unless < 3.0 mmol/l
• If plasma potassium < 3.5 mmol/l, give 40 mmol added potassium
-
Give in 1 litre of fluid
-
Avoid infusion rate of > 20 mmol/hr
• If plasma potassium is 3.5- 5.0 mmol/l, give 20 mmol added potassium
• If plasma potassium is > 5.0 mmol/l, or patient is anuric, give no added potassium
Bicarbonate:
• Its use is controversial. It can be used in severely acidotic patient (pH < 7.0) .
• Complete correction of the acidosis should not be attempted.
Antibiotics:
• Infections must be carefully sought and vigorously treated since it may not be possible
to abolish ketosis until they are controlled.
COMPLICATIONS OF DIABETIC KETOACIDOSIS:
1.
Cerebral oedema; may be caused by very rapid reduction of blood glucose, use of
hypotonic fluids and/or bicarbonate.
• High mortality.
• Treat with mannitol, oxygen.
2.
Acute respiratory distress syndrome.
3.
Thromboembolism.
4.
Disseminated intravascular coagulation (rare).
5.
Acute circulatory failure
Page of
92
105
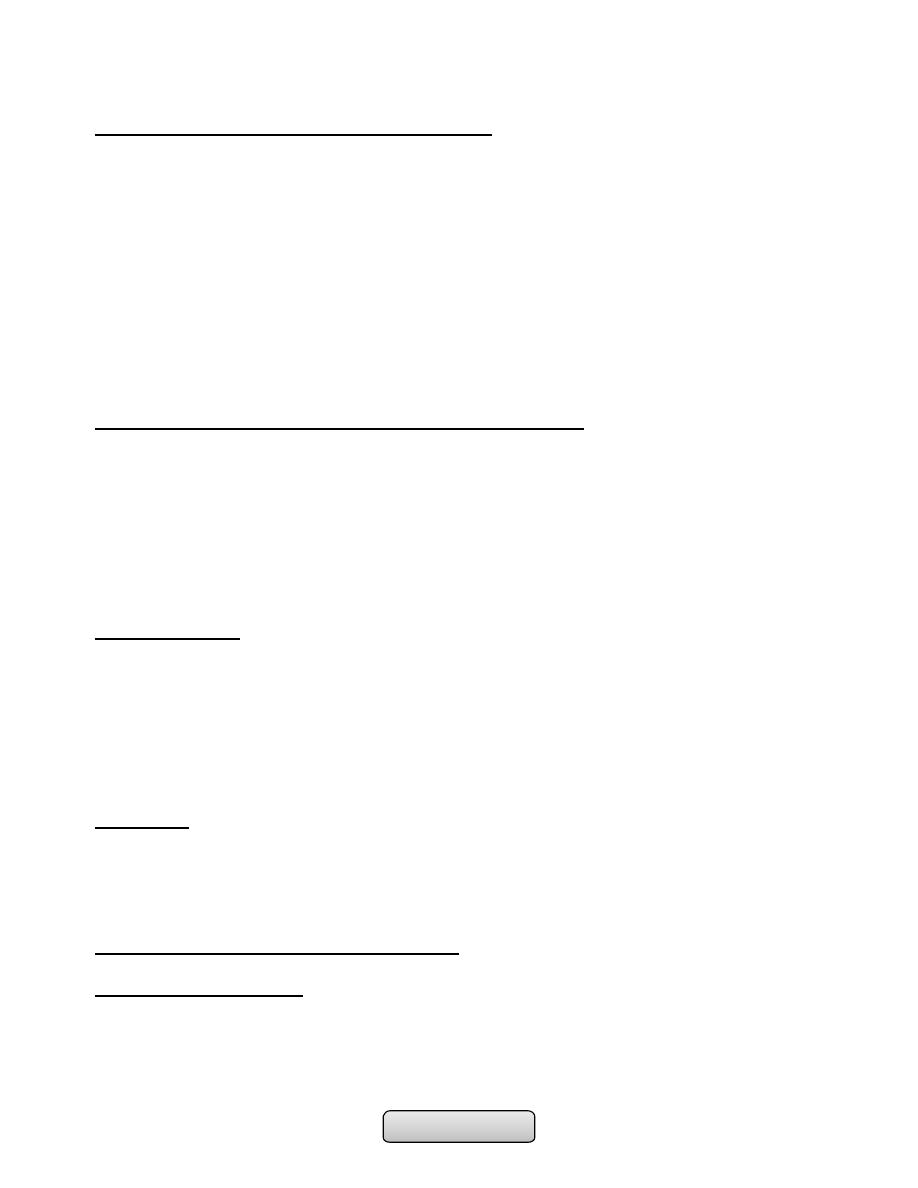
Internal Medicine: 4
th
Stage TUCOM Dr.Hassan
NON-KETOTIC HYPEROSMOLAR DIABETIC COMA:
• This condition is characterised by;
1.
Severe hyperglycaemia (> 50 mmol/l (900 mg/dl)).
2.
Without significant hyperketonaemia or acidosis.
3.
Severe dehydration and pre-renal azotemia are common.
4.
hyperosmolality (>350 mosmol/L)
• Plasma osmolality = 2 (Na+) + 2 (K+) + Glucose + Urea (all in mmol/L). The normal
value is 280-300 mmol/L
• It usually affects elderly patients, with type 2 DM, with a several-week history of
polyuria, weight loss, and diminished oral intake that lead to confusion, lethargy, or
coma. Physical examination reflects profound dehydration, hypotension, tachycardia,
and altered mental status.
• Mortality is high (40%).
Treatment differs from ketoacidosis in two main respects;
• Firstly, these patients are usually relatively sensitive to insulin and approximately half
the dose of insulin recommended for the treatment of ketoacidosis should usually be
employed (3 units/hr).
• Secondly, the plasma osmolality is high, which may be depressed conscious level if it
(> 340 mmol/kg). The patient should be given 0.45% saline until the osmolality
approaches normal, when isotonic (0.9%) saline should be substituted.
• Thromboembolic complications are common, and prophylactic subcutaneous low
molecular weight heparin is recommended.
LACTIC ACIDOSIS:
• In coma due to lactic acidosis the patient is likely to be taking metformin for type 2
diabetes.
• patient is very ill and overbreathing but not as profoundly dehydrated.
• The patient's breath does not smell of acetone, ketonuria is absent and the plasma
bicarbonate and pH are markedly reduced (pH < 7.2).
• The diagnosis is confirmed by a high (usually > 5.0 mmol/l) concentration of lactic
acid in the blood
Treatment:
• Intravenous sodium bicarbonate sufficient to raise the arterial pH to above 7.2, along
with insulin and glucose.
• Sodium dichloroacetate may be given to lower blood lactate.
• The mortality in this condition is > 50%.
MICROVASCULAR CHRONIC COMPLICATIONS:
DIABETIC NEPHROPATHY;
• Is an important cause of morbidity and mortality, and is now among the most common
causes of end-stage renal failure (ESRF) in developed countries.
• About 20 to 30% of diabetic patients develop nephropathy, and the incidence
increases with duration of diabetes.
Page of
93
105
Internal Medicine: 4
th
Stage TUCOM Dr.Hassan
• Microalbuminuria; (30 to 300 mg/24 hours) is an important indicator of risk of
developing diabetic nephropathy after 10 years of type 1 diabetes and it increase the
risk of macrovascular disease in patients with type 2 diabetes.
Pathologically:
• There is thickening of the glomerular basement membrane and glomerulosclerosis
which either difusse or nodular (Kimmelstiel–Wilson nodule) which is pathognomonic
of diabetic nephropathy.
Risk factors for developing diabetic nephropathy:
• Poor control of blood glucose.
• Long duration of diabetes.
• Presence of other microvascular complications.
• Ethnicity (e.g. Asian races, Pima Indians).
• Pre-existing hypertension.
• Family history of diabetic nephropathy.
• Family history of hypertension
Management:
• Improved control of blood glucose:
-
Treatment with metformin should be stopped when creatinine is higher than 150
µmol/l (1.7 mg/dl) as the risk of lactic acidosis is increased. Long-acting
sulphonylureas should be replaced by short-acting agents to decrease risk of
hypoglycemia.
• Improved control of blood glucose:
-
Treatment with metformin should be stopped when creatinine is higher than 150
µmol/l (1.7 mg/dl) as the risk of lactic acidosis is increased. Long-acting
sulphonylureas should be replaced by short-acting agents to decrease risk of
hypoglycemia.
• Aggressive reduction of blood pressure:
-
Institution of angiotensin-converting enzyme inhibitor (ACE-I) therapy.
-
ACE inhibitor treatment reduced the progression to established proteinuria
regardless of whether blood pressure was elevated or not.
-
Similar benefits from angiotensin II receptor antagonists in patients with type 2
diabetes.
-
Non-dihydropyridine calcium antagonists (diltiazem, verapamil) may be suitable
alternatives when ACE inhibitor is contraindicated.
• Aggressive cardiovascular risk factor reduction; with use of ACE inhibitors, statins and
aspirin.
• Renal replacement therapy may benefit diabetic patients at an earlier stage than
other patients with ESRF.
• Renal transplantation can dramatically improve the life of many.
DIABETIC RETINOPATHY:
• Diabetic retinopathy is one of the most common causes of blindness in adults between
30 and 65 years of age in developed countries.
Page of
94
105
Internal Medicine: 4
th
Stage TUCOM Dr.Hassan
• Pathogenesis; Hyperglycaemia leads to endothelial cell proliferation, resulting in
capillary closure and retinal ischemia, that leads to production of vascular endothelial
growth factor (VEGF), which stimulate endothelial cell growth (causing new vessel
formation).
Types of diabetic retinopathy:
1.
Non-proliferative 'background' retinopathy:
• Venous dilatation.
• Peripheral:
-
Microaneurysms (dots).
-
Haemorrhages (Blots).
-
Exudate.
2.
Pre-proliferative retinopathy:
• Clusters/sheets of microaneurysms and small blot haemorrhages and/or large retinal
haemorrhages.
• Multiple cotton wool spots.
• Macular oedema with perimacular exudates.
3.
Proliferative retinopathy:
• Pre-retinal haemorrhage.
• Neovascularisation.
• Fibrosis.
• Exudative maculopathy
Treatment:
• Good glycaemic and blood pressure control.
• Regular screening for retinopathy is essential in all diabetic patients.
• Photocoagulation is used: to destroy areas of retinal ischaemia (since it is thought
that this plays a major role in the development of neovascularisation) , to seal leaking
microaneurysms and to gliose new vessels directly on the retinal surface.
DIABETIC NEUROPATHY:
• This is a relatively early and common complication affecting approximately 30% of
diabetic patients.
CLASSIFICATION OF DIABETIC NEUROPATHY:
A.
Somatic:
1.
Polyneuropathy:
a)
Symmetrical, mainly sensory and distal.
b)
Asymmetrical, mainly motor and proximal (including amyotrophy).
2.
Mononeuropathy (including mononeuritis multiplex)l
B.
Visceral (autonomic):
1.
Cardiovascular.
2.
Gastrointestinal.
3.
Genitourinary.
4.
Sudomotor.
5.
Vasomotor.
6.
Pupillary.
..............................................................................................................
Page of
95
105
Internal Medicine: 4
th
Stage TUCOM Dr.Hassan
ADRENAL GLANDS DISEASES
Functional anatomy and physiology:
• The adrenal glands lie at the superior pole of each kidney. Each adrenal gland weighs
approximately of 4-5 g.
• Composed of two distinct regions: the cortex and the medulla.
1. Adrenal cortex: represents 90% of adrenal gland, consists of three anatomic zones:
-
Outer zona glomerulosa, which secretes the mineralocorticoid aldosterone.
-
Intermediate zona fasciculata, which secretes cortisol.
-
Inner zona reticularis, which secretes adrenal androgens.
2. Adrenal medulla; represents 10% of adrenal gland, its the center of the adrenal
gland, which secrets catecholamines: epinephrine, norepinephrine and dopamine
in response to stress and activation of sympathetic nervous system.
• The synthesis of all steroid hormones begins with cholesterol and is catalyzed by a
series of regulated, enzyme-mediated reactions.
Adrenal gland is under control of:
1. Hypothalamic-pituitary-adrenal (HPA) axis; regulate cortisol and androgen
production.
2. Renin-angiotensin-aldosterone (RAA) system.
Glucocorticoids:
• Cortisol is the major glucocorticoid in humans.
• Highest in the morning and lowest in the middle of the night.
• Increase in state of stress, including any illness.
• Affect metabolism, cardiovascular function, behavior, and the inflammatory/immune
response.
• Its secretion is stimulated by (ACTH).
• Cortisol can also activate mineralocorticoid receptors, but it normally inhibited by
11β-HSD2.
Mineralocorticoids:
• Aldosterone is the body's most important sodium-retaining hormone.
• Under influence of renin-angiotensin-aldosterone system.
• Renin secretion from the juxtaglomerular apparatus in the kidney is stimulated by low
perfusion pressure in the afferent arteriole, low sodium concentrations at the macula
densa, or increased sympathetic nerve activity.
Adrenal androgens:
❖
Are secreted in response to ACTH
❖
Initiation of puberty (the adrenarche).
❖
Excess adrenal androgen secretion results in acne, hirsutism, and virilization.
Page of
96
105
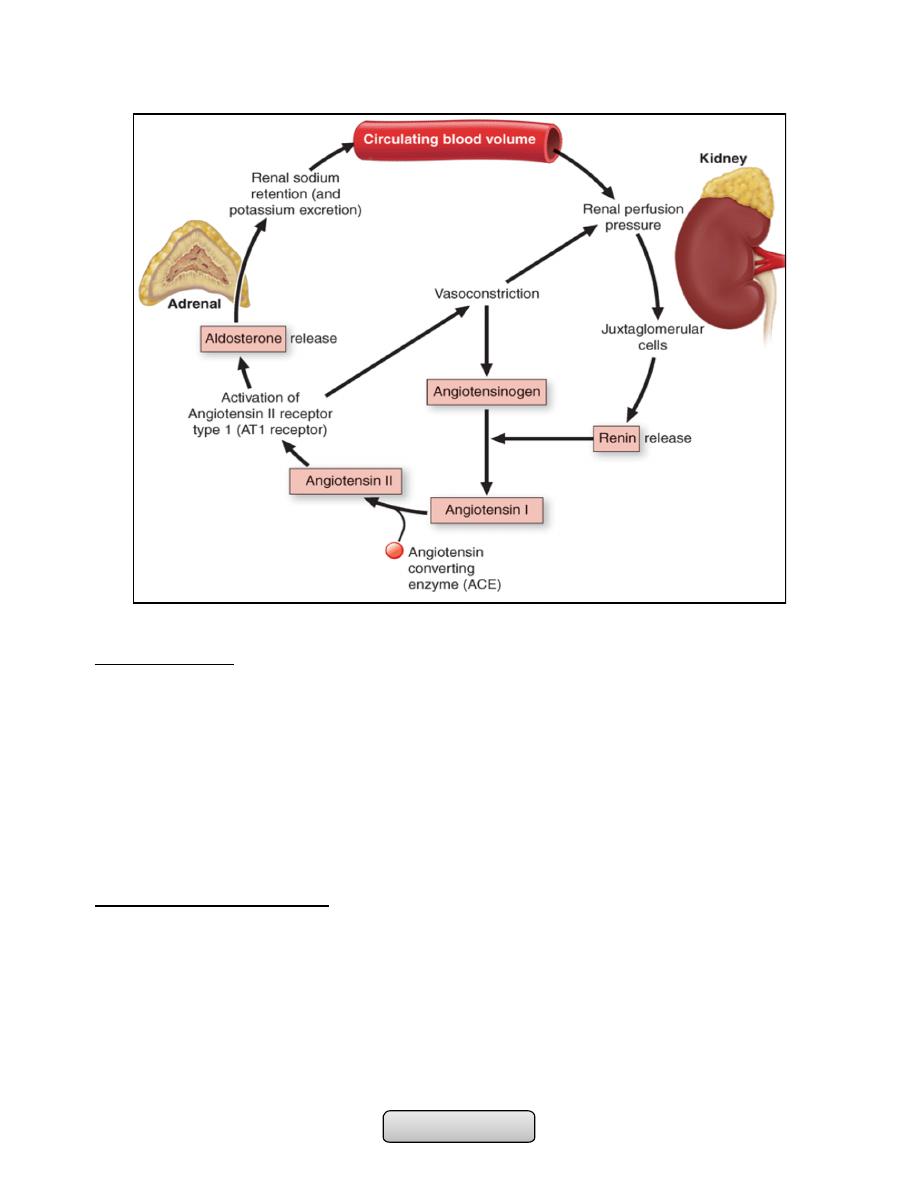
Internal Medicine: 4
th
Stage TUCOM Dr.Hassan
Catecholamines:
• Are produced mainly by the chromaffin cells of the adrenal medulla and the
sympathetic nervous fibers.
• Which includes noradrenaline (norepinephrine), adrenaline (epinephrine) and
dopamine.
• Prepare the body for physical activity (fight or flight response). Some typical effects
are increases in heart rate, blood pressure, blood glucose, and sympathetic
activation.
• No clinical consequences attributable to deficiency of circulating catecholamines.
Disorders of adrenal glands:
1. Cushing's syndrome.
2. Adrenal insufficiency.
3. Other adrenal disease including;
-
Congenital adrenal hyperplasia.
-
Primary hyperaldosteronism.
-
Phaeochromocytoma.
Page of
97
105
Internal Medicine: 4
th
Stage TUCOM Dr.Hassan
Cushing's syndrome:
• Cushing's syndrome is a syndrome that reflects excessive tissue exposure to cortisol.
• Most common cause is iatrogenic; prolonged administration of synthetic
glucocorticoids
• Non-iatrogenic Cushing's syndrome is rare
• Cushing's disease and adrenal tumour are four times more common in women
• Ectopic ACTH syndrome is more common in men
Aetiology:
1. ACTH-dependent:
1) Pituitary adenoma secret ACTH (Cushing's disease).
2) Ectopic ACTH syndrome (e.g. bronchial carcinoid, small-cell lung carcinoma,
pancreatic neuro-endocrine tumour).
3) latrogenic (ACTH therapy).
2. Non-ACTH-dependent:
1) Iatrogenic (chronic glucocorticoid therapy for asthma) .
2) Adrenal adenoma.
3) Adrenal carcinoma
Clinical Manifestations:
• Fat redistribution (dorsocervical and supraclavicular fat pads, centripetal obesity,
weight gain) (95%).
• Menstrual irregularities (80% of affected women).
• Thin skin/plethora (80%).
• Moon facies (75%).
• Increased appetite (75%).
• Hypertension (75%).
• Altered mentation (poor concentration, decreased memory, euphoria) (70%)
• Diabetes mellitus/glucose intolerance (65%), Striae (65%), Hirsutism (65%), Proximal
muscle weakness (60%), Psychological disturbances (emotional lability, depression,
mania, psychosis) (50%), Decreased libido/impotence (50%).
• Acne (45%), Osteoporosis/pathologic fractures (40%), Virilization (in women) (40%),
Easy bruisability (40%), Poor wound healing (40%), Edema (20%), Increased infections
(10%) and Cataracts (5%).
Ectopic ACTH syndrome:
• Very high ACTH level (no negative feedback) is associated with marked pigmentation.
• Very high cortisol levels overcome the barrier of 11β-HSD2 in the kidney and cause
hypokalemic alkalosis that leads to myopathy and hyperglycemia (by inhibiting insulin
secretion).
• The onset is usually rapid and may be associated with cachexia.
Page of
98
105
Internal Medicine: 4
th
Stage TUCOM Dr.Hassan
INVESTIGATIONS:
• Whether the patient has Cushing's syndrome, and to elucidate the aetiology.
• There is no place for a random measurement of daytime plasma cortisol.
I. Does the patient have Cushing's syndrome?
A. Urine free cortisol;
1. 24-hr timed collection, normal range depends on assay:
a) 50 µg/24 hours --- normal.
b) 100 and 500 µg/24 hours --- Cushing's disease.
2. greater than 500 µg/24 hours --- ectopic ACTH syndrome and cortisol-secreting
adrenal adenomas or carcinomas.
B. Diurnal rhythm of plasma cortisol; the plasma concentration is highest in the early
morning (between 6:00 and 8:00 am)= 8- 25 µg/dL and lowest around midnight=
less than 5 µg/dL.
C. Overnight dexamethasone suppression test (suspected Cushing's syndrome); 1 mg
orally at midnight; measure plasma cortisol at 0800-0900 hrs. Plasma cortisol < 60
nmol/l (< 2.2 µg/dl) excludes Cushing's.
D. Low-dose dexamethasone suppression test (to confirm Cushing's syndrome); 0.5
mg 6-hourly for 48 hrs; sample 24-hr urine cortisol during second day and 0900-hr
plasma cortisol after 48 hrs:
1. Urine cortisol < 100 nmol/day (36 µg/day) or plasma cortisol < 60 nmol/l (< 2.2
µg/dl) excludes Cushing's.
E. Insulin tolerance test; Peak plasma cortisol > 120% of baseline excludes Cushing's.
II. What is the cause of the Cushing's syndrome?
A. Basal ACTH levels; are normal or elevated in Cushing's disease and the ectopic
ACTH syndrome and are suppressed in adrenal Cushing's syndrome.
B. High-dose dexamethasone suppression test; 2 mg 6-hourly for 48 hrs; sample 24-hr
urine cortisol at baseline and during second day:
1. Urine cortisol < 50% of basal suggests pituitary-dependent disease.
2. > 50% of basal suggests ectopic ACTH syndrome.
C. Corticotrophin-releasing hormone test; 100 µg ovine CRH i.v. and monitor plasma
ACTH and cortisol for 2 hrs Peak plasma cortisol > 120% and/or ACTH > 150% of
basal values suggests pituitary-dependent disease; lesser responses suggest ectopic
ACTH syndrome.
D. Inferior petrosal sinus sampling; Catheters placed in both inferior petrosal sinuses
and simultaneous sampling from these and peripheral blood for ACTH.
1. > 200% compared to peripheral ACTH, suggests pituitary-dependent disease.
2. < 150% suggests ectopic ACTH syndrome.
3. The test is usually performed by vascular radiologists on an outpatient basis.
With local anesthesia, femoral catheters are advanced bilaterally up to the
inferior petrosal sinuses. After confirmation of catheter location by
fluoroscopy, several ACTH samples are drawn simultaneously from the right and
Page of
99
105
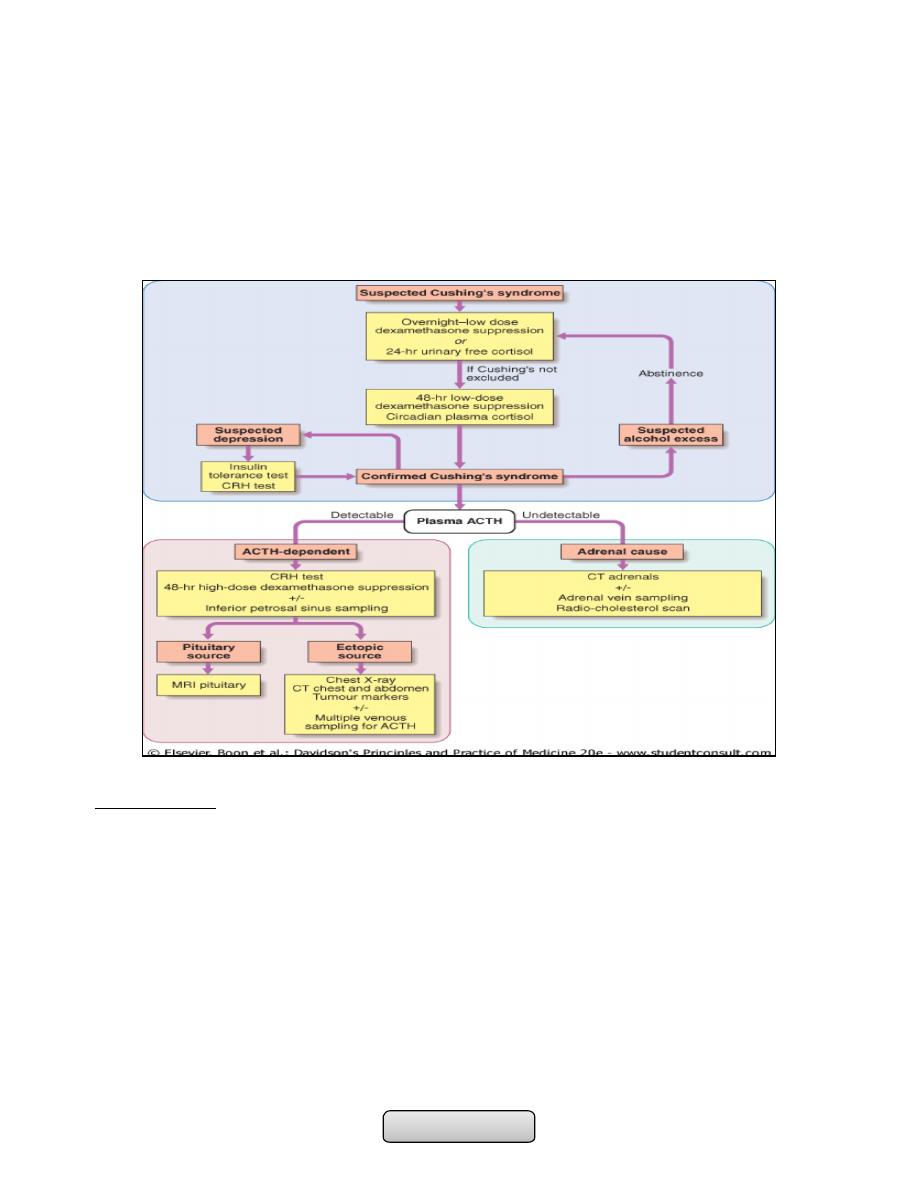
Internal Medicine: 4
th
Stage TUCOM Dr.Hassan
left at the same time that a peripheral level is being drawn from an arm vein.
CRH can also be injected to provoke ACTH release. Samples are then assayed
for ACTH, and the pituitary-to-peripheral ratios are calculated.
E. Imaging:
1. Pituitary gland MRI with gadolinium for localizing a pituitary microadenomas.
2. CT or MRI detects adrenal adenomas or carcinomas.
3. CXR ,CT chest or abdomen.
MANAGEMENT:
1. Medical therapy; given for a few weeks prior to operation. (inhibit corticosteroid
biosynthesis) including metyrapone, aminoglutethimide and ketoconazole.
2. Cushing's disease; Trans-sphenoidal surgery with selective removal of the adenoma is
the treatment of choice. Nelson's syndrome (bilateral adrenalectomy in cushing's
disease) that leads to pituitary macroadenoma and very high ACTH levels causing
pigmentation. Nelson's syndrome can be prevented by pituitary irradiation.
3. Adrenal tumours;
1. Adenomas: are removed surgically.
2. Carcinomas are resected if possible + tumour bed irradiated + adrenolytic drug
mitotane.
3. Metastases; cytotoxic chemotherapy.
Page
of
100
105
Internal Medicine: 4
th
Stage TUCOM Dr.Hassan
4. Ectopic ACTH syndrome;
1. Localized tumours causing this syndrome (e.g. bronchial carcinoid) should be
removed.
2. Non-resectable malignancies, using medical therapy.
Adrenal insufficiency:
• Adrenal insufficiency results from inadequate secretion of cortisol and/or
aldosterone.
• A high index of suspicion is therefore required in patients with unexplained fatigue,
hyponatraemia or hypotension.
Aetiology;
• The most common cause is due to an ACTH deficiency (i.e. secondary adrenocortical
failure), usually because of inappropriate withdrawal of chronic glucocorticoid
therapy.
Secondary (↓ACTH);
• Withdrawal of suppressive glucocorticoid therapy:
• Hypothalamic or pituitary disease
Primary (↑ACTH); usually describe as Addison's disease:
Common causes;
• Autoimmune;
-
Sporadic
-
Polyglandular syndromes
• Tuberculosis
• HIV/AIDS
• Metastatic carcinoma
• Bilateral adrenalectomy
Rare causes;
• Lymphoma
• Intra-adrenal haemorrhage (Waterhouse-Friedrichsen syndrome following
meningococcal septicaemia)
• Amyloidosis
• Haemochromatosis
Corticosteroid biosynthetic enzyme defects;
• Congenital adrenal hyperplasias
• Drugs: Aminoglutethimide, metyrapone, ketoconazole, etomidate etc.
Page
of
101
105
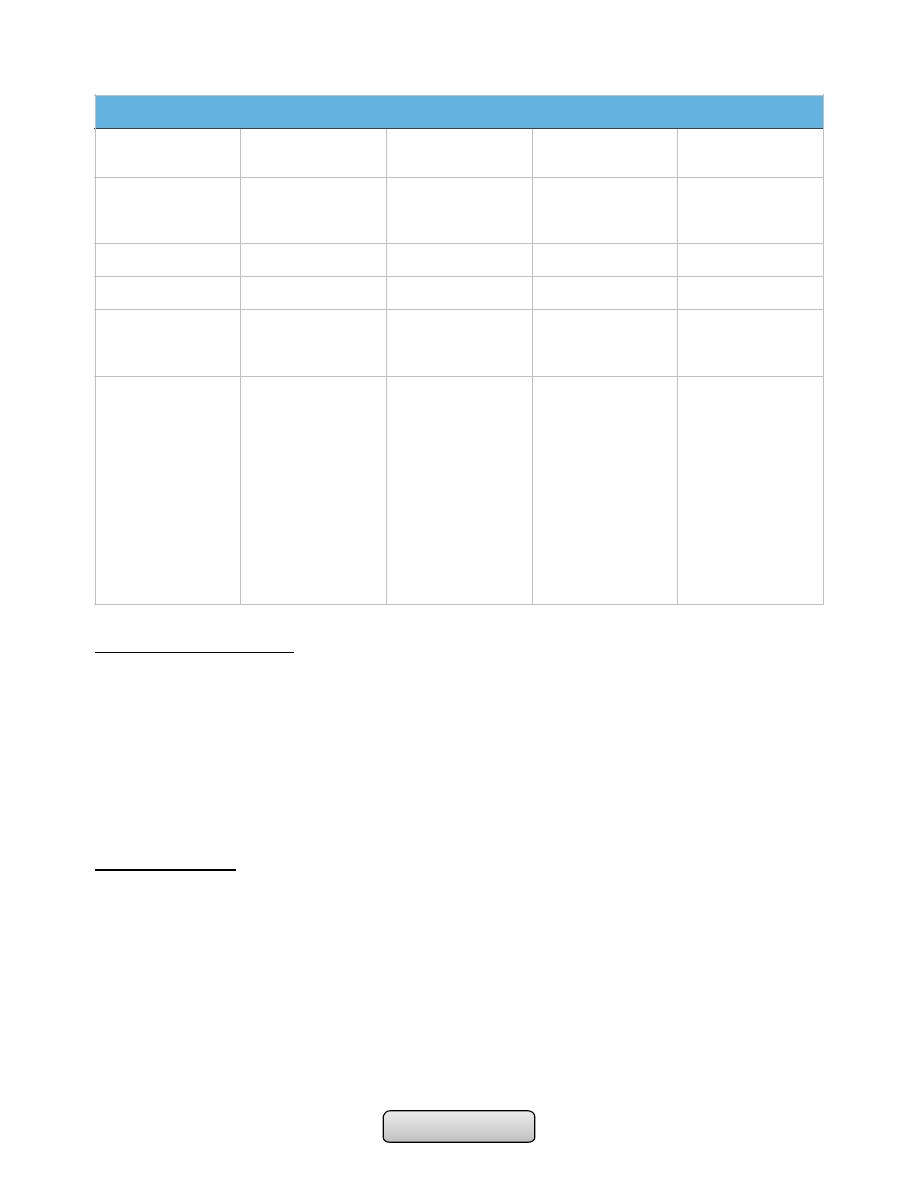
Internal Medicine: 4
th
Stage TUCOM Dr.Hassan
ACUTE ADRENAL CRISIS:
• Circulatory shock with severe hypotension
• Hyponatraemia, hyperkalaemia and, in some instances, hypoglycaemia and
hypercalcaemia.
• Muscle cramps, nausea, vomiting, diarrhoea and unexplained fever may be present.
• The crisis is often precipitated by intercurrent disease, surgery or infection.
• Treatment should not be delayed pending results of investigations.
INVESTIGATIONS:
A. Assessment of glucocorticoids;
1. Random plasma cortisol is usually low in patients with adrenal insufficiency, but
it may be within the normal range yet inappropriately low for a seriously ill
patient.
2. ACTH stimulation test;
a) Diagnosis of primary or secondary adrenal insufficiency.
b) Assessment of hypothalamic-pituitary-adrenal axis in patients taking
suppressive glucocorticoid therapy:
c) Dose; 250 µg ACTH (Synacthen) by I.M. injection at any time of day.
Clinical features of adrenal insufficiency
Glucocorticoid
insufficiency
Mineralocorticoid
insufficiency
ACTH excess
Adren androgen
insufficiency
Withdrawal of
exogenous
glucocorticoid
+
-
-
+
Hypopituitarism
+
-
-
+
Addison's disease
+
+
+
+
Congenit adrenal
hyperplasia (21
OHase deficiency)
+
+
+
-
Clinical features
Weight loss Malaise
Weakness Anorexia
Nausea Vomiting
diarrhoea or
constipation
Postural
hypotension
Shock
Hypoglycaemia
Hyponatraemia
(dilutional)
Hypercalcaemia
Hypotension
Shock
Hyponatraemia
(depletional)
Hyperkalaemia
Pigmentation
Sun-exposed areas
Pressure areas,
e.g. elbows, knees
Palmar creases,
knuckles
Mucous
membranes
Conjunctivae
Recent scars
Decreased body
hair and loss of
libido, especially in
female
Page
of
102
105
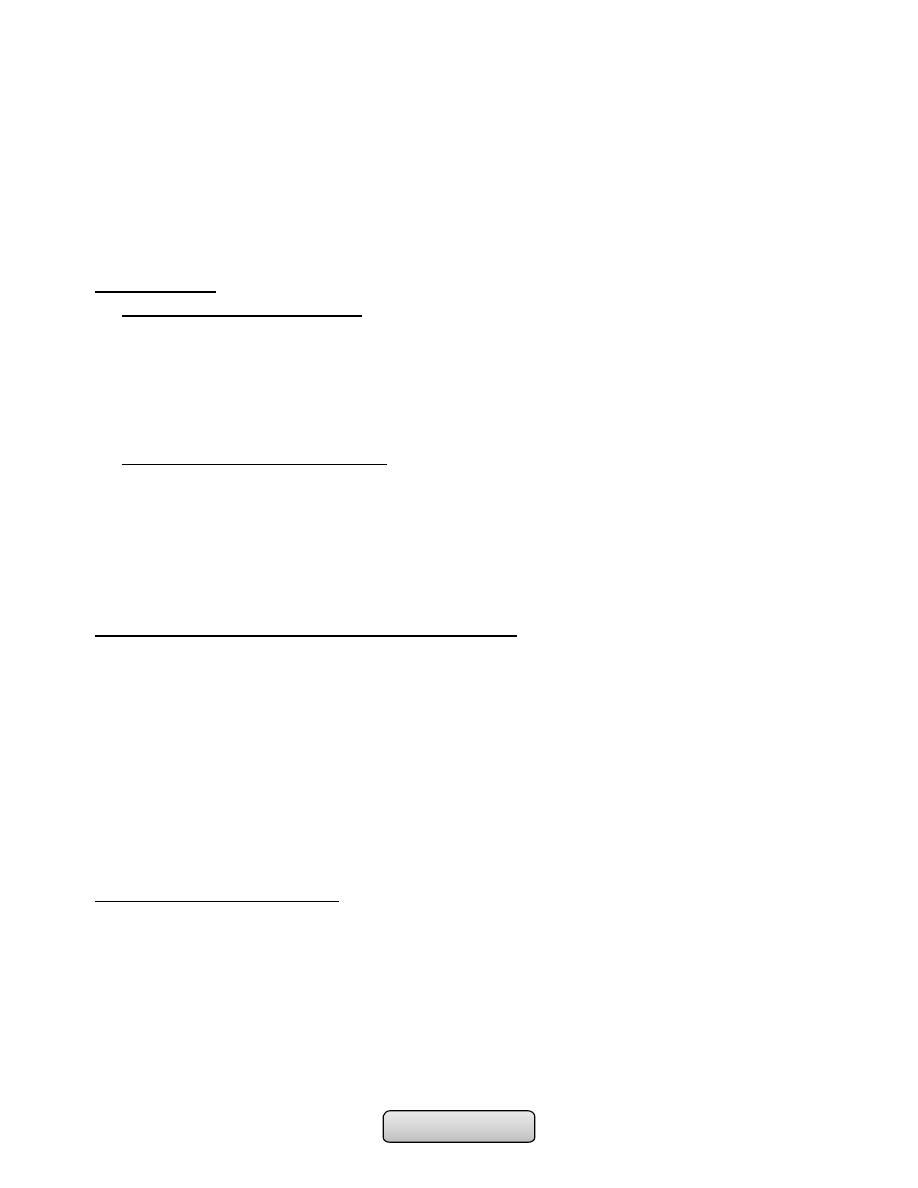
Internal Medicine: 4
th
Stage TUCOM Dr.Hassan
d) 0 and 30 minutes for plasma cortisol.
e) Normal subjects plasma cortisol > 460 nmol/l ( 170 µg/dl) either at baseline
or at 30 minutes.
B. Assessment of mineralocorticoids;
1. Plasma renin activity is high, with plasma aldosterone is low. Hyponatraemia
and Hyperkalaemia.
MANAGEMENT:
1. Glucocorticoid replacement;
• Cortisol (hydrocortisone) is the drug of choice, given by mouth, 15 mg on waking and
5 mg at ~1800 hrs.
• An adrenal crisis; intravenous hydrocortisone succinate 100 mg and intravenous fluid
(normal saline and 10% dextrose for hypoglycaemia).
• Parenteral hydrocortisone should be continued (100 mg I.M. 6-hourly) until
gastrointestinal symptoms abate before starting oral therapy.
2. Mineralocorticoid replacement;
• fludrocortisone from being metabolised by 11β-HSD2 and thereby confers a longer
half-life and access to mineralocorticoid receptors. The usual dose is 0.05-0.1 mg
daily.
• In adrenal crisis, however, rapid replacement of sodium deficiency is more
important than administration of fludrocortisone. Intravenous saline should be
infused as required to normalise haemodynamic indices
Advice to patients on glucocorticoid replacement:
1. Intercurrent stress; e.g. Febrile illness-double dose of hydrocortisone.
2. Surgery;
1. Minor operation; hydrocortisone 100 mg i.m. with pre-medication.
2. Major operation; hydrocortisone 100 mg 6-hourly for 24 hours, then 50 mg i.m.
6-hourly until ready to take tablets.
3. Vomiting; Must have parenteral hydrocortisone if unable to take by mouth.
4. Steroid card; Patient should carry this at all times give information regarding
diagnosis, steroid, dose and doctor.
5. Bracelet; Patients should be encouraged to buy one of these
Primary hyperaldosteronism:
• Hypertensive patients with hypokalaemia (including hypokalaemia induced by
thiazide diuretics), poor control of blood pressure with conventional therapy, or
presentation at a young age, or family history of early onset hypertension.
• Most patients with Primary hyperaldosteronism have Idiopathic bilateral adrenal
hyperplasia, while only minority have adrenal adenoma secreting aldosterone (Conn's
syndrome).
Page
of
103
105
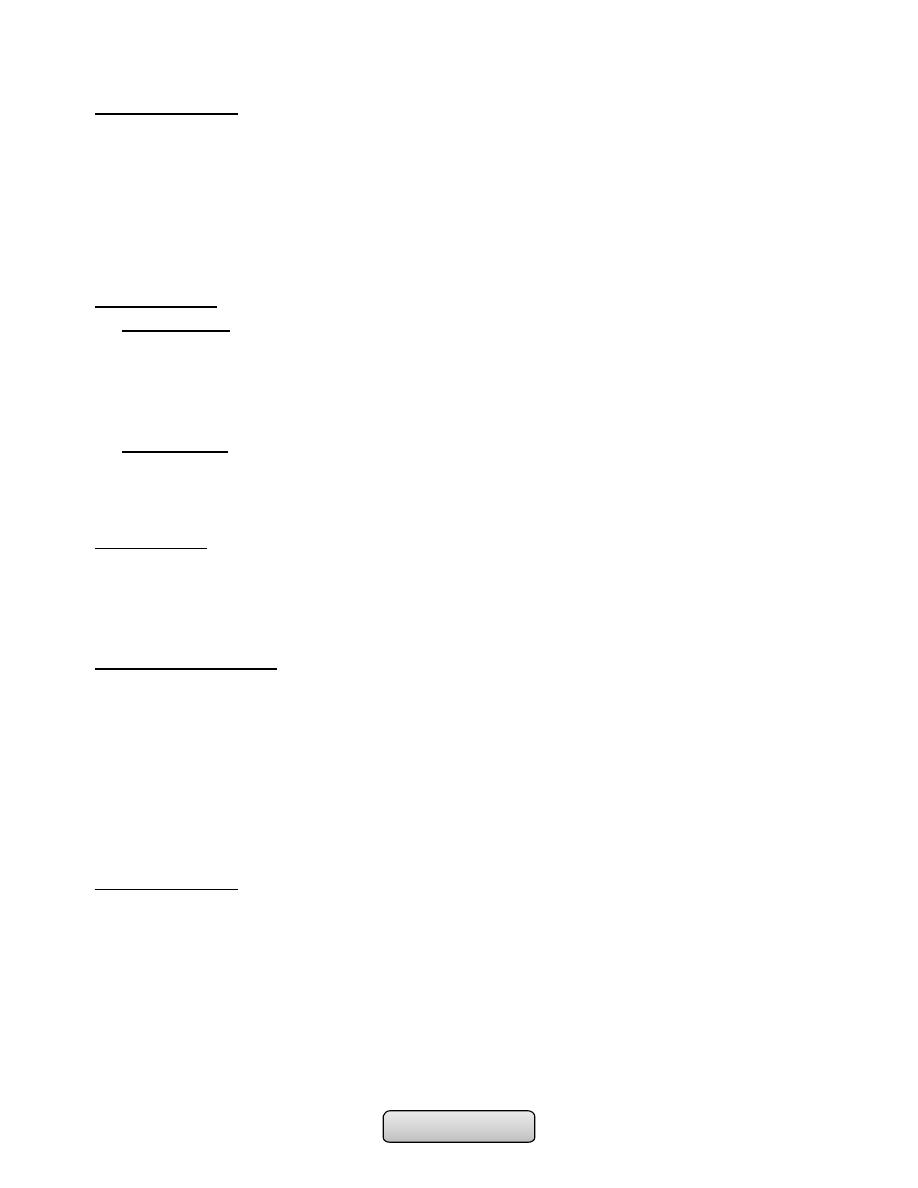
Internal Medicine: 4
th
Stage TUCOM Dr.Hassan
Clinical features:
• Asymptomatic.
• Sodium retention may cause oedema.
• Hypokalaemia causes muscle weakness (or even paralysis, especially in Chinese),
polyuria (secondary to renal tubular damage which produces nephrogenic diabetes
insipidus) and occasionally tetany (because of associated metabolic alkalosis and low
ionised calcium).
• B.P is elevated but accelareted phase is rare.
Investigations:
• Biochemical;
-
Hypokalaemia and elevated bicarbonate. Plasma sodium is usually in upper end of
normal range.
-
Measurements of plasma renin activity and aldosterone . renin is low and
aldosterone level is high.
• Localisation;
-
Abdominal CT: to localize the tumour.
-
Adrenal CT should only be performed when the biochemistry supports the diagnosis
of adrenal tumour.
Management:
• Idiopathic bilateral adrenal hyperplasia; Mineralocorticoid receptor antagonists
(spironolactone or eplerenone) or potassium sparing diuretics are used.
• Conn's adenoma; Medical therapy few weeks before unilateral adrenalectomy.
Phaeochromocytoma:
• This is a rare tumour of chromaffin tissue that secretes catecholamines and is
responsible for less than 0.1% of cases of hypertension.
• Rule of tens:
-
10% are malignant.
-
10% are extra-adrenal (i.e. elsewhere in the sympathetic chain).
-
10% are familial.
Clinical features:
These depend on the pattern of catecholamine secretion:
• Hypertension (usually paroxysmal; often postural drop of blood pressure).
• Paroxysms of:
-
Pallor (occasionally flushing)
-
Palpitations
-
Sweating
-
Headache
-
Anxiety (fear of death-angor animi)
Page
of
104
105
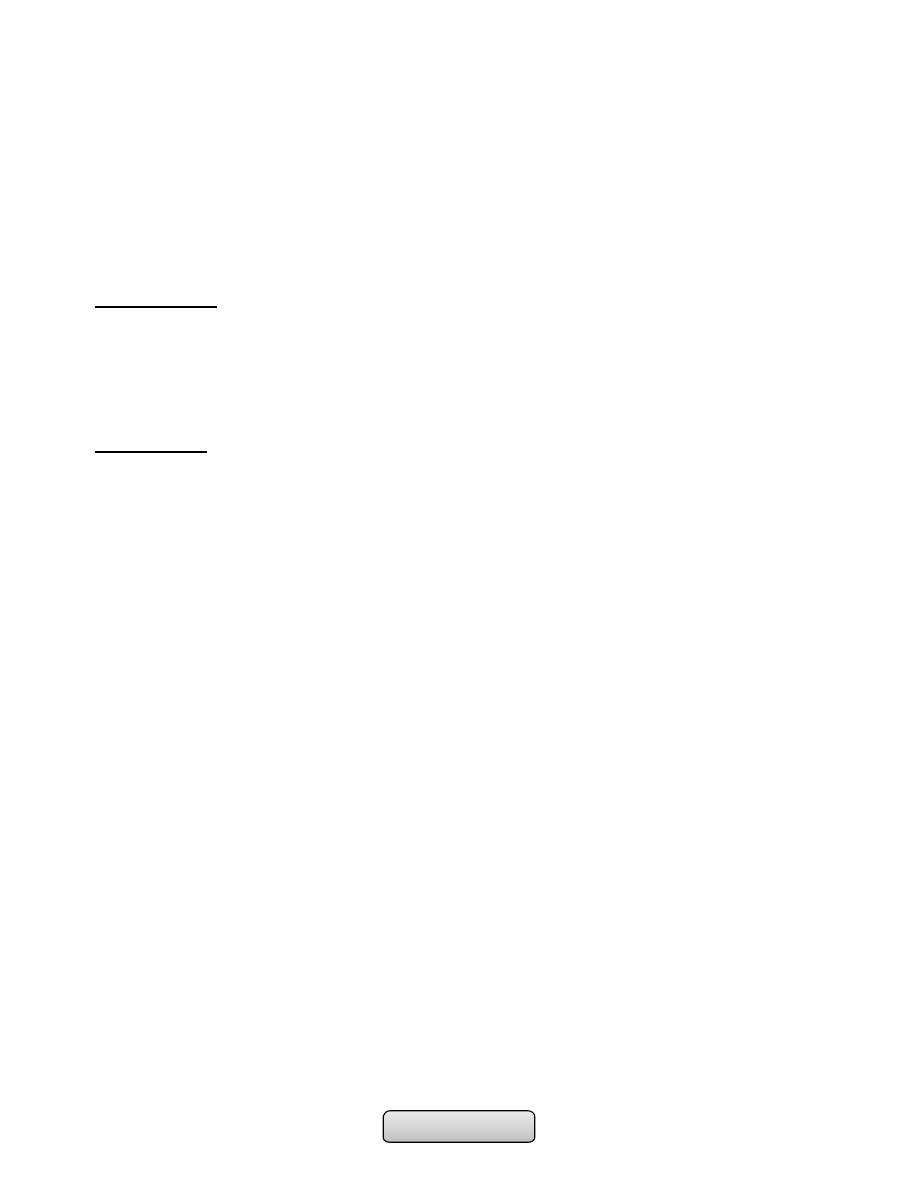
Internal Medicine: 4
th
Stage TUCOM Dr.Hassan
• Abdominal pain, vomiting.
• Constipation.
• Weight loss.
• Glucose intolerance.
• Complication of hypertension: e.g. stroke, myocardial infarction, left ventricular
failure, hypertensive retinopathy or accelerated-phase hypertension.
• Familial syndromes associated with phaeochromocytoma including neurofibromatosis,
Von Hippel-Lindau syndrome and MEN type 2.
Investigations:
• Biochemical; Measuring the hormones (adrenaline/epinephrine, noradrenaline/
norepinephrine and dopamine) in plasma or their metabolites (e.g. vanillyl-mandelic
acid (VMA), conjugated metanephrine and normetanephrine) in urine.
-
Samples should be collected during a period of attacks.
• Localisation; abdominal CT or MRI.
Management:
• Surgery is the curative treatment
• Patient should be prepared before surgery for at least 6 weeks with oral α-blocker
phenoxybenzamine and restoration of normal plasma volume.
• During surgery sodium nitroprusside and the short-acting α-antagonist phentolamine
are useful in controlling hypertensive episodes which may result from anaesthetic
induction or tumour mobilisation
• Post-operative hypotension may occur and require volume expansion and, very
occasionally, noradrenaline (norepinephrine) infusion.
•
Quiz
Q1- List the complications of GERD.
Q2- A 24 year old man with iron deficiency anemia, weight loss and chronic diarrhea
present to you complain from an itchy vesicular rash on his elbows. What is the diagnosis?
Q3- List the extraintestinal features of active ulcerative colitis.
Q4- A 50 year old male present with massive hematemesis and splenomegaly. What is the
diagnosis?
Q5- Which of the following tests most reliable distinguish active hepatitis B from carrier
state?
A-HBs Ag B-anti HBc Ab C-HBc Ag D-HBe Ag
Page
of
105
105
