1
Infant of diabetic mother (IDM)
• Women with diabetes mellitus during pregnancy (Type 1, Type 2, and gestational) are all at
increased risk for adverse pregnancy outcomes.
• Adequate glycemic control before and during pregnancy is crucial for improving outcome.
• Most infants born to diabetic mothers are large for gestational age.
• If the diabetes is complicated by vascular disease, infants may have growth restriction,
especially those born after 37 wk gestation.
• The neonatal mortality rate is over 5 times that of infants of non diabetic mothers
Problems of Infants of Diabetic Mothers
Birth trauma
Birth asphyxia
Hypoglycemia
Hypocalcemia
Hypomagnesemia
Hyperbilirubinemia
Surfactant deficiency, related respiratory distress syndrome (hyaline membrane disease)
Polycythemia
Renal vein thrombosis
Cardiac septal hypertrophy and cardiomyopathy
Congenital malformations
Diabetic mothers have a high incidence of;
polyhydramnios
preeclampsia
pyelonephritis
preterm labor
chronic hypertension
High fetal mortality rate at all gestational ages, especially after 32 wk
Pathophysiology
• Maternal hyperglycemia causes fetal hyperglycemia, and increased the fetal pancreatic
response leads to fetal hyperinsulinemia;
• Fetal hyperinsulinemia and hyperglycemia cause increased hepatic glucose uptake and
glycogen synthesis, accelerated lipogenesis, and protein synthesis .
• Related pathologic findings are hyperplasia of the pancreatic β islet cells, increased weight of
the placenta and infant organs, myocardial hypertrophy, except for the brain.
• Hyperinsulinism and hyperglycemia produce fetal acidosis, which may result in an increased
rate of stillbirth.
• Separation of the placenta at birth suddenly interrupts glucose infusion into the neonate
without a proportional effect on the hyperinsulinism, and hypoglycemia and poor lipolysis
develop during the 1
st
hr after birth.
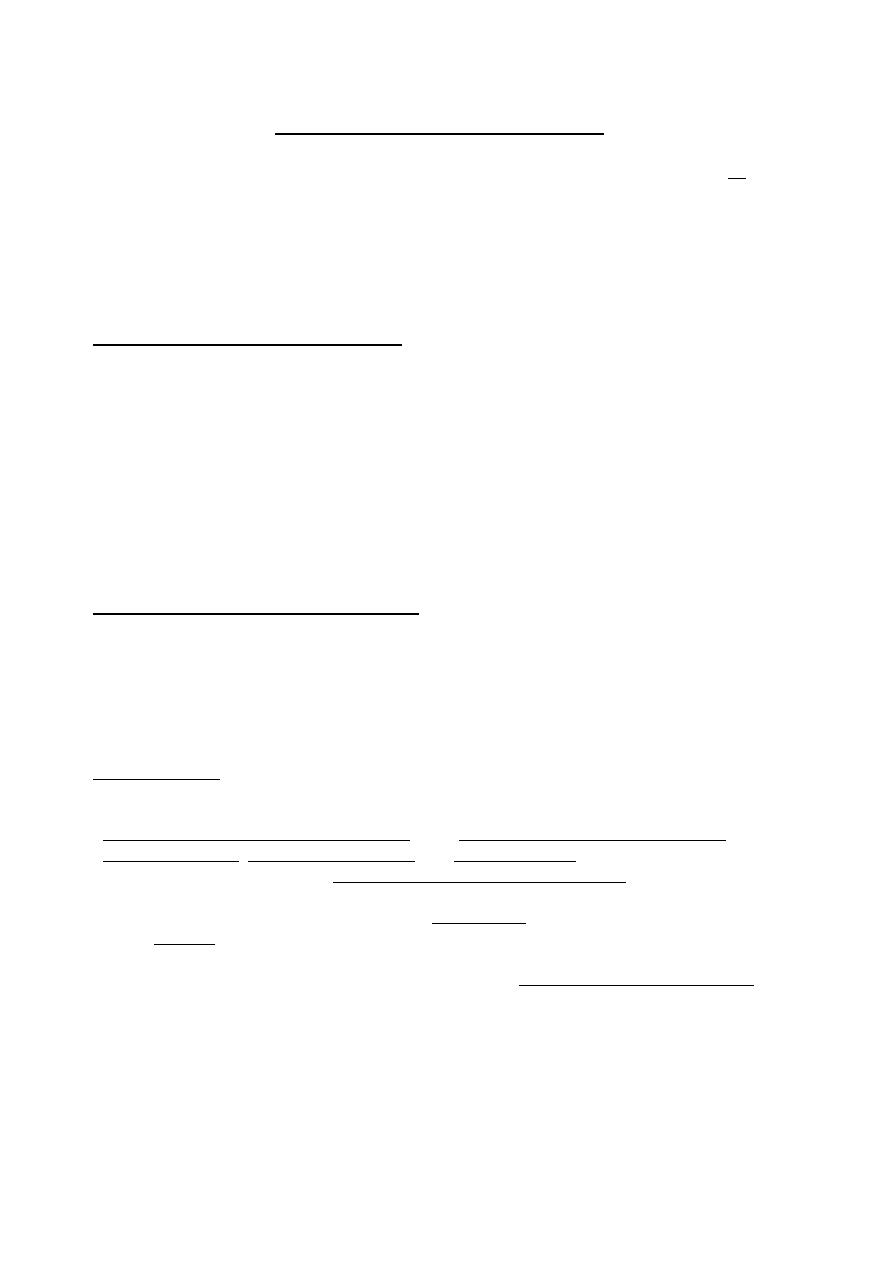
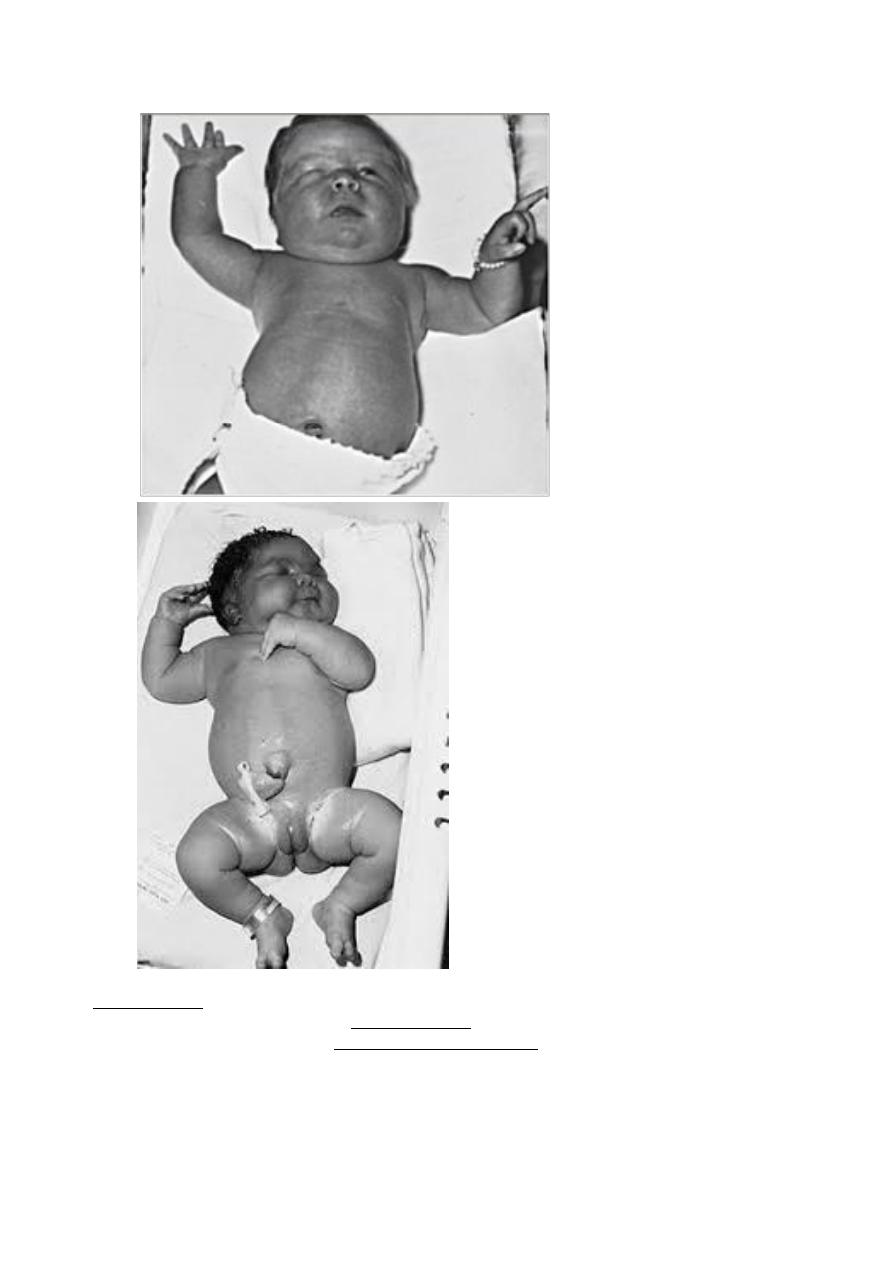
CLINICAL MANIFESTATIONS
• Infants tend to be large and plump as a result of increased body fat and big viscera.
• They have puffy, plethoric facies.
• These infants if delivered before term or the mother had associated vascular disease, then may
have normal or low birth-weight.
2
Hypoglycemia
• Develops in 25–50% of infants of diabetic mothers
• Occurs in 15–25% of infants of gestational diabetes mothers, and only small percentage of
these infants become symptomatic.
• The nadir in an infant's blood glucose concentration is usually reached between 1 - 3 hr after
birth; and spontaneous recovery may begin by 4–6 hr after birth.
• The infants tend to be jumpy, tremulous, and hyper-excitable during the 1
st
3 days of life,
although hypotonia, lethargy, and poor sucking may also occur.
3
Tachypnea
• Develops in many infants of diabetic mothers during the 1
st
2 days of life.
• Infants of diabetic mothers have a higher incidence of respiratory distress syndrome may be
related to the antagonistic effect of insulin on stimulation of surfactant synthesis by cortisol.
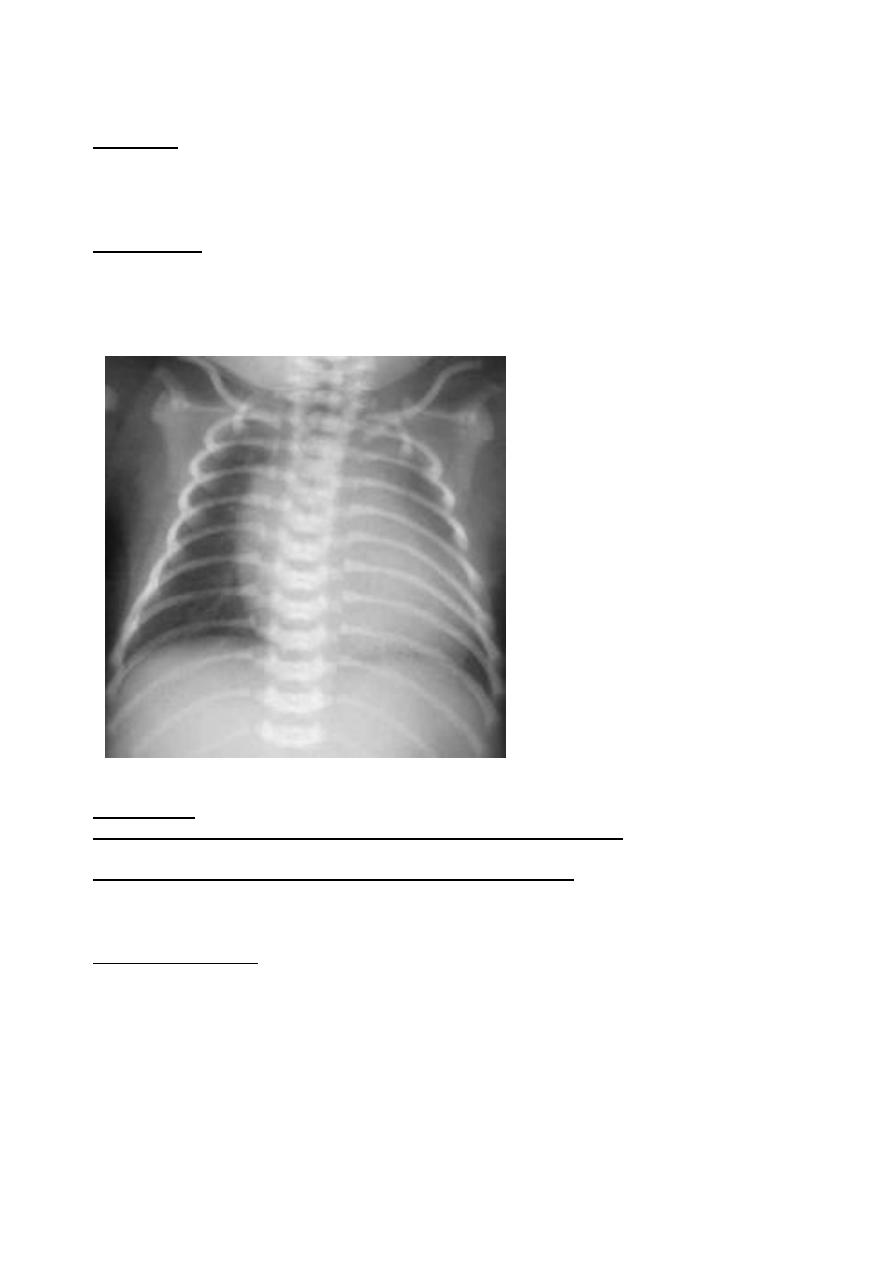
Cardiomegaly
• Cardiomegaly is common in 30% of IDM
• Heart failure occurs in 5–10% of infants of diabetic mothers.
• Congenital heart disease is more common in infants of diabetic mothers.
• Asymmetric septal hypertrophy may occur, and inotropic agents worsen the obstruction and so
are contraindicated.
Birth trauma is also a common sequel of fetal macrosomia.
Neurologic development and ossification centers tend to be immature and correlate with
brain size (which is not increased) and gestational age rather than total body weight.
Hyperbilirubinemia, polycythemia, and renal vein thrombosis; are increased, and the
incidence of the latter should be suspected in infants with a flank mass, hematuria, and
thrombocytopenia.
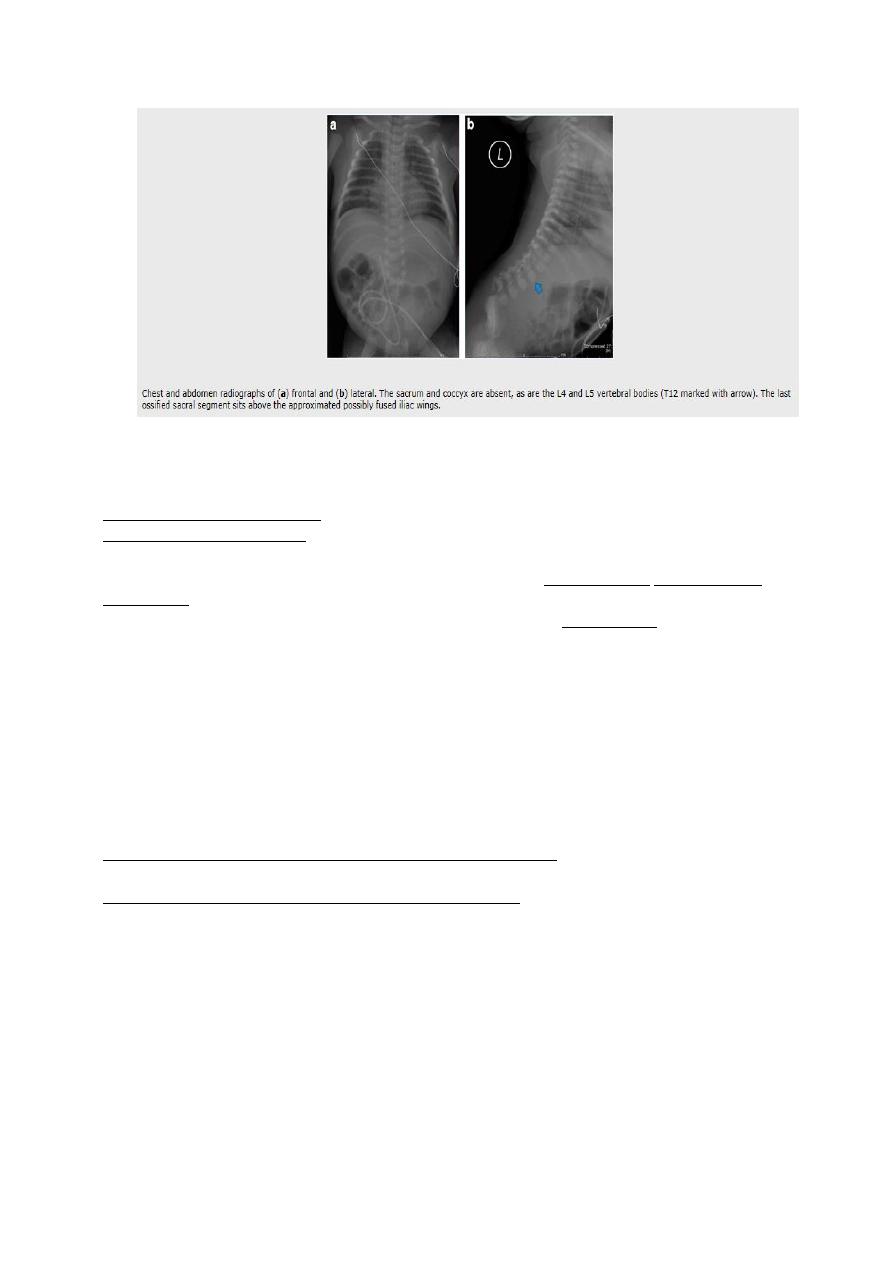
Congenital anomalies
• The incidence is 3X in infants of diabetic mothers;
• cardiac malformations (VSD, ASD, TGA, coarctation of the aorta, others)
• lumbosacral agenesis are most common.
• neural tube defects
• hydronephrosis, other renal anomalies.
4
TREATMENT:
Prenatal evaluation of all pregnant women with overt or gestational diabetes, and planning the
delivery in hospitals where expert obstetric and pediatric care is available.
Preconception glucose control reduces the risk of anomalies and other adverse outcomes, and
glucose control during labor reduces the incidence of neonatal hypoglycemia.
Regardless of size, all infants of diabetic mothers should initially receive intensive care.
Hypoglycemia is defined; plasma glucose of 30 to 45 mg/dl (25 to 40 mg/dl in whole blood) in
term infants.
The best treatment of mild, transient neonatal hypoglycemia is early feeding, whether the
neonate is an IDM or not.
A plasma or blood glucose level of less than 20 or 25 mg/dl, respectively, requires
intravenous glucose administration unless the infant readily takes a good feeding and remains
normoglycemic.
Asymptomatic infants should have a blood glucose determination within 1 hr of birth and then
every hour for the next 6–8 hr;
If clinically well and normoglycemic, oral or gavage feeding with breast milk or formula
should be started as soon as possible and continued at 3 hr intervals. If any question arises
about an infant's ability to tolerate oral feeding, the feeding should be discontinued and
glucose is given by peripheral intravenous infusion at a rate of 4–8 mg/kg/min.
Hypoglycemia should be treated, even in asymptomatic infants, by frequent feeding and/or
intravenous infusion of glucose.
Bolus injections of hypertonic glucose should be avoided because they may cause further
hyperinsulinemia and potentially produce rebound hypoglycemia
5
HYPOCALCEMIA
• Calcium concentration in the immediate newborn period decreases in all newborn infants.
• Hypocalcemia is usually defined as a total serum concentration less than 7 mg/dl.
Clinical Findings
• Hypocalcemic tetany; includes a high-pitched cry, jitteriness, tremulousness, and seizures.
• Apnea, muscle twitching, laryngospasm.
The next 2 signs are rare in the immediate newborn period.
• Chvostek sign :facial muscle spasm when the side of the face (over the 7
th
nerve) is tapped.
• Trousseau sign :carpopedal spasm induced by partial inflation of a blood pressure cuff
Hypocalcemia tends to occur at two different times in the neonatal period:
Early-onset hypocalcaemia; occurs in the first 2 days of life and is associated with
prematurity, maternal diabetes, asphyxia, and, rarely maternal hypoparathyroidism.
Late-onset hypocalcemia; occurs at approximately 7–10 days and is observed in;
• Infants receiving modified cow's milk rather than infant formula (high phosphorus intake).
• In infants with hypoparathyroidism
• In infants with hypomagnesemia.
• Mothers with vitamin D deficiency .
Treatment
A. oral calcium therapy:
• The oral administration of calcium salts is a preferred method of treatment for chronic forms
of hypocalcemia resulting from hypoparathyroidism but is rarely used in early-onset
hypocalcemia.
• Calcium in the form of calcium gluconate can be given as a diluted solution or added to
formula feedings several times a day.
• If a 10% solution of calcium gluconate is used, the dose is 5–10 ml/kg/day given orally in
divided doses, every 4 - 6 hours.
B. intravenous calcium therapy:
• Intravenous calcium therapy given in symptomatic hypocalcemia
• The infusion must be given slowly so that there is no sudden increase in calcium concentration
of blood entering the right atrium, which could cause severe bradycardia and even cardiac
arrest.
Hypomagnesaemia
• Hypomagnesemia occurs when serum magnesium levels fall below 1.5 mg/dl
(0.62 mmol/l).
• It occurs during exchange transfusion with citrated blood, which is low in magnesium
because of binding by citrate, approximately 10 days are required for return to normal.
• Hypomagnesemia should also be suspected in any patient with tetany not responding
to calcium therapy.
• Immediate treatment consists of intramuscular injection of magnesium sulfate. For newborn
infants, 25-50 mg/kg/dose every 8 hr for 3-4 doses usually suffices.
6
