P
EDIATRICS
CARDIOLOGY
C o l l e g e o f m e d i c i n e
A l - M u s t a n s i r y i a h U n i v e r s i t y
A B D E L - S A L A M D A W O O D
P e d i a t r i c C a r d i o l o g i s t
M.B.Ch.B.; F.I.B.M.C.S. (Pediatrics); F.I.B.M.S. (Cardiology)
2 0 1 7

Reference: website, photo, audio,
handwriting
Time: 45 min
Keep Qs & As to the end
Attendance list
Quiz at the end
2
C
ONTENTS
:
C
ONGENITAL
H
EART
D
ISEASES
V
ENTRICULAR
S
EPTAL
D
EFECT
A
TRIAL
S
EPTAL
D
EFECT
A
TRIOVENTRICULAR
S
EPTAL
D
EFECT
P
ATENT
D
UCTUS
A
RTERIOSUS
C
OARCTATION
O
F
T
HE
A
ORTA
P
ULMONARY
S
TENOSIS
T
ETRALOGY
O
F
F
ALLOT
T
RANSPOSITION
O
F
G
REAT
A
RTERIES
H
EART
F
AILURE
C
ARDIOMYOPATHY
Main Menu
Click on the gray circle opposite each item for selective tour.
CONGENITAL HEART
DISEASES (CHD)
Main Menu
A B D E L - S A L A M D A W O O D
P e d i a t r i c C a r d i o l o g i s t
M.B.Ch.B.; F.I.B.M.C.S. (Pediatrics); F.I.B.M.S. (Cardiology)
CONGENITAL HEART DISEASES (
CONT
.)
These are abnormalities in the cardio-
circulatory structures or function that presented
at birth, even if it is discovered later.
5
6
When “not” to
auscultate the heart
…

7
when to auscultate
the heart …
ETIOLOGY
:
Mostly unknown, but appears to result from
interaction
among
many
factors,
genetic,
environmental and maternal diseases, so it is a
multifactorial etiology.
8
I
NCIDENCE
:
They occur in 8/1000 of live births (about 1%
of this risk increase to 4% for 2
nd
pregnancy
following the birth of a child with CHD & 20% to
siblings having CHD).
9
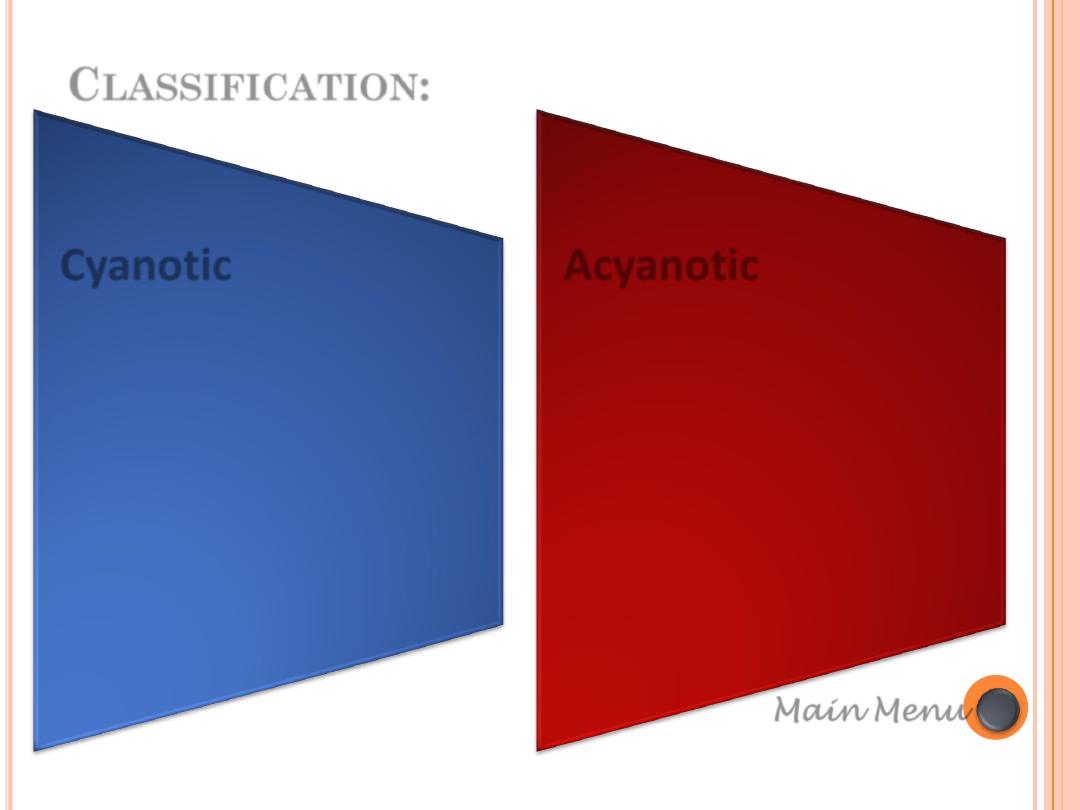
Cyanotic
• Tetralogy Of Fallot 8%
• Transposition of the great
arteries 5%
• Single ventricle 2%
• Tricuspid atresia 2%
• Other complex CHD < 1%
(e.g. double outlet
ventricle & truncus
arteriosus)
Acyanotic
• Ventricular septal defects
(VSD) 10%
• Atrial septal defects (ASD) 10%
• Patent ductus arteriosus (PDA)
10%
• Pulmonary stenosis 10%
• Coarctation of the aorta 8%
• Aortic stenosis 6%
Main Menu
C
LASSIFICATION
:

C
LASSIFICATION OF CONGENITAL HEART DISEASE
:
1.
Conditions with ↑ PBF: ( intar- or extracardiac Lt
→ Rt shunt “without” RV outflow obstruction): best
examples VSD, PDA.
2.
Conditions with ↓ PBF: (shunt “with” RV outflow
obstruction): eg. TOF
3.
Conditions with normal PBF: eg. Coarctation
of aorta, Pulmonary stenosis (PS), Aortic stenosis (AS).
11
PBF: Pulmonary Blood Flow; PDA: patent ductus arteriosus; RV: Right
Ventricle; TOF: Tetralogy of Fallot; VSD: Ventricular Septal Defect

1. C
ONDITIONS WITH
↑ PBF:
Examples:
Ventricular septal defect (VSD); Atrial septal defect (ASD); Patent ductus
arteriosus (PDA); Total anomolus pulmonary venous drainage (TAPVD);
Transposition of great arteries (TGA); Tricuspid atresia without pulmonary
stenosis (PS); Single ventricle without PS.
Clinical Features:
1.
Signs& symptoms of heart failure
2.
Recurrent chest infections
3.
Failure to thrive
Complications:
Pulmonary hypertension +/- Eisenmenger’s syndrome
Chest X-rays:
1.
Cardiomegaly
2.
Plethoric lungs.
12

1. C
ONDITIONS WITH
↑ PBF (
CONT
.):
Echocardiography :
Defining the defect with “no PS”.
Medical Treatment:
1.
Antifailure medications.
2.
Nutritional support
3.
Treatment of infections
4.
SBE prophylaxis
Surgical Treatment:
Palliative: Pulmonary artery (PA) banding
Definitive: closure of the defect
13

C
ONDITIONS WITH
↓
PBF
:
EXAMPLES:
1.
Tetralogy of Fallot (TOF)
2.
Double outlet right ventricle (DORV) with PS
3.
Single ventricle with PS.
CLINICAL FEATURES:
1.
Cyanosis
2.
Hypercyanotic spells (cyanotic spells; Fallot spells; “tet” spells).
Complications:
1.
Polycythemia
2.
Cerebrovascular accident (CVA)
3.
Brain abscess
14

C
ONDITIONS WITH
↓
PBF
(
CONT
.):
Chest X-rays:
1.
“Small” heart
2.
Oligemic lung
Echocardiography :
Different cardiac anomalies “with PS”.
Medical Treatment:
1.
Beta-Blockers
2.
Treatment of complication (eg. Hypercyanotic spells- see later)
15
C
ONDITIONS WITH
↓
PBF
(
CONT
.):
Surgical Treatment:
Palliative: shunt operation (eg. BT shunt
(1)
, Glenn operation
(2)
)
Definitive: according to the lesion.
(1)
“Modified”
Blalock-Taussig (BT) shunt
: using prosthetic matrial e.g., Gore-Tex tube
between the subclavian artery and the ipsilateral pulmonary artery. The “classic”
one connects the subclavian a. directly to the ipsilateral pulmonary artery.
(2)
Glenn operation
: anastomosis between SVC and distal RPA in end-to-end fashion.
Fontan operaion
: complete seperation of of the pulmonary and systemic circuits.
The SVC blood is directed to the RPA (Glenn shunt) and right atrial appendage is
anastomed to the LPA which direct all IVC blood to LPA. Nowadays various forms of
Fontan modifications
16
Conditions with ↓ PBF
Conditions with ↑ PBF
TOF
DORV with PS
Single ventricle with PS
VSD; ASD;PDA; TAPVD; TGA; Tricuspid
atresia without (PS); Single ventricle
without PS.
Examples
Cyanosis
Hypercyanotic spells (cyanotic spells
Fallot spells; “tet” spells).
Signs& symptoms of heart failure
Recurrent chest infections
Failure to thrive
Clinical Features
Polycythemia
Cerebrovascular accident (CVA)
Brain abssess
Pulmonary hypertentin +/-
Eisenmenger’s syndrome
Complications
“Small” heart
Oligemic lung
Cardiomegaly
Plethoric lungs
Chest X-rays
Different cardiac anomalis “with PS”
Defining the defect with “no PS”
Echocardiography
Beta-Blockers
Treatment of complication (eg.
Hypercyanotic spells- see later)
Antifailure medications
Nutritional support
Treatment of infections
SBE prophylaxis
Medical Treatment:
Palliative: shunt operation (eg. BT shunt,
Glenn operation)
Definitive: according to the lesion.
Palliative: Pulmonary artery (PA)
banding
Definitive: closure of the defect
Surgical Treatment
17
IN SUMMARY:

F
EW IMPORTANT NOTES
:
“Pulmonary hypertension”
is defined as a mean
pulmonary artery pressure >25 mmHg at rest or >30
mmHg with exercise. It may be idiopathic, familial, or
associated with multiple other diseases.
“Shunt size”
: The extent of extra flow is assessed as the
ratio of measured pulmonary blood flow (Qp) to
systemic blood flow (Qs). In the normal case, where no
connection exists, the ratio Qp:Qs is 1:1. Left-to-right
shunting results in a Qp:Qs >1, while right-to-left
shunting results in a Qp:Qs <1. For example, a Qp:Qs of
2:1 indicates that the pulmonary blood flow is twice that
of systemic blood flow.
18

F
EW IMPORTANT NOTES
(
CONT
.):
The triad of systemic-to-pulmonary communication,
pulmonary vascular disease and cyanosis is called
“Eisenmenger syndrome”
. The diagnosis of Eisenmenger
syndrome implies that the development of pulmonary
vascular disease as a consequence of increased
pulmonary blood flow, and requires exclusion of other
causes of PAH.
19
Main Menu
VENTRICULAR
SEPTAL DEFECT (VSD)
A B D E L - S A L A M D A W O O D
P e d i a t r i c C a r d i o l o g i s t
M.B.Ch.B.; F.I.B.M.C.S. (Pediatrics); F.I.B.M.S. (Cardiology)
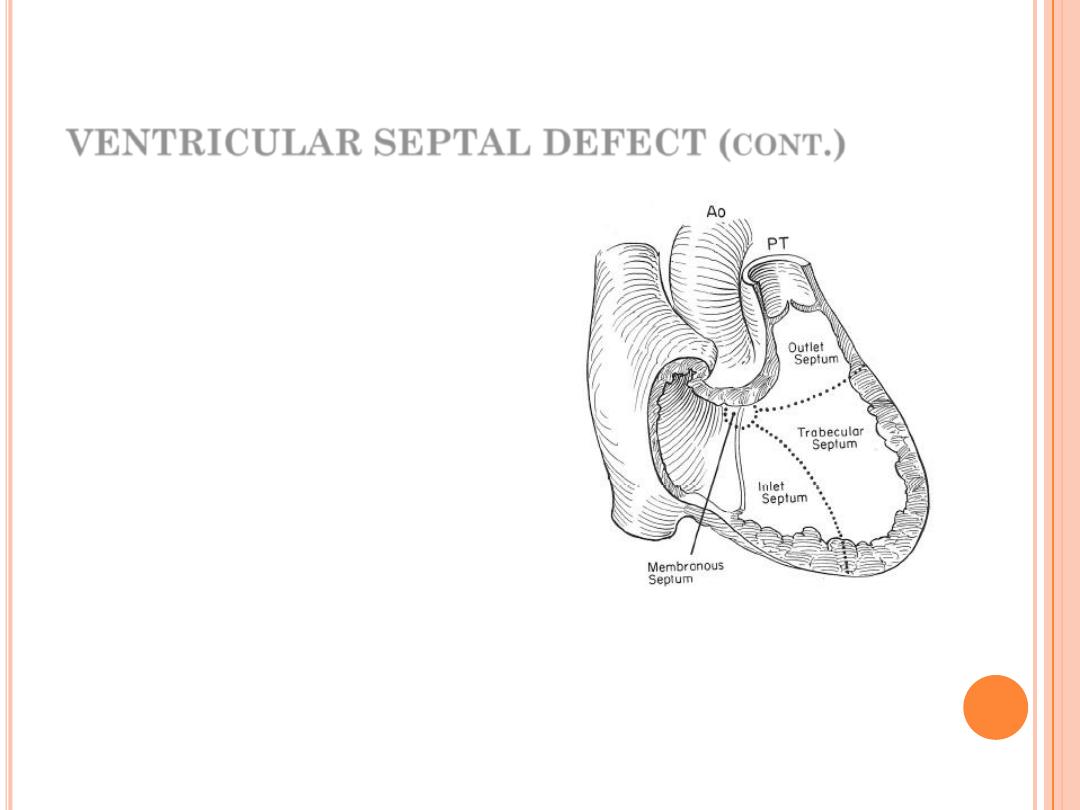
VENTRICULAR SEPTAL DEFECT (
CONT
.)
✓
The most common CHD
✓
Anatomically: classified into:
1.
Perimembranous VSD 80%
2.
Muscular VSD 5%
3.
Inlet VSD 5%
4.
Outlet VSD.
✓
Hemodynamically (functionally)
classified into:
1.
Small VSD (small Lt.-Rt. Shunt)
2.
Moderate VSD
3.
Large VSD
21
Pathophysiologiy:
The magnitude of the L-R shunt depends on: size of
VSD & degree of pulmonary vascular resistance.
In large VSD, there is no resistance to the flow
large
shunt
progressive increase in right ventricular (RV)
& pulmonary artery pressure
pulmonary vascular
resistance which causes Rt.-Lt. (
Eisenmenger syndrome
)
which is irreversible.
In small VSD, there is high resistance to the flow
through the VSD
small Lt.-Rt. Shunt
pressure is
normal in RV and pulmonary artery (PA).
VENTRICULAR SEPTAL DEFECT (cont.)
22
VENTRICULAR SEPTAL DEFECT (
CONT
.)
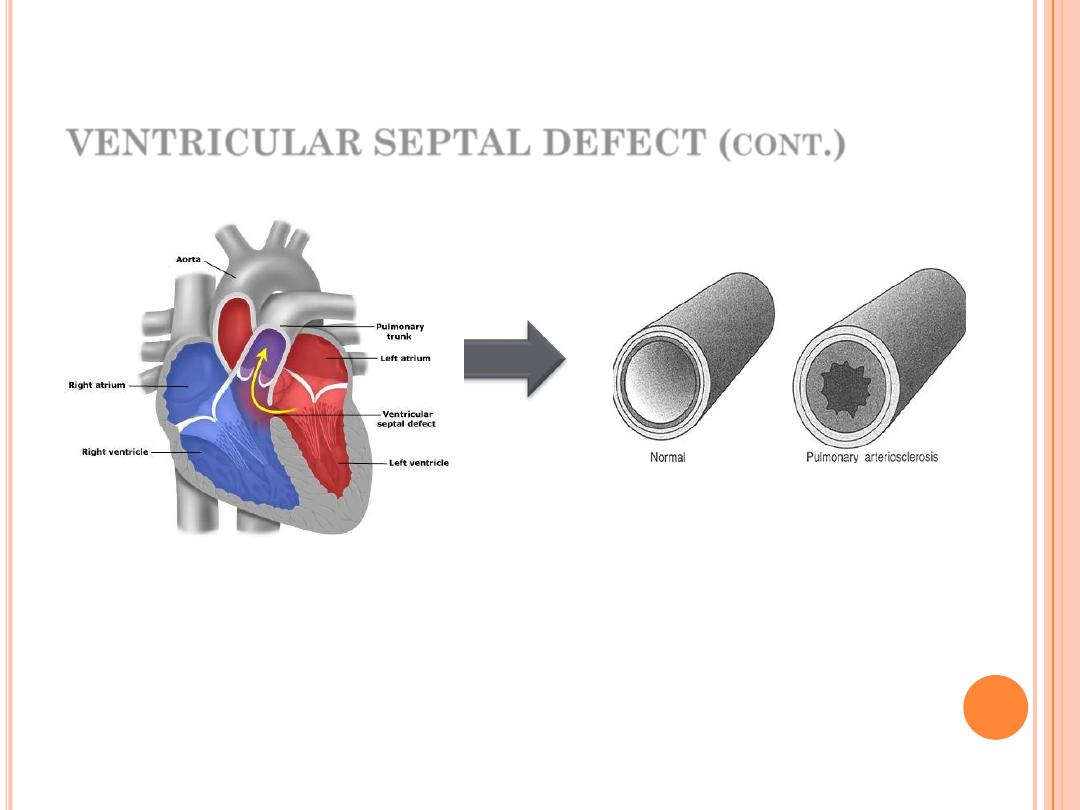
Ventricular septal defect. Some blood
flows through the septal defect from
the left ventricle to the right ventricle
and back around through the lungs to
the left ventricle again.
(Left) Normal pulmonary artery. (Right)
High pressure and rapid flow of blood
into the small pulmonary arteries causes
them
to
thickened;
pulmonary
arteriosclerosis takes place. It cannot be
reversed
23
VENTRICULAR SEPTAL DEFECT (
CONT
.)
Clinical features:
Small VSD: asymptomatic.
O/E: loud harsh, grade 4-6 pansystolic murmur at the
lower left sternal border.
Large VSD: heart failure (between the age of 2-8 weeks);
the patient will show tachypnoea, dyspnoea, recurrent
pulmonary infections, feeding difficulty, poor growth
and excessive sweating.
O/E: the murmur is soft with loud P2.
24
VENTRICULAR SEPTAL DEFECT (
CONT
.)
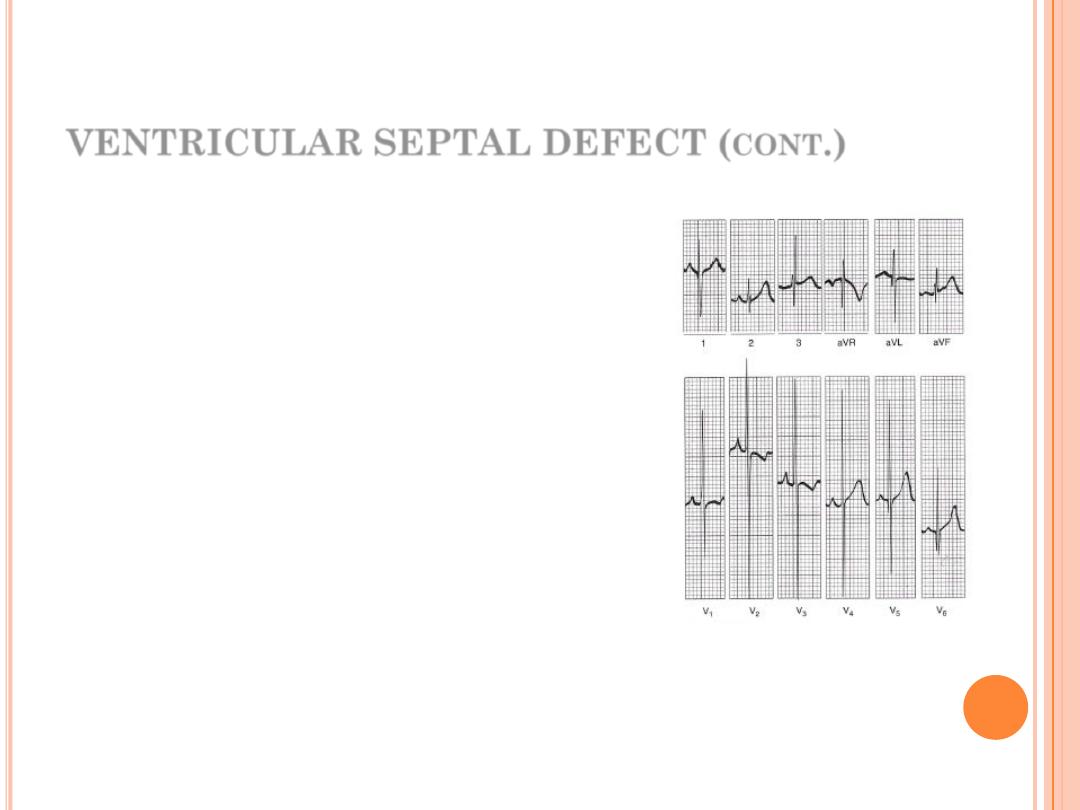
Diagnosis:
ECG:
small VSD normal ECG
large VSD biventricular hypertrophy
ECG with biventricular
hypertrophy in large VSD.
25
VENTRICULAR SEPTAL DEFECT (
CONT
.)
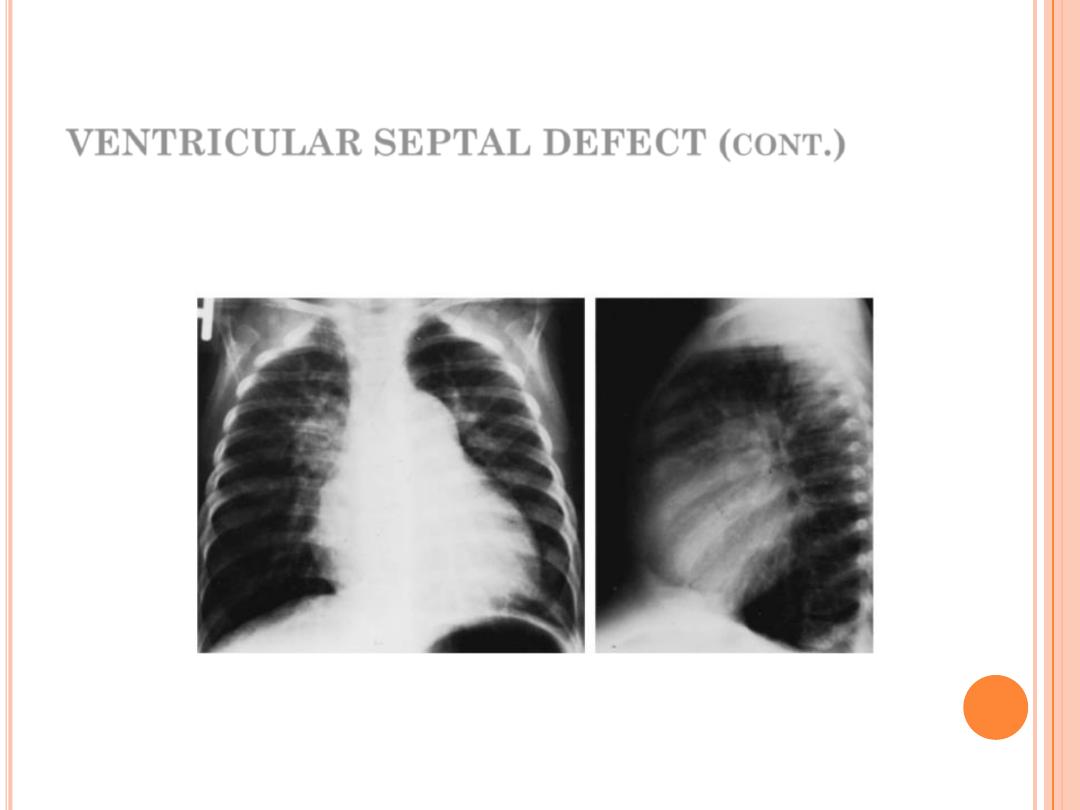
CXR:
small VSD normal
large VSD cardiomegaly, dilated pulmonary vessels (plethoric lung)
Posteroanterior and lateral views of chest roentgenograms
of a ventricular septal defect with a large shunt and
pulmonary hypertension.
26
VENTRICULAR SEPTAL DEFECT (
CONT
.)
Echo:
two-dimensional & Doppler echo must be done in all
patients to determine the following:
✓
Size
✓
Anatomical location
✓
Size & direction of intercardiac shunt
✓
The degree of pulmonary hypertension
✓
Presence e of associated lesion (as TOF)
27
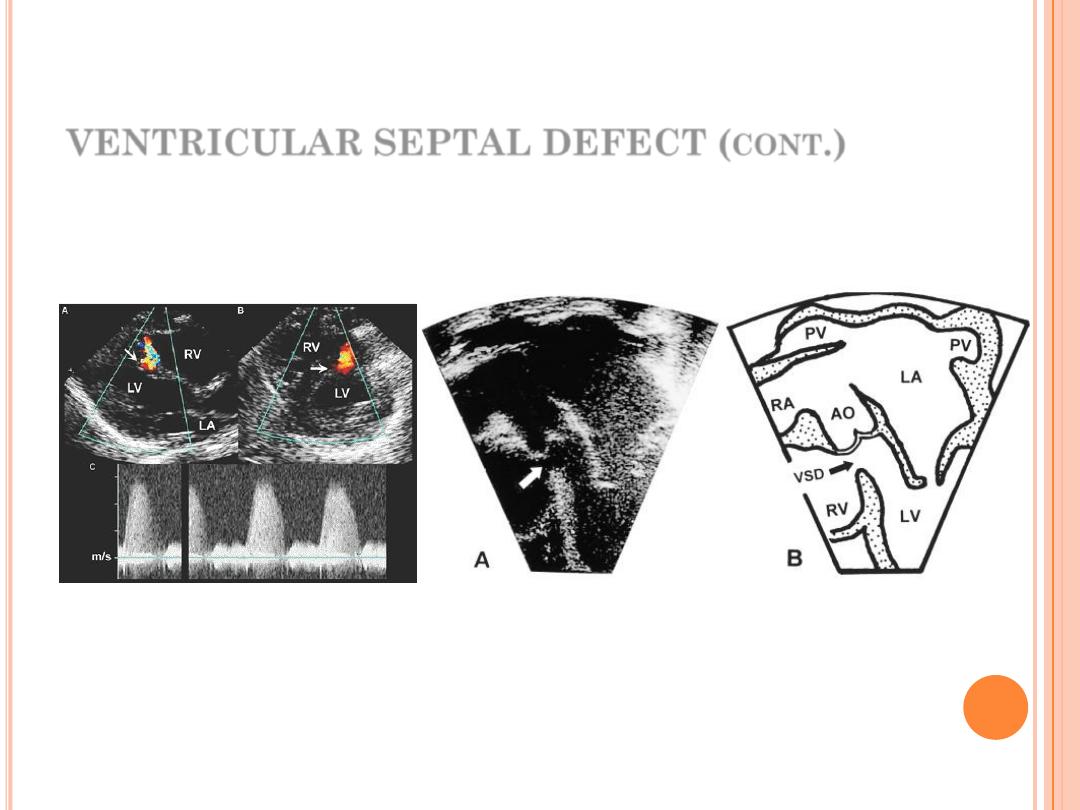
PLAX & PSAX views of echo
showing muscular VSD
A5C view echo showing membranous VSD
VENTRICULAR SEPTAL DEFECT (
CONT
.)
28
VENTRICULAR SEPTAL DEFECT (
CONT
.)
Catheterization & angiography:
A small number of patients with VSD requires cath.
Benefits:
1.
Clear anatomical picture of the location and no. of VSD in
patients when surgery is required.
2.
Estimation of magnitude of the shunt & pulmonary
vascular resistance.
3.
Closing some VSDs.
29
VENTRICULAR SEPTAL DEFECT (
CONT
.)
Natural history:
Small VSD: 50% close spontaneously (the majority during the
1
st
2 years of life); the other will remain asymptomatic.
Large VSD: Without surgical repair, most patients will develop
pulmonary hypertension and some reach to Eisenmenger
syndrome (10%), but 5% will develop infundibular &
pulmonary stenosis.
30
VENTRICULAR SEPTAL DEFECT (
CONT
.)
Management:
Small VSD: The patient needs no treatment apart from
follow-up.
Large VSD: we have medical, surgical and catheterization
options.
31

Medical:
1.
Treatment of heart failure.
2.
Treatment of infection, especially respiratory.
3.
Nutritional support.
VENTRICULAR SEPTAL DEFECT (cont.)
32
Surgical:
Either pulmonary artery banding or total surgical repair.
Indications:
1.
Hemodynamically significant Qp:Qs (>1.5)
2.
LA or LV enlargement
3.
Pulmonary hypertension
4.
Failure to thrive with intractable CHF
5.
Previous episode of SBE
“Catheterization based treatment:”
Most muscular VSD and some membranous VSD can be
closed by devices placed during cardiac catheterization.
VENTRICULAR SEPTAL DEFECT (cont.)
33

Main Menu
Main Menu
ATRIAL SEPTAL
DEFECT (ASD)
A B D E L - S A L A M D A W O O D
P e d i a t r i c C a r d i o l o g i s t
M.B.Ch.B.; F.I.B.M.C.S. (Pediatrics); F.I.B.M.S. (Cardiology)

Reference: website, photo, audio,
handwriting
Time: 45 min
Keep Qs & As to the end
Attendance list
Quiz at the end
36
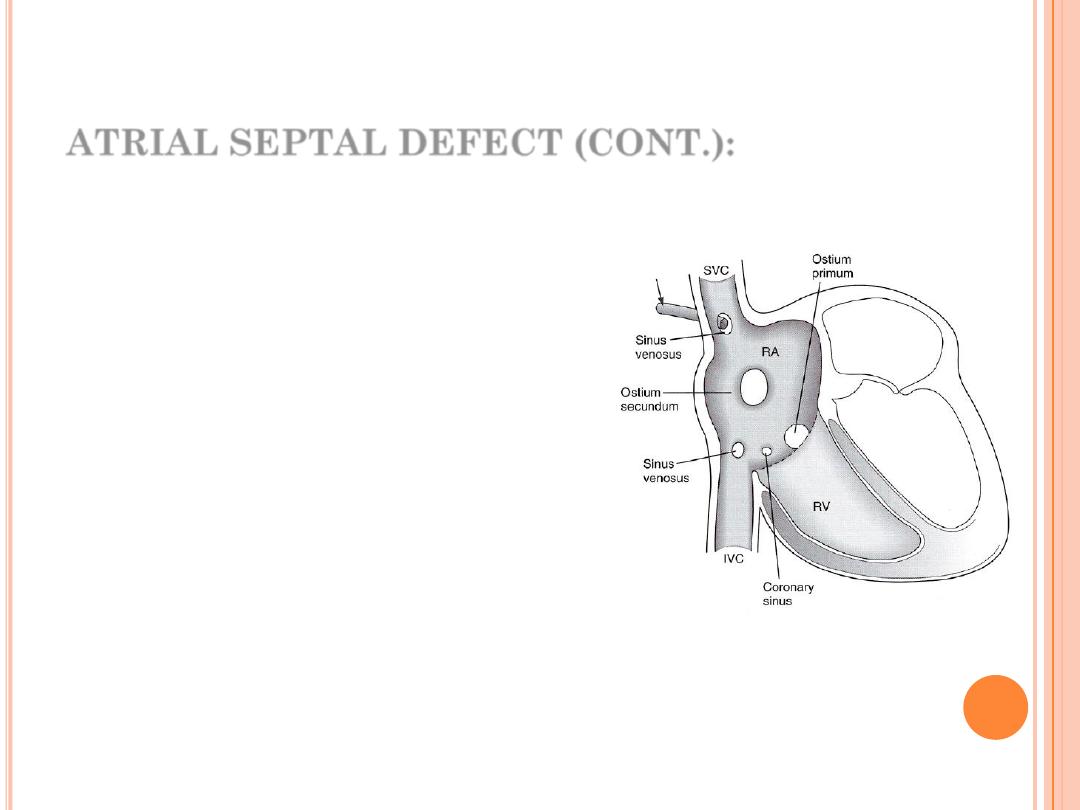
ATRIAL SEPTAL DEFECT (CONT.):
An opening in the inter-atrial septum
other than patent foramen ovale
More common in females (F:M ratio is
3:1).
It has 4 types:
1.
Primum ASD (in lower part) 10%
2.
Secondum ASD (in the middle)
80%
3.
Sinus venosus (near the vena
cavae) 10%
4.
Coronary sinus ASD: rare
37
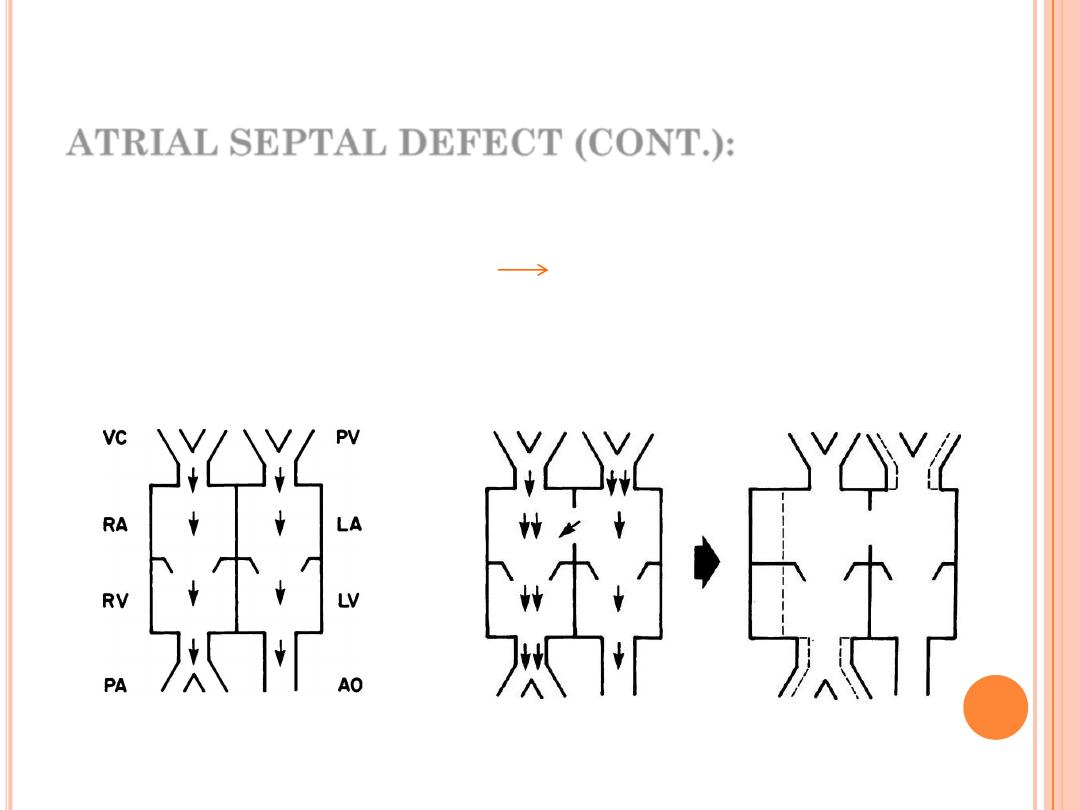
ATRIAL SEPTAL DEFECT (CONT.):
Hemodynamic effect:
There will be chronic Lt.
Rt. Shunt which causes
volume overload on the Rt. sided cardiac structures &
result in their dilatation & increase of pulmonary blood
flow.
38
Normal Physiology
Left-to-right Physiology (Atrial level)
ATRIAL SEPTAL DEFECT (CONT.):
Clinical Features: (mostly secondum type)
Most of them are asymptomatic.
Normal growth
Dx accidentally: Wide, fixed splitting of 2
nd
heart sound,
soft ejection systolic murmur at the 2
nd
left intercostal
space, no thrill (grade 3) & parasternal RV heave.
39
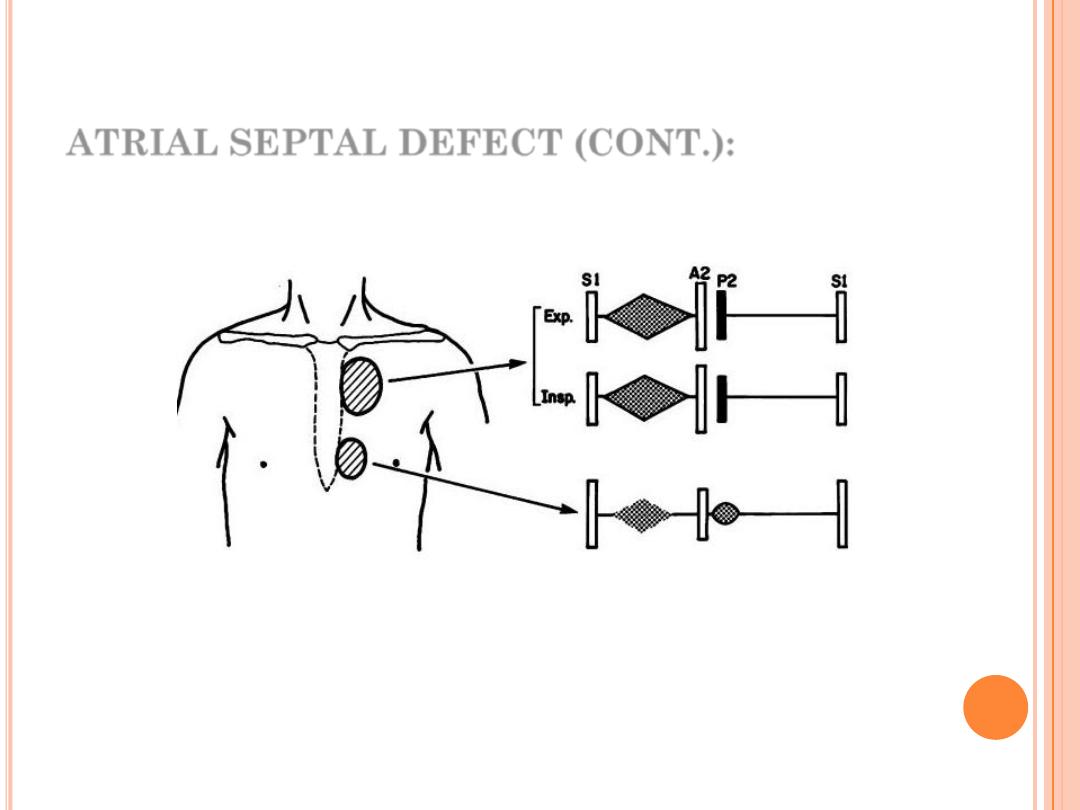
ATRIAL SEPTAL DEFECT (CONT.):
Cardiac findings of ASD: wide, fixed splitting of 2
nd
heart
sound, soft ejection systolic murmur at the 2
nd
left
intercostal space
40
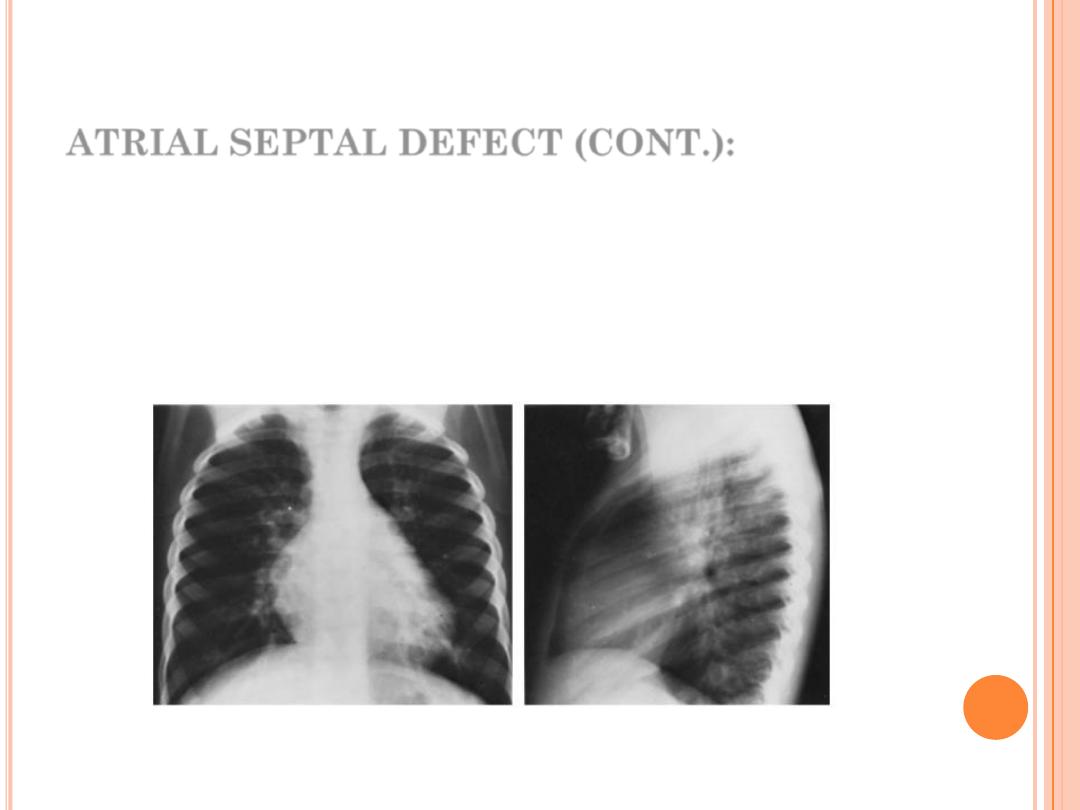
ATRIAL SEPTAL DEFECT (CONT.):
Dx:
CXR:
1. Cardiomegaly of RV configuration. 2. Round apex peak.
3. Increase pulmonary marking
41
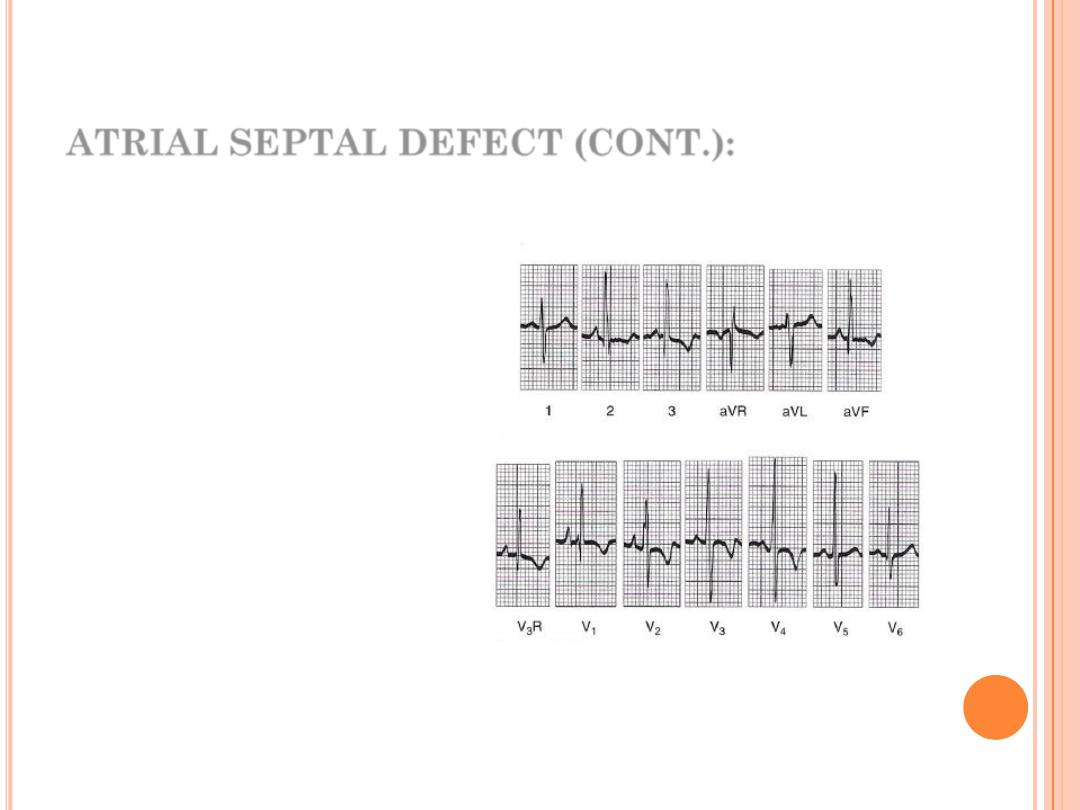
ATRIAL SEPTAL DEFECT (CONT.):
ECG:
1.
Right axis deviation (RAD)
2.
Incomplete RBBB
3.
Peaked P-wave (RA
enlargement)
42
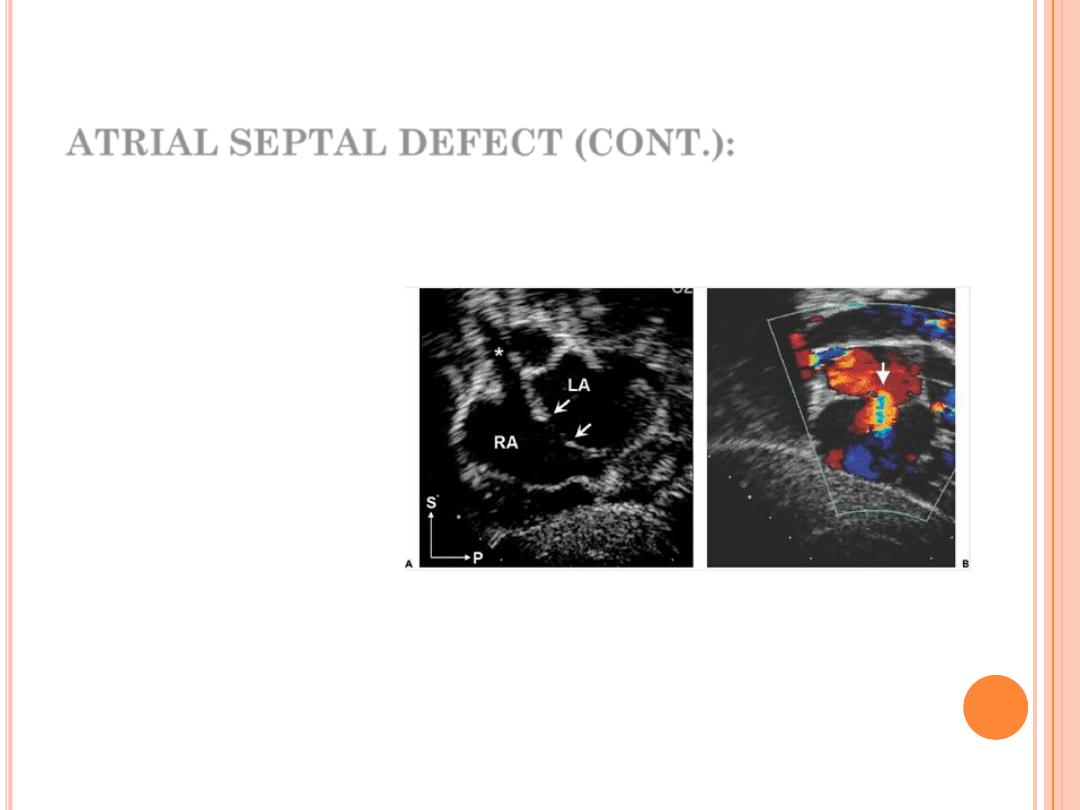
ATRIAL SEPTAL DEFECT (CONT.):
Echo:
Trans-thoracic & trans-esophageal echocardiography is
essential for Dx.
Typical anatomy of a moderate secondum atrial septal defect.
A:
Subcostal sagittal plane image
(bicaval view) showing the central gap in the septum typical of a secondum defect (arrows). *, Superior
vena cava; LA, left atrium; P, posterior; RA, right atrium; S, superior.
B:
Color Doppler map showing the
shunt flow crossing from LA to RA (arrow). To obtain the bicaval (sagittal) view A, the scan plane was
rotated clockwise approximately 90 degrees from the subcostal four-chamber (coronal) plane in B
43
ATRIAL SEPTAL DEFECT (CONT.):
Cardiac Catheterization:
Not essential for Dx, indicated in:
1.
Therapeutic aim.
2.
Exclude associated cardiac anomaly as patent anomalies.
44

ATRIAL SEPTAL DEFECT (CONT.):
Natural history:
1.
Spontaneous closure occurs more than 80% of the time in
patients with defects between 3 and 8 mm before 1½ years of
age. An ASD with a diameter greater than 8 mm rarely closes
spontaneously.
2.
Most children with an ASD remain active and asymptomatic.
3.
If a large defect is untreated, CHF and pulmonary hypertension
develop in adults who are in their 20s and 30s.
4.
With or without surgery, atrial arrhythmias (flutter or fibrillation)
may occur in adults.
5.
Infective endocarditis does not occur in patients with isolated
ASDs.
6.
Cerebrovascular accident, resulting from paradoxical
embolization through an ASD, is a rare complication.
45
ATRIAL SEPTAL DEFECT (CONT.):
Treatment:
Closure of ASD is indicated after the
age of 3 years when:
1.
Symptomatic with CHF
2.
Volume overload (Qp:Qs >1.5:1)
3.
Pulmonary Hypertension
Surgical closure is indicated only in
cases where catheter closure is not
possible (primum) or failed
46
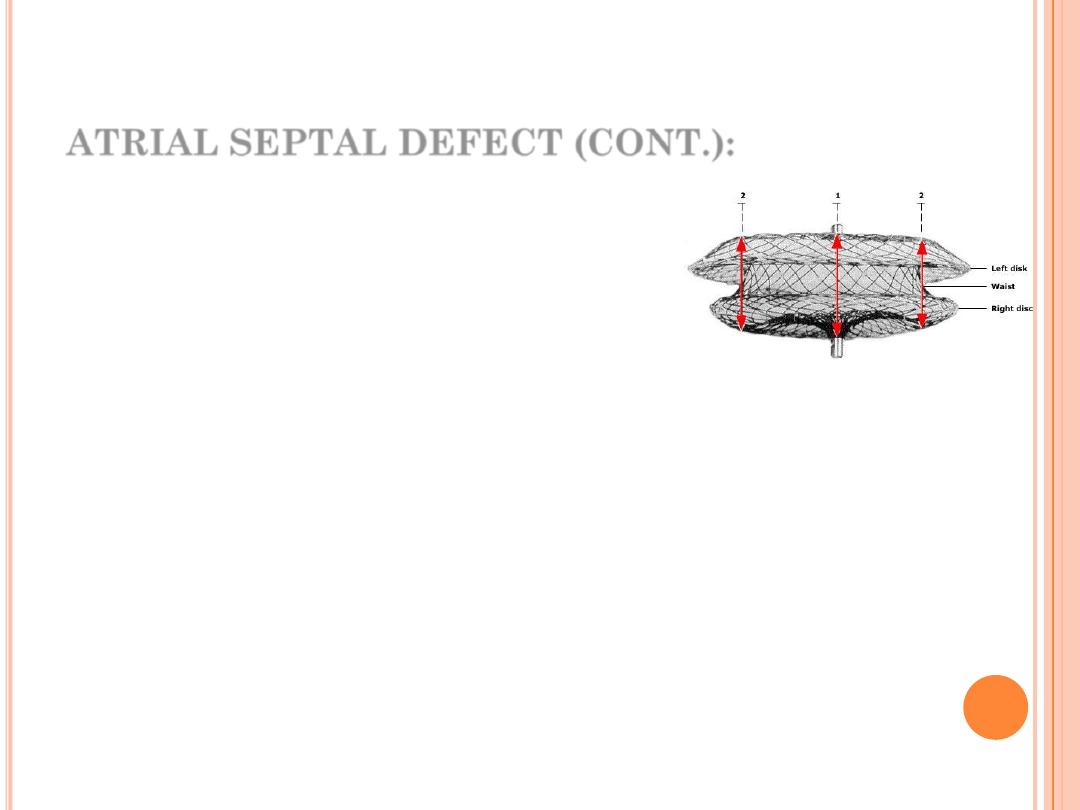
In the lateral view the Amplatzer septal occluder has
a waist between the left and right atrial discs;
the left atrial disc is slightly larger than the right one.
Broken lines and red arrows indicate measurement
sites.
ATRIAL SEPTAL DEFECT (CONT.):
47
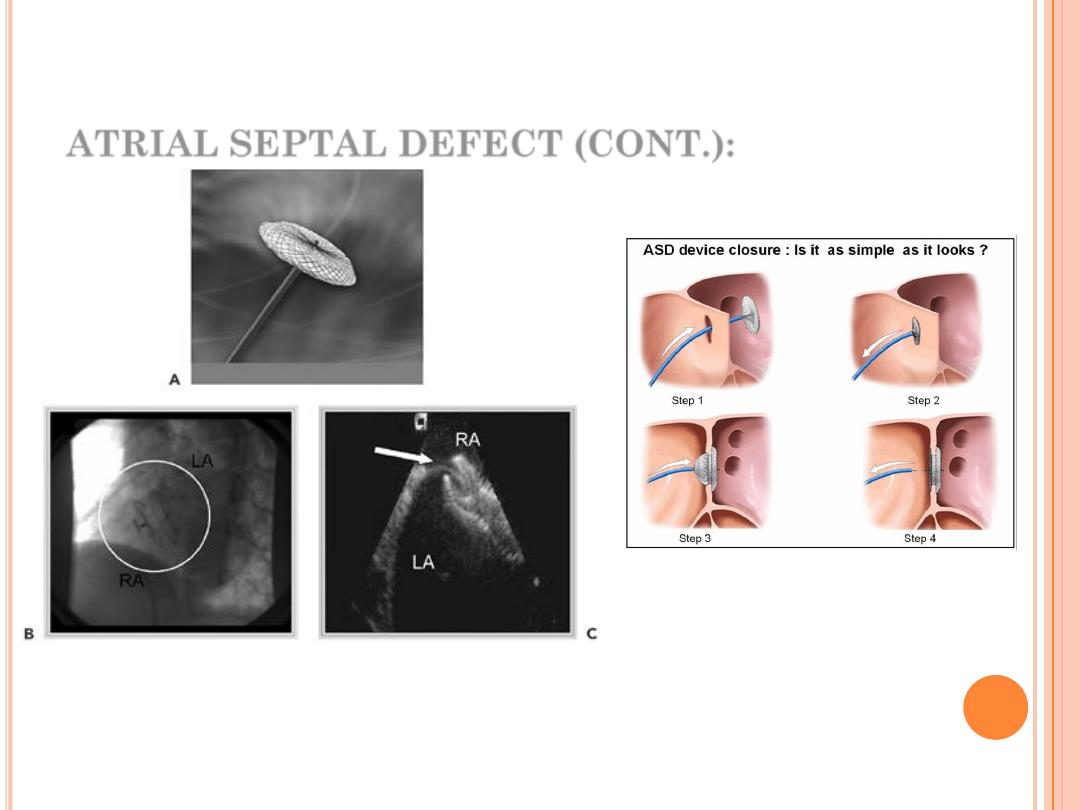
A. Amplatzer Septal Occluder (AGA Medical, Golden Valley, MN). B. Postimplant fluoroscopy (device in
circle). C. Postimplant intracardiac echo image, showing device entrapping thin septum primum
(arrow). LA, left atrium; RA, right atrium.

Main Menu
Main Menu
ATRIOVANTRICULAR
SEPTAL DEFECT
(E
NDOCARDIAL
C
USHION
D
EFECT
)
A B D E L - S A L A M D A W O O D
P e d i a t r i c C a r d i o l o g i s t
M.B.Ch.B.; F.I.B.M.C.S. (Pediatrics); F.I.B.M.S. (Cardiology)
ATRIOVANTRICULAR SEPTAL DEFECT (
CONT
.):
It is a group of anomalies sharing a defect at the site
of atrioventricular septum and abnormality in the
atrioventricular valve.
Common in Down's syndrome, so all patients with
Down's syndrome (children) should have cardiac
evaluation if symptomatic or before 6 months of age.
Equal no. of males and females are affected.
50
Partial
: ASD primum, clefted
mitral valve.
Complete
: ASD primum, large
inlet VSD, common single
atrio-ventricular valve.
ATRIOVANTRICULAR SEPTAL DEFECT (
CONT
.):
Classification:
51
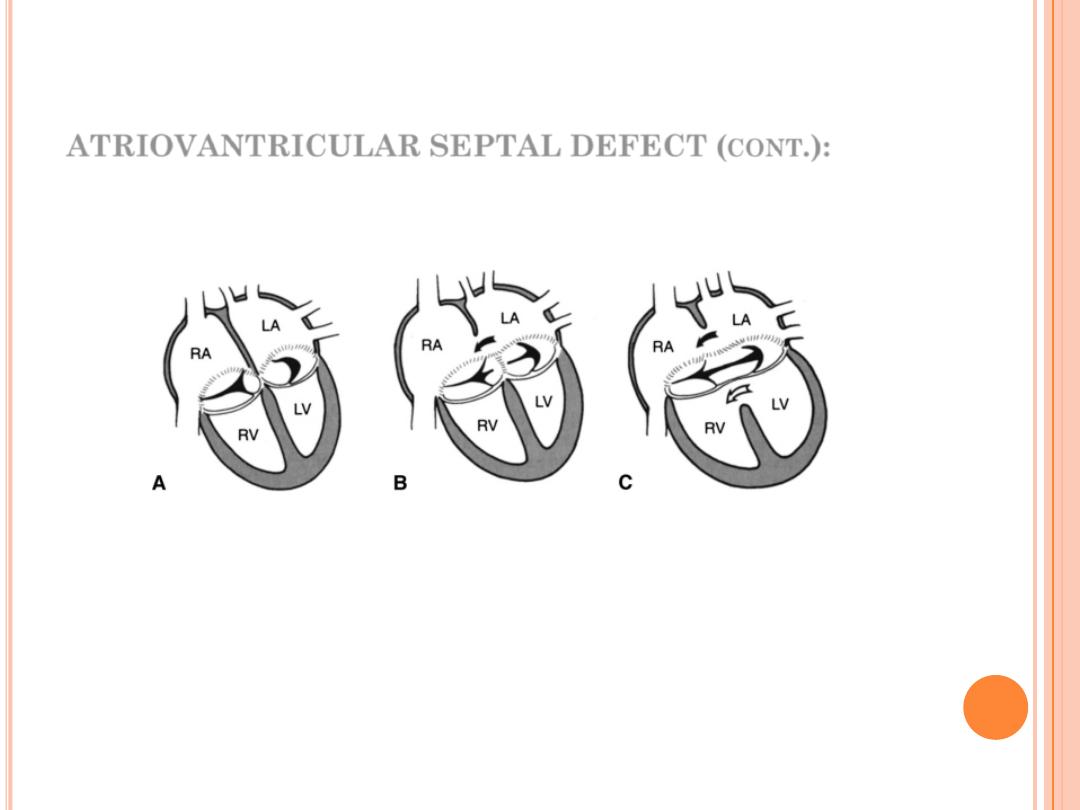
ATRIOVANTRICULAR SEPTAL DEFECT (
CONT
.):
Partial defect
:
Classification of AV septal defect
Complete defect
Normal heart
52
ATRIOVANTRICULAR SEPTAL DEFECT (
CONT
.):
Clinical features:
Partial: either asymptomatic (mainly) or mild symptoms.
O/E: features of ASD + murmur of mitral regurgitation.
Complete: as the above with heart failure and/or
pulmonary vascular disease.
53
ATRIOVANTRICULAR SEPTAL DEFECT (
CONT
.):
CXR:
Cardiomegaly is always present and involves all four
cardiac chambers. Pulmonary vascular markings are
increased, and the main PA segment is prominent.
ECG:
1.
“Superior” QRS axis with the QRS axis between -40 and -150
degrees is characteristic of the defect.
2.
Most of the patients have a prolonged PR interval (first-degree
AV block).
3.
RVH or RBBB is present in all cases, and many patients have LVH,
too.
.
54
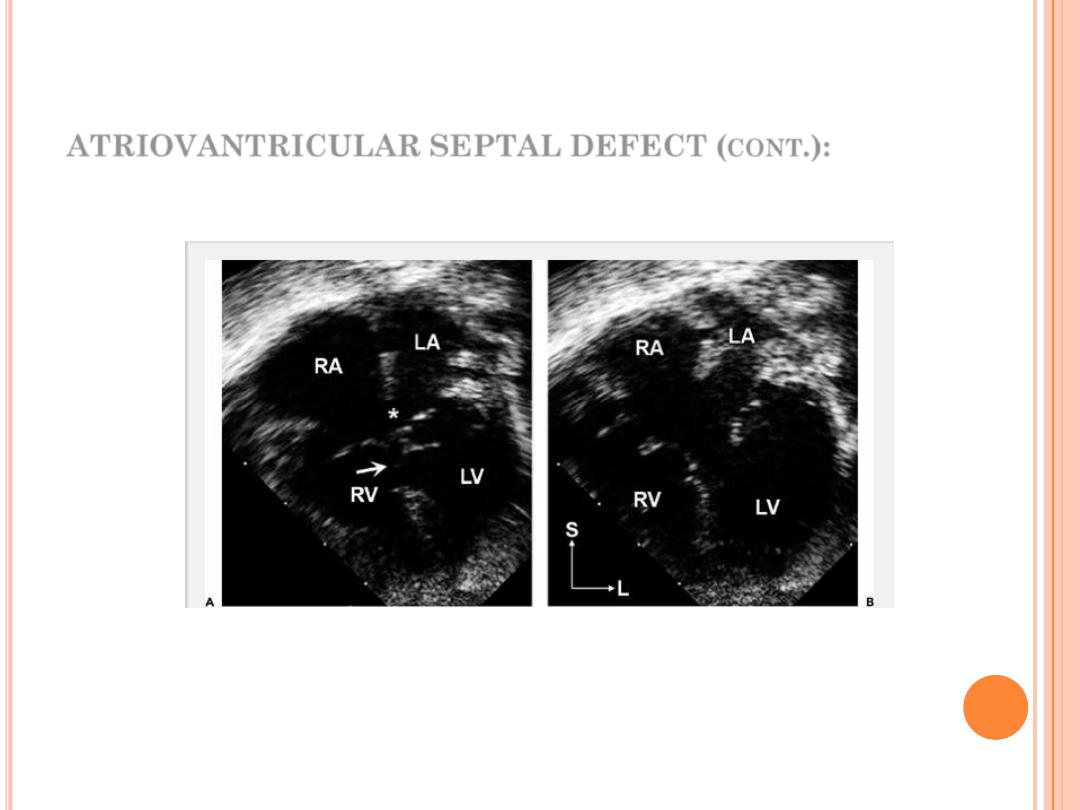
ATRIOVANTRICULAR SEPTAL DEFECT (
CONT
.):
Echo: is diagnostic.
A4C view in systole(A) & diastole (B) showing complete AV septal defect.
55
ATRIOVANTRICULAR SEPTAL DEFECT (
CONT
.):
Natural history:
It depends on the size of various atrial and
ventricular defects and the amount of mitral
regurgitation.
The ostium primum ASD with no mitral
regurgitation has the same benign natural
history of simple secondum ASD, but with
complete AV-canal defect, heart failure and/or
pulmonary vascular disease may occur.
Rx:
Repair the septal effect (patching or total
septation), it will cause complete repair.
56

Main Menu
Main Menu
PATENT DUCTUS
ARTERIOSUS (PDA)
A B D E L - S A L A M D A W O O D
P e d i a t r i c C a r d i o l o g i s t
M.B.Ch.B.; F.I.B.M.C.S. (Pediatrics); F.I.B.M.S. (Cardiology)
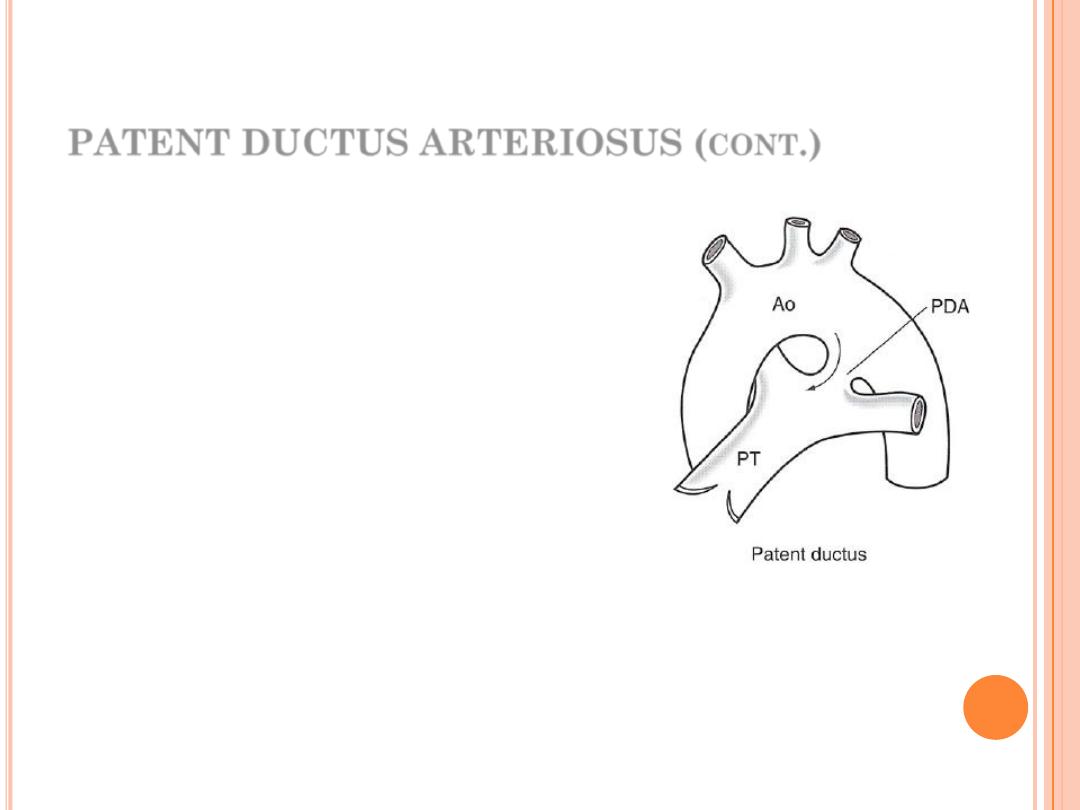
PATENT DUCTUS ARTERIOSUS (
CONT
.)
It is a channel that connect the
pulmonary
artery
with
the
descending aorta (isthmus part).
It results from the persistence of
patency
of
the
fetal
ductus
arteriosus after birth.
It is the most common lesion in
infant of mothers with congenital
rubella
PDA more common in females (like
ASD).
59
PATENT DUCTUS ARTERIOSUS (
CONT
.)
Clinical features:
Patients with small PDA usually are “asymptomatic” but
large PDA will result in heart failure & pulmonary
hypertension along with growth failure.
O/E:
Collapsing pulse with pulse pressure
on auscultation classical continuous machinery
murmur (systolic & diastolic) at the pulmonary area with
a thrill (not always ?).
60
PATENT DUCTUS ARTERIOSUS (
CONT
.)
ECG:
In small PDA, it is normal, but large PDA left ventricular
hypertrophy (LVH) or biventricular hypertrophy.
61
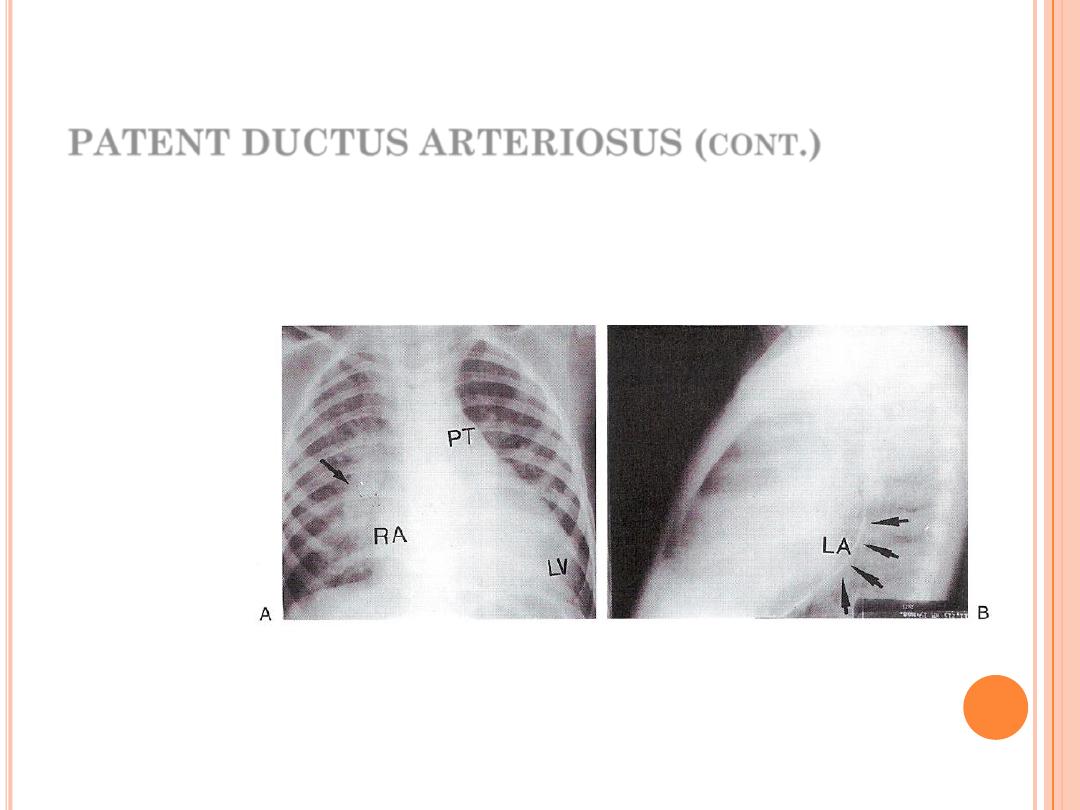
PATENT DUCTUS ARTERIOSUS (
CONT
.)
Chest X-ray:
Cardiomegaly, plethoric lung, and prominent pulmonary conus.
62
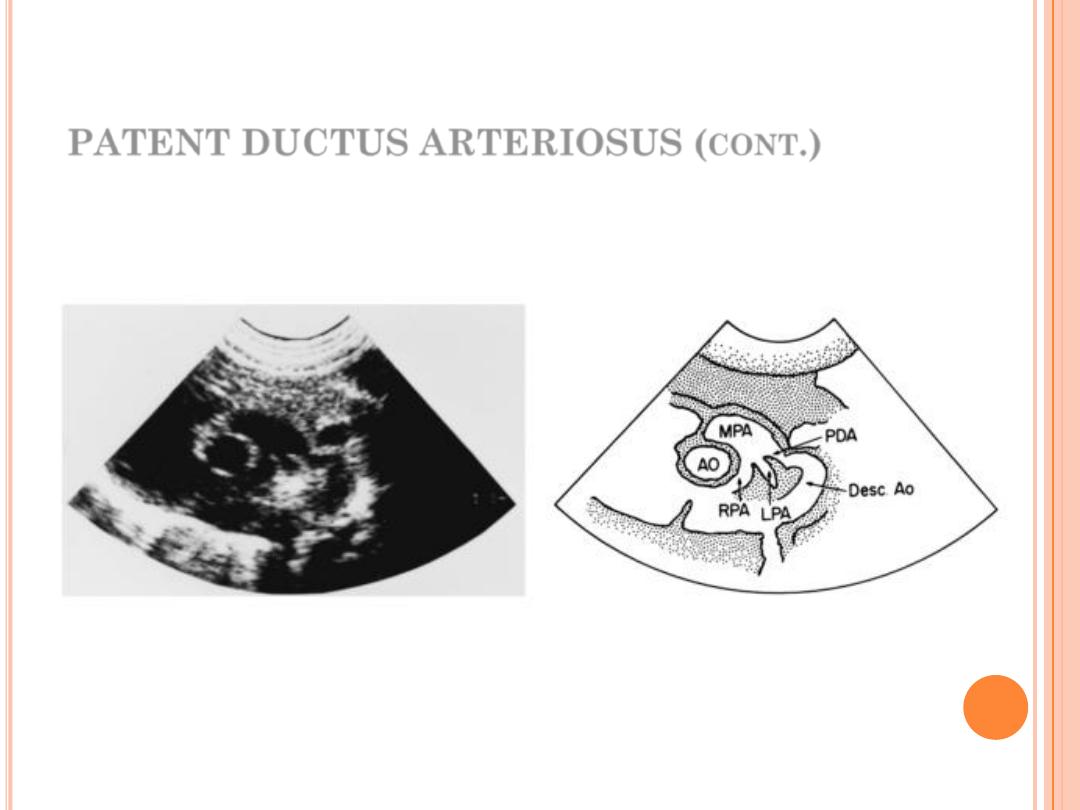
PATENT DUCTUS ARTERIOSUS (
CONT
.)
Echo: is diagnostic
63
PATENT DUCTUS ARTERIOSUS (
CONT
.)
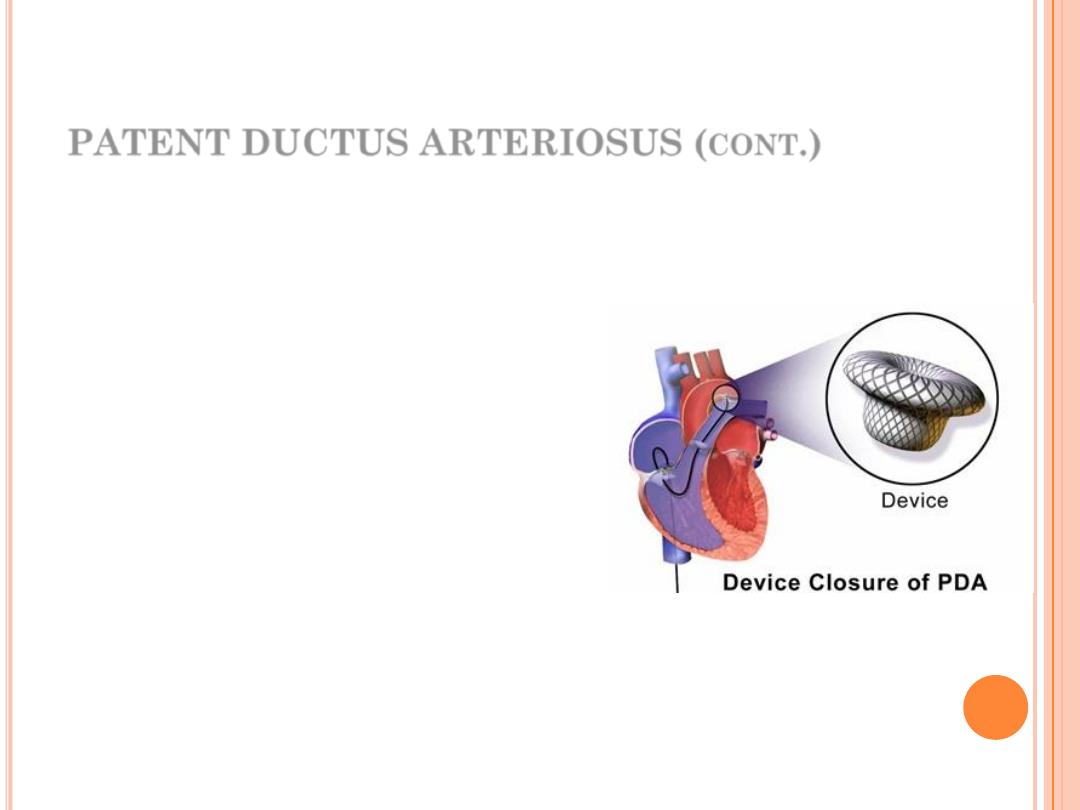
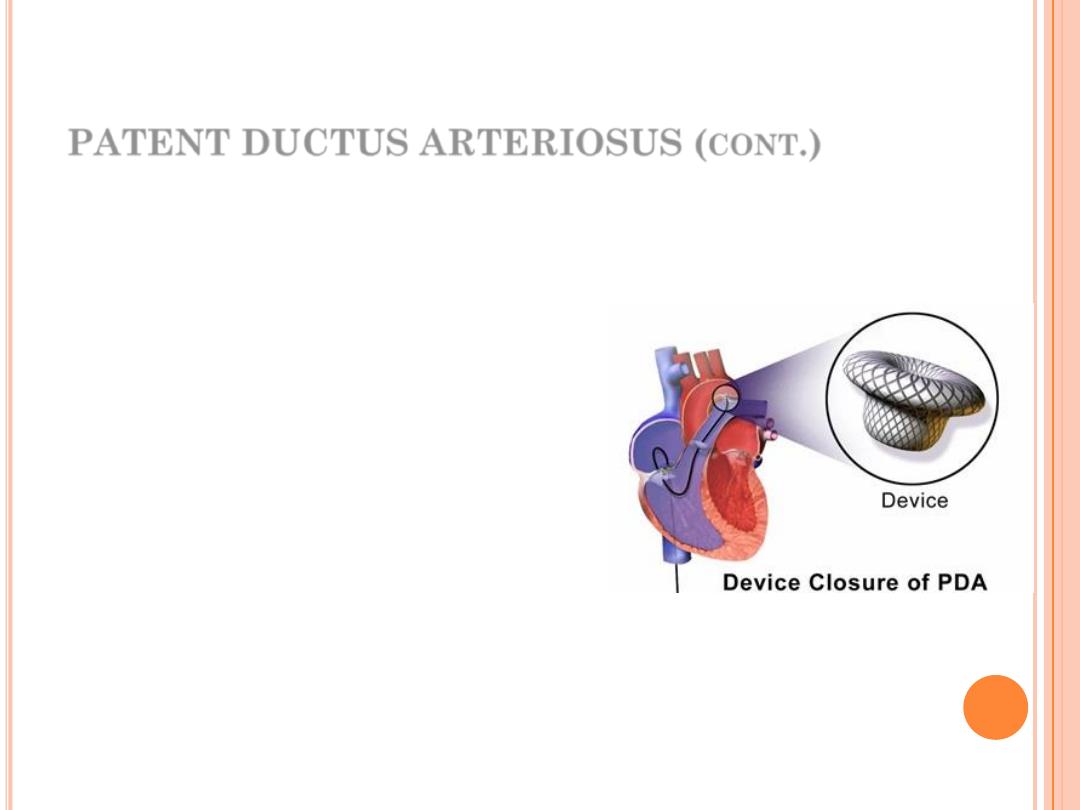
Rx:
“Closure should be done” (6
months – 1 year) whatever the
size due to possible
complications.
Most PDA closures can be done
by transcatheter device or coil
and some need surgical closure
(when catheter closure is not
possible or failed).
64
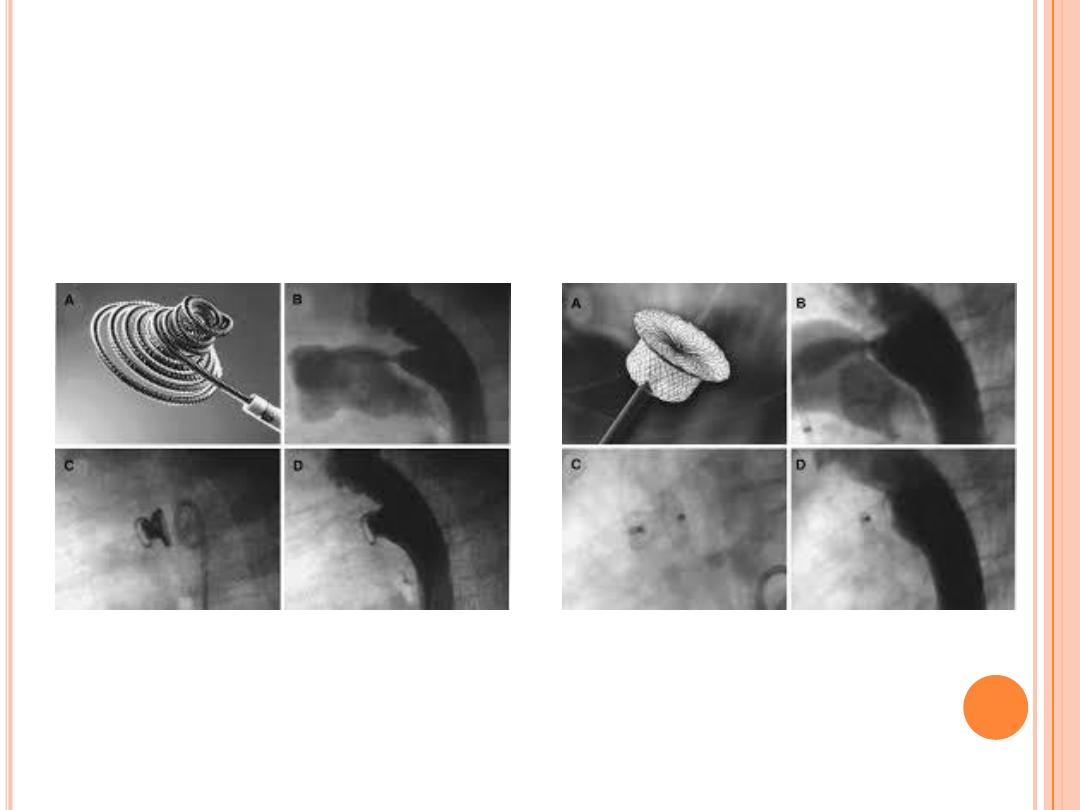
65
Coil Closure
Device Closure
PATENT DUCTUS ARTERIOSUS (
CONT
.)
Homework:
PDA closure in premature babies
is an exception. Why?
Submit next week
66

Main Menu
Main Menu
COARCTATION OF
THE AORTA
A B D E L - S A L A M D A W O O D
P e d i a t r i c C a r d i o l o g i s t
M.B.Ch.B.; F.I.B.M.C.S. (Pediatrics); F.I.B.M.S. (Cardiology)
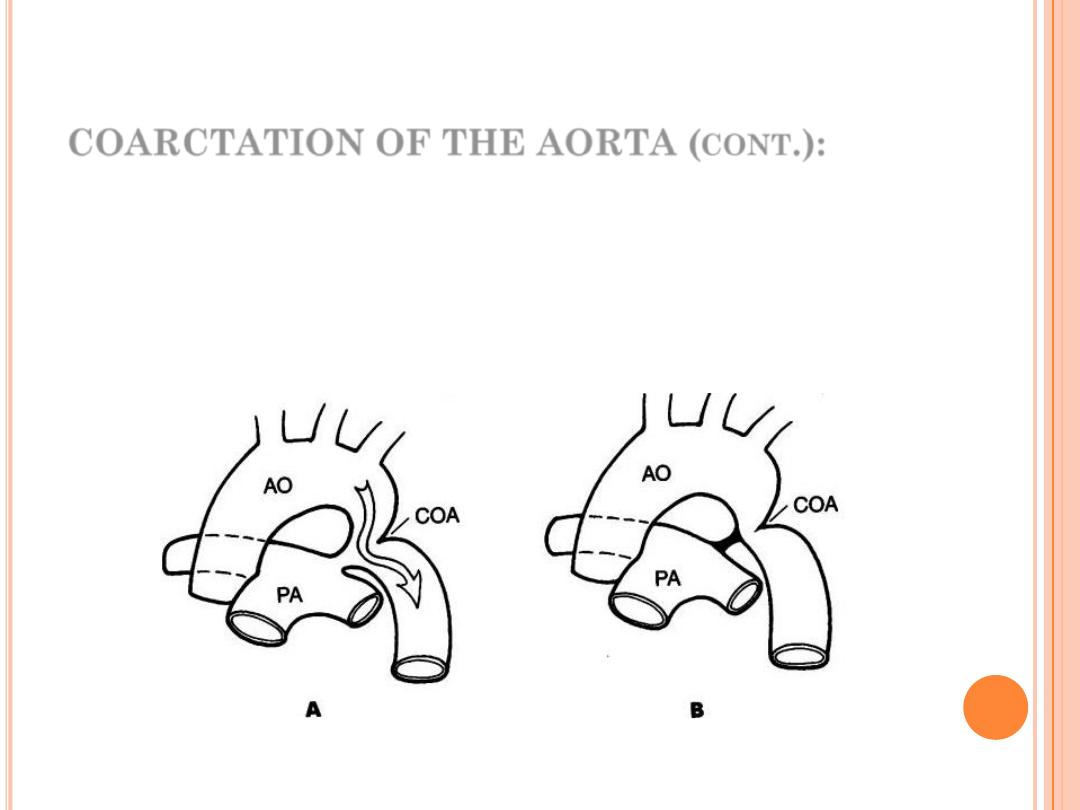
COARCTATION OF THE AORTA (
CONT
.):
✓
Localized, discrete narrowing of the thoracic aorta occurs
in 6-8% of congenital heart disease.
✓
More common in males with M:F = 2:1.
✓
More common cardiac lesion in Turner syndrome.
69
COARCTATION OF THE AORTA (
CONT
.):
C/F:
In infants, usually presented with congestive heart failure,
dyspnoea, poor feeding.
In older children, might be only systemic hypertension
OE: Radiofemoral delay and pressure difference between
the upper and lower limb by 20 mmHg (diagnostic)
70
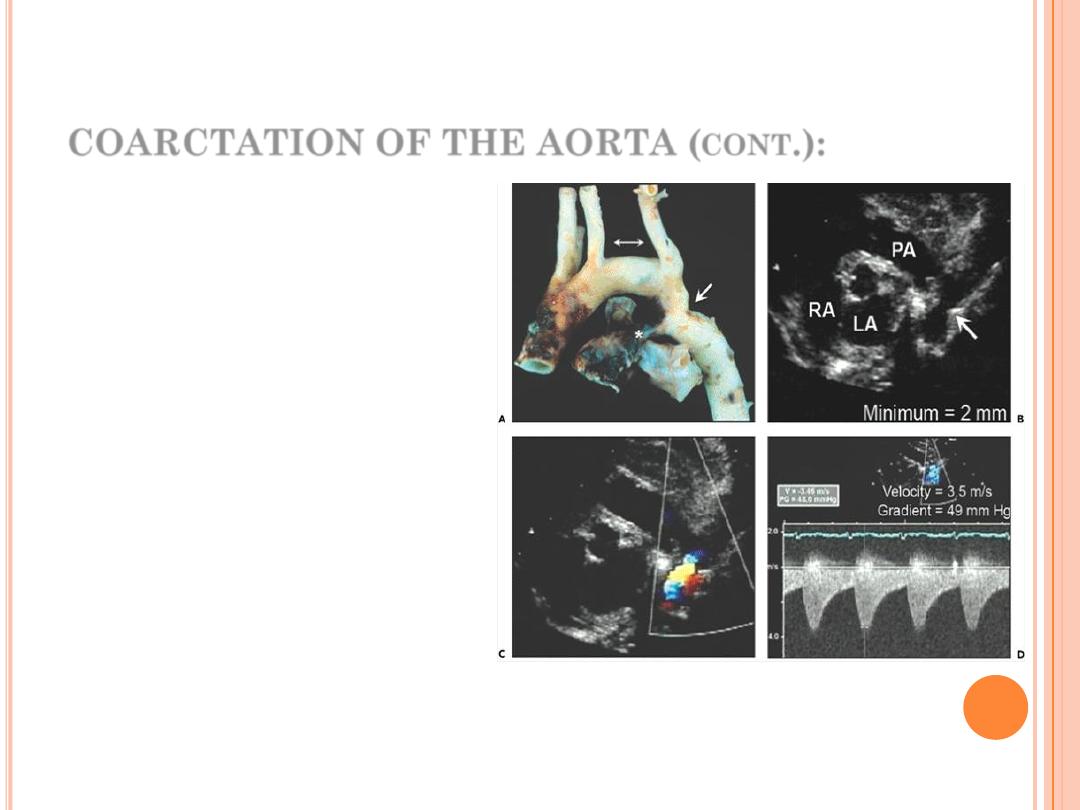
COARCTATION OF THE AORTA (
CONT
.):
Diagnostic tests:
Chest x-rays shows
characteristic features
in older children…
How? (Homework)
Echo:
diagnostic, non-
invasive, relatively cheap
test of choice.
71
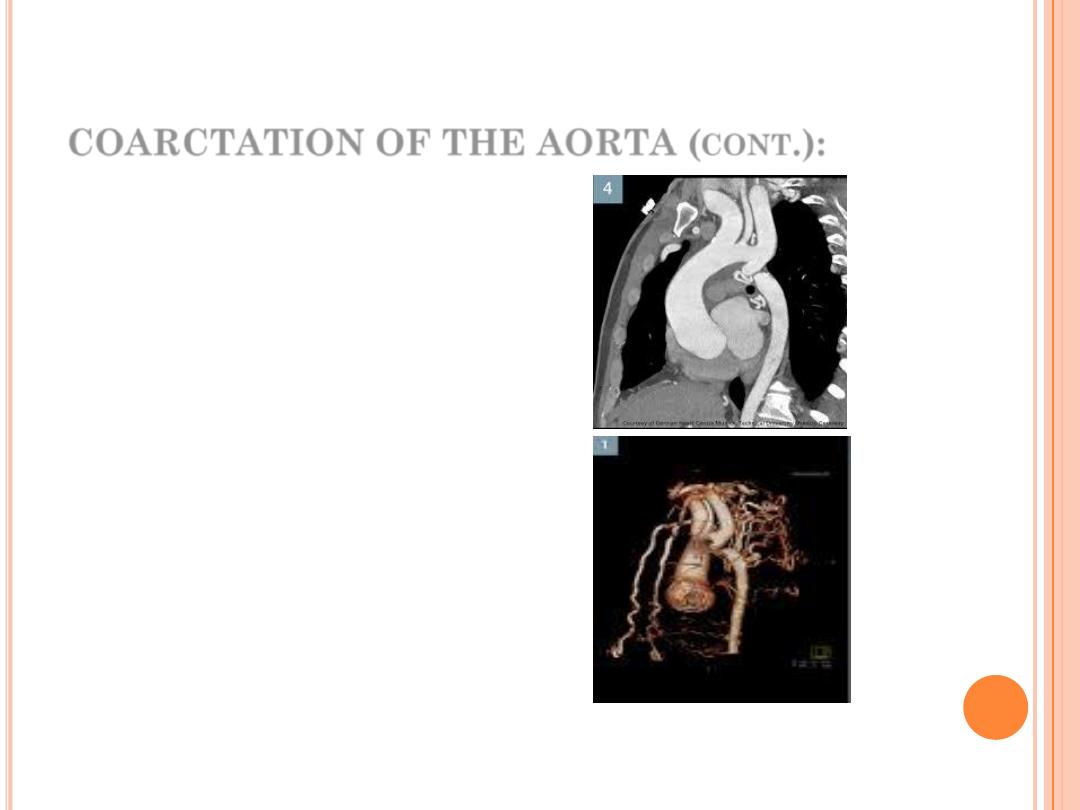
COARCTATION OF THE AORTA (
CONT
.):
Diagnostic tests:
MRI & CT angiography:
radiation exposure,
costlier, needs GA, not
always available
used in difficult cases
only
.
72
COARCTATION OF THE AORTA (
CONT
.):
Rx:
1.
Balloon angioplasty (with or
without stent)
2.
Surgery, e.g. by end to end
anastomosis.
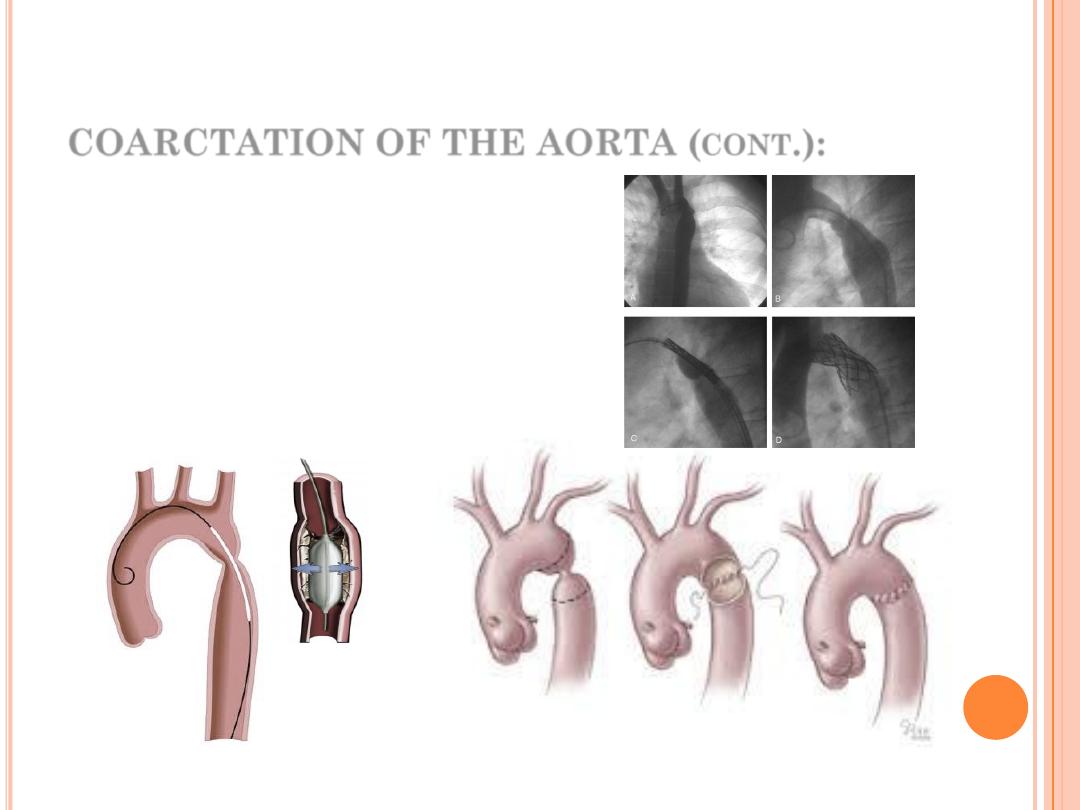
73
Balloon Angioplasty
Surgical Angioplasty

Prognosis:
The mean age of death for untreated coarctation is
about 34 years and the most common cause of death
are: heart failure, aortic rupture, infective endocarditis,
intracranial hemorrhage (due to B.P. or aneurysm).
74
THANKS FOR
LISTENING
Visit our channel on the you tube:
https://www.youtube.com/watch?v=3mBp2
WV0dwU
