
HCG
It is produced by cytotrophoblast detected in
maternal blood from 10 th day of fertilization
&peaks at 60-90ds then decline to amoderate
constant level
1-For the 1
st
6-8w of pregnancy it maintains
the corpus luteum to ensure continued
progesterone out put until production shifts to
the placenta
2-regulate steroid biosynthesis in the placenta
& fetal adrenal gland &stimulates the fetal
testicle to secrete testosterone .

• Human placental lactogen (HPL)
It is protein produced by syncytotrophoblas.
It’s level rise slowly up to 40 weeks of
pregnancy.
It decreases maternal insulin sensitivity & promotes
release of FFA from maternal stores
– alternative
source of energy for her metabolism
.
HPL level is low in case of;
threatened
abortion & IUGR
3
It is steroid produced by feto-placental units
from
fetal liver , adrenals and placental
cytotrophoblast.
.
The level increase in early
pregnancy up to 38 weeks then after it
decrease. It originates from corpus luteum in
early pregnancy then from the placenta. Estriol
is the most abundant form in pregnancy & can
be used as indicator for placental function
sudden decline of esteriol in maternal
circulation indicate fetal compromise.
. Oestrogen

4
• Progesterone:
It is steroid produced by CL in 1
st
6-7w of
pregnancy thereafter by placental
syncytiotrophoblast ( no fetal role ).
The level of progesterone increase in the
pregnancy from early stage until the onset
of labour.
It is important for support of pregnancy and
increased vascularity of the placental bed.It
prevents uterine contraction &play acentral
role in maintaining uterine quiescence
throught pregnancy.

Amniotic fluid
It surrounds the fetus, produced by:
1- In early pregnancy secreted by amnion ,but
by 10
th
w it is mainly atransudate of fetal
serum via the skin & umbilical cord .
2- From 16w the net increase in AF is through a
small imbalance between urine & lung fluids
secretion & removal by fetal swallowing.
It’s volume increases progressively(10w:30ml,
20w:300ml,38w:1000ml) but from term there
is rapid fall in volume(40w:800ml,42w:350ml)
It
t

Function of amniotic fluid
.
1-It protect fetus mechanical injury
2-Allows room for fetal growth, movement
&development while preventing limb contracture
3-Is of value for assessing fetal well being e.g in
renal agenesis, cystic kidneys or fetal growth
restriction oligohydramnios results but when
there is reduced removal of fluid in conditions like
anencephaly & esophageal/ duodenal artesia
polyhydramnios results.
4-Permits fetal lung development as there is two-
way movement of fluide into the fetal bronchioles
& its absence in 2
nd
trimester is associated with
pulmonary hypoplasia.
It
t
Fetal Circulation

Umbilical cord
At term about 50 cm long 2 cm in diameter,
contain :
2 umbilical arteries: return non-oxygenated
blood, fetal waste, CO2 to placenta
1umbilical vein: brings oxygenated blood and
nutrients to the fetus
There is no nerve in cord or placenta .The
arteries are spiral and give a cord-like shape.
The vessels are packed and protected by a
viscous fluid which is Wharton Jelly.
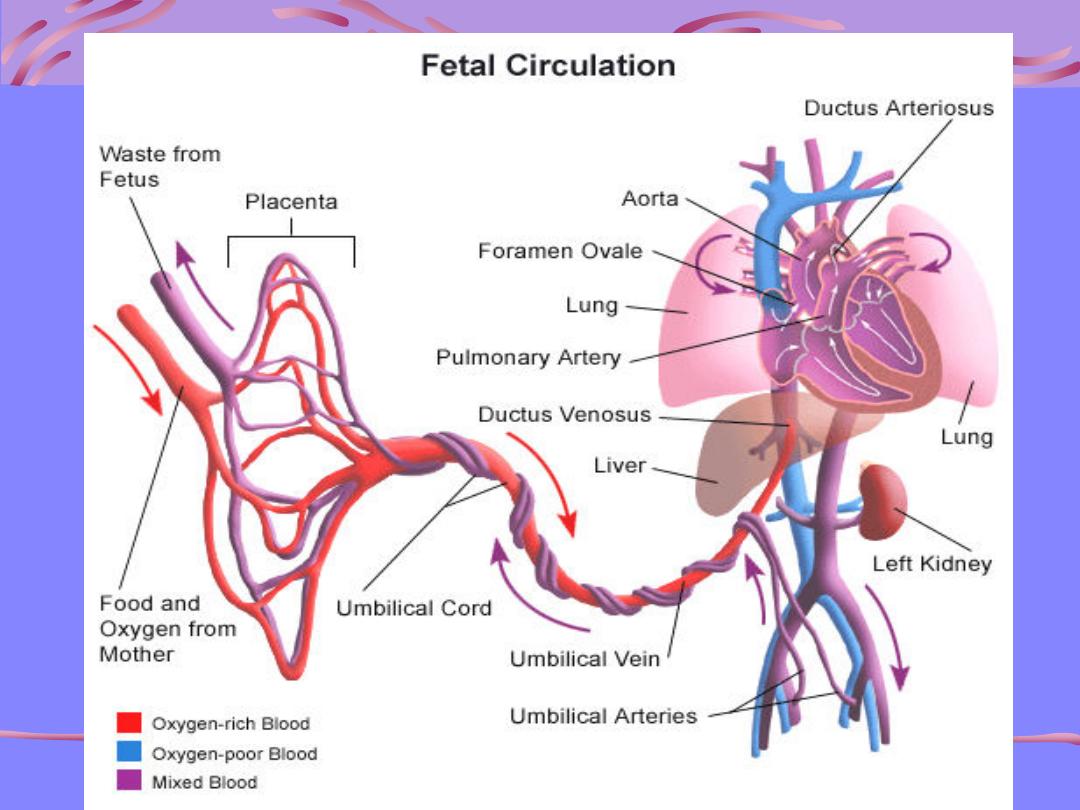
Shunts in fetal circulation
The fetal circulation is quite different from
that of adult & characterized by 4 shunts
which ensure that the best oxygenated
blood from the placenta is delivered to the
fetal brain thses are:
Umblical circulation.
Ductus venosus
Foramen ovale
Ductus arteriosus
Anatomy and Physiology
The umblical arteries arise from the
caudal end of the dorsal aorta & carry
deoxygenated blood from fetus to
placenta for gas & nutrient exchange. .
Oxygenated blood is returned to the fetus
via the umbilical vein to the fetal liver.
Fetal Circulation
Small amount of blood routed to growing liver
But the bulk passes through the ductus
venosis to by pass the liver & joins the
inferior vena cava as it enters the Rt
atrium.
Ductus Venosis is a narrow vessel & high blood
velocities are generated within it .This
streaming of blood together with the crista
dividens in Rt atrium prevents mixing of
oxygenated Bd from ductus venosus with
desaturated Bd from IVC.
Fetal Circulation
IVC empties into the right atrium of
the heart
The ductus venosus stream then passes to the
left atrium through the foramen ovale
(
Small physiological defect in the atrial septum)
Completely bypasses the non-functioning
lungs
Fetal Circulation
Blood continues journey to the left ventricle blood
is then pumped into the aorta
About 50% of blood is circulated to the upper
extremities
The remainder passes down the aorta to mix with
Bd of reduced oxygen saturation from Rt ventricle
via the ductous arteriosus
Deoxygenated Bd returning from the head & lower
body flows to the Rt atrium
Fetal Circulation
From the right atrium, the blood goes
to the right ventricle then to the
pulmonary arteries
Pulmonary arteries
Small amount goes to the maturing lungs
Rest of blood is shunted away from
lungs by ductous arteriosus back to
descending aorta
Fetal Circulation
By this means the desaturated blood from Rt Vt
passes down the aorta to enter the two
umbilical arteries to the placenta for re-
oxygenation.
Prior to birth, the ductus arteriosus remains
patent due to the production of PG E2&
prostacyclin , which act as vasodilators & its
premature closure has been reported with the
administration of cyclooxygenase inhibitors.
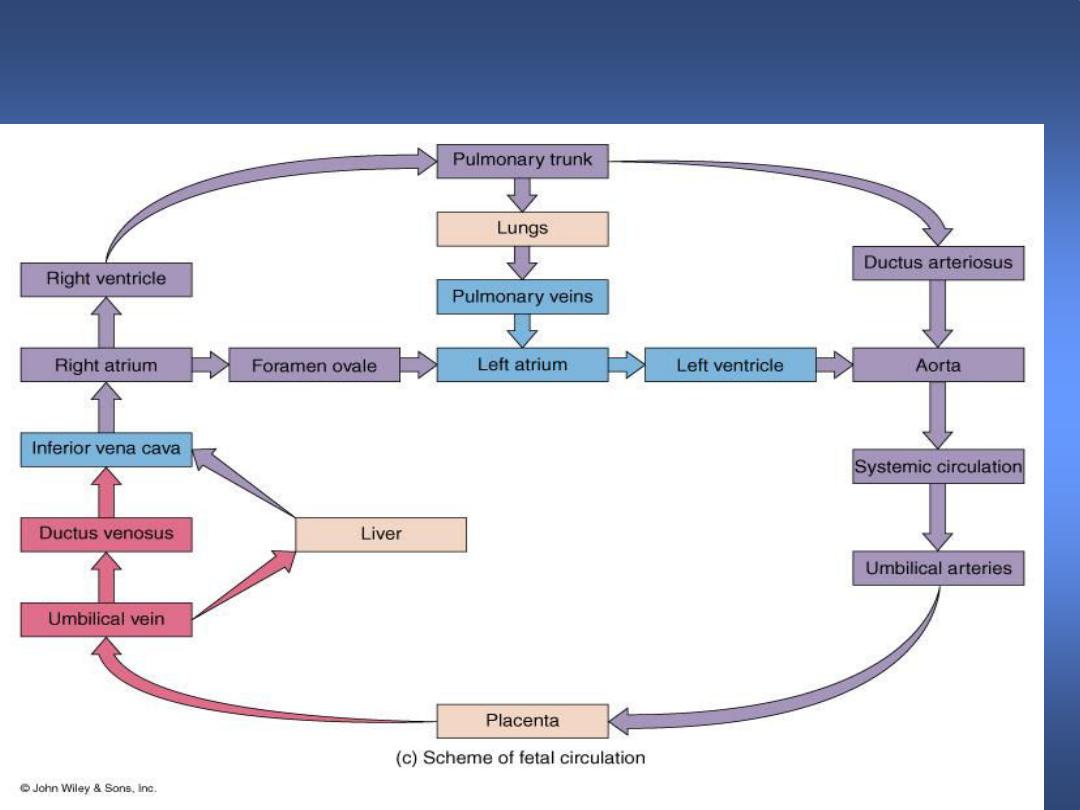
Flow Chart of Fetal Circulation
Conversion of Fetal to Infant
Circulation
At birth
Clamping the cord shuts down low-pressure
system & causes cessation of flow in ductus
venosus , a fall in pressure in the Rt atrium
&closure of foramen ovale.
Ventilation of the lungs opens the pulmonary
circulation , with a rapid fall in pulmonary
vascular resistance.

Conversion: Fetal to Infant
Circulation
With the 1
st
breath more heavily oxygenated blood
passing through the ductus arteriosus with the fall
in pulmonary vascular resistance, causes it’s
constriction & functional closure within a few days
of birth.
Occasionally, this transition from fetal to adult
circulation is delayed (persistent fetal circulation
commonly premature infants ), resulting in Lt-to-Rt
shunting of blood from the aorta through the
ductus arteriosus to the lungs & pulmonary
congestion .
Conversion (cont)
What happens to these special
structures after birth?
Umbilical arteries atrophy and become
fibrous ligaments
Umbilical vein becomes part of the fibrous
support ligament for the liver
The foramen ovale is closed by fibrous
structure

Post natal changes
Gas exchange function is transferred
from placenta to the lungs.
Separation of systemic and pulmonary
circulations
Increased metabolism to maintain body
temperature and hence increased
cardiac output.
Change from right to left shunting to
left to right blood flow
Fetal vs. Infant Circulation
Fetal
Low pressure system
Right to left shunting
Lungs non-functional
Increased pulmonary
resistance
Decreased systemic
resistance
Infant
High pressure system
Left to right blood flow
Lungs functional
Decreased pulmonary
resistance
Increased systemic
resistance
