
Pre conceptional
counselling
and
Antenatal care
(ANC)
• Is a meeting with a health care professional (generally
obstetrician) by a woman before attempting to become
pregnant. It generally includes preconception risk
assessment for any potential complication of pregnancy
as well as modification of risk factors.
• It is recommended that the woman should visit the
physician 3- 6 months before attempt to conceive to
prepare her body for successful pregnancy.
Pre-conceptional care
1.Medical history:
DM:-
• Optimize glycemic control to
decrease risk of miscarriage
and congenital anomaly.
• Treat nephropathy &
retinopathy.
• Folic acid supplementation
5mg daily \3months.
• HbA1C less than 6.5%
HT:-
• Assess RFT.
• Change ACEIs &
thiazide diuretic to
methyldopa or Ca
channal blocker.

Epilepsy:-
• Risk of congenital anomaly in offspring of epileptic
mother is 2-3 times higher than general population, so
optimize control, avoid multiple agent.
• Folic acid supplementation.
• If no seizure for 2 years perform EEG than withdraw
drug over 3 mon, with involvement of neurologist.
Thrombo embolism:- test for thrombophilia, if pt on
warfarin change to heparin.

Asthma:- optimize control, fewer medication &
offer influenza vaccine.
Cardiac disease:-counsel pt about morbidity and
mortality during pregnancy , involvement of
cardiologist.
Depression & anxiety:-avoid benzodiazepine cause
cleft lip& withdrawal symptoms in neonate.
2.Gyaenecological &reproductive hx:
• if irregular cycle investigate for PCOS & treat.
• hx of PTL, IUGR, PE high RR assess before
pregnancy.
• hx of PID test for tubal patency.
• hx of EP advice pt to see Dr as soon as she
believe that she is pregnant.

3. Livinng environment
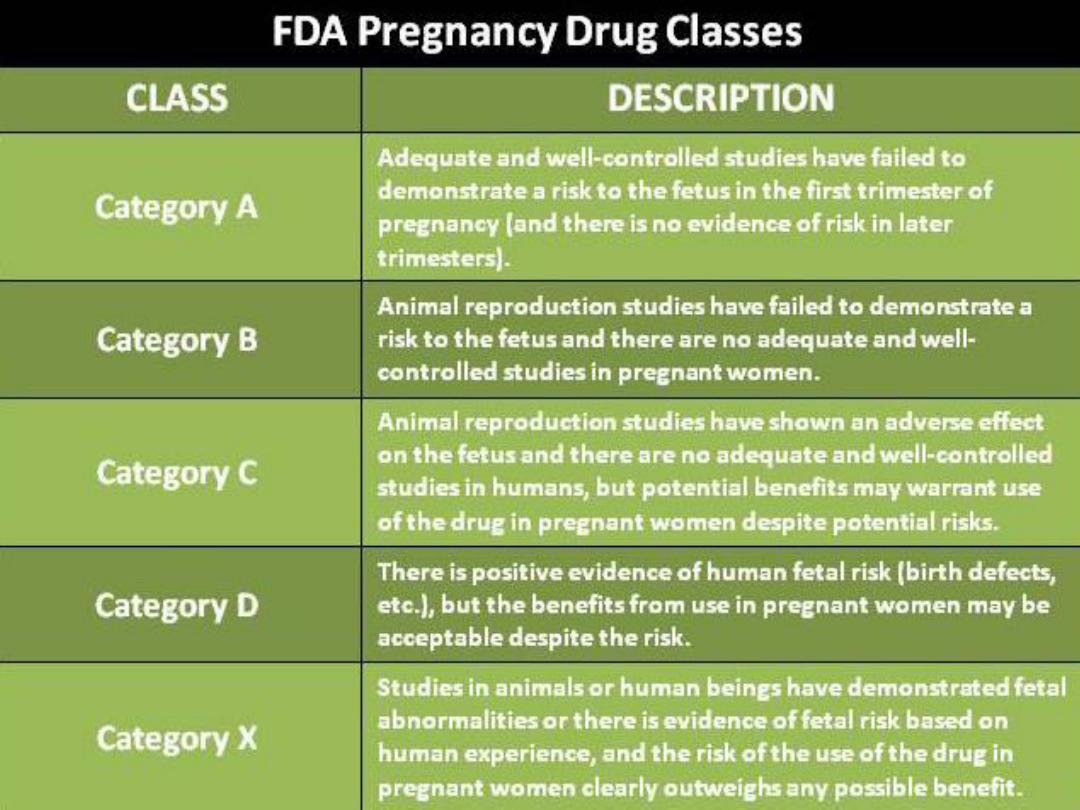
Drugs:- are classify to A,B,C,D,X, x should never taken
when trying to conceive or in pregnancy e.g folic
acid antagonist, avoid vit A more than 5000 IU daily.
Smoking:- stop bf pregnancy because increase risk of
EP, PTL& placental abruption.
Folic acid 3 months bf conception &continue during
1
st
trimester.

Diet ----women trying to conceive should have diet
rich in iron, vit.B, Ca.
Caffeine----high intake increase risk of miscarriage
(2 cup coffee &6 glasses of cola).
Fish ----large fish contain excessive amount of
mercury that harm the developing fetus.
Weight---both extreme of wt decrease fertility, try
to reach optimal BMI bf pregnancy(20-25)kg\m2.

Exercise: avoid vigorous exercise to avoid increase
in core temperature because hyperthermia
associated with NTD , also avoid long time spent
in hot tubs.
4. Fetility review: assess regular cycle & ovulation,
discuss fertility after contraception. Ovulation
occure 2 wk after pills , seek medical care if
regular cycle not occur 2-3 m after pill, review
frequency &timing of intercourse
5.Medical examination & testing:
a-full medical examination for breast & abdomen,
gynaecological hx &ex including pap smear and if
mammography is indicated best time is bf pregnancy.
b-screen for infectious disease: HIV(both
partners),syphilis(both),GC & chlamydia
(both),hepatitis B Ag & Ab, test immunity for rubella,
Test for toxoplasma& CMV. Dental & gum disease
increase the risk of PTL, so should be treated bf
pregnancy & during pregnancy to improve out come

Antenatal care
Aims of ANC
To prevent, detect & manage those factors
adversely affecting the health of mother and baby.
To provide advice, reassurance, education and
support for women &her family.
To deal with minor problems of pregnancy.
To provide general health screening.
• Booking visit: is the 1
st
ANC visit during which
history, examination & of investigation are
performed to provide appropriate care and to
determine whether risk factors are present or
not which require specialize care.
1
st
step in booking is confirmation of pregnancy:
by symptoms of pregnancy e.g amenorrhea,
breast tenderness, nausea.

2
nd
step is dating the pregnancy:-
Dating by LMP: the EDD is calculated by taking
date of LMP, counting forward by 9 months
&adding 7 days provided cycle is regular.
Dating by US: dating by US is more accurate
especially if there is menstrual irregularity, so
all women should offer US between 10-14
weeks.

Benefits of dating US
1.Accurate dating in women with irregular cycle or poor
recollection of LMP.
2. Reduce incidence of induction of labour for prolonged
pregnancy.
3.Maximizing potential for serum screening to detect fetal
abnormalities.
4. Early diagnosis of multiple pregnancy.
5. Detection of asymptomatic failed IUP.
Booking history;
• past medical hx
• past surgical hx
• Obstetric hx
• gynaecological hx
• family &social hx
• Age and race must be mentioned in booking
visit (advance mat. age is a risk factor for
chromosomal abnormality, thalasaemia
occur in certain ethnic group)
The booking examination:
1. Accurate measurement of blood pressure.
2. Abdominal examination to detect size of uterus.
3. Detection of abnormal scar indicative of previous
surgery.
4. Measurement of Ht & Wt to calculate BMI, women
with low BMI at risk of IUGR, while obese women
at risk of GDM,PE. The approximate weight gain
during pregnancy is 12 kg. 2kg in the first 20 weeks
and 10 kg in the remaining 20 weeks (1.5-2 kg per
months until term). Height of over 150 cm
indication of an average-sized pelvis
Booking investigation
1. FBC : as screen for anaemia & TCP.
2. Blood group & red blood cell antibody: if RH
–ve
prophylactic dose given as single dose at 28 wk
or in divided doses at 28 & 34 wk, or given after
sensitizing events e.g threartened miscarriage,
APH, & delivery of baby will require additional
anti
–D.

3.Urine analysis : MSU should be examine in
early pregnancy to detect asymptomatic
bacteriuria.
4.Rubella : rubella infection in 1
st
TMS cause
serious congenital abnormalities, so if there is
no previous hx of rubella infection ,should be
advised to avoid contact with infected person
&to undergo rubella immunization after
current pregnancy to protect future
pregnancies

5.Hepatitis B: HBsAg +ve indicate recent infection or
carrier state, if HBsAB +ve indicate previous
infection or immunization. Immunization for baby
after birth by Ig & vaccine decrease rate of
infection.
6.HIV.
7.Syphilis : transmission to fetus cause serious
anomalies which can be prevented by simple
antibiotic treatment.
8. Hb studies; in high risk women screened for
haemoglobinopathy.
Screening for fetal anomaly
1. Screening for down s syndrome: nuchal
translucency at 11-14 wk, serum biochemistry at
15-20 wk.
2. screening for NTD e.g spina bifida & anencephaly:
by maternal serum alpha feto protein at 15-20 wk,
detailed anomaly scan at 18-20 wk.
3. Screening for congenital structural anomalies : by
US 18-20 wk
Screening for clinical conditions:
1.Gestational diabetes; all women should be assessed
for risk factors for GDM at booking visit, if risk
factors are present ,women should be offered 2hr
75 g OGTT at 24-28 wk.
A previous hx of GDM should prompt OGTT at 16-18
wk ,if results are normal, test should be repeated at
24-28 wk.
Risk factors for GDM: BMI more than 30 kg/m2,
Previous baby weighing 4.5 kg or more, Previous
GDM, 1
ST
Degree relative with DM.

2. pre-eclampsia : all women should be screened for
PE at each visit by BP measurement and testing for
protein in urine , if risk factor for PE identified at
booking visit, extra visits should be arranged.
3. preterm labour:- Women with hx of PTL should
offer screening for bacterial vaginosis, UTI,
&cervical length by US.
4. Fetal growth & wellbing: SFH should be checked at
each visit from 24 wk. Listen to FH at each visit in
2
nd
& 3
rd
TMS by pinard stethoscope or Doppler US.
No need for growth scan in absence of risk factors.
Follow
–up visit:
Subsequent visits have been scheduled at intervals
of 4 weeks until 28 weeks, then every 2 weeks
until 36 weeks, and weekly thereafter. Women
with complicated pregnancies require return
visits at 1-2 week intervals.
at each visit from 20 wk: BP & protein in urine,
SFH.
at 36 wk: fetal presentation & engagement.
at 28 wk anti D for Rh
–ve women a single dose or
in divided doses at 28 & 34 wk
Work
– A woman with an uncomplicated
pregnancy who is employed, may continue to
work without interruption until the onset of
labor.
Postpartum, the patient may resume working 4-
6weeks after an uncomplicated delivery.
Working during pregnancy should be limited or
contraindicated in:
• Vaginal bleeding
• Short (<3 cm) or dilated cervix before
36 weeks gestation
• Uterine malformation
• Pregnancy-induced hypertension
• Fetal growth restriction
• Multiple gestation
• Prior history of preterm birth
• Polyhydramnios
• maternal medical disorders that are associated
with impaired placental perfusion
