Dr. Nawal Pediatric
1
Acute infectious URT obstruction
Stridor, a rasping sound heard predominantly on inspiration
Hoarseness (inflammation of the vocal cords)
A barking cough like a sea lion
A variable degree of dyspnoea
Croup (Laryngotracheobronchitis)
Etiology & Epidemiology
• Para influenza virus commonest
• Other viruses
• Age 3mon.-5years.
• Higher in boys.
• Common in late fall& winter.
• Recurrence frequent 3-6y.
Clinical Manifestations
• URTI 1–3 days
• barking cough, hoarseness, inspiratory stridor.
• low-grade fever temp. ; some children are afebrile.
• characteristically worse at night .
• Agitation and crying aggravate the symptoms.
• The child prefer to sit up in bed or be held upright.
Dr. Nawal Pediatric
2
Physical Examination
• hoarse voice, coryza.
• normal to moderately inflamed pharynx.
• Rarely, progresses to an increasing respiratory rate; dyspnea; and continuous stridor.
• Hypoxia and low oxygen saturation are seen only when complete airway obstruction is imminent.
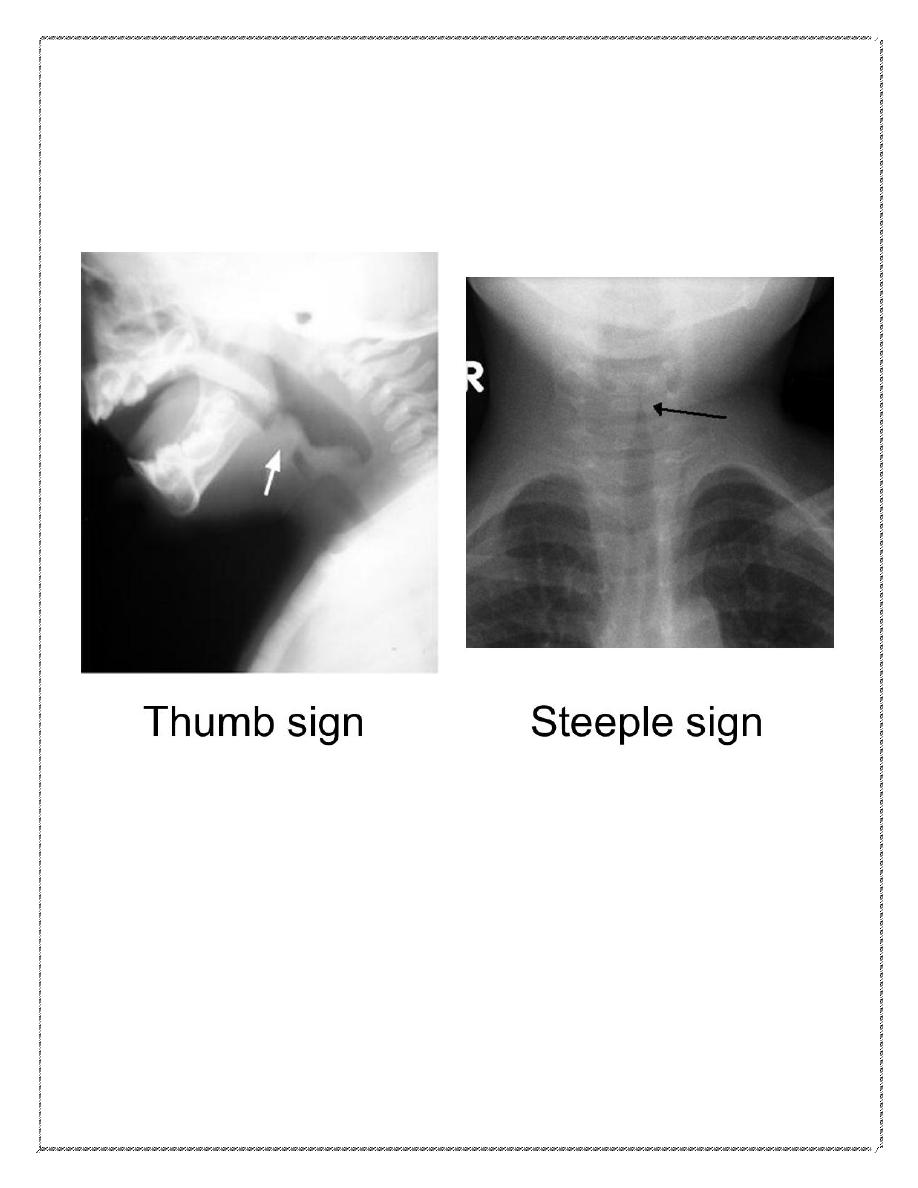
Radiographs of the neck may show subglottic narrowing or “steeple sign”.
considered only:-
o after airway stabilization in children who have an atypical presentation or clinical course.
o Distinguish between severe laryngotracheobronchitis and epiglottitis.
Acute Epiglottitis (Supraglottitis)
Etiology& Epidemiology
H.influenza type b in prevaccine era, age 2-4y.
Strep.pyogen, strep.pneumoniae, staph. In vaccinated child
Clinical Features
• Dramatic, potentially lethal condition .
• High fever, sore throat, dyspnea, and rapidly progressing respiratory obstruction.
• Appears toxic, swallowing is difficult.
• Breathing is labored.
• Drooling , the neck is hyperextended.
• Tripod position
• rapidly increasing cyanosis and coma.
Dr. Nawal Pediatric
3
• Stridor is a late finding and suggests near- complete airway obstruction.
• The diagnosis requires visualization of a large, “cherry red” swollen epiglottis by laryngoscopy,
(should be performed in an operating room or intensive care unit).
• Anxiety-provoking interventions ( phlebotomy, intravenous line placement, placing the child supine,
or direct inspection of the oral cavity) should be avoided until the airway is secure.
• Classic lateral radiographs show the “thumb sign”
• If the concern for epiglottitis still exists after the radiographs, direct visualization should be
performed
Acute Infectious Laryngitis
• Laryngitis is a common illness. Viruses cause most cases
Spasmodic Croup
• Occurs most often in children 1–3 yr
• Clinically similar to acute ltb ( history of a viral prodrome and fever in the patient and family are
frequently absent).
• The cause is viral in some cases, but allergic and psychologic factors could be.
Differential Diagnosis
1- Bacterial tracheitis
2- Diphtheritic croup
3- foreign body
4- A retropharyngeal or peritonsillar abscess
5- angioedema of the subglottic areas as part of anaphylaxis .
6- extrinsic compression of the airway (laryngeal web, vascular ring) and intraluminal obstruction from
masses (laryngeal papilloma, subglottic hemangioma); .
Dr. Nawal Pediatric
4
7- hypocalcemic tetany.
8- infectious mononucleosis, trauma, and tumors or malformations of the larynx.
Complications
viral croup 15% .
Infection of middle ear, terminal bronchioles, pulmonary parenchyma.
Bacterial tracheitis If associated with S. aureus, toxic shock syndrome may develop.
Epiglottitis:
Pneumonia, cervical lymphadenitis, otitis media, or, rarely, meningitis or septic arthritis.
Mediastinal emphysema and pneumothorax are the most common complications of tracheotomy
Treatment (croup)
1- Airway management.
• Mist has been traditionally used to treat croup.. There is no evidence to support the effectiveness
of mist therapy
• cold night air
2- Medications
A- Nebulized racemic epinephrine : decrease in the laryngeal mucosal edema. 0.25–0.75 mL of
2.25% racemic epinephrine in 3 mL of normal saline can be used as often as every 20 min..
The duration of activity of racemic pinephrine is <2 hr. Therefore, observation is mandated.
B- Oral or IM dexamethasone used a single dose of 0.6 mg/kg.
C- Nebulized budesonide.
D- A helium-oxygen mixture (Heliox) may be effective in children with severe croup who may
need intubation.
Dr. Nawal Pediatric
5
Indications of hospitalizations:
1. Progressive stridor.
2. Severe stridor at rest.
3. Respiratory distress.
4. Hypoxia, cyanosis, depressed mental status.
5. poor oral intake.
6. The need for reliable observation.
Epiglottitis
Is a medical emergency
1- artificial airway placed under controlled conditions, either in an operating room or intensive care
unit. Regardless of the degree of apparent respiratory distress, because lower mortality rate.
2- oxygen . .
3- cultures of blood, epiglottic surface, and, in selected cases, cerebrospinal fluid should be collected
after airway stabilization.
4- ceftriaxone, cefotaxime, or a combination of ampicillin and sulbactam should be given parenterally,
antibiotics should be continued for 7–10 days..
Chemoprophylaxis
Indications for rifampin prophylaxis (20 mg/kg orally once a day for 4 days; maximum dose, 600 mg) :
(1) any contact <48 mo of age who is incompletely immunized;
(2) any contact <12 mo who has not received the primary vaccination series;
(3) an immunocompromised child in the household
Dr. Nawal Pediatric
6
Prognosis
Untreated epiglottitis has a mortality rate of 6%. but if early diagnosis is made and appropriate treatment
is initiated the prognosis is excellent.
The outcome of acute LTB, laryngitis, and spasmodic croup is also excellent.
Arranged by: Mustafa Hürmüzlü
