
Investigations of Genitourinary
Disorders
Ahmed MH
A’zzaw, MD
CABMS(Urology)
Kirkuk University, College of Medicine,
Department of Surgery

Laboratory investigation
Urine analysis
• This is best performed on a mid-stream
specimen of urine. After cleansing the
external urethral meatus, the first 20 ml or so
of urine (containing bacteria and cells from
urethra) are discharged before collecting the
next part of the voided urine in a sterile
container.

Laboratory investigation cont.
…
Chemical tests
• "Dipstick" = a strip coated with chemicals for
measuring the urine pH and for detecting the
presence of glucose, protein or blood; bilirubin,
urobilinogen, ketones and nitrites can also be
detected.
The urine pH
• Varies between 4.5 and 8.0 Persistently alkaline urine
(pH > 8.0) suggest infection with urea-splitting
organism such as Proteus mirabilis

Laboratory investigation cont.
…
Protein
• The amount of protein in the urine is normally
less than 100 mg/24 h. Dipstick will only
detect levels greater than 300 mg/l Transient
proteinuria (e.g. UTI) or persistent
(glomerulopathia)
Glycosuria
• Usually diabetes mellitus, rarely renal
glycosuria

Laboratory investigation cont.
…
Microscopy
Microscopical examination of urine directly
of the urinary sediment studied after
centrifugation
• Red blood cells
• White blood cells
• Epithelial cells
• Casts - from glomerular disorders (hyaline or
cellular)
Laboratory investigation cont.
…
• Crystals - related to stone disease
• Bacteria - Gram stain should be performed; if
tuberculosis is suspected, the urinary
sediment should be stained using the Ziehl-
Nielsen methods
• Ova schistosomiasis

Laboratory investigation cont.
…
Culture
• The specimen should be plated out promptly
or refrigerated until processing to prevent
multiplication of bacteria after voiding.
• Significant infection is present if there are
more than 100 000 (= 10
5
) organism/ml ,
whilst counts less than 10 000 (=10
3
)/ml
suggest contamination.

Laboratory investigation cont.
…
• Antibiotic sensitiveness is determined using
culture plates with antibiotic discs that inhibit
the growth of susceptible organisms.
• If tuberculosis is suspected, three early
morning samples of urine (EMU) are taken
and
cultured on Lowenstein-Jensen medium
.

Laboratory investigation cont.
…
Blood tests
Renal function studies
• the plasma urea (normal range 2,3-6,9 mmol/l) and creatinine
(normal range 50-120 µmol/l)
• creatinine clearance (normally 100-140 ml/min) - closely
approximates to the glomerular filtration rate (GFR)
Haematology
• Anaemia - tumours, renal impairment
• White blood cell count - may raised in infections
• ESR - elevated in certain disorders, tumors, retroperitoneal
fibrosis
Other tests
• PSA - see BPH and prostate cancer

Diagnostic imaging
Plain abdominal X-ray (KUB)
• The KUB (a plain X-ray to include the kidneys,
ureters and bladder) is useful to detect:
- Radio-opaque urinary calculi (90% of calculi)
unless they overlie areas of the bony skeleton
- Soft tissue masses in the renal areas and pelvis
- Gallstones (10%)
- Pelvic phleboliths

Diagnostic imaging cont.
…
- Calcified lymph nodes
- Sclerotic deposits in prostate cancer
(osteoplastic metastases
- for other tumours are more typical osteolythic
metastases)
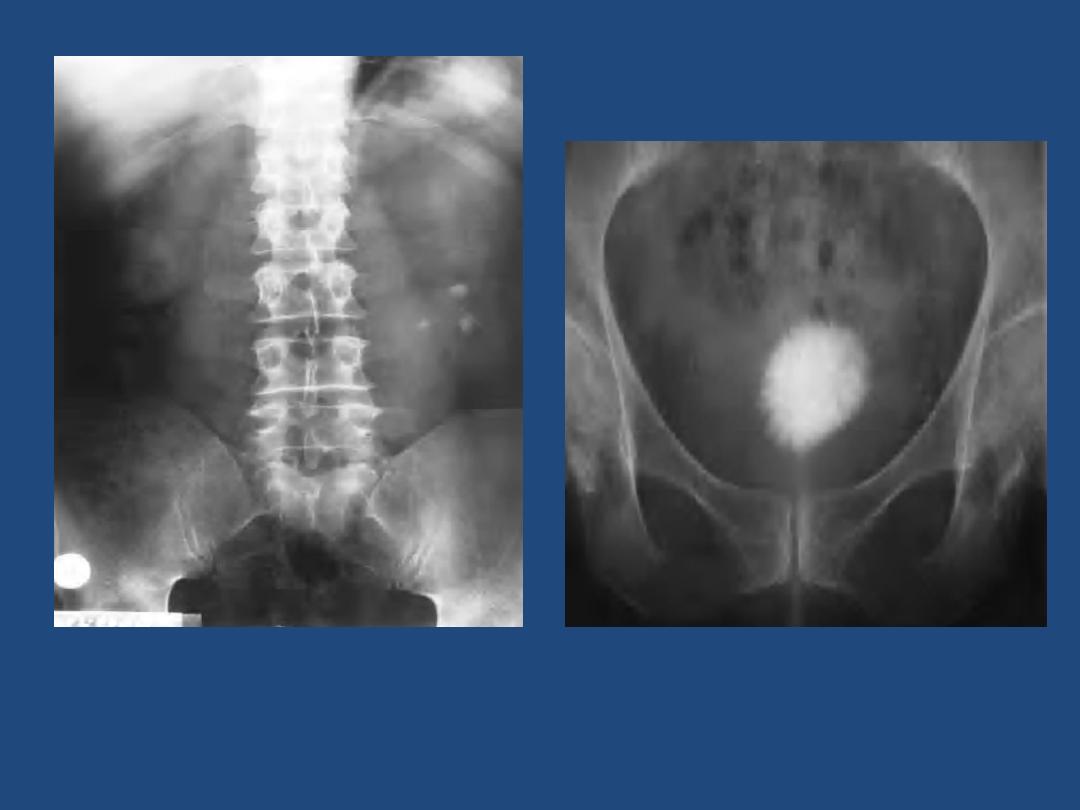
Fig. plain X-ray of pelvis with
cystolithiasis
Fig. plain X-ray with multiple left
nephrolithiasis

Diagnostic imaging cont.
…
Intravenous urography (IVU)
- After a plain film, iodine-containing contrast
medium is injected intravenously and serial
films are taken to follow its excretion by the
kidneys
- The nephrogram phase - on the initial film 1-3
minutes after injection, contrast medium is in
the glomeruli and proximal tubules so that a
clear image of the renal outline is obtained

Diagnostic imaging cont.
…
- The pyelogram phase - subsequent excretion of
contrast medium outlines the collecting
systems, renal pelvis, ureter and bladder,
showing any structural abnormalities or filling
defects
- The procedure may be complicated by allergic
reaction to the contrast medium, ranging in
severity from a mild urticarial rash to
anaphylactic shock .

Diagnostic imaging cont.
…
Ultrasound
- The most frequently used radiological
techniques in urological disorders
- Almost all urological out-patient department
are able to perform ultrasound immediately
after physical examination
- Colour-flow Doppler techniques - measuring
blood flow
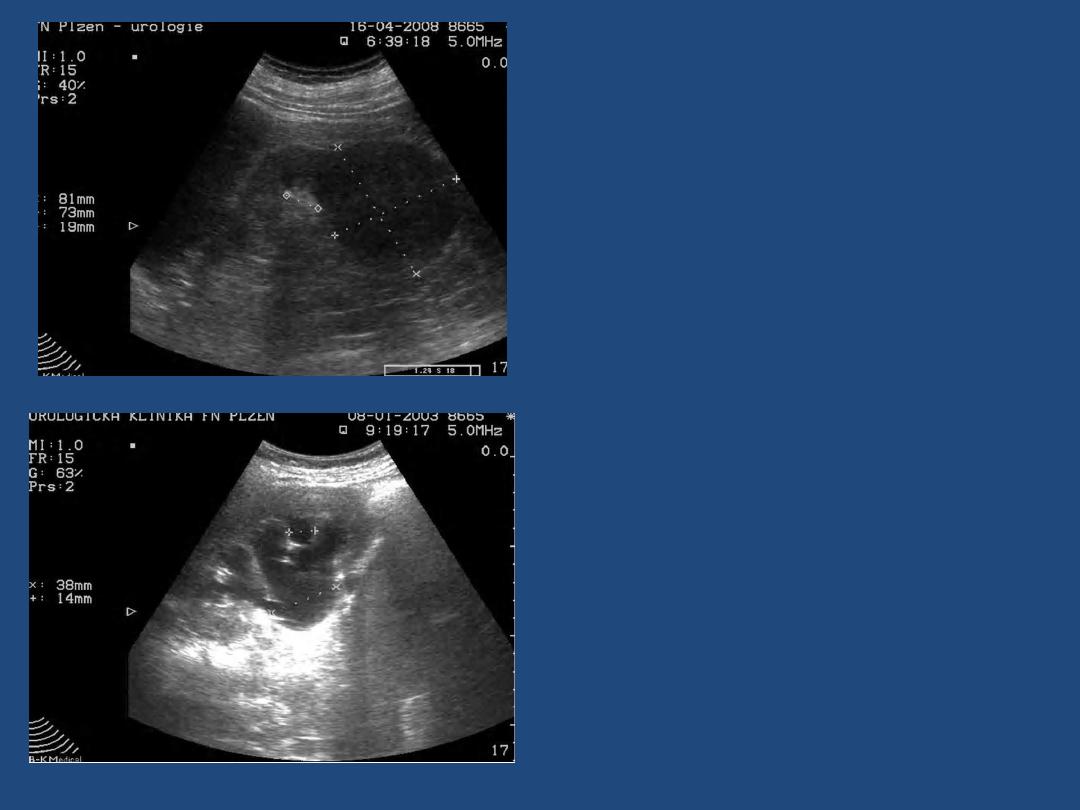
Fig. Ultrasonography of the kidney with
a tumour 81 x 73 mm (T2
)
Fig. Ultrasonography of the kidney with
hydronephrosis
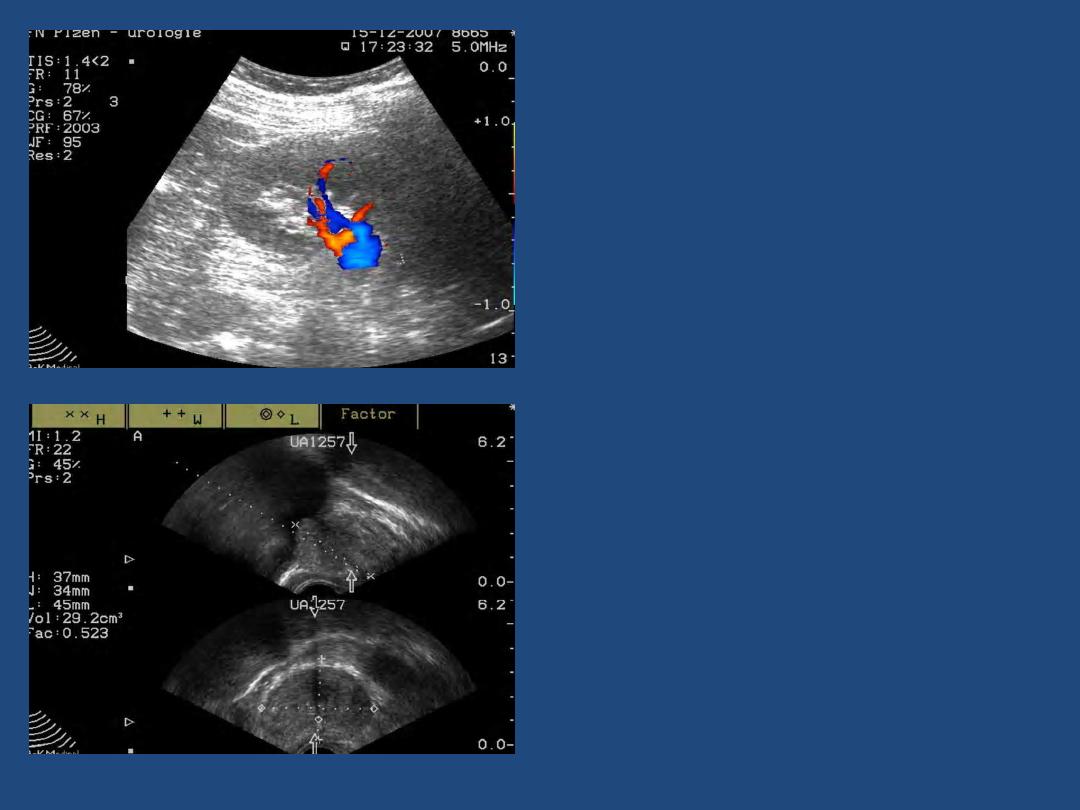
Fig. Transrectal ultrasonography of prostate in
two plains (sagittal and transversal)
Fig. Colour-flow Doppler of blood
supply of the kidney

Diagnostic imaging cont.
…
CT scanning (computed tomography)
- Multidetector Spiral CT
- It enables reconstructions in different planes
and biphasic CT angiography
PET/CT
- Combination of positive emission tomography
and CT.
- It allows precise localisation of tumours.
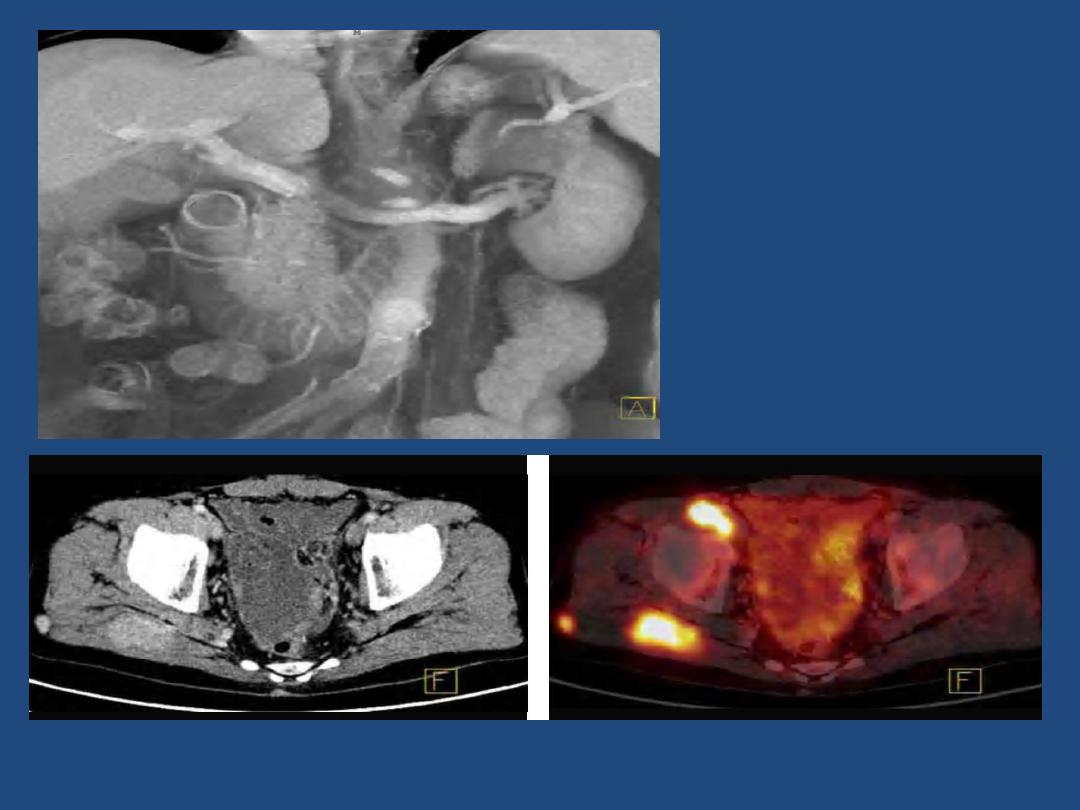
Fig. Biphasic CT angiography
of the left kidney.
Fig. PET/CT with metastases of kidney cancer to the soft tissue around the right hip joint.
Diagnostic imaging cont.
…
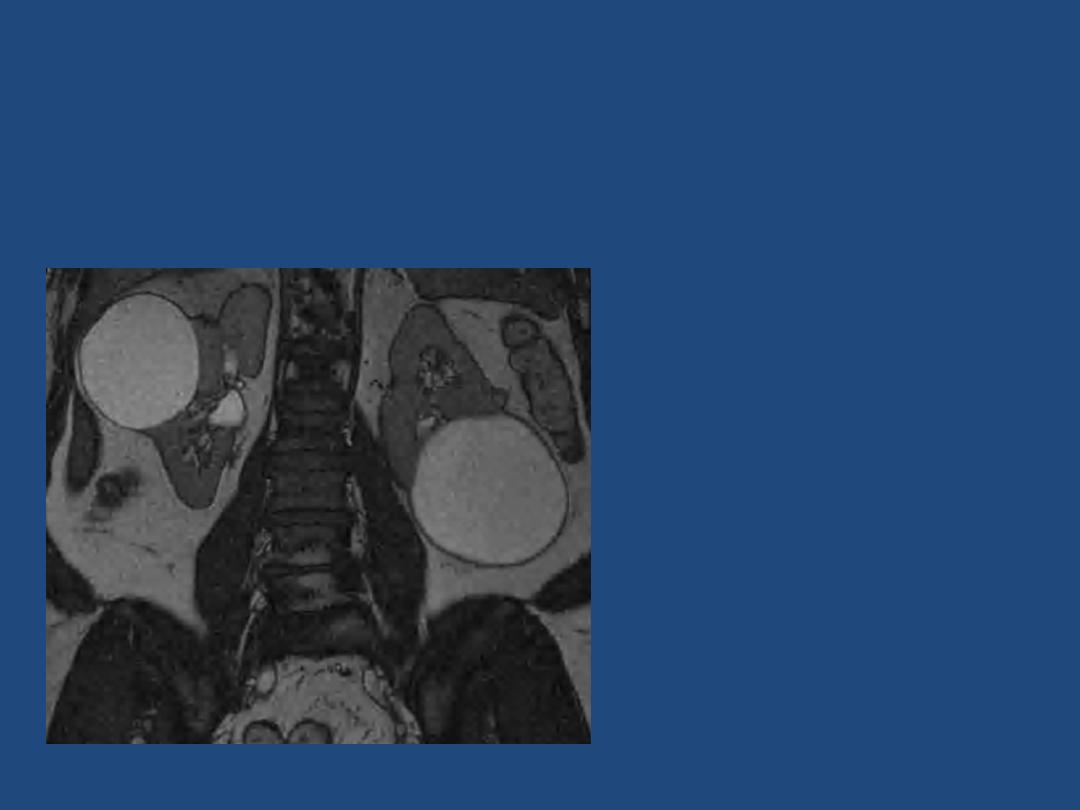
MRI (magnetic resonance imaging)
Fig. MRI Coronary Plain with Kidneys
with bilateral simple renal cyst

Diagnostic imaging cont.
…
Arteriography
- Renal arteriography is used in diagnosis of
renal vascular disorders, renal tumours and
renal trauma; therapeutic embolisation of the
renal artery can be performed at the same
time to control bleeding from the kidney.

Diagnostic imaging cont.
…
- Iliac arteriography is useful for assessing the
pelvic tumours or trauma, and therapeutic
embolisation of the internal iliac artery is
occasionally used for uncontrollable bladder
haemorrhage, pelvic trauma, and priapism.

Diagnostic imaging cont.
…
Other radiological techniques
Antegrade pyelogram
- contrast medium is injected via
a small-bore needle passed into the collecting
system under local anaesthetic or via a percutaneous
nephrostomy
Ascending ureterogram
- using a catheter inserted into
the ureteric orifice at cystoscopy
Urethrography (ascending and descending)
- contrast
medium is instilled directly into urethra (ascending
urethrography), contrast medium is passed out and is
performed with micturition

Diagnostic imaging cont.
…
Cystogram (it can demonstrate vesicourethral
reflux) and descending urethrography.
Urethrography is useful for diagnosis of
urethral stricture mainly.
Lymphography
- following injection of contrast
medium into a lymphatic in the foot is used to
demonstrate the iliac and para-aortic nodes in
pelvic malignancy; nowadays, it has been
replaced by CT scanning

Diagnostic imaging cont.
…
Radionuclide studies
• Renal scintigraphy
It is useful mainly for dynamic diagnosis - upper
urinary tract obstruction, assessing of renal
function of both kidneys.
• Bones scintigraphy
It is most widely used in the detection of bony
metastases from prostatic, bladder and renal
carcinoma.

Specialized Methods of
Urological Treatment
Ahmed MH
A’zzaw, MD
CABMS(Urology)
Kirkuk University, College of Medicine,
Department of Surgery

CATHETERISATION
• Catheters are used mainly therapeutically to
relieve urinary retention.
Types and sizes of catheters
Material :
- soft silicon coated latex (silicon is highly
resistant to incrustation) , it can be introduced
up to 4 weeks
- 100% silicon - it can be introduced up to 8
weeks (it is better, but more expensive)

CATHETERISATION cont.
…
Types of catheters :
1.
One way catheter
: for dilatation of urethral
stricture, to discover residual urine (better it is
performed by ultrasound), to introduce contrast
medium into the bladder
2.
Two way catheter
: self-retaining balloon catheter =
Foley catheter
3. Three way catheter
: for irrigation (lavage) of bladder
(by bleeding to bladder after prostatectomy, due to
bladder tumour)

CATHETERISATION cont.
…
Division by a tip of catheter :
Nelaton - straight round tip
Tiemann - curved pointed tip
Size of catheters :
French scale = Charrie scale = circumference in
mm diameter is size in F (Ch) divided by
( = 3.14) e.g. catheter 18 F has diameter 6 mm


CATHETERISATION cont.
…
• Indications of catheterization
– Diagnostic
– Therapeutic
• Contraindications
• Complications

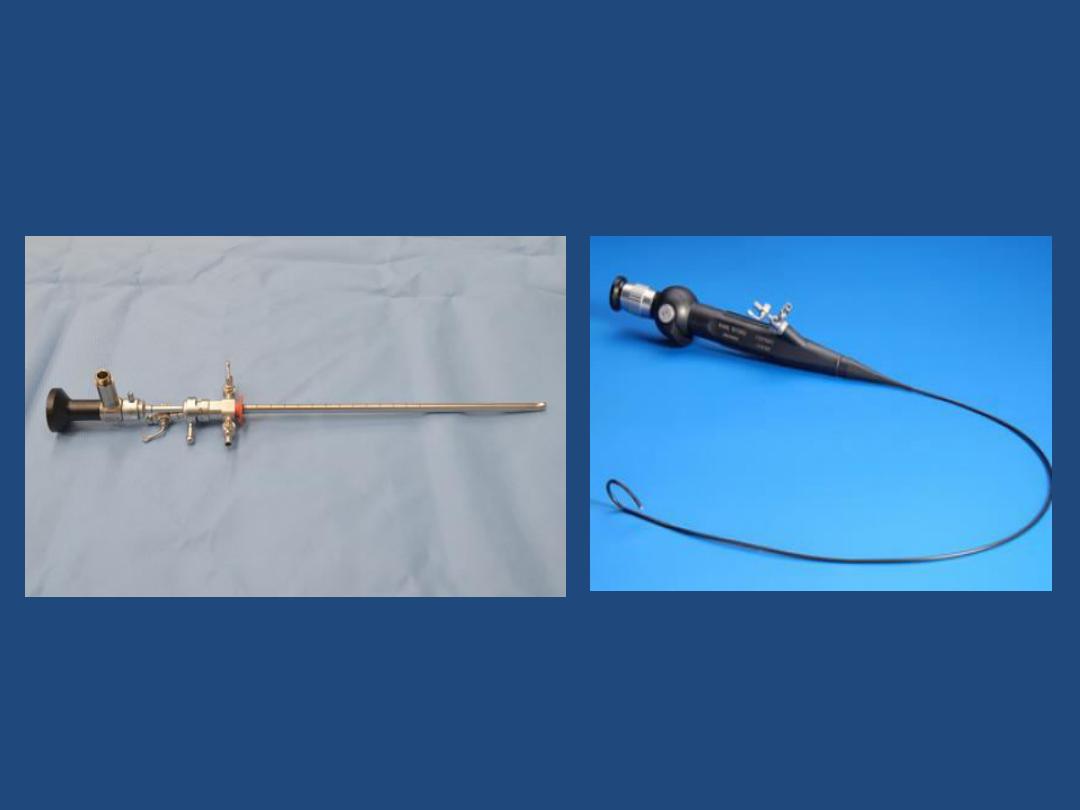
ENDOSCOPY
Two types of endoscopes:
1. rigid .
2. flexible
.
Examination is more difficult, an endoscope is
more expensive, through this endoscope can
be passed only flexible instruments, but for
patient is this flexible endoscopy more
pleasant

ENDOSCOPY
cont. …
• Panendoscopy :
Uretroscopy and cystoscopy =
endoscopy of urethra and urinary bladder
• Ureteroscopy :
Endoscopy of ureter
• Ureterorenoscopy :
Endoscopy of ureter and renal
pelvis too
Endoscopic operations
• Lithotripsy :
disintegration of stone in bladder and
ureter
• Transurethral resection
of prostate (TURP = TUPE)
and bladder tumour ( TURT )

ENDOSCOPY
cont. …
Nephroscopy
• It is used mainly for treatment of stones =
nephrolitholapaxy

Nephrostomy
To the dilated renal pelvis is introduced under
ultrasound and/or radiological control
catheter (= percutaneous nephrostomy).
Percutaneous nephrostomy step by step:
• Needle puncture of dilated renal pelvis under
X-ray or/and ultrasonography control
• Guide wire passed down needle Dilatation of
channel over guide wire
• "pig-tail" catheter inserted over guide wire
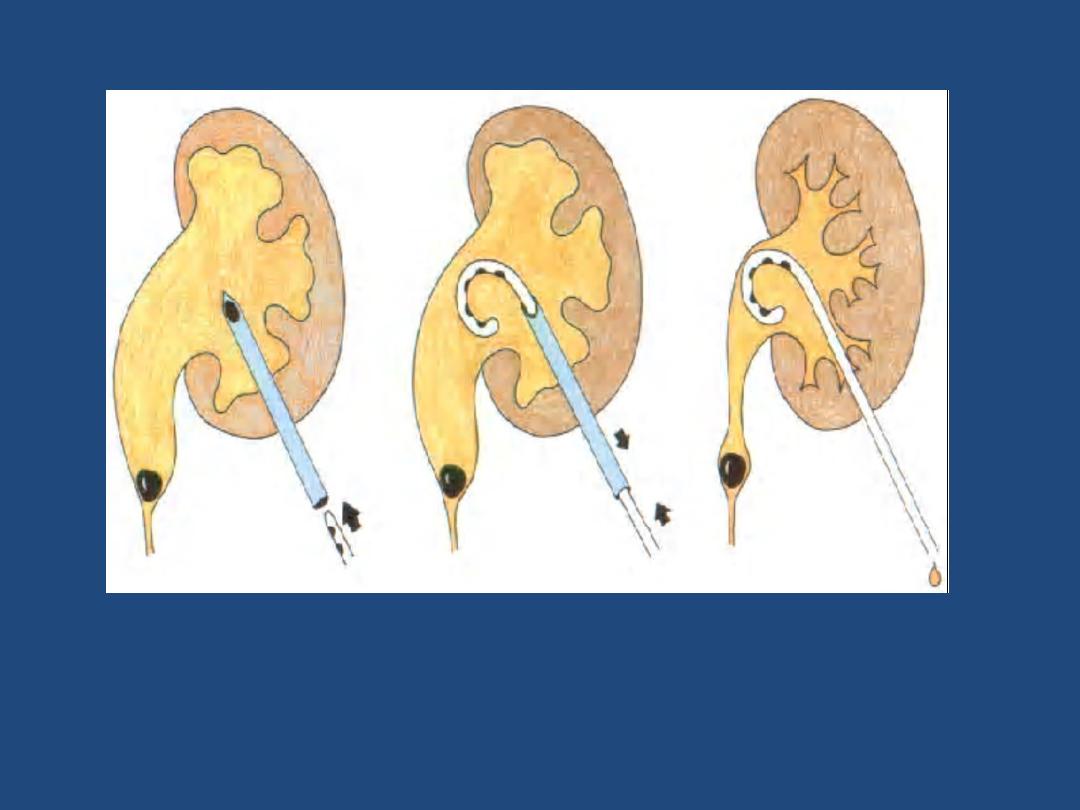
Fig. Scheme of introduction of percutaneous nephrostomy.

BIOPSY
Prostate biopsy
• Indication: suspicion on prostate cancer It is
performed transrectal (or transperineal) under
mainly ultrasound control
Biopsy of kidney
• It is done under ultrasonography or CT
control. Mainly used in nephrology, biopsy for
kidney tumour is indicated rarely.
