Esophagus
Dr. Nadim Nafie Ibrahim
Thoracic and Cardiovascular surgeon
F I B M S
Congenital anomalies
Congenital esophageal atrasia and
tracheo-esophageal fistula
Congenital esophageal stenosis
Duplication cyst
Congenital achalesia
Congenital short esophagus
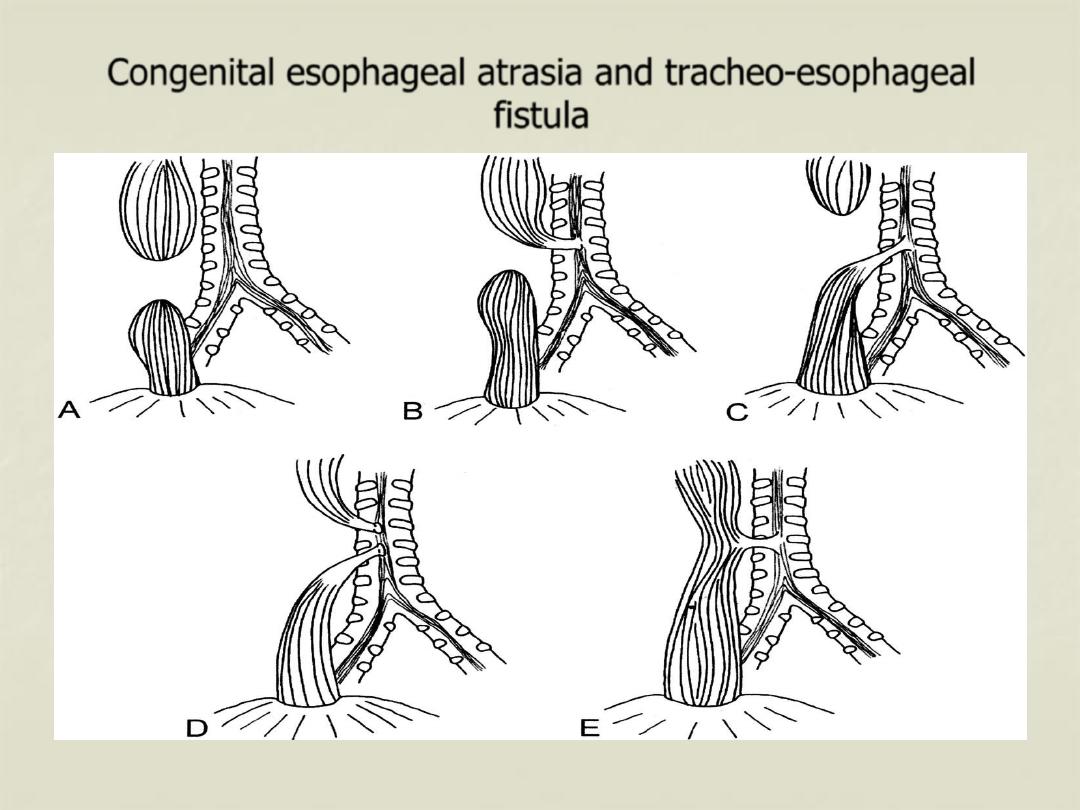
Congenital esophageal atrasia and tracheo-esophageal
fistula
Could be divided into five groups:
Group A: (8 %) esophageal atrasia without TE fistula, the upper esophagus ending
blindly and the lower esophagus beginning blindly with a considerable gab
between the two segments.
Group B: (1 %) esophageal atrasia with a fistula between the upper pouch and the
trachea, but the lower esophagus not communicating with the respiratory tract.
Group C: (87 %) this is the most common variety, esophageal atrasia, the upper pouch
being blind and the lower esophageal segment communicating with the
trachea.
Group D: (1 %) esophageal atrasia with both segments communicating with the trachea
by separate fistulae.
Group E: (4 %) TE fistula but without atrasia (so-called H fistula).
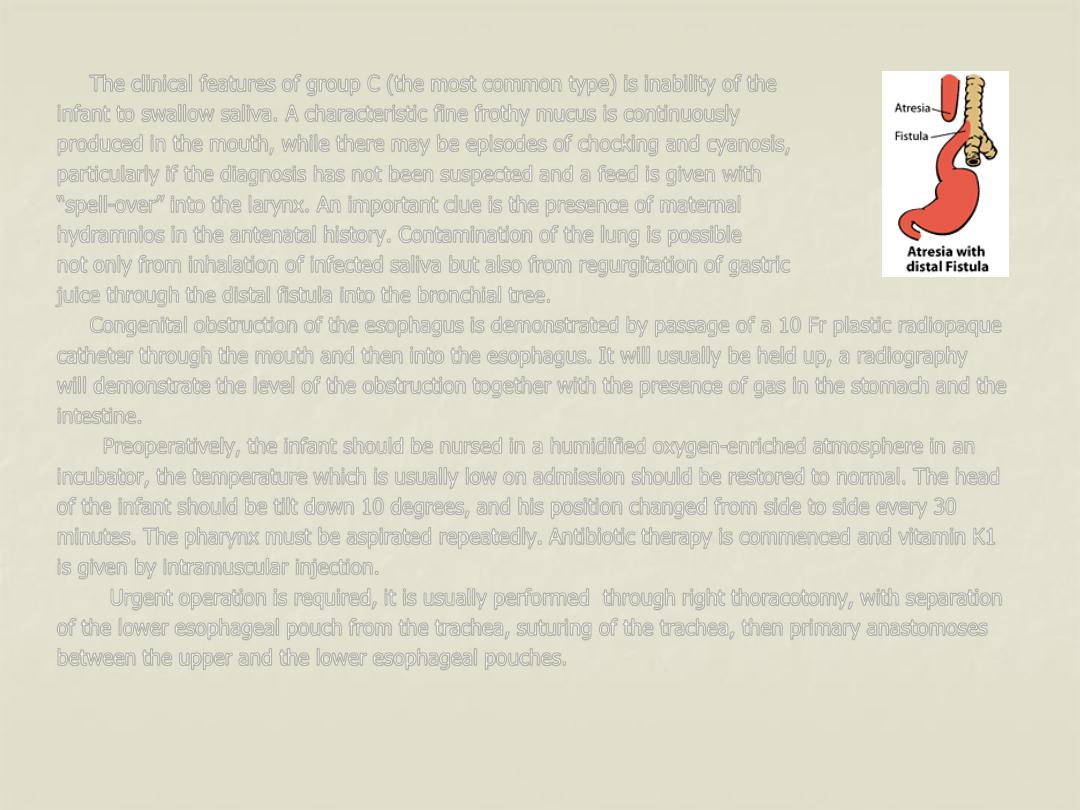
The clinical features of group C (the most common type) is inability of the
infant to swallow saliva. A characteristic fine frothy mucus is continuously
produced in the mouth, while there may be episodes of chocking and cyanosis,
particularly if the diagnosis has not been suspected and a feed is given with
“spell-over” into the larynx. An important clue is the presence of maternal
hydramnios in the antenatal history. Contamination of the lung is possible
not only from inhalation of infected saliva but also from regurgitation of gastric
juice through the distal fistula into the bronchial tree.
Congenital obstruction of the esophagus is demonstrated by passage of a 10 Fr plastic radiopaque
catheter through the mouth and then into the esophagus. It will usually be held up, a radiography
will demonstrate the level of the obstruction together with the presence of gas in the stomach and the
intestine.
Preoperatively, the infant should be nursed in a humidified oxygen-enriched atmosphere in an
incubator, the temperature which is usually low on admission should be restored to normal. The head
of the infant should be tilt down 10 degrees, and his position changed from side to side every 30
minutes. The pharynx must be aspirated repeatedly. Antibiotic therapy is commenced and vitamin K1
is given by intramuscular injection.
Urgent operation is required, it is usually performed through right thoracotomy, with separation
of the lower esophageal pouch from the trachea, suturing of the trachea, then primary anastomoses
between the upper and the lower esophageal pouches.
Surgical anatomy of the esophagus
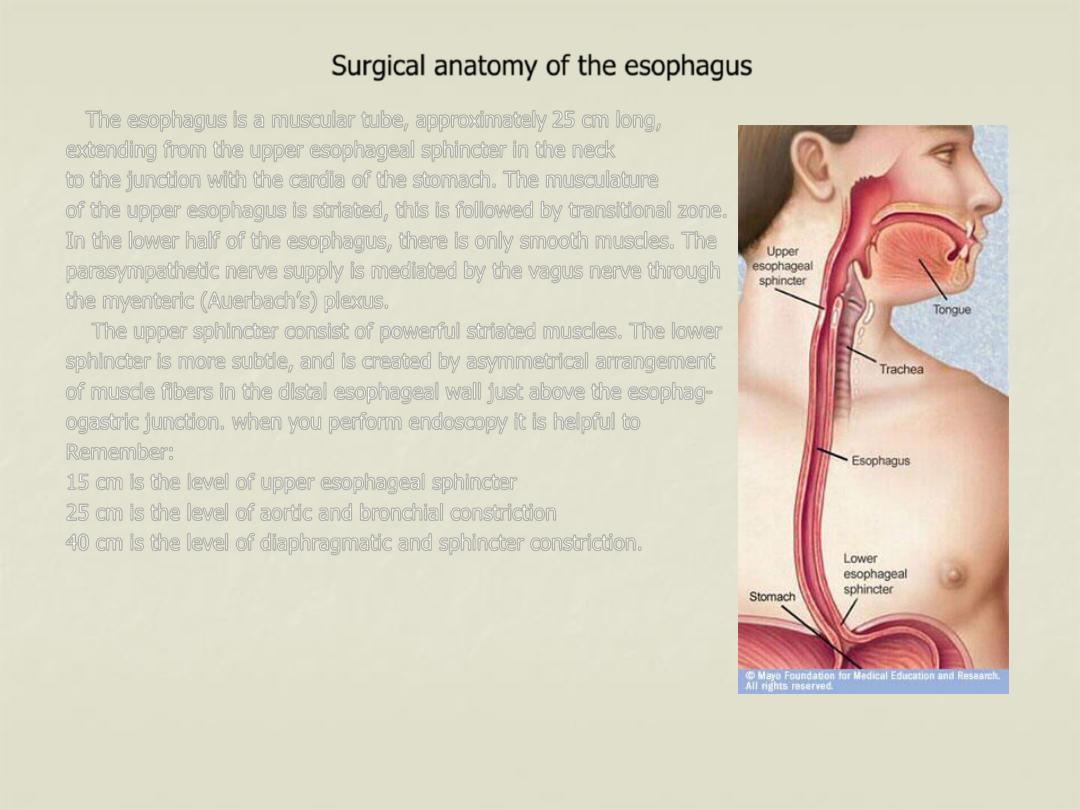
The esophagus is a muscular tube, approximately 25 cm long,
extending from the upper esophageal sphincter in the neck
to the junction with the cardia of the stomach. The musculature
of the upper esophagus is striated, this is followed by transitional zone.
In the lower half of the esophagus, there is only smooth muscles. The
parasympathetic nerve supply is mediated by the vagus nerve through
the myenteric (Auerbach’s) plexus.
The upper sphincter consist of powerful striated muscles. The lower
sphincter is more subtle, and is created by asymmetrical arrangement
of muscle fibers in the distal esophageal wall just above the esophag-
ogastric junction. when you perform endoscopy it is helpful to
Remember:
15 cm is the level of upper esophageal sphincter
25 cm is the level of aortic and bronchial constriction
40 cm is the level of diaphragmatic and sphincter constriction.
Physiology of the esophagus
The main function of the esophagus is to transfer food from the mouth to the stomach in a
coordinated fashion.
* The initial movement from the mouth is voluntary.
* The pharyngeal phase of swallowing involve sequential contraction of the oropharyngeal
musculature, closure of the nasal and respiratory passages, cessation of breathing and opening of
upper esophageal sphincter.
* The body of the esophagus propel the bolus through a relaxed lower esophageal sphincter (LES)
into the stomach, taking air with it. This coordinated esophageal wave is called primary
peristalsis. It is under vagal control (involuntary).
* The LES is a zone of relatively high pressure that prevents gastric contents from refluxing into the
lower esophagus. in addition to opening in response to primary peristaltic wave, the sphincter
also relaxes to allow air to escape from the stomach and at the time of vomiting. The normal LES
is 3-4 cm long and has pressure of 10-25 mm Hg.
* Secondary peristalsis is normal reflux response to a stubborn food bolus or refluxed materials,
designed to clear the esophagus by contraction that is not proceeded by conscious swallowing.
* Tertiary contractions are non-peristaltic waves that are infrequent (<10 %).
