Esophagus
Dr. Nadim Nafie Ibrahim
Thoracic and Cardiovascular surgeon
F I B M S
Gastro-esophageal reflux diseases
Aetiology
Normal competence of gastro-esophageal junction is maintained by LES. Failure of the LES is
caused by inadequate pressure, inadequate overall length, or abnormal position, i.e., the portion
exposed to positive-pressure environment of the abdomen. In normal circumstances, the LES relaxes
transiently as a coordinated part of swallowing, as a means of allowing vomiting to occur, and in
response to stretching of the gastric fundus, particularly after meal to allow swallowing air to be
vented. Most episodes of physiological reflux occur during postprandial transient lower esophageal
relaxations (TLESRs).
In early stages of GERD, most pathological reflux occur as a result of an increase number of
TLESRs rather than a persistent fall in overall sphincter pressure. In more sever GERD, LES pressure
tends to be generally low, and this loss of sphincter function seems to be made worse if there is loss
of an adequate length of intra-abdominal esophagus.
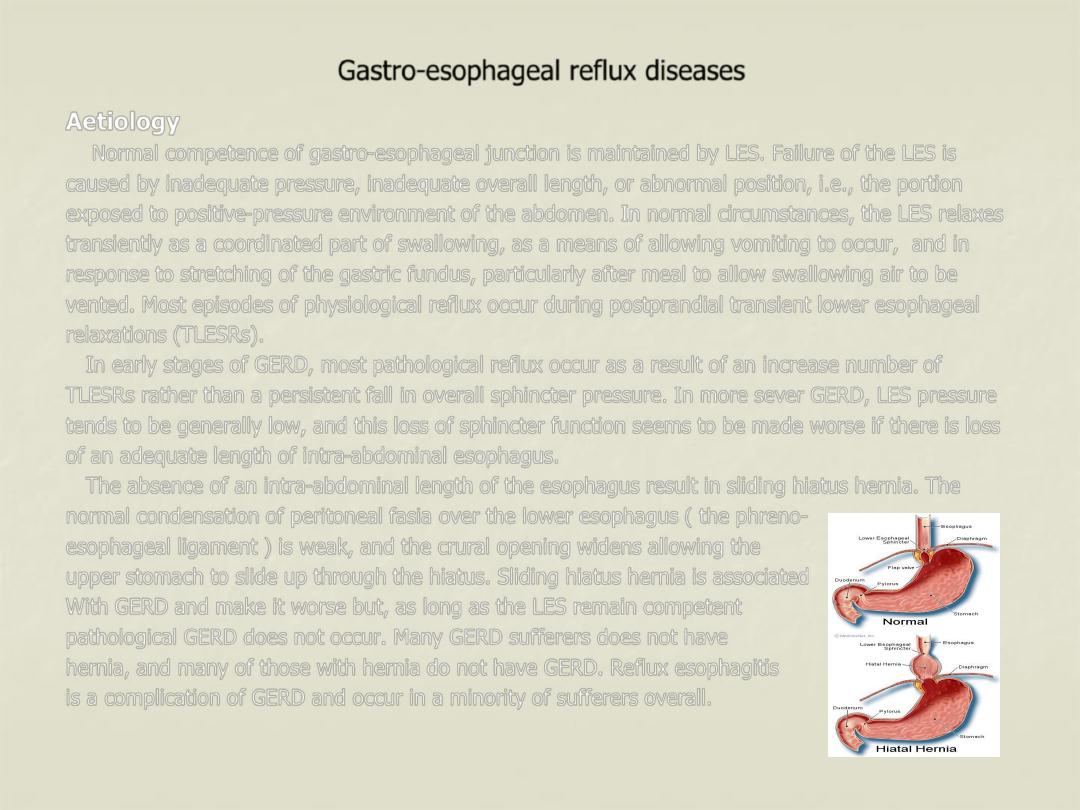
The absence of an intra-abdominal length of the esophagus result in sliding hiatus hernia. The
normal condensation of peritoneal fasia over the lower esophagus ( the phreno-
esophageal ligament ) is weak, and the crural opening widens allowing the
upper stomach to slide up through the hiatus. Sliding hiatus hernia is associated
With GERD and make it worse but, as long as the LES remain competent
pathological GERD does not occur. Many GERD sufferers does not have
hernia, and many of those with hernia do not have GERD. Reflux esophagitis
is a complication of GERD and occur in a minority of sufferers overall.
Clinical features
The classical triad of symptoms is retrosternal burning pain (heart burn), epigastric pain (some
time radiated through to the back) and regurgitation. Most patients do not experience all three.
Symptoms are often provoked by food, particularly those that delay gastric emptying (e.g. fats, spicy
foods). As the condition become more sever, gastric juice may reflux to the mouth and produce an
unpleasant taste often described as “acid’ or “bitter”. A proportion of patients have odynophagia with
hot beverages. Some patients present with less typical symptoms such as angina-like chest pain,
pulmonary or laryngeal symptoms.
Diagnosis
•
In most cases, the diagnosis is assumed rather than proven, and treatment is empirical.
•
Investigation is only required when: a- the diagnosis is in doubt, b- when the patient does not
response to proton pump inhibitor (PPI), c- if dysphagia is present.
•
The most appropriate examination is endoscopy and biopsy. If the typical appearance of reflux
esophagitis, peptic stricture or Barrett’s esophagus is seen, the diagnosis is clinched, but visible
esophagitis is not always present because the widespread use of PPIs, which cause rapid healing
of early mucosal lesions.
•
In patients with atypical or persistent symptoms despite therapy, esophageal manometry and 24-
hour esophageal pH recording (gold standard test) may be justified to establish the diagnosis and
to guide management. These tests are essential in patients being considered for anti-reflux
surgery.
Management
Medical management
•
Simple measures include advice about weight loss, smoking, excessive consumption of alcohol,
tea or coffee, the avoidance of large meals late at night and a modest degree of head-up tilt of
the bed.
•
PPIs are the most effective drug treatment for GERD. Most patients have rapid improvement in
symptoms within few days, and more that 90 % can expect full mucosal healing at 8 weeks time.
•
If medical management is unsuccessful, these patients should be formally investigated.
Surgery
The need for surgery should have been reduced as medications has improved so much.
Indication for surgery
•
“volume” reflux.
•
“hermit” lifestyle in which the least deviation from life style rules leads to symptoms.
•
Poor compliance, this is due to side effects of treatment.
•
Psychological distress with intolerance of minor symptoms.
Which operation?
All the operations must achieve the following:
•
An intra-abdominal segment of esophagus.
•
Crural repair.
•
Some form of wrap of the upper stomach (fundoplication) around the intra-abdominal esophagus.
Operations that fail to address all the three components have inferior success rate.
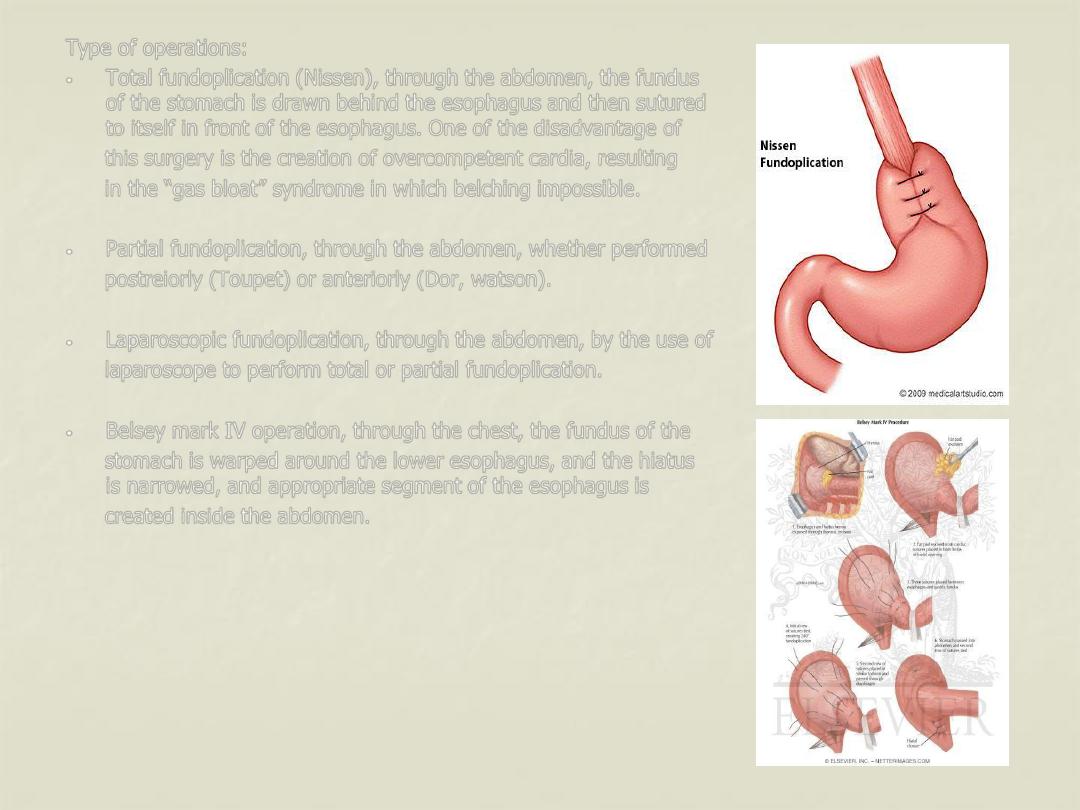
Type of operations:
•
Total fundoplication (Nissen), through the abdomen, the fundus
of the stomach is drawn behind the esophagus and then sutured
to itself in front of the esophagus. One of the disadvantage of
this surgery is the creation of overcompetent cardia, resulting
in the “gas bloat” syndrome in which belching impossible.
•
Partial fundoplication, through the abdomen, whether performed
postreiorly (Toupet) or anteriorly (Dor, watson).
•
Laparoscopic fundoplication, through the abdomen, by the use of
laparoscope to perform total or partial fundoplication.
•
Belsey mark IV operation, through the chest, the fundus of the
stomach is warped around the lower esophagus, and the hiatus
is narrowed, and appropriate segment of the esophagus is
created inside the abdomen.
Complications of gastro-esophageal reflux diseases
Stricture
Occur mainly in late middle-aged and elderly, it is about 1-2 cm above the esophago-gastric
junction, and should be distinguished from carcinoma. Peptic strictures generally respond well to
dilatation and long term treatment with a PPI.
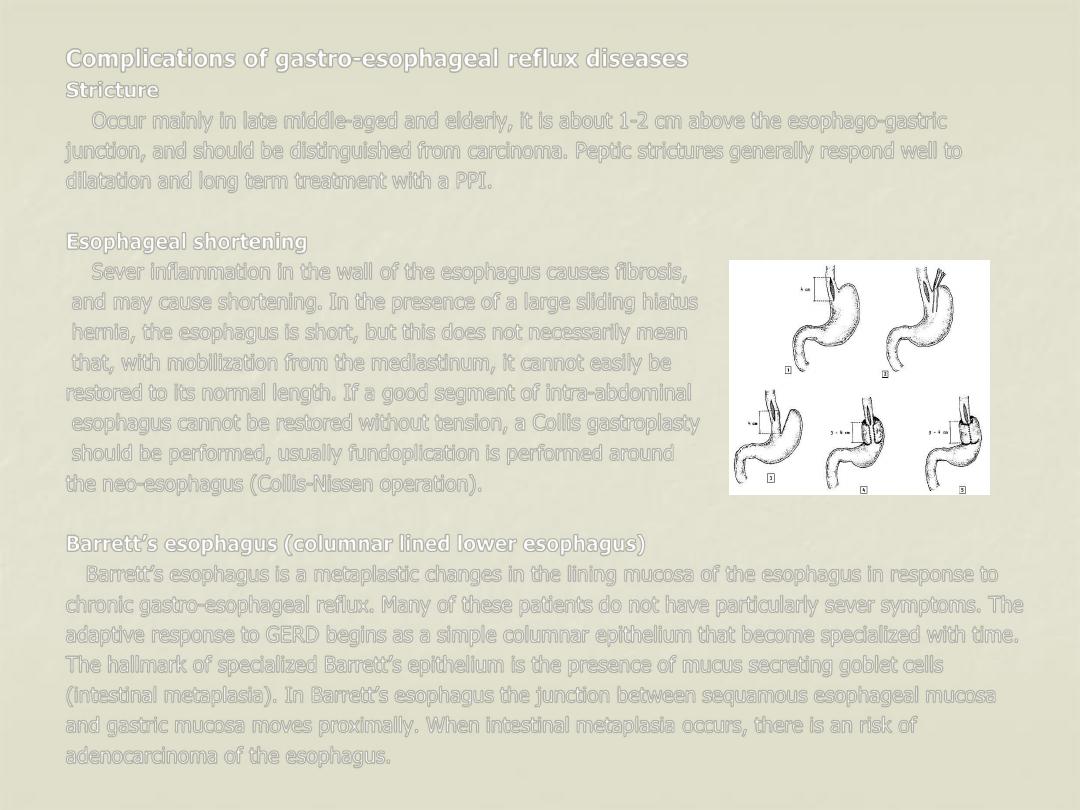
Esophageal shortening
Sever inflammation in the wall of the esophagus causes fibrosis,
and may cause shortening. In the presence of a large sliding hiatus
hernia, the esophagus is short, but this does not necessarily mean
that, with mobilization from the mediastinum, it cannot easily be
restored to its normal length. If a good segment of intra-abdominal
esophagus cannot be restored without tension, a Collis gastroplasty
should be performed, usually fundoplication is performed around
the neo-esophagus (Collis-Nissen operation).
Barrett’s esophagus (columnar lined lower esophagus)
Barrett’s esophagus is a metaplastic changes in the lining mucosa of the esophagus in response to
chronic gastro-esophageal reflux. Many of these patients do not have particularly sever symptoms. The
adaptive response to GERD begins as a simple columnar epithelium that become specialized with time.
The hallmark of specialized Barrett’s epithelium is the presence of mucus secreting goblet cells
(intestinal metaplasia). In Barrett’s esophagus the junction between sequamous esophageal mucosa
and gastric mucosa moves proximally. When intestinal metaplasia occurs, there is an risk of
adenocarcinoma of the esophagus.
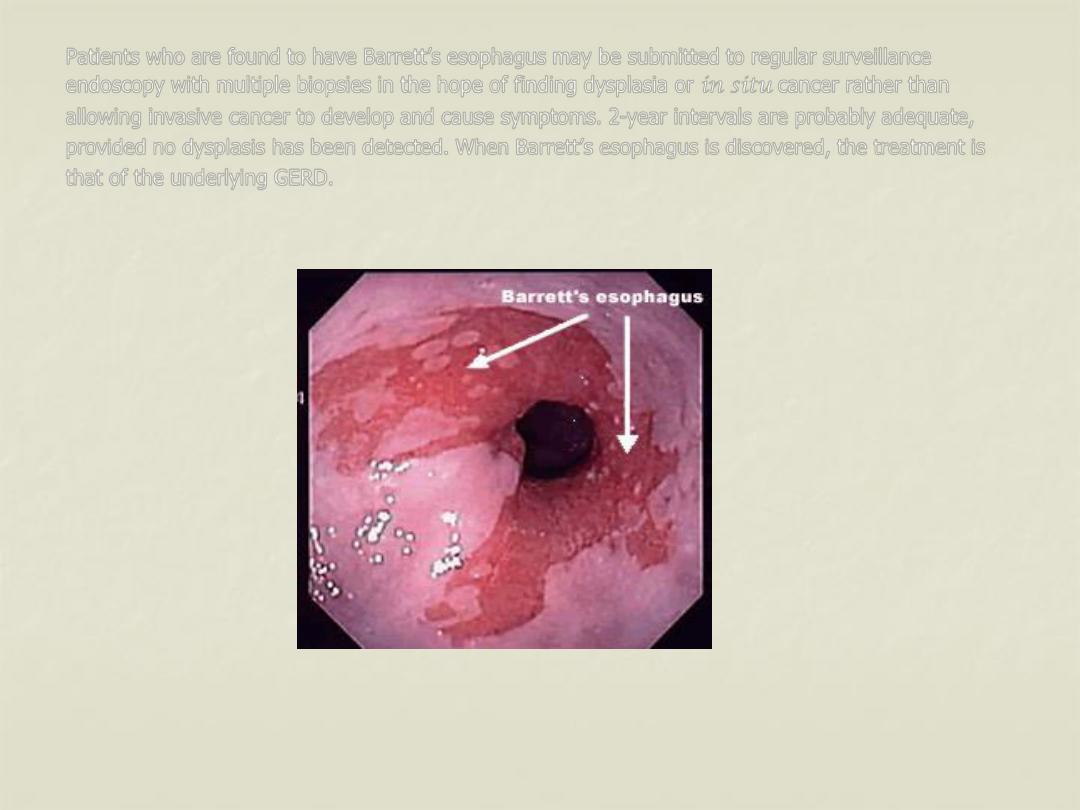
Patients who are found to have Barrett’s esophagus may be submitted to regular surveillance
endoscopy with multiple biopsies in the hope of finding dysplasia or in situ cancer rather than
allowing invasive cancer to develop and cause symptoms. 2-year intervals are probably adequate,
provided no dysplasis has been detected. When Barrett’s esophagus is discovered, the treatment is
that of the underlying GERD.
Neoplasms of the esophagus
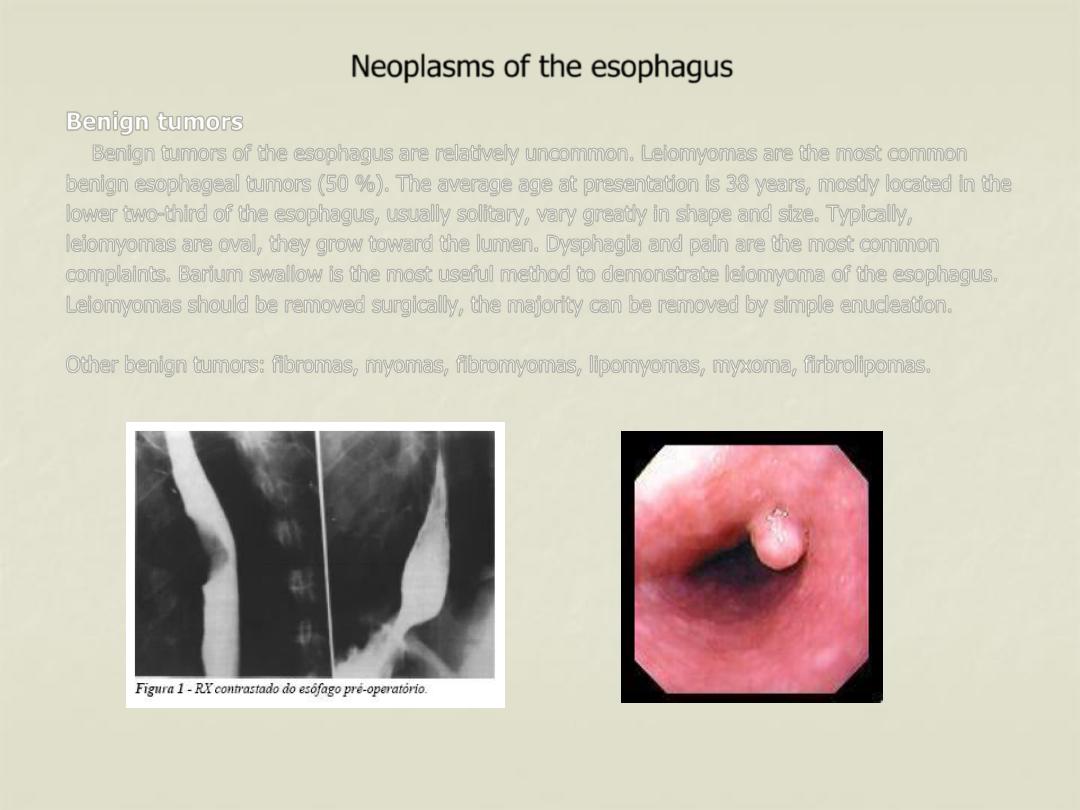
Benign tumors
Benign tumors of the esophagus are relatively uncommon. Leiomyomas are the most common
benign esophageal tumors (50 %). The average age at presentation is 38 years, mostly located in the
lower two-third of the esophagus, usually solitary, vary greatly in shape and size. Typically,
leiomyomas are oval, they grow toward the lumen. Dysphagia and pain are the most common
complaints. Barium swallow is the most useful method to demonstrate leiomyoma of the esophagus.
Leiomyomas should be removed surgically, the majority can be removed by simple enucleation.
Other benign tumors: fibromas, myomas, fibromyomas, lipomyomas, myxoma, firbrolipomas.
Malignant tumors
Non-epithelial primary malignancies are also rare, as in malignant melanoma. Secondary
malignancies rarely involve the esophagus with the exception of bronchogenic carcinoma by direct
invasion of the primary tumor or contagious lymph node.
Carcinoma of the esophagus
Cancer of the esophagus is the sixth most common cancer in the world. It is a disease of mid to
late adulthood, with a poor survival rate. Only 5-10% of those diagnosed will survive for 5 years.
Pathology and aetiology
Sequamous cell carcinoma is the most common type, generally affect the upper two-thirds of the
esophagus. Adenocarcinoma is increasing in incidence, and usually affects the lower one-third. The
geographical variation and the aetiology is as the following:
•
Sequamous cell cancer is endemic in south Africa and in the Asia “cancer belt” that extends
across the middle of Asia from north Iran to china. The highest incidence in the world is in Linxian
in Henan province in china. The cause of the disease in the endemic areas in unknown, but it is
probably due to the combination of fungal contamination of food and nutritional deficiencies.
•
Tobacco and alcohol are major factors are major factors in the occurrence of sequamous cancer.
•
Obesity and the GERD is likely to be an important factor for the increase incidence of
adenocarcinoma.
Clinical features
Most esophageal neoplasm present with mechanical symptoms, principally dysphagia. Other
symptoms include vomiting, regurgitation, odynophagia and weight loss. Clinical findings suggestive
of advance malignances and surgical cure is unlikely include:
•
Recurrent laryngeal nerve palsy
•
Horner’s syndrome
•
Chronic spinal pain.
•
Diaphragmatic paralysis.
•
Cutaneous tumor metastasis.
•
Enlarged supraclavicular lymph nodes.
Both denocarcinoma and sequamous cell carcinoma tend to disseminate early. Tumor can
spread in three ways:
•
Direct spread occur both laterally through the esophageal wall layers and longitudinally within the
esophageal wall.
•
Lymphatic spread, either longitudinally through the submucosal lymphatic channels,
consequently, the length of the esophagus involved by the tumor is much longer than the
macroscopic length of the malignancy at the epithelial surface. lymph node spread occur
commonly, Any regional lymph nodes from the superior mediastinum to the coeliac axis and
lesser curvature of the stomach may be involved regardless of the location of the primary lesion
within the esophagus.
•
Haematogenous spread may involve different organs including the liver, lung, brain and bones.
Investigations
•
Endoscopy is the first line investigation for most patients, it provides direct view of the
esophageal mucosa and any lesion allowing its site and size to be documented. Cytology and
biopsy specimens taken via the endoscopy are crucial for accurate diagnosis.
•
Transcutaneous ultrasound, used mainly to assess spread to the liver.
•
Chest radiography, to assess spread to the lungs and mediastinum.
•
Bronchoscopy, may reveal either impingement or invasion of the main airways in over 30% of
patients with cancer in the upper third of the esophagus.
•
Laparoscopy, this is useful technique for the diagnosis of intra-abdominal metastasis. It has the
advantage of enabling tissue samples or peritoneal cytology to be obtained.
•
Computerised tomography (CT scan), for assessment of the esophagus, the size and site and the
direct invasion of the tumor, lymph nodes involvement , and haematogenous spread.
•
Endoscopic ultrasound (EUS), it is more accurate than CT scan in determination the depth of
spread of malignant tumor through the esophageal wall, the invasion of the adjacent organs, and
metastasis to lymph nodes.
•
Positron emission tomography (PET), reduction in PET activity following chemotherapy might be a
way of predicting responders to this approach.
Treatment of malignant tumors
At the time of diagnosis, around two
–third of all patients with esophageal cancer will already have
incurable disease and must be offered some form of palliation. As dysphagia is the predominant
symptom in advanced esophageal cancer, the principle aim of palliation is to restore adequate
swallowing. A varity of methods are available, this include:
•
Intubations like souttar tube, which made of coiled silver wire, or other types of rigid plastic or
rubber tubes, usually placed under endoscopic and/or radiological control.
•
expanding metal stent, more commonly used now in most centers allover the world, also inserted
under radiographic or endoscopic control.
•
Other methods, like endoscopic laser treatment to core a channel through the tumor or
brachytherapy which include delivering intraluminal radiation with short penetration distance to a
tumor.
Surgery alone is best suited to patients with disease confined to the esophagus without nodal
metastasis, with a prospect of cure in between 50% and 80%. The operative approaches are:
•
Left thoracoabdominal approach, which opens the abdominal and the thoracic cavity together,
this approach is limited proximally by the aortic arch and should be avoided when the primary
tumor is at or above this level.
•
Ivor Lewis operation, the most widely practiced approach in the world, with an initial laparotomy
and construction of gastric tube, followed by right thoracotomy to excise the tumor and create
an esophageogastric anastomoses.
•
Transhiatal esophagectomy (without thoracotomy), the stomach is mobilized through a midline
abdominal incision, and the esophagus is mobilized through an incision in the neck. it may be
useful procedure for tumor of lower esophagus.
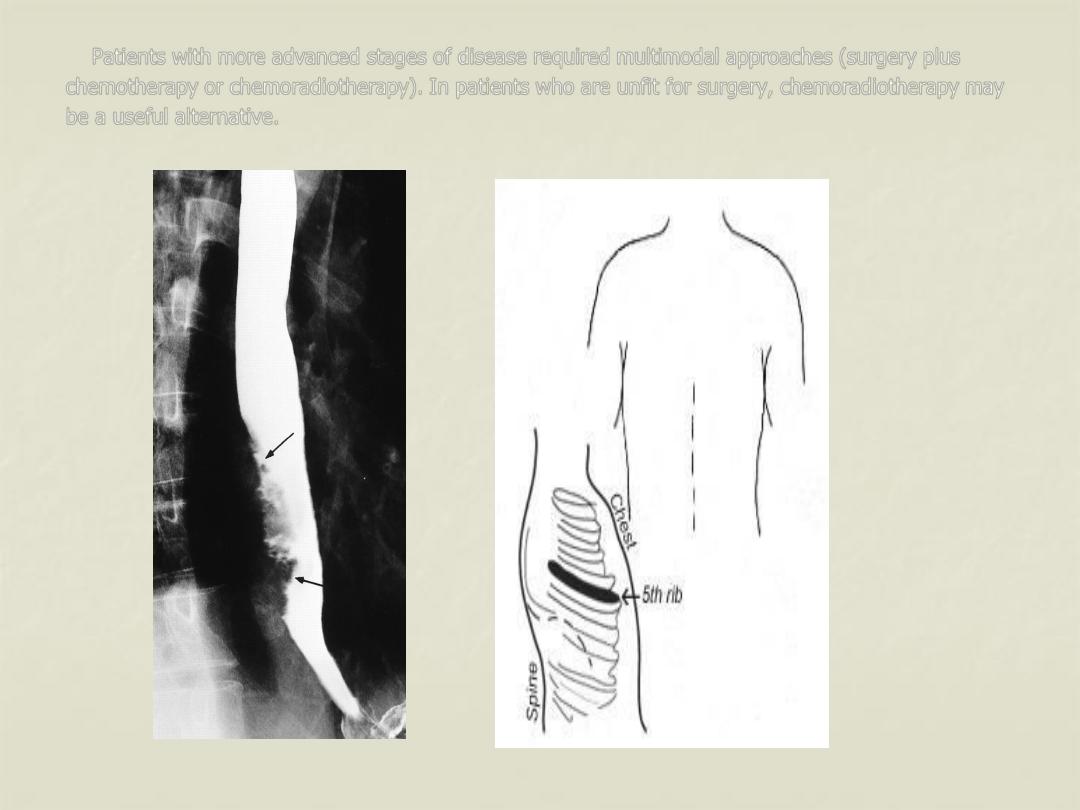
Patients with more advanced stages of disease required multimodal approaches (surgery plus
chemotherapy or chemoradiotherapy). In patients who are unfit for surgery, chemoradiotherapy may
be a useful alternative.
Achalasia
Pathology and aetiology
Achalasia (Greek “failure to relax”)
is uncommon.
It is due to loss of the ganglion cells in
the
myenteric (Auerbach’s) plexus, the cause
of which is unknown
.
The physiological abnormalities are a
non-relaxing LES and absent peristalsis in the body of the esophagus. In its earliest stages
,
the
esophagus is of normal caliber and still exhibit contractile (although non-peristaltic) activity. With
time, the esophagus dilates and contractions disappears, so that the esophagus empties mainly by the
hydrostatic pressure of its contents. This is nearly always incomplete, leaving residual food and fluid.
The gas bubble in the stomach is frequently absent. The esophagus may becomes huge, and
tortuous with persistent retention esophagitis due to fermentation of food residues “ megaesophagus”.
Clinical features
The disease is most common in middle life, but can occur at any age. It typically presents with
dysphagia. Patients often present late, having had relatively mild symptoms for many years
Regurgitations is frequent, and may be overspill into the trachea, especially at night.
Diagnosis
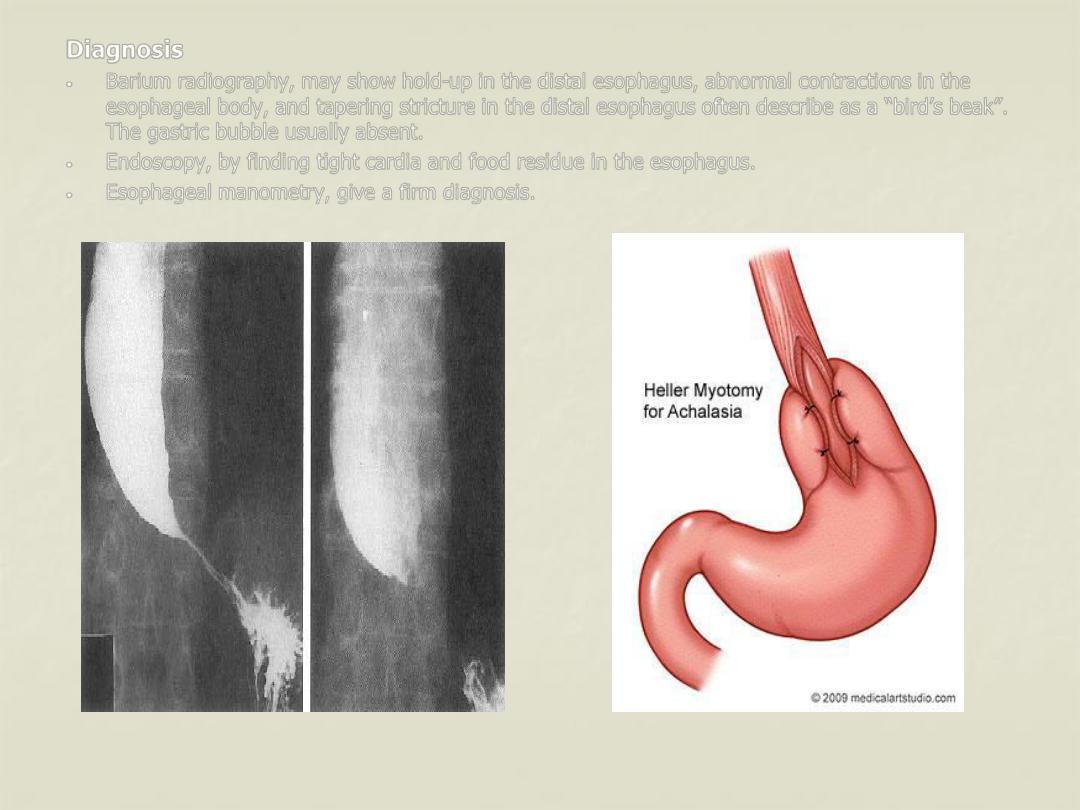
•
Barium radiography, may show hold-up in the distal esophagus, abnormal contractions in the
esophageal body, and tapering stricture in the distal esophagus often describe as a “bird’s beak”.
The gastric bubble usually absent.
•
Endoscopy, by finding tight cardia and food residue in the esophagus.
•
Esophageal manometry, give a firm diagnosis.
Treatment
Achalasia respond well to treatment. The two main methods are forceful dilatation of the cardia
and Heller’s myotomy.
Pneumatic dilatation
This involve stretching the cardia with a balloon to disturb the muscle and render it less competent.
The balloon are inserted over a guide wire. Perforation is the major complication (less than 5%). In
the well developed centers forceful dilatation is curative in 75-85% of cases.
Heller’s myotomy
This involve longitudinal cutting in the muscles of the lower esophagus and cardia. The major
complication is GERD, and many surgeons, therefore, add a partial anterior fundoplication (Heller’s-
Dor’s operation). The operation is ideally performed through the thoracic approach, but could be done
through abdominal approach, and recently, through minimal access laparoscopic approach. It is
successful in more than 90% of cases and may be used after failed dilatation.
Botulinum toxin
This is done by endoscopic injection into the LES. It acts by interfering with cholinergic excitatory
neural activity at the LES. The effect is not permanent, and the injection usually has to be repeated
after a few months. For this reason, its use is restricted to elderly patients with other comorbidities.
Drugs
Drug such as calcium channel antagonists or sublingual nifedipine may be useful for transient relief
of symptoms.
Miscellaneous conditions
Zinker’s diverticulum (pharyngeal pouch)
It protrudes posteriorly above the cricopharyngeal sphincter through the natural week point (the
dehiscence of Killian) between the oblique and the horizontal fibers of the inferior pharyngeal
constrictors.
Epiphrenic diverticulum
Situated in the lower esophagus above the diaphragm, they may be quite large, but causing few
symptoms.
Plummer-Vinson syndrome
Also called Paterson-kelly syndrome, dysphagia occur because of the presence of a post-cricoid
web that is associated with iron deficiency anemia, glossitis, and Koilonychia.
Schatzki’s ring
Is a circular ring in the distal esophagus, usually at the sequamocolumnar junction, it may
associated with reflux disease. Most are asymptomatic, when associated with dysphagia, dilatation
with anti-reflux drugs must be used.
