Anterior Cervical
Triangle
2
To list strap muscles
To describe muscular triangle
To describe the anatomy of thyroid gland with important
clinically related points
To define the parathyroids
To relate the main vessels & nerves in the region to these
structures
To relate thyroid surgery & its complication to anatomical
basis
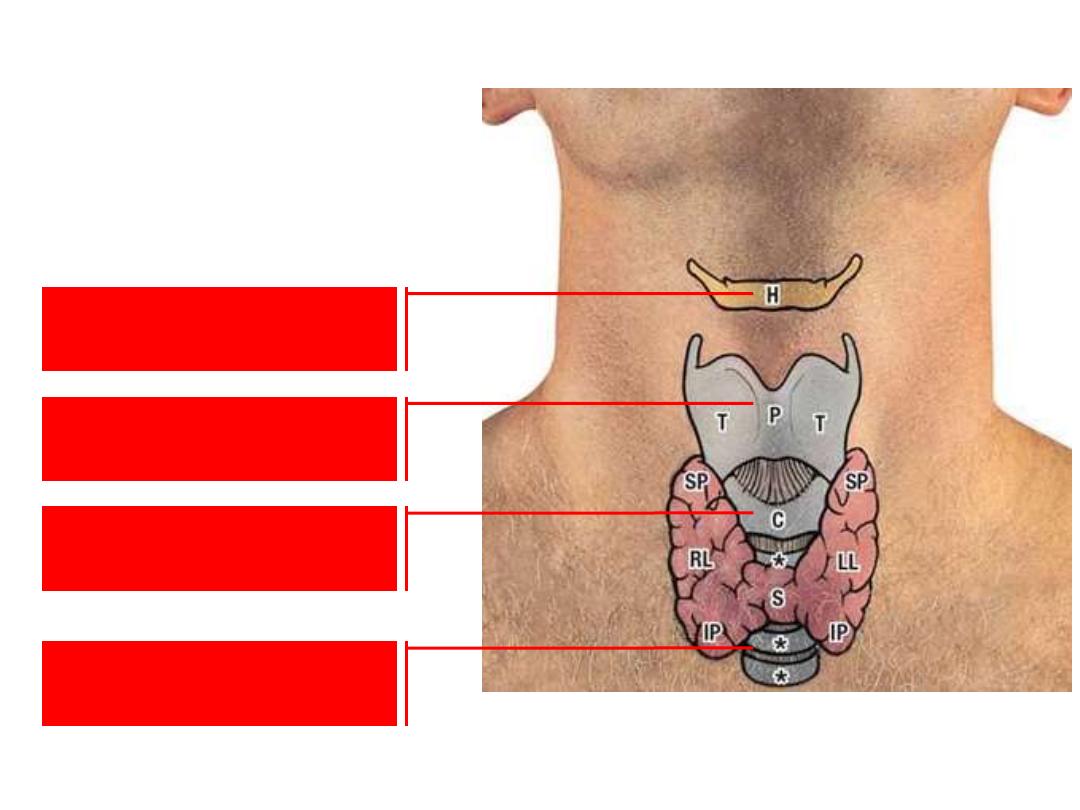
Midline surface landmarks in the neck:
Hyoid bone
Thyroid C
Cricoid C
Trachea
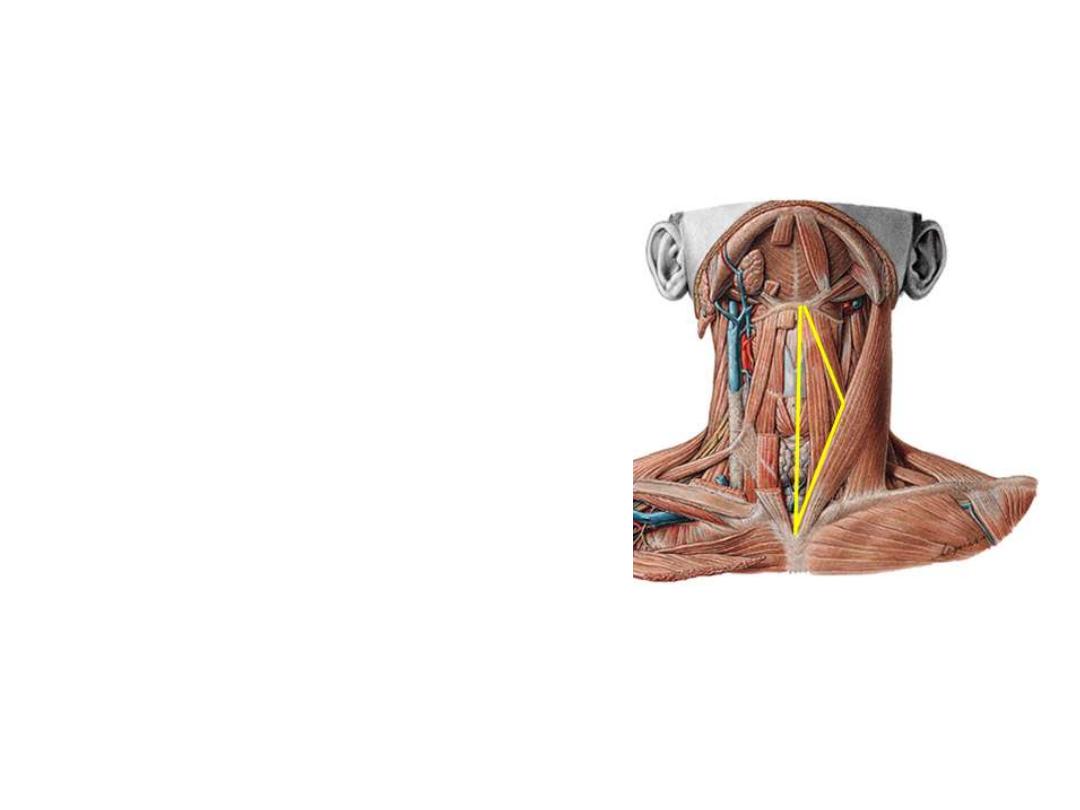
Thyroid gland:
Thyroid gland lies theoretically in
the muscular triangle.
The triangle is bounded by the
midline, omohyoid SB & lower part
of SCM
The gland lies in a bag of
pretracheal fascia attaches it to
laryngeal cartilages
Skin, superficial fascia, investing
then pretracheal fascia should be
opened in order to reach the gland
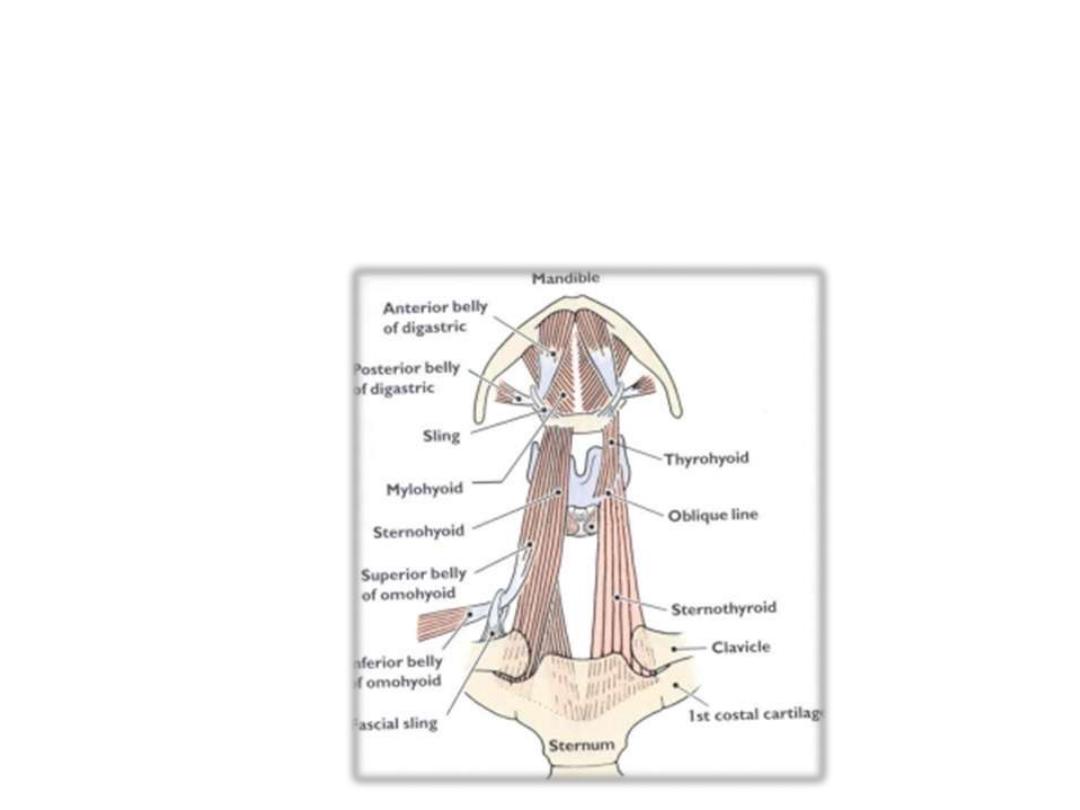
The strap (infrahyoid) muscles:
-Four muscles arranged in two layers
-Superficial layers contain two muscles lying side by side (sternohyoid &
omohyoid)
-The two deep muscles are lying one above the other (sternothyroid & thyrohyoid)
-Their attachment is reflected by their names between the manubrium, thyroid
cartilage & hyoid bone

-Omohyoid, a two belly muscle arises from the scapula & inserted to the hyoid
bone
-They are segmentally supplied by ansa cervicalis
(except thyrohyoid??)
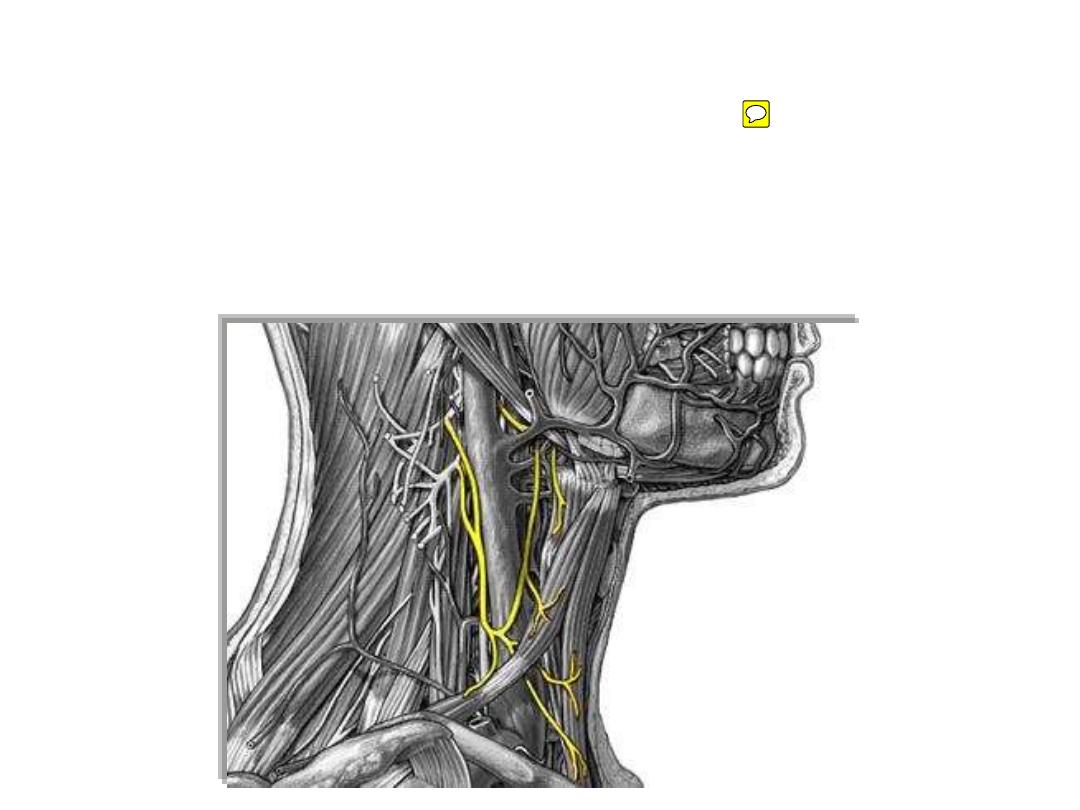
Ansa cervicalis:
-Y- shaped nerve trunk lies close to the IJV
-Formed by:
1- Superior root (C1); from C1 fibers accompanying the hypoglossal nerve
2- Inferior root (C2&3); from cervical plexus
- Supplies the strap muscles except thyrohyoid
Action of infrahyoid muscles:
•Anchoring the hyoid to the sternum
& scapula
•Stabilize the hyoid for more tongue
fixation
•Depression of the larynx during:
-Speech: changing voice resonance
-Swallowing: after initial elevation
for airway protection
The pretracheal fascia:
•Fascial bag enclosing the thyroid gland
•Attached to the thyroid cartilage
•Makes the gland moves up with swallowing
The thyroid gland:
An butterfly like endocrine gland formed of two lateral lobes connected in
the midline by an isthmus
The gland weighs 20-40 gm
The ductless gland is responsible for producing & secreting T3 & T4
hormones which are responsible for metabolism
Calcitonin is the 3
rd
hormone secreted by the gland
The lateral lobe:
-Pyramidal in shape
-It has thin anterior & thick rounded posterior borders
-Extends from the oblique line of thyroid cartilage down to the 6
th
tracheal ring
(C8-T1 vertebral level)
-It is 50-60 mm in height
C7

The isthmus:
-Lies opposite to tracheal rings 2-4
-It is the only part of the gland fused to the pretracheal fascia
-Should be divided in routine tracheostomies
-10-15 mm in height
The pyramidal lobe:
- Not often present (20-30%)
- Arises from the isthmus & points mainly to the left
- Indicates the site of thyroglossal duct
Levator glandulae thyroideae:
-Not often present
-Extends from the pyramidal lobe
-More on the left side
-Represents embryological pathway

Thyroglossal cyst:
-Along the embryological pathway (midline neck swelling)
-Moves when the tongue is protruded
-In the subhyoid region
Lateral relations:
-
Anteriorly; sternothyroid + sternohyoid
-
Posteriorly; carotid sheath (note the structural arrangement)
Medial relations:
-
Anteriorly; Larynx + trachea
-
Posteriorly; pharynx + oesophagus
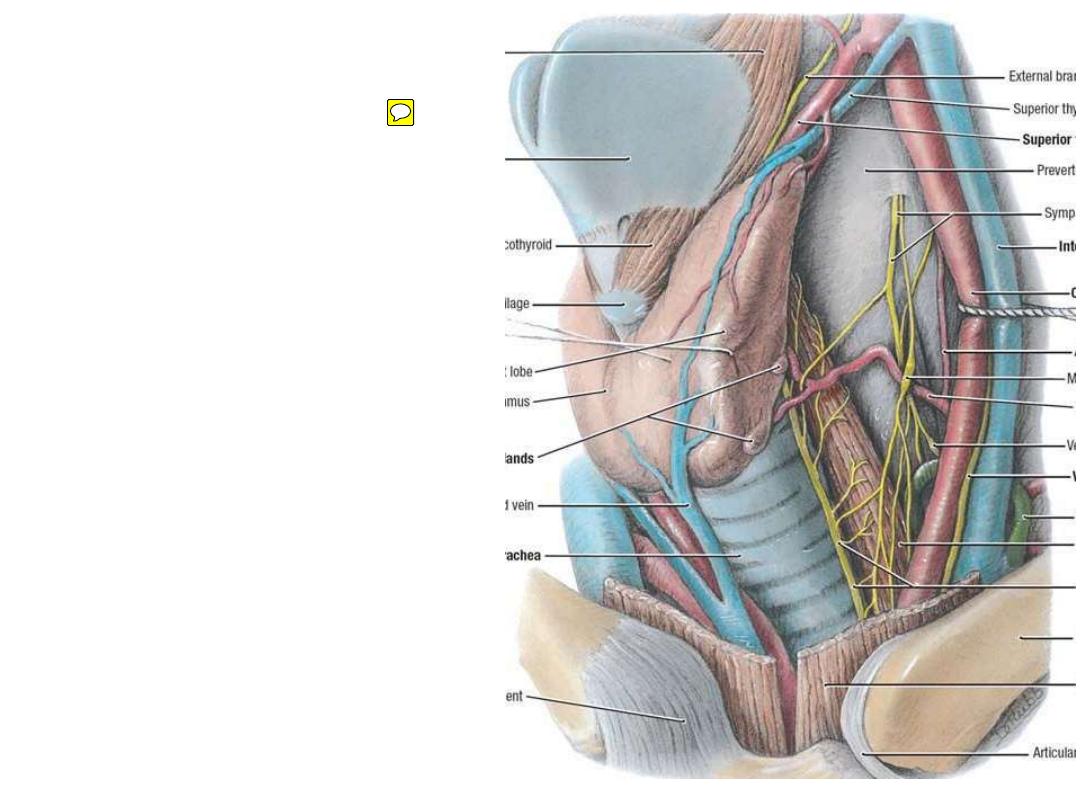
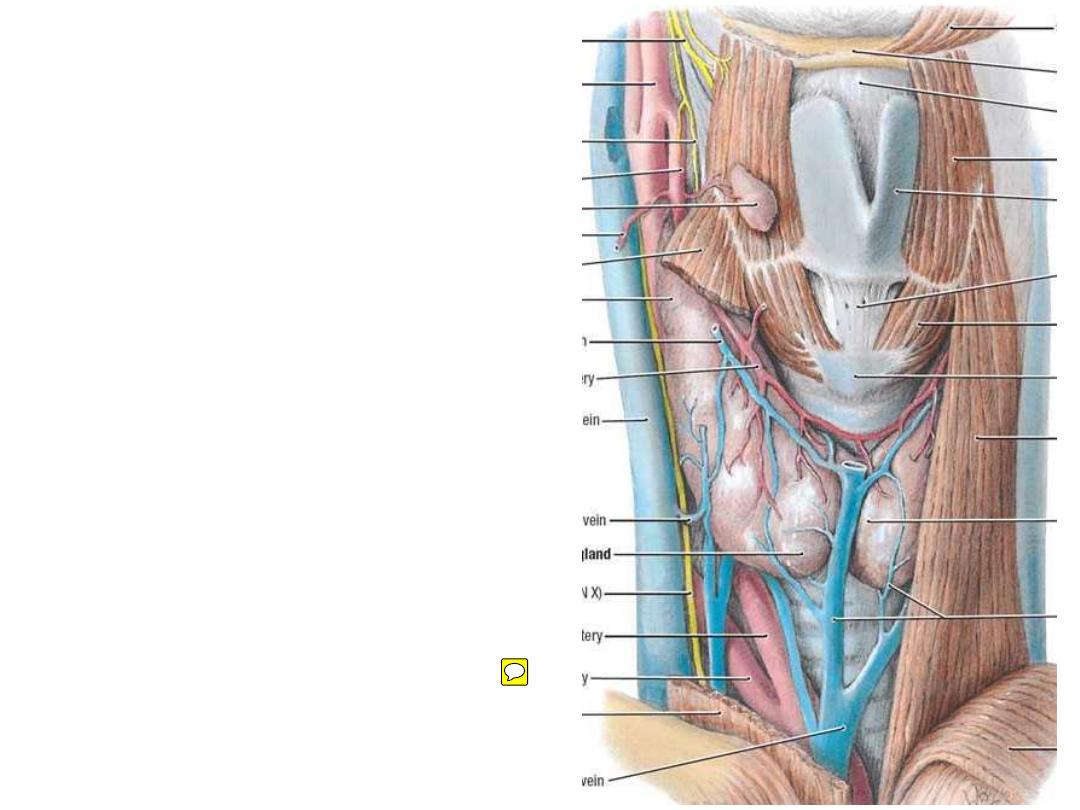
Arteries:
1- Superior thyroid artery:
-The most proximal branch of
ECA
-Enters the gland apex
-Divides
within
the
fascial
covering
into
anterior
&
posterior
branches
which
anastomose
with
similar
branches of inferior thyroid a.
-Accompanied
by
external
laryngeal nerve
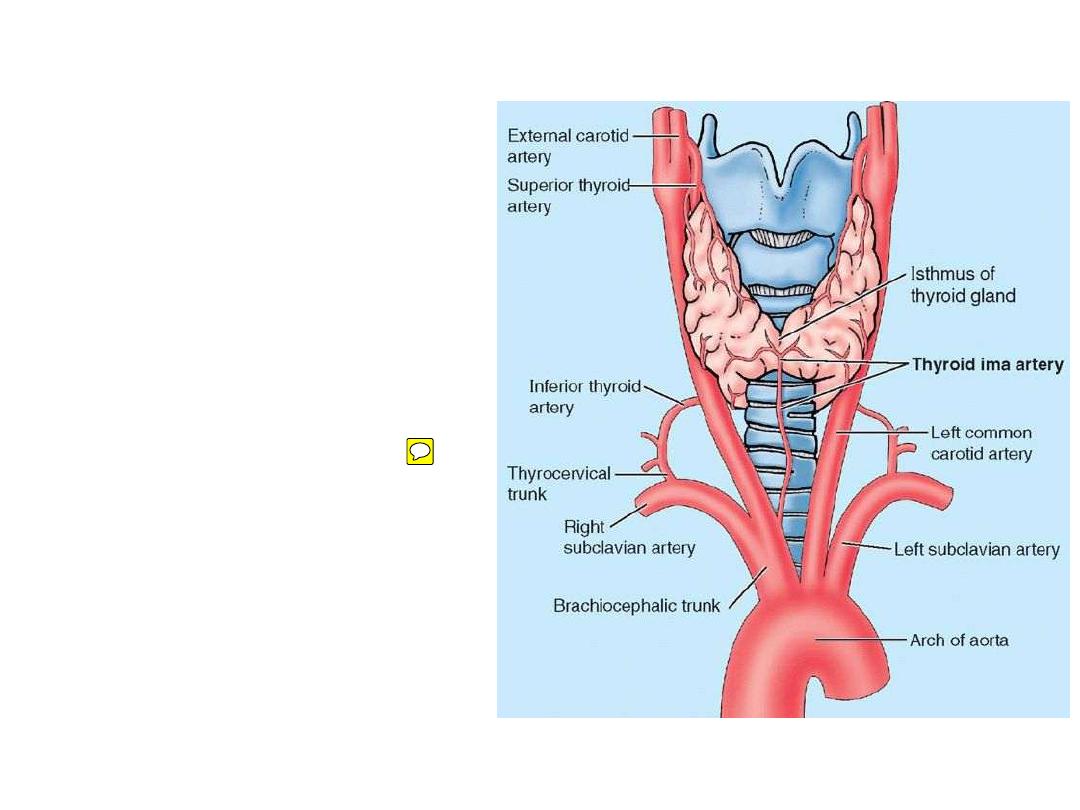
2- Inferior thyroid artery:
-The continuation of thyrocervical
trunk
-Divides & anastomoses like the
superior one
-Accompanied by the recurrent
laryngeal nerve
3- Thyroidea ima artery:
-From brachiocephalic trunk or
aortic arch
-Only present in 10%
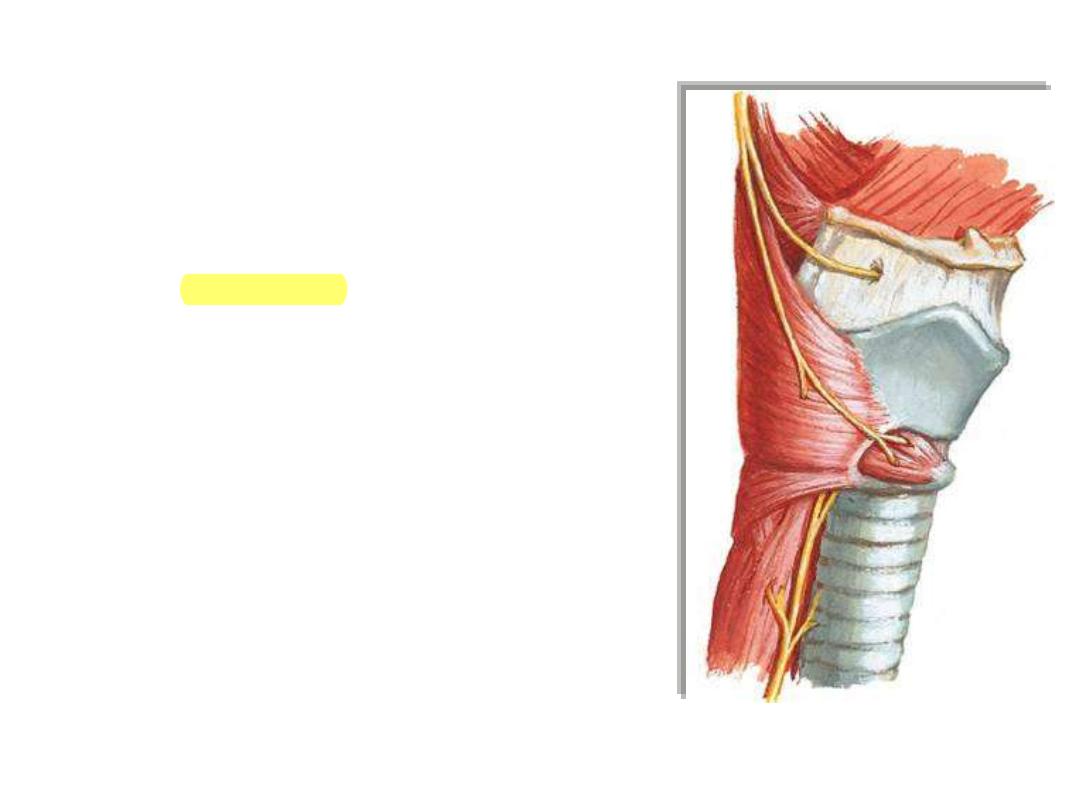
External laryngeal nerve:
- Branch of superior laryngeal n. (vagal branch)
- Accompanies the ST artery
- Supplies cricothyroid muscle
Recurrent laryngeal nerve:
- Branch of vagus
- Descends to reach the right subclavian artery
(R) & ligamentum arteriosum (L) where it
hooks & recurs up to the larynx
- Accompanies IT artery
- Supplies most of laryngeal mucosa & muscles
Veins:
1- Superior thyroid v; to the IJV
2- Middle thyroid v.; to the IJV
3- Inferior thyroid plexus; to the
left brachiocephalic vein
Nerves:
Sensory; recurrent laryngeal n.
Sympathetic; vascular branches
of middle cervical ganglion
Clinical notes:
A midline neck swelling which
moves with deglutition is considered
thyroid-related
until
proved
otherwise
Incisions for thyroidectomy best to
be
done
along
Langer
lines
(transverse) for cosmetic purposes
Clinical notes:
Recurrent laryngeal nerve is
frequently injured during thyroid
operations
Enlarged thyroid may be so
huge to go inside the superior
mediastinum
(retrosternal goiter)
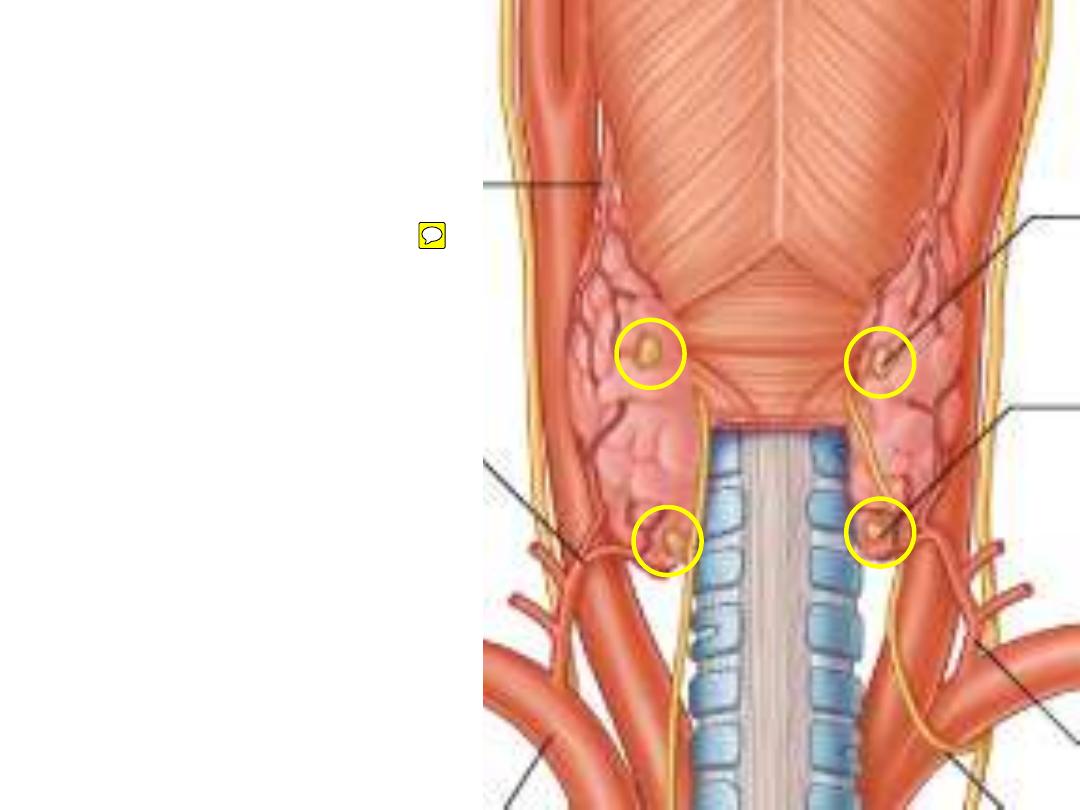
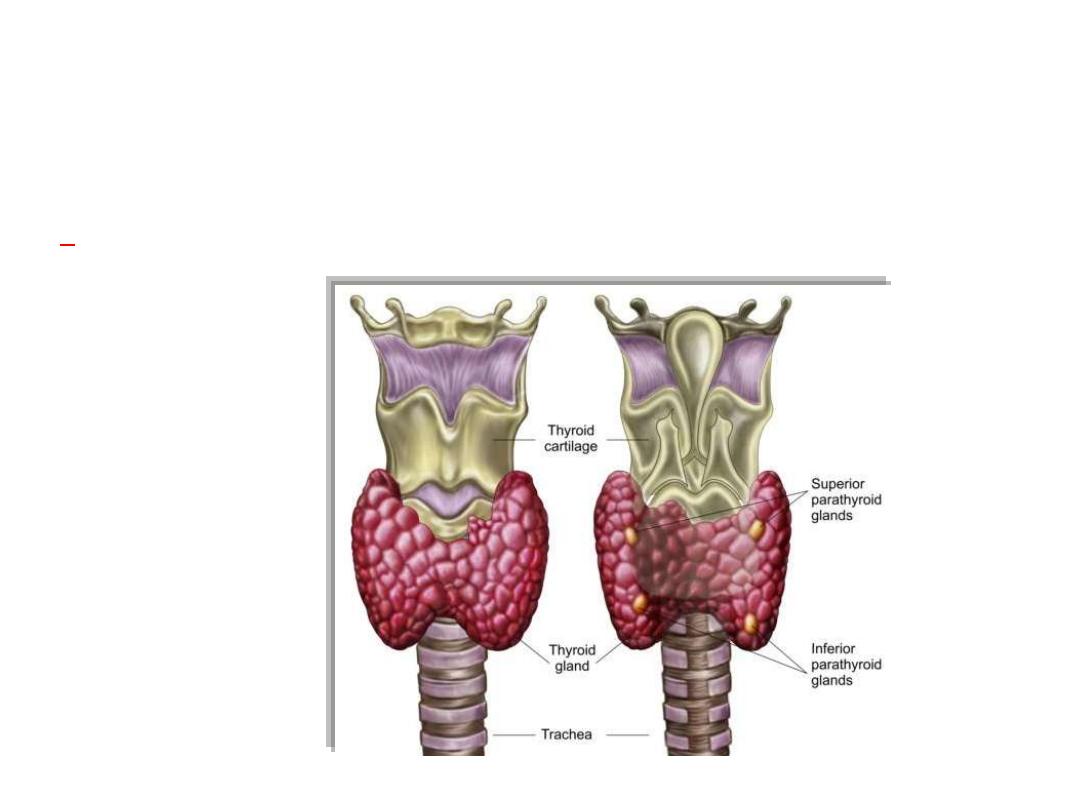
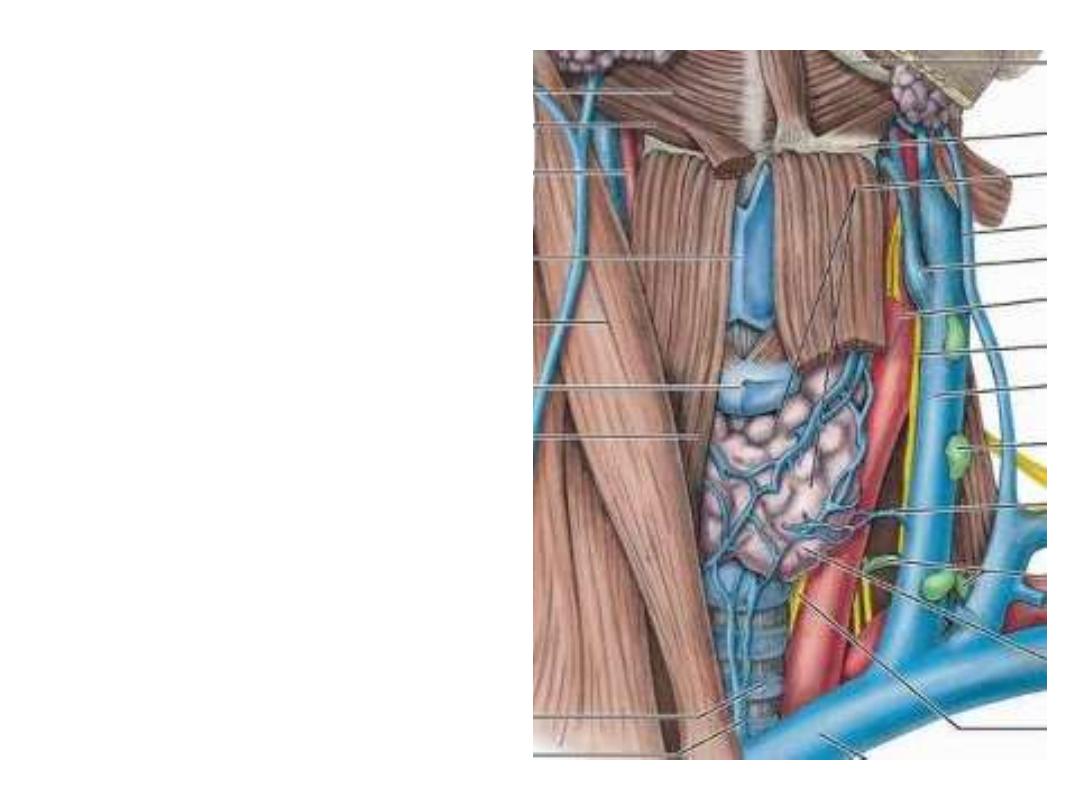
The parathyroid glands:
-Two pairs, superior & inferior
-Lie in the posterior part of the
lateral lobe of the thyroid gland
-Blood
supply,
nerves
&
lymphatics like the thyroid gland
-Often excised with the thyroid
gland
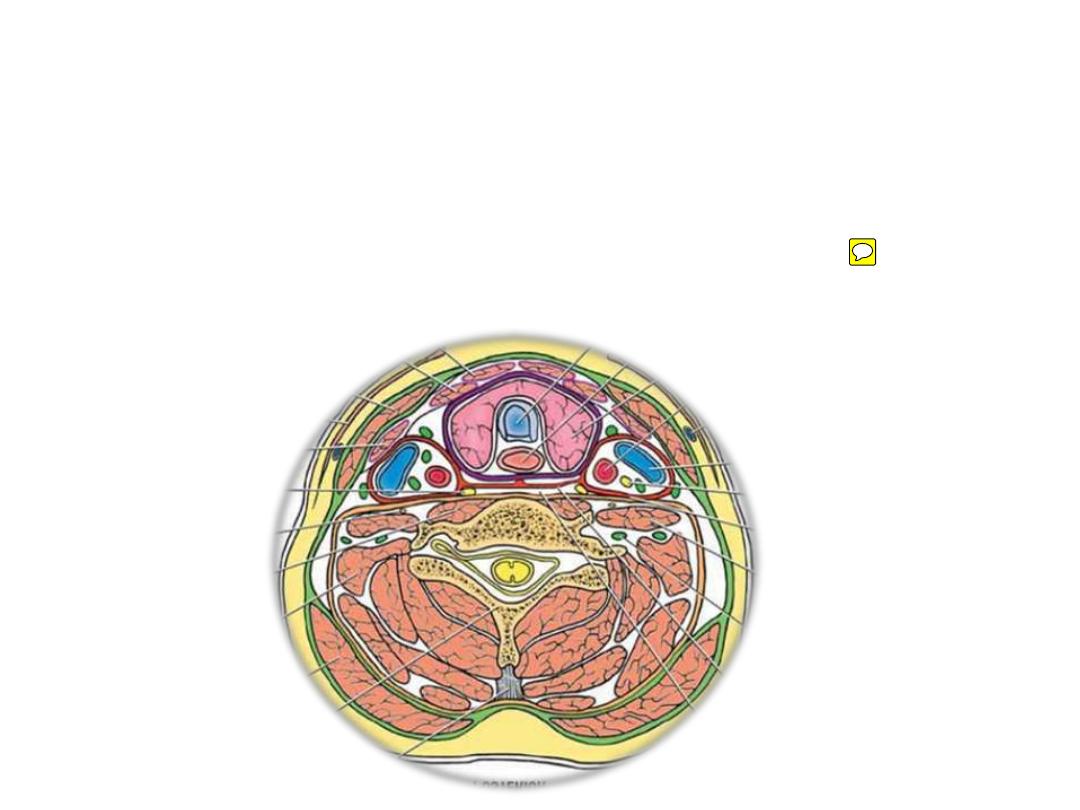
The trachea:
-12 cm, fro C6-T4
-Rings are C- shaped completed behind
by trachealis
Relations:
-The CCA; posterolateral
-Thyroid lobe; anterolateral down to the
6
th
ring
-Thyroid isthmus; anterior (rings 2-4)
-Oesophagus; behind
Arteries:
Inferior thyroid artery
Veins;
Inferior thyroid veins
Nerves;
Recurrent laryngeal nerve
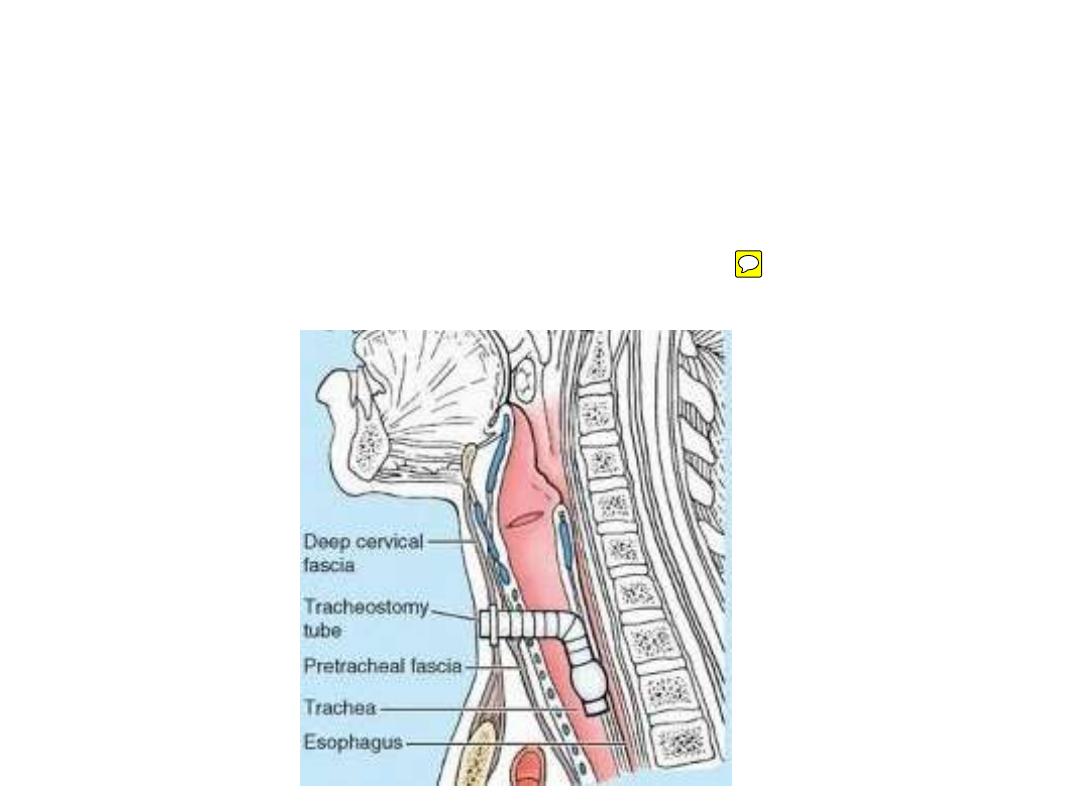
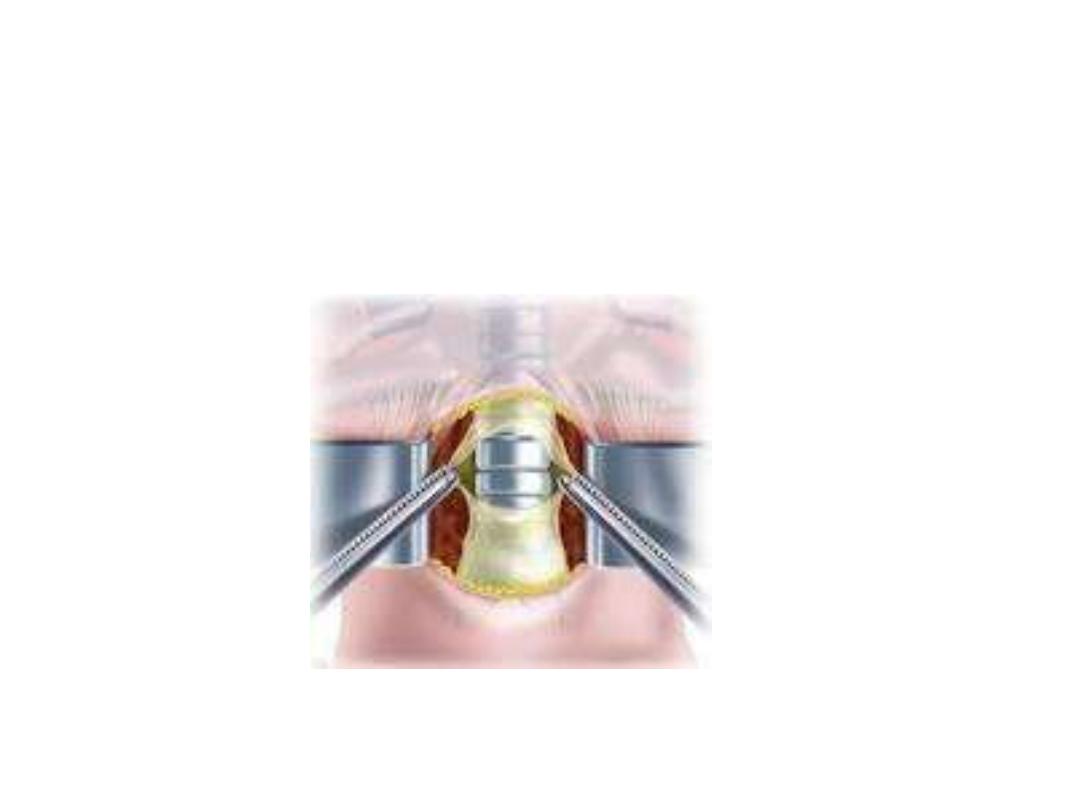
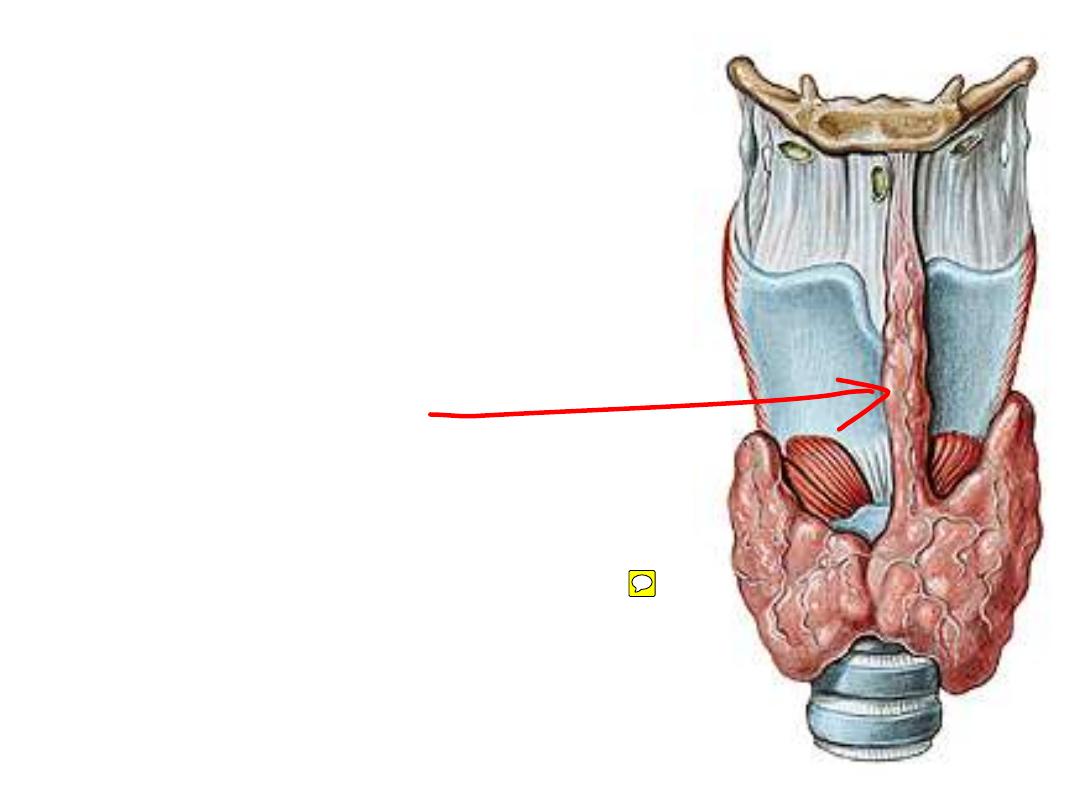
Tracheostomy:
Opening the trachea to relieve airway obstruction
Structures encountered in this operation:
-Jugular venous arch
-Sternohyoid & sternothyroid
-Thyroid isthmus
pretrachesl fascia
thyroid isthmus
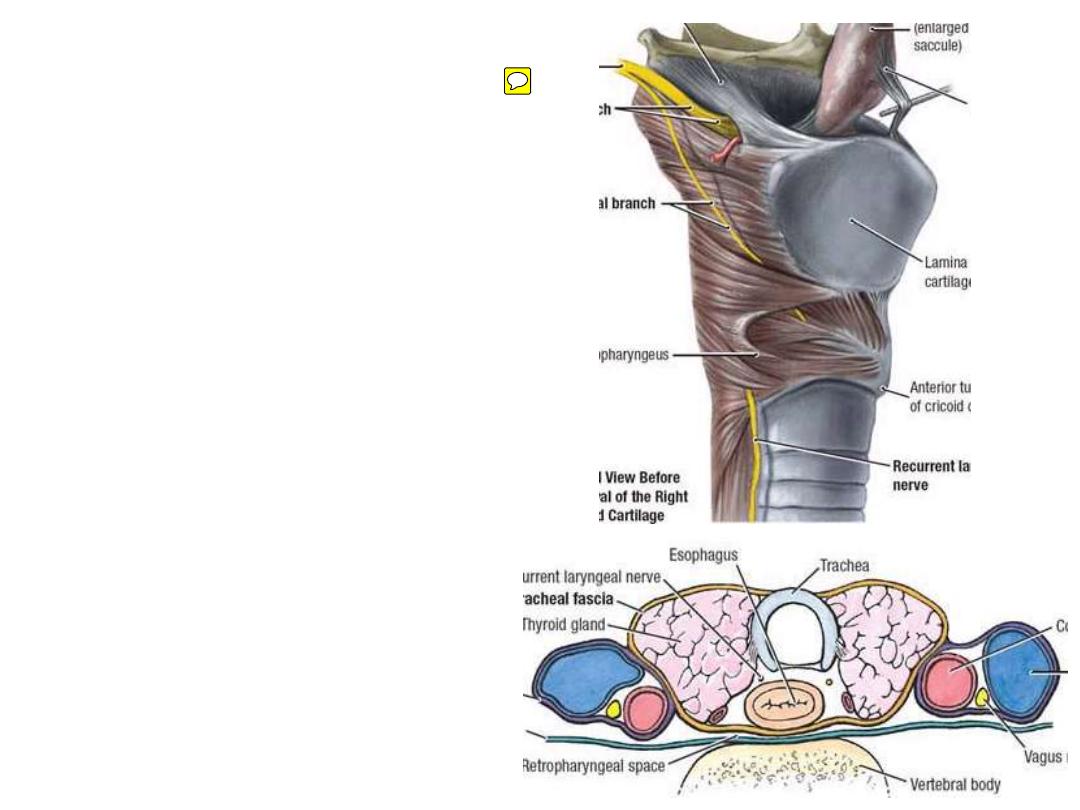
The oesophagus:
•25 cm long muscular tube
•Extends from the pharynx (C6) to
the gastro-esophageal junction
(T11)
•Lies in the midline posterior to
the trachea
•Recurrent
laryngeal
nerve
occupies the groove between it &
the trachea
•Posterior to it is the prevertebral
fascia & sympathetic trunk
Vessels & nerves;
like trachea
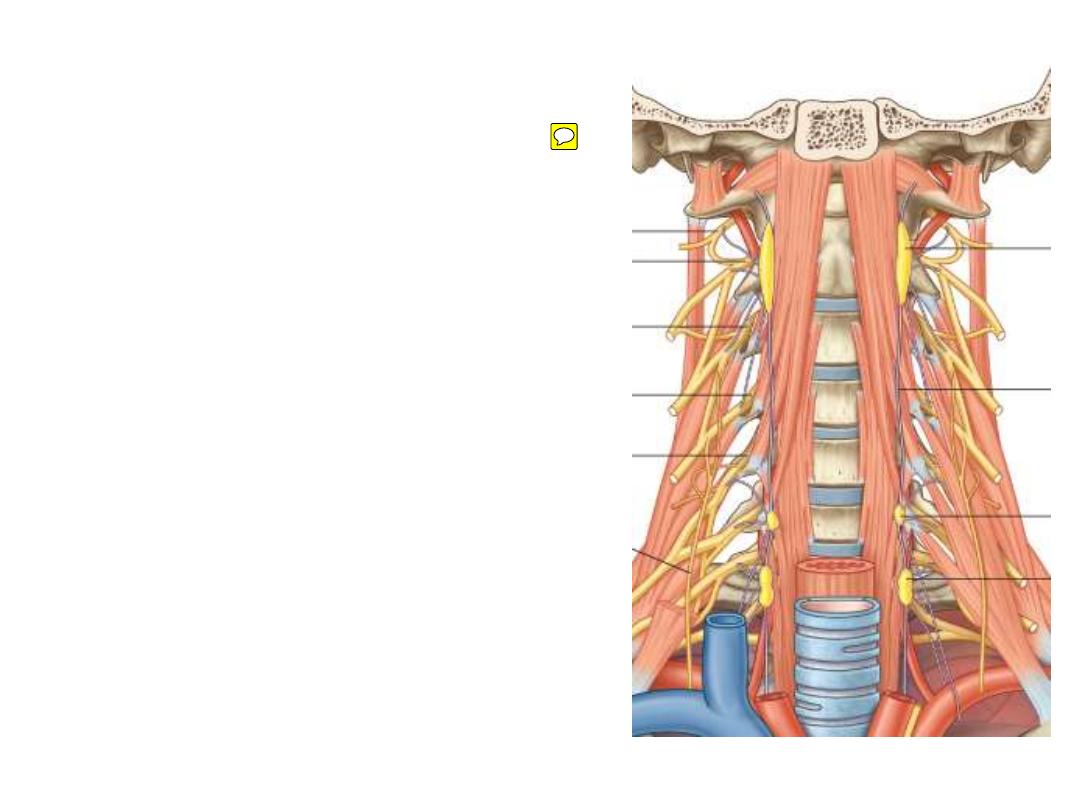
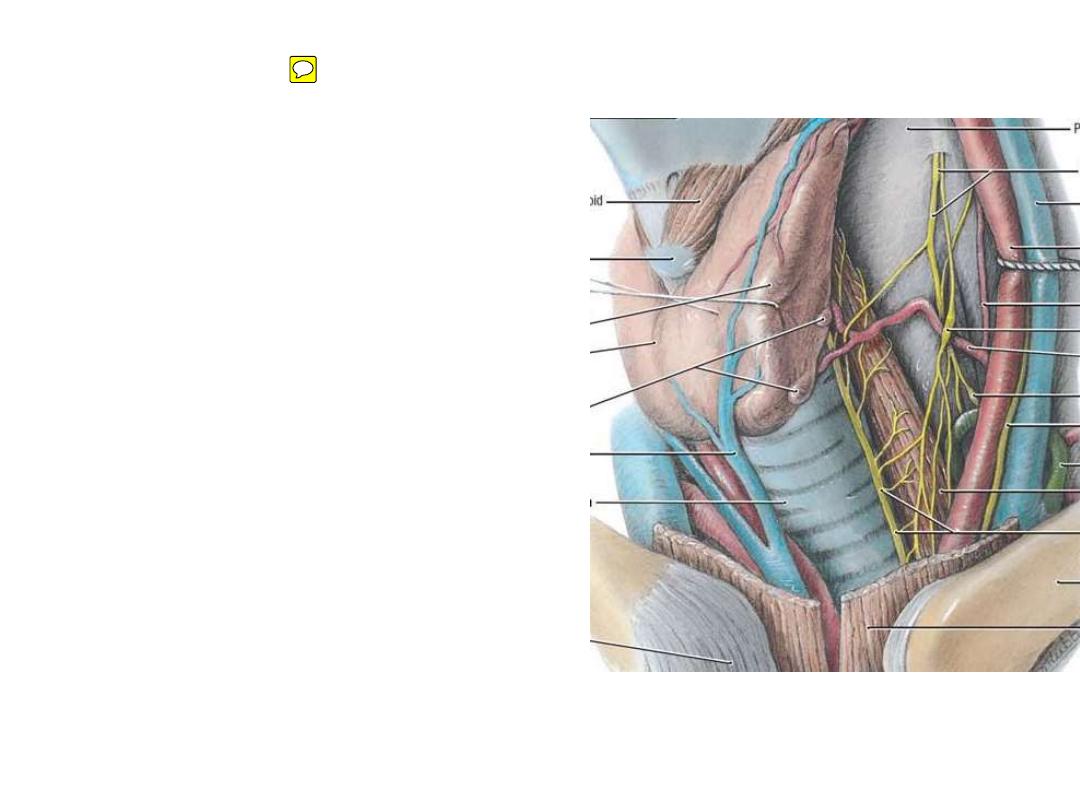
The Cervical Sympathetic Trunk:
•Mainly made of preganglionic fibers
from upper thoracic segments
•Possesses three ganglia:
-Superior; C2 level
-Middle; C6 level
-Inferior (stellate?); neck of first rib
•Ganglia has three sets of branches:
-Somatic
-Visceral
-vascular
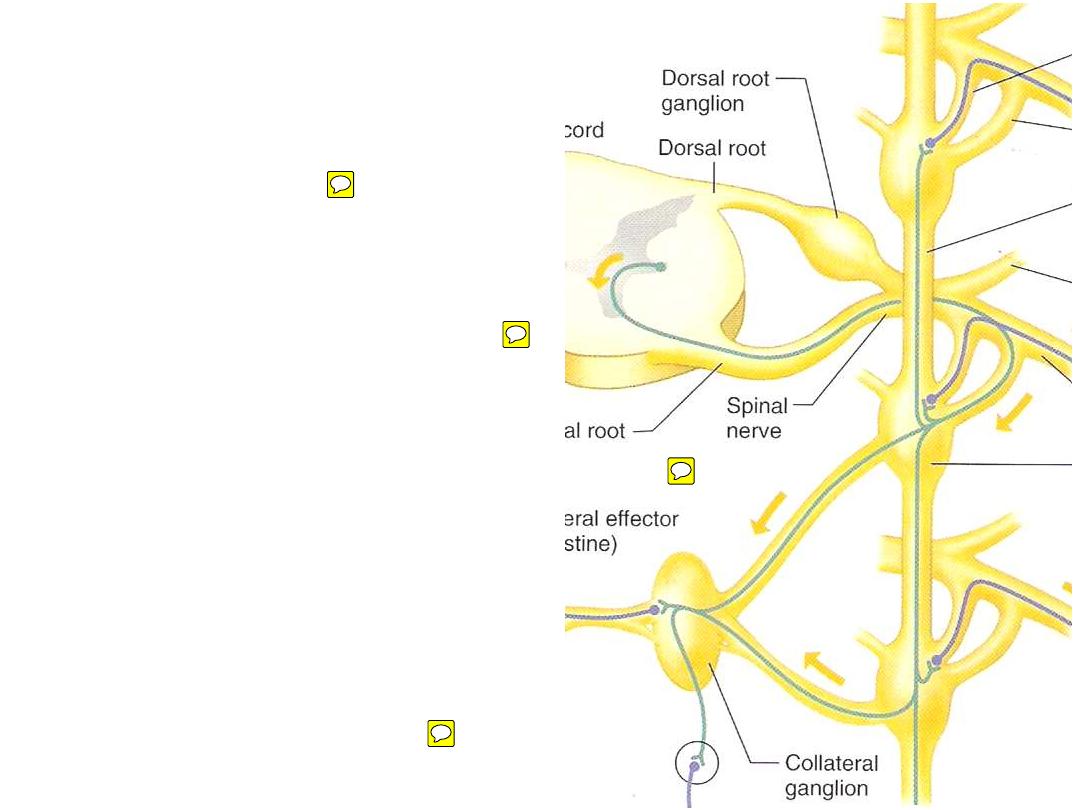
When the preanglionic fiber reaches the
ganglion, it takes one of the following
behaviors:
1- Synapse in the same ganglion & give
postganglionic fibers with its own
spinal nerve
2- Bypass the ganglion & synapse in
another ganglion (higher or lower)
giving
postganglionic
fibers
that
accompany spinal nerves not belonging
to its original segment
3- Bypass the ganglion & synapse in
ganglia outside the trunk (splanchnics)
4- Go to adrenal medulla
1
2
3
Visceral
Vascular
Somatic
Ganglion
A nerve from
each ganglion
to the cardiac
plexus
Along ICA
C1-C4
Superior
Along inferior thyroid a.
C5&6
Middle
Along vertebral a.
C7&8
Inferior
Branches:
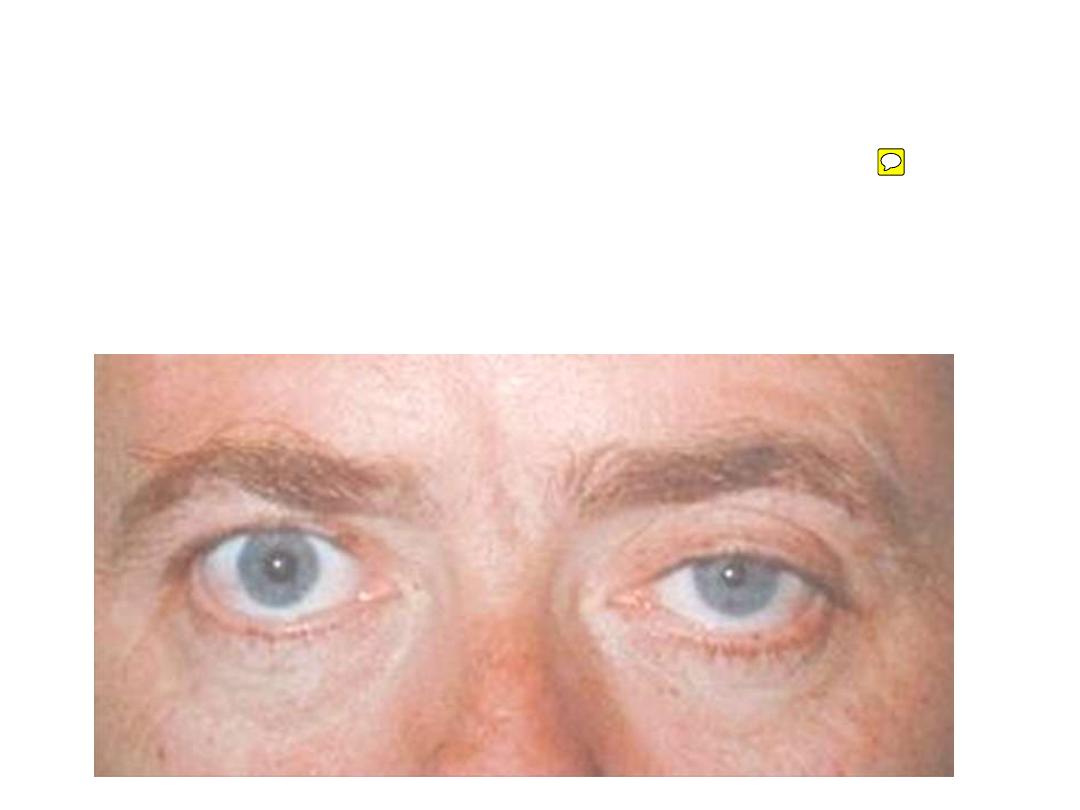
Horner syndrome
:
Injury of the sympathetic trunk affecting T1 segment
-Meiosis: paralysis of the dilator pupillae muscle
-Ptosis: partial paralysis of the levator palpebrae superioris
.
-Flushing & anhydrosis: reduced vascular & glandular sympathetic
activity in the skin
