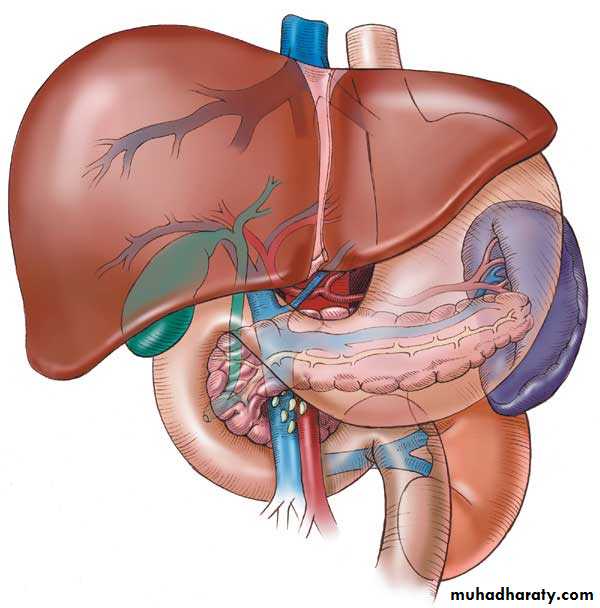
liver
The largest single organ in the human body.In an adult, it weighs about three pounds and is roughly the size of a football.
Located in the upper right-hand part of the abdomen, behind the lower ribs
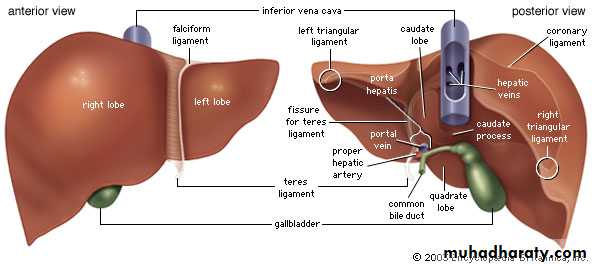
The liver is divided) into four lobes: the right (the largest lobe), left, quadrate and caudate lobes.
Supplied with blood via the protal vein and hepatic artery.
Blood carried away by the hepatic vein.It is connected to the diaphragm and abdomainal walls by five ligaments.
Gall Bladder
Muscular bag for the storage, concentration, acidification and delivery of bile to small intestine
• The liver is the only human organ that has the remarkable property of self-regeneration. If a part of the liver is removed, the remaining parts can grow back to its original size and shape.
LIVER FUNCTION TESTS
Alanine transaminse (ALT)Aspartate transaminase (AST )
ALKALINE PHOSPHATASE
BILIRUBIN
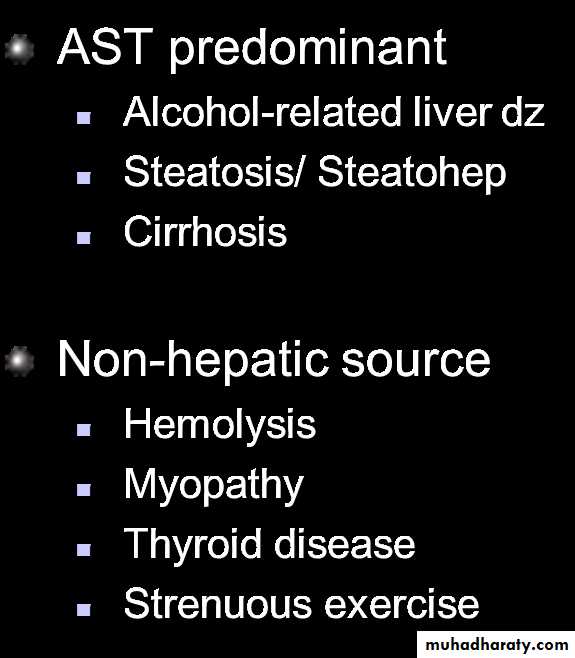
ALT and AST
Enzymes, found in HepatocytesReleased when liver cells damaged
ALT is specific for liver injury
AST (SGOT) is also found in skeletal and cardiac muscle
Transaminitis: < 5 x normal
ALT predominantChronic Hep B / C
Acute A-E, EBV, CMV
Hemochromatosis
Medications / Toxins
Autoimmune Hepatitis
Alpha-1-antitrypsin
Wilson’s Disease
Celiac Disease
ALKALINE PHOSPHATASE
Found in hepatocytes that line the bile canaliculiLevel is raised in Biliary obstruction (causes stretch of the bile canaliculi)
BUT also found in BONE and PLACENTA
GGT is also found in bile canaliculi and therefore can be used in conjunction with Alk Phos for predicting liver origin
BUT GGT can be raised by many drugs including Alcohol and therefore non specific
BILIRUBIN
Water insoluble product of heme metabolismTaken up by liver and conjugated to become water soluble so it can be excreted in bile and into bowel.
Patient looks Jaundiced if bilirubin >2.5
If patient is vomiting GREEN, then they have bowel obstruction below the level of the Ampulla of Vater.
WHAT IS THE DEAL WITH DIRECT AND INDIRECT BILIRUBIN?
Prehepatic disease (eg hemolysis) causes high bilirubin which is non conjugated ie. Indirect fraction higherHepatic disease causes increased conjugated and unconjugated bilirubin
Post hepatic disease eg. Gallstones have increased conjugated (direct) bilirubin and lead to dark urine and pale stool
TESTS OF LIVER FUNCTION
PROTHROMBIN TIME/ INR
ALBUMIN
PROTHROMBIN TIME/INR
Measure of the Vitamin K dependent clotting factors ie. II, VII, IX and X.The liver is involved in activating Vitamin K. Therefore in liver damage, these clotting factors cannot be produced.
Before you believe that prolonged INR is due to liver disease just make sure the patient has adequate Vitamin K by giving 10mg sc.
Giving Vitamin K has no effect on INR if patient has impaired synthetic function.
ALBUMIN
Albumin has a half life of 21 days, so the drop that occurs with hepatic dysfunction does not occur acutely
That said, acute illness can cause albumin to drop rapidly – a process thought to be due to cytokines increasing the rate of albumin metabolism
HOWEVER, don’t forget that low albumin also occurs in NEPHROTIC syndrome, so always check the urine for protein
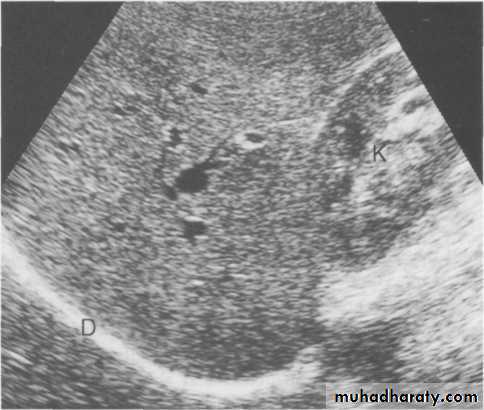
Radiological examination of the liver
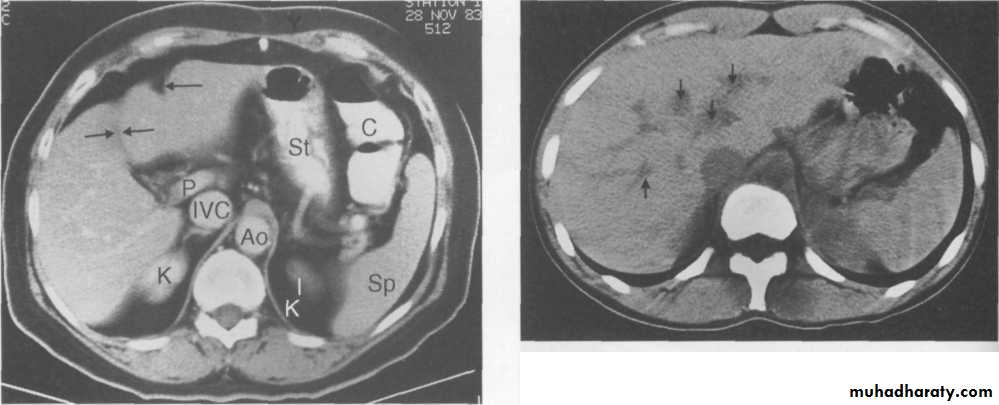
Ultrasound of the liver.Ultrasound of normal liver. Longitudinal scan showing uniform echo pattern interspersed with bright echoes of portal triads and echo-free areas of hepatic and portal veins. D, diaphragm; K, right kidney
CT.scan
CT scan showing unopacified hepatic veins (arrows) which should not be confused with metastases.
MRI of the liver
Magnetic resonance imaging is used as a problem-solving technique to give additional information to ultrasound and CT. Axial sections give images akin to CT but images can also be obtained in the coronal and sagittal planes. By using special sequences information can also be obtained on the arterial and venous circulation of the liver.Radionuclide liver imaging
Radionuclide liver scanning (99mTc-labelled sulphur or tin colloid) has been almost completely replaced by ultrasound, CT and MRI. The hepatobiliary agents which also show the liver parenchyma, but their primary indication is to show disease of the extrahepatic biliary system.Percutaneous transhepatic cholangiography
Percutaneous transhepatic cholangiography is accomplished by injecting contrast material under fluoroscopic vision through a narrow gauge needle placed in the parenchyma of the liver. has the advantage of allowing the operator to institute biliary drainage if necessary. It is increasingly reserved for patients with biliary obstruction who need permanent or temporary biliary drainage. Needle biopsy of masses, drainage of fluid collections, and placement of external and internal drainage (choledochoduodenal) stents all can be accomplished percutaneously.
Magnetic resonance cholangiopancreatography (MRCP)
Special sequences enable the biliary duct system to be visualized directly without the need for any contrast agentLiver trauma
Largest organ,2nd most common injured,
Blunt trauma most common
Friable parenchyma, thin capsule, fixed position in relation to spine
prone to blunt injury .Right lobe larger, closer to ribs.
more injury
In children
compliant ribs,
transmitted force
Mechanisms of injury:-
simple compression against ribs, spine,ligamentous attachment to diaphragm and the posterior abdominal wall ,shear forces during deceleration injury
High-velocity bullet injuries
burst injuries with distant contusions and parenchymal disruption.
Associations
management
Initial resuscitation as per ATLS protocol
It is important to note the mechanism of injury
Clinical picture may vary from mild RUQ pain through to peritonism to haemorrhagic shockStable patients undergo CT imaging
Unstable patients require resuscitation and laparotomyLow-velocity penetrating injury
1.Stab wounds2.percutaneous biopsy
3.cholangiography
4.biliary drainage,
capsular tears, hematoma, bile leaks, arteriobiliary fistulas, and hemoperitoneum, arterial aneurysms
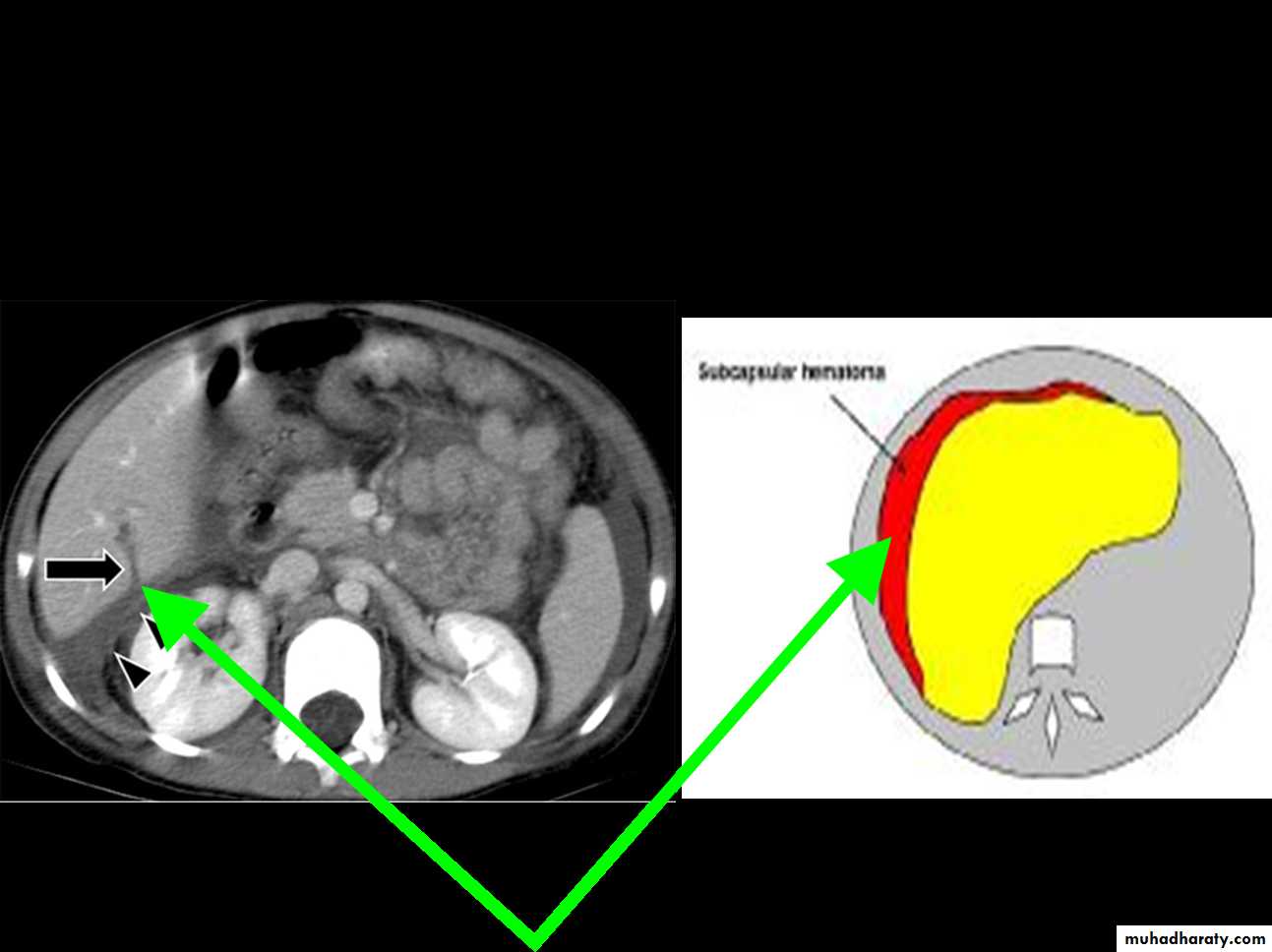
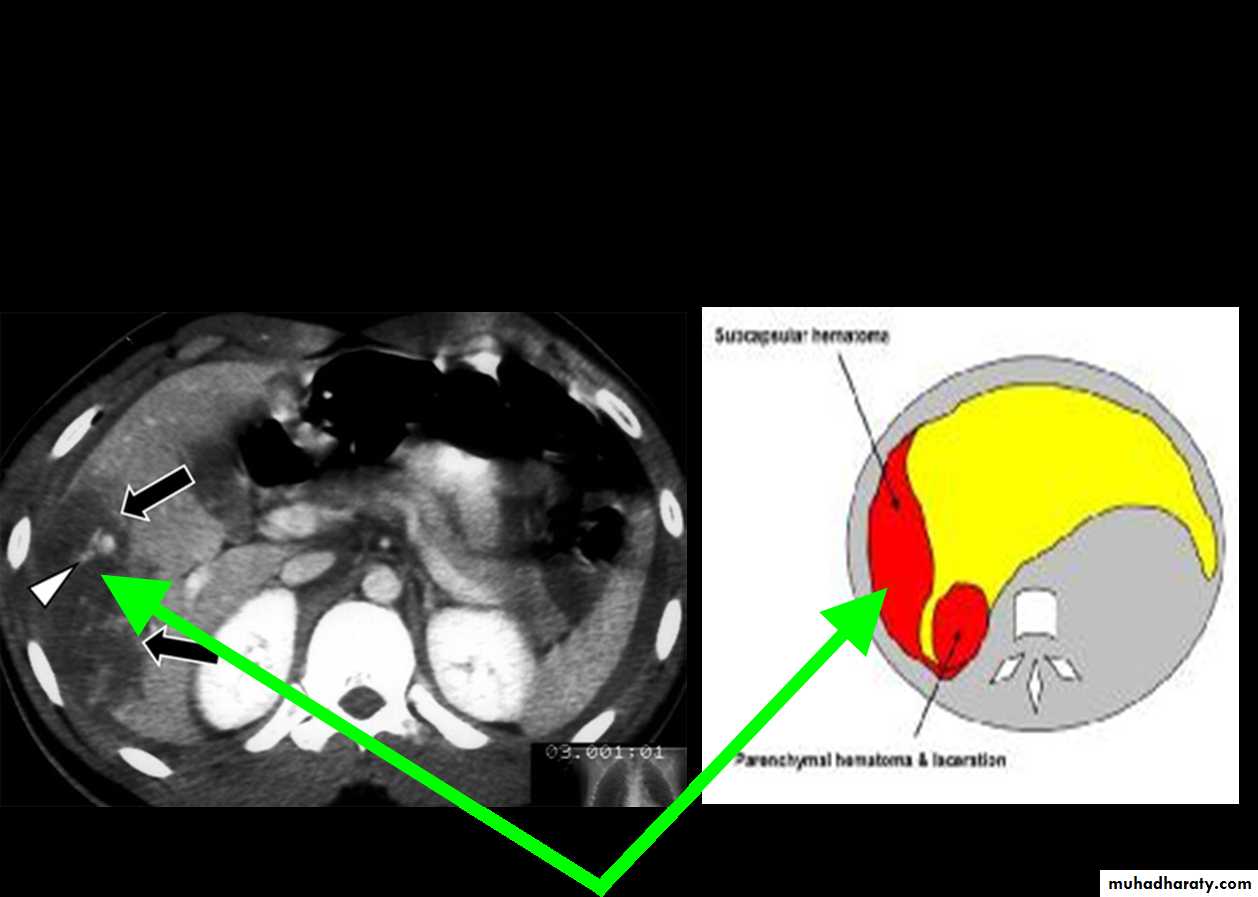
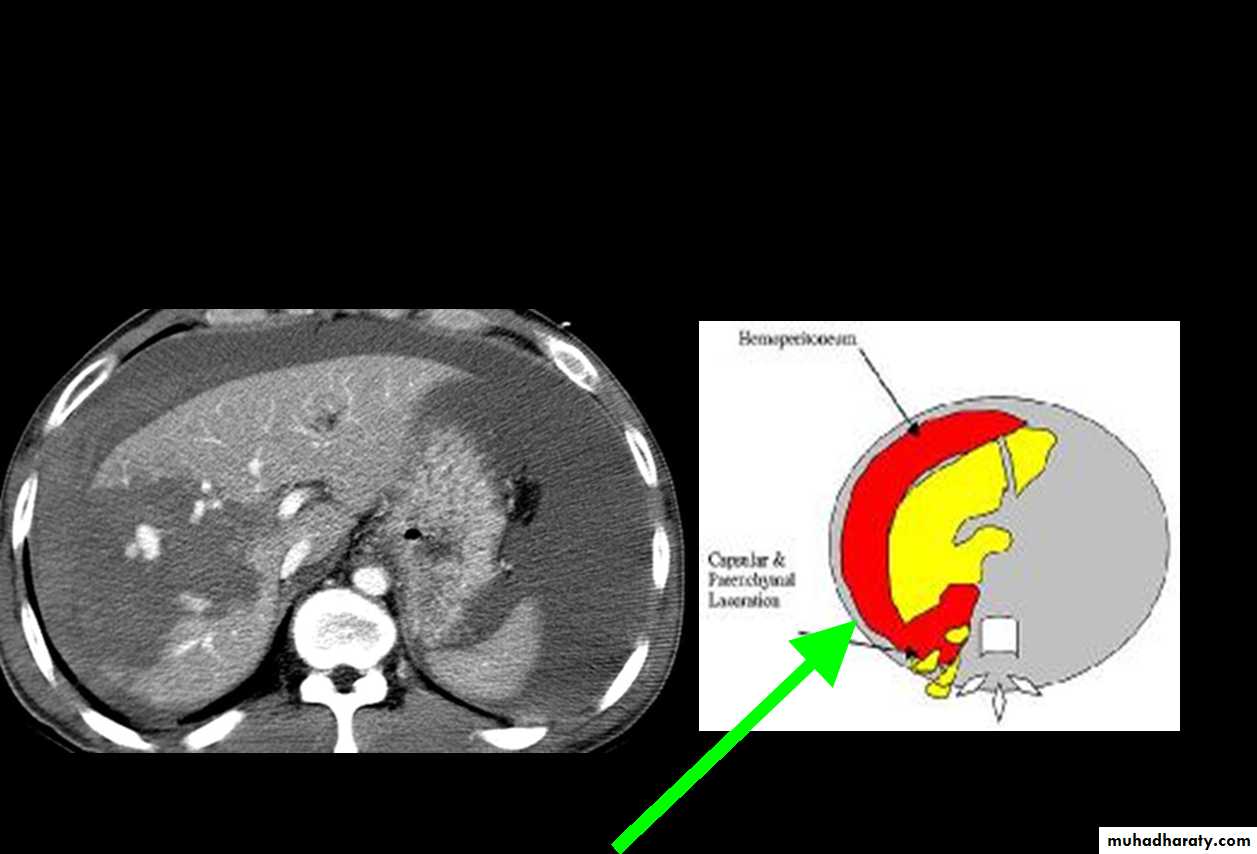
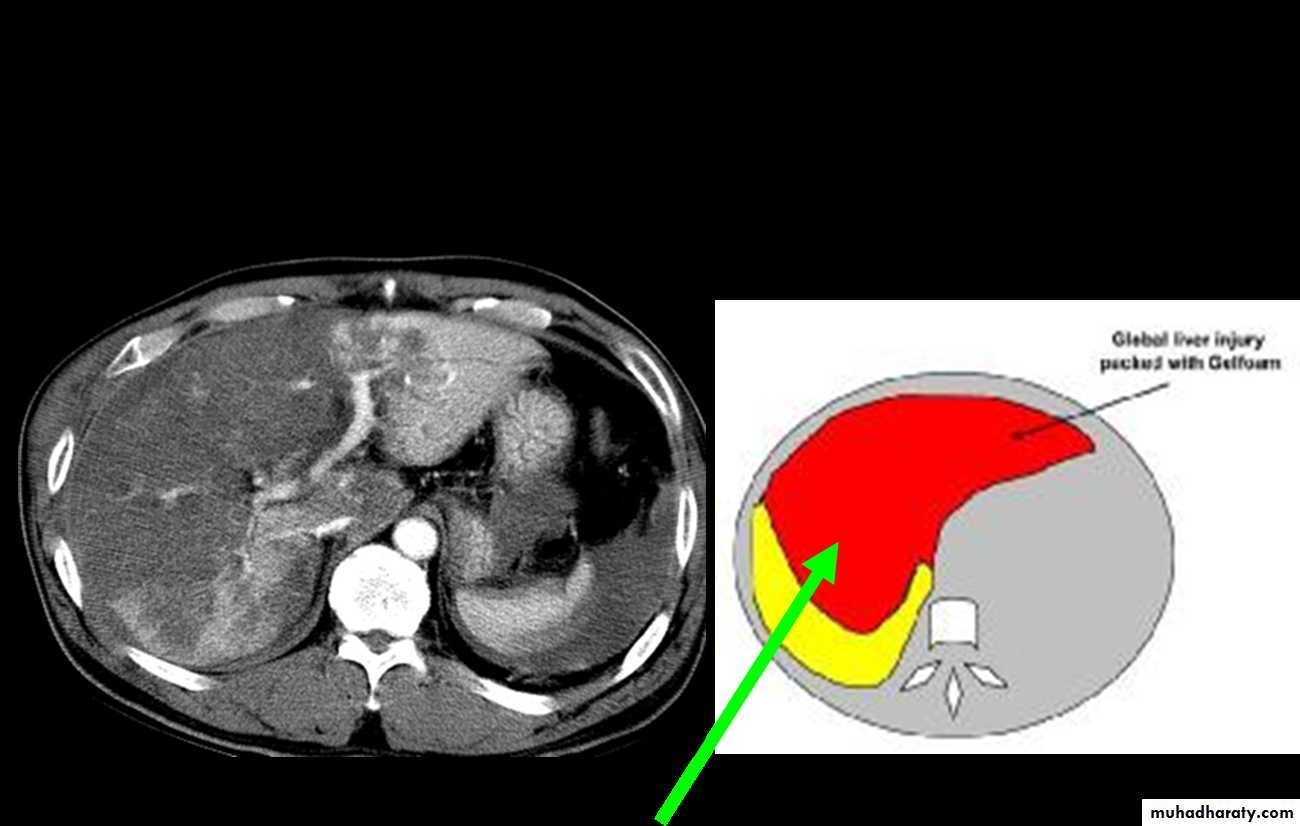
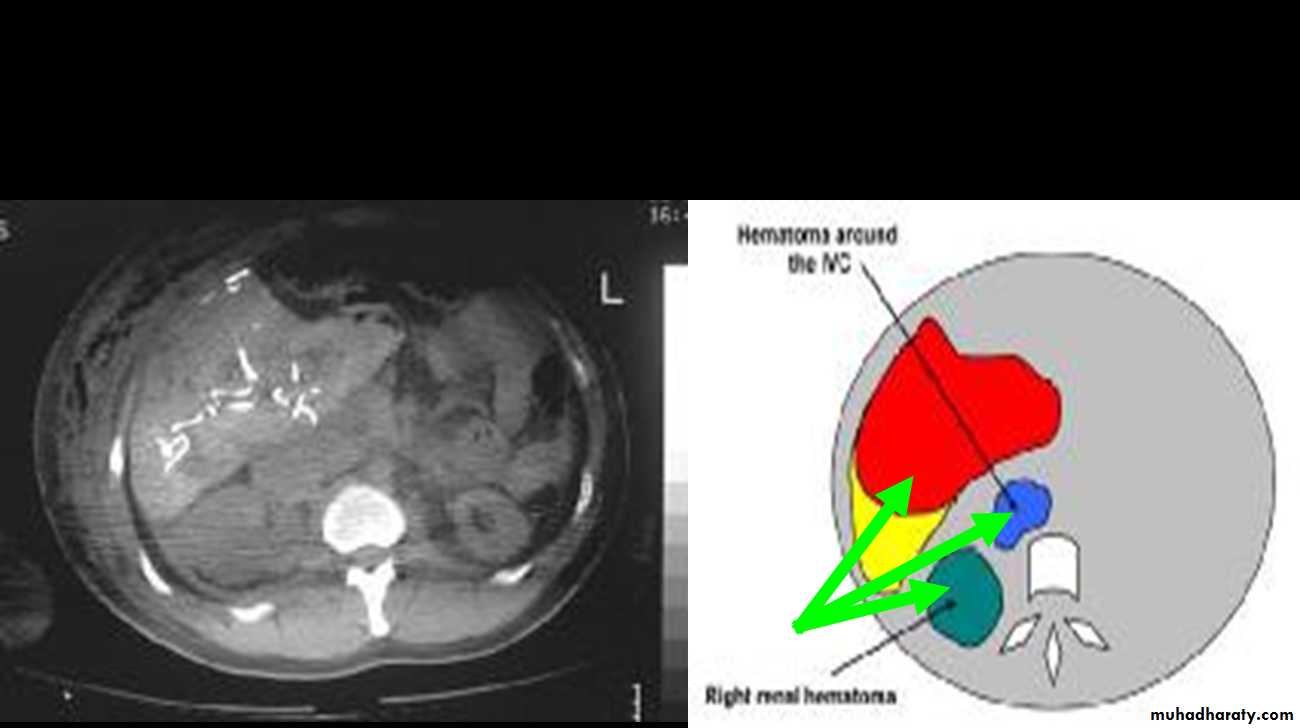
Types of injury
Parenchymal damage
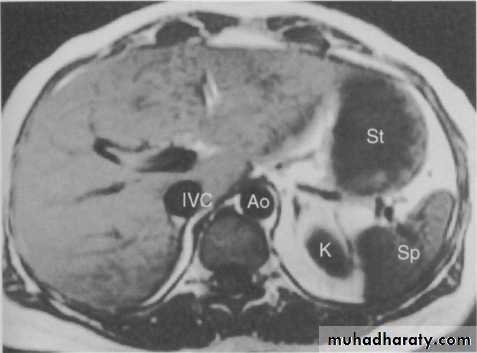
Subcapsular hematoma
Laceration
Contusion
Hepatic vascular disruption
Bile duct injury
CT Scans
Accurate in localizing the site of liver injury and any associated injuries
Used to monitor healing
CT criteria for staging liver trauma uses AAST liver injury scaleGrades 1-6
Classification(AASTI-Subcapsular hematoma<1cm, superficial laceration<1cm deep.
Treatment
ConservativeBlunt liver trauma,
Haemodynamically stable
No other injuries requiring surgery
Surgical
Penetrating injuries
Haemodynamically unstable
Other injuries requiring surgery
HYDATID CYST DISEASE
Hydatid disease is a worldwide zoonosis produced by the larval stage of the Echinococcus tapeworm .The two main types of hydatid disease are caused by E granulosus and E multilocularis.
E granulosus is commonly seen in the great grazing regions of the world—particularly the Mediterranean region, Africa, South America, the Middle East, Australia, and New Zealand—and is the most frequently encountered type of hydatid disease in humans
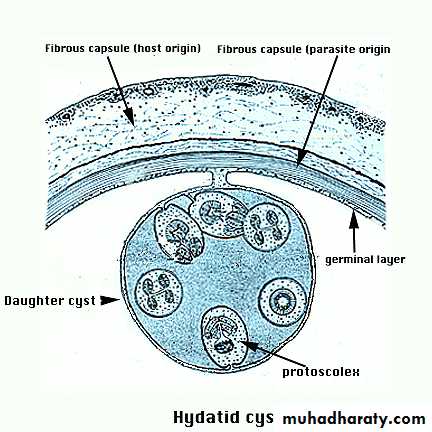
The hydatid cyst has three layers:
(a) the outer pericyst, composed of modified host cells that form a dense and fibrous protective zone;(b) the middle laminated membrane, which is acellular and allows the passage of nutrients;
(c) the inner germinal layer, where the scolices (the larval stage of the parasite) and the laminated membrane are produced.
• Daughter vesicles (brood capsules) are small spheres that contain the protoscolices and are formed from rests of the germinal layer. Before becoming daughter cysts, these daughter vesicles are attached by a pedicle to the germinal layer of the mother cyst. At gross examination, the vesicles resemble a bunch of grapes
Hydatid disease involves the liver in approximately 75% of cases, the lung in 15%, and other anatomic locations in 10%
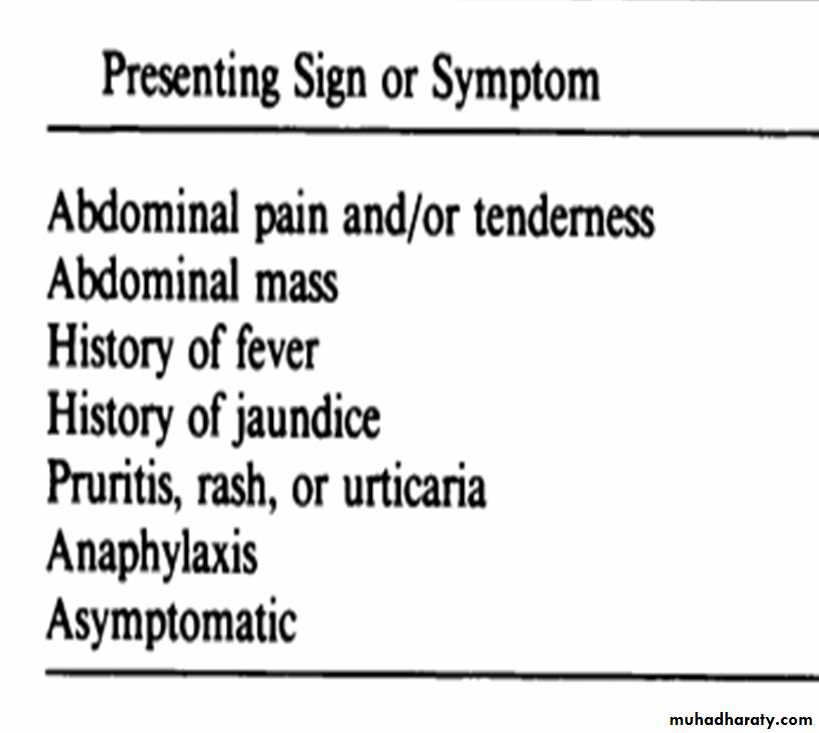
The clinical features are highly variable. The spectrum of symptoms depends on the following:
Involved organs
Size of cysts and their sites within the affected organ or organs
Interaction between the expanding cysts and adjacent organ structures, particularly bile ducts and the vascular system of the liver
Symptoms due to pressure usually take a long time to manifest, except when they occur in the brain .
Most symptomatic cysts are larger than 5 cm in diameter.
Bacterial infection of cysts and spread of protoscolices and larval material into bile ducts or blood vessels
Immunologic reactions such as asthma, anaphylaxis, or membranous nephropathy secondary to release of antigenic material
The right lobe is the most frequently involved portion of the liver.
Once in the human liver, cysts grow to 1 cm during the first 6 months and 2–3 cm annually thereafter, depending on host tissue resistance.Clinical presentation of liver disease
Work Up
Generally, routine laboratory tests do not show specific results.• In patients with rupture of the cyst in the biliary tree, marked and transient elevation of cholestatic enzyme levels occurs, often in association with hyperamylasemia and eosinophilia (as many as 60%).
• Indirect hemagglutination test and enzyme-linked immunosorbent assay are the most widely used methods for detection of anti-Echinococcus antibodies (immunoglobulin G [IgG]).These tests give false positive results in cases of schistosomiasis and nematode infestations that is why they are not specific for diagnosing hydatidosis. Immunoelectrophoresis : depends on the formation of specific arc of precipitation ( called arc 5 ) which is highly specific and can be used to exclude cross-reactions caused by noncestode parasites
Imaging Studies:
Plain radiography
Ultrasound examination
CT scaning
MRI
Management Options
Medical .Surgery.
PAIR.
Medical treatment
Indications: Chemotherapy is indicated in patients with primary liver or lung cysts that are inoperable (because of location or medical condition), patients with cysts in 2 or more organs, and peritoneal cysts.Chemotherapeutic agents: Two benzimidazoles are used, albendazole and mebendazole. Albendazole is administered in several 1-month oral doses (10-15 mg/kg/d) separated by 14-day intervals. The optimal period of treatment ranges from 3-6 months, with no further increase in the incidence of adverse effects if this period is prolonged. Mebendazole is also administered for 3-6 months orally in dosages of 40-50 mg/kg/d
Contraindications: Early pregnancy, bone marrow suppression, chronic hepatic disease, large cysts with the risk of rupture, and inactive or calcified cysts are contraindications. A relative contraindication is bone cysts because of the significantly decreased response.
Outcome : Response rates in 1000 treated patients were that 30% had cyst disappearance (cure), 30-50% had a decrease in the size of the cyst (improvement), and 20-40% had no changes. Also, younger adults responded better than older adults
PAIR
This technique, performed using either ultrasound or CT guidance, involves aspiration of the contents via a special cannula, followed by injection of a scolicidal agent for at least 15 minutes, and then reaspiration of the cystic contents. The cyst is then filled with isotonic sodium chloride solution. Perioperative treatment with a benzimidazole is mandatory (4 d prior to the procedure and 1-3 mo after).The cysts should be larger than 5 cm in diameter
Indications: Inoperable patients; patients refusing surgery; multiple cysts in segment I, II, and III of the liver; and relapse after surgery or chemotherapy are indications for the PAIR technique
Contraindications: Early pregnancy, lung cysts, inaccessible cysts, superficially located cysts (risk of spillage), and cysts communicating with the biliary tree (risk of sclerosing cholangitis from the scolecoidal agent).
Surgical Management
Indications:1-Large liver cysts with multiple daughter cysts; superficially located single liver cysts that may rupture (traumatically or spontaneously).
2-liver cysts with biliary tree communication or pressure effects on vital organs or structures.
3-infected cysts .
4-cysts in lungs, brain, kidneys, eyes, bones
Concomitant treatment with benzimidazoles (albendazole or mebendazole) has been reported to reduce the risk of secondary echinococcosis. Treatment is started 4 days preoperatively and lasts for 1 month.
Contraindications: General contraindications to surgical procedures (eg, extremes of age, pregnancy, severe preexisting medical conditions); multiple cysts in multiple organs; cysts that are difficult to access; dead cysts; calcified cysts; and very small cysts are contraindications.
Complications
1-All the usual complications related to the surgical procedure and anesthesia2-Related to the parasite Recurrence
Metastasis
Infection
Spillage and seeding (secondary echinococcosis) - Allergic reaction or anaphylactic shock
3-Related to the medical treatment
Hepatotoxicity
Anemia
Thrombocytopenia
Alopecia
Embryotoxicity
Teratogenicity
Complications , cont
4-Related to PAIR
Hemorrhage
Mechanical damage to other tissue
Infections
Allergic reaction or anaphylactic shock
Persistence of daughter cysts
Sudden intracystic decompression leading to biliary fistulas
5-Related to scolicidal agents - Chemical sclerosing cholangitis
Liver tumor
BenignMalignant
HemangiomaFocal nodular hyperplasia
Adenoma
Liver cysts
Primary liver cancers
Hepatocellular carcinomaFibrolamellar carcinoma
Hepatoblastoma
2. Metastases
Benign Liver Lesions
HemangiomaFocal nodular hyperplasia
Adenoma
Cysts
HemangiomaClinical Features
The commonest liver tumor5% of autopsies
Usually single small
Well demarcated capsule
Usually asymptomatic
Diagnosis and Management
DiagnosisUS: echogenic spot, well demarcated
CT: venous enhancement from periphery to center
MRI: high intensity area
No need for FNA
Treatment
No need for treatment
Focal Nodular Hyperplasia (FNH)Clinical Features
Benign nodule formation of normal liver tissueCentral stellate scar
More common in young and middle age women
No relation with sex hormones
Usually asymptomatic
May cause minimal pain
Focal Nodular Hyperplasia (FNH)Diagnosis and Management
Diagnosis:US: Nodule with varying echogenicity
CT: Hypervascular mass with central scar
MRI: iso or hypo intense
FNA: Normal hepatocytes and Kupffer cells with central core.
Treatment:
No treatment necessaryPregnancy and hormones OK
Hepatic AdenomaClinical features
Benign neoplasm composed of normal hepatocytes no portal tract, central veins, or bile ducts
More common in women
Associated with contraceptive hormones
Usually asymptomatic but may have RUQ pain
May presents with rupture, hemorrhage, or malignant transformation (very rare)
Hepatic AdenomaDiagnosis and Management
DXUS: filling defect
CT: Diffuse arterial enhancement
MRI: hypo or hyper intense lesion
FNA : may be needed
Tx
Stop hormones
Observe every 6m for 2 y
If no regression then surgical excision
Malignant Liver Tumors
Hepatocellular carcinoma (HCC)Fibro-lamellar carcinoma of the liver
Hepatoblastoma
Intrahepatic cholangiocarcinoma
Others
HCC: Incidence
The most common primary liver cancer
Increasing in US and all the world
HCC: Risk Factors
The most important risk factor is cirrhosis from any cause:Hepatitis B (integrates in DNA)
Hepatitis C
Alcohol
Aflatoxin
Other
HCC: labs
Labs of liver cirrhosisAFP (Alfa feto protein)
Is an HCC tumor markerValues more than 100ng/ml are highly suggestive of HCC
Elevation seen in more than 70% of pt
HCC: Diagnosis
Clinical presentationElevated AFP
US
Triphasic CT scan: very early arterial perfusion
MRI
Biopsy
HCC: Resection
Feasible for small tumors with preserved liver function (no jaundice or portal HTN)Recurrence rate is high
Secondary Liver Metastases
The most common site for blood born metastasesCommon primaries : colon, breast, lung, stomach, pancreases, and melanoma
Mild cholestatic picture (ALP, LDH) with preserved liver function
Dx imaging or FNA
Treatment depends on the primary cancer
In some cases resection or chemoembolization is possible