
Lecture-2
Work of Breathing
Under resting conditions, the respiratory muscles normally perform “work” to cause
inspiration but not to cause expiration. The work of inspiration can be divided into three parts
that required: (1) to expand the lungs against the lung and chest elastic forces, called
compliance work or elastic work; (2) to overcome the viscosity of the lung and chest wall
structures, called tissue resistance work; and (3) to overcome airway resistance to movement
of air into the lungs, called airway resistance work.
●During quite breathing, 3-5% of total energy of the body is spent for respiration, while in
heavy exercise; it increases up to 50 folds.
Pulmonary Volumes (fig 5)
A lung volume refers to a basic volume of the lung, the following lung volumes can be
measured directly or indirectly with a spirometer:
1. The tidal volume (VT) is the volume of air inspired or expired with each normal breath; it
amounts to about 500 ml in the adult male.
2. The inspiratory reserve volume (IRV) is the extra volume of air that can be inspired
over and above the normal tidal volume when the person inspires with full force; it is usually
equal to about 3000 ml.
3. The expiratory reserve volume (ERV) is the maximum extra volume of air that can be
expired by forceful expiration after the end of a normal tidal expiration; this normally
amounts to about 1100 ml.
4. The residual volume (RV) is the volume of air remaining in the lungs after the most
forceful expiration; this volume averages about 1200 ml.
Pulmonary Capacities (fig 5)
Lung capacities are the sum of two or more basic lung volumes.
1-Inspiratory Capacity (IC): the maximal volume of air that can be inspired from normal
end-expiration or VT + IRV (about 3500 ml).
2-The functional residual capacity (FRC): equals the ERV + RV. This is the amount of air
that remains in the lungs at the end of normal expiration (about 2300 ml).
3-The vital capacity: equals the IRV+ VT+ ERV. This is the maximum amount of air a
person can expel from the lungs after first filling the lungs to their maximum extent (about
4600 ml).
4. The total lung capacity is the maximum volume to which the lungs can be expanded with
the greatest possible effort (about 5800 ml); it is equal to the vital capacity plus the residual
volume.
●All pulmonary volumes and capacities are about 20 to 25 per cent less in women than in
men, and they are greater in large and athletic people than in small and asthenic people.

● Functional residual capacity cannot be determined by spirometry directly but can be
determined by using helium dilution method.
●The residual volume (RV) can be determined by subtracting expiratory reserve volume
(ERV), as measured by normal spirometry, from the FRC (RV = FRC – ERV).
●The total lung capacity (TLC) can be determined by adding the inspiratory capacity (IC)
to the FRC (TLC = FRC + IC).
●The minute respiratory volume is the total amount of new air moved into the respiratory
passages each minute; this is equal to the tidal volume times the respiratory rate per minute.
The tidal volume (500 ml) multiplied by the respiratory rate (12/min) = 6000ml/minute.
Alveolar Ventilation
It is the rate at which new air reaches the gas exchange areas of the lungs which are the
alveoli, alveolar sacs, alveolar ducts, and respiratory bronchioles.
“Dead Space” and Its Effect on Alveolar Ventilation
The dead space is the space where no gas exchange occurs and on expiration, the air in the
dead space is expired first. It is either normal or called anatomically (150 ml) which are nose,
pharynx, larynx, trachea, bronchi, bronchioles); or physiological dead space whereby some
alveoli are not functional because of absent or partial blood supply (normally it should be
zero).
So the total dead space is the sum of anatomical and physiological dead spaces and so
normally equals to 150 ml and this increases slightly with age.
So the alveolar ventilation per minute is the total volume of new air entering the alveoli and
adjacent gas exchange areas each minute.
The volume of alveolar ventilation per minute= respiration rate per minute*{tidal volume-
dead space volume}
12*{500-150} =12*300= 4200 ml/min.
Functions of the Respiratory passageways (fig 6)
The air is distributed to the lungs by way of the trachea, bronchi, and bronchioles.
To keep the trachea from collapsing there are multiple cartilage rings extend about five sixths
of the way around the trachea. In the walls of the bronchi there are less extensive curved
cartilage plates also maintain a reasonable amount of rigidity yet. These plates become
progressively less extensive in the later generations of bronchi and are gone in the
bronchioles, bronchioles kept open as alveoli due to transpulmonary pressure.
●All wall areas of the trachea and bronchi are not occupied by cartilage plates are composed
mainly of smooth muscle. Also, the walls of the bronchioles consist of smooth muscle except
the respiratory bronchiole, which are mainly pulmonary epithelium and underlying fibrous
tissue plus a few smooth muscle fibers.

Resistance to airflow in the bronchial tree: In normal quiet breathing, less than 1cm of
water pressure gradient need to cause enough airflow from the alveoli to the atmosphere.
The greatest airflow resistance occurs in the larger bronchioles (bronchi near the trachea)
than in the minute air passages of the terminal bronchioles, this due to that there are few of
these larger bronchi in comparison with terminal bronchioles through each of which only a
minute amount of air must pass, but in disease conditions the minute air passages play a
greater role in determining air way resistance because they are easily occluded.
Nerve stimulation
“Sympathetic” Dilation of the Bronchioles: Direct control of the bronchioles by
sympathetic nerve fibers is weak. However, the bronchial tree is exposed to norepinephrine
and epinephrine released into the blood by sympathetic stimulation of the adrenal gland
medullae. Both these hormones especially epinephrine, because of its greater stimulation of
beta-adrenergic receptors—cause dilation of the bronchial tree.
Parasympathetic Constriction of the Bronchioles:
A few parasympathetic nerve fibers derived from the vagus nerves penetrate the lung
parenchyma secrete acetylcholine which causes mild to moderate constriction of the
bronchioles.
●Sometimes the parasympathetic nerves are also activated by reflexes that originate in the
lungs. This initiated by noxious gases, dust, cigarette smoke, or bronchial infection leading to
irritate the epithelial membrane of the respiratory passageways and constrict them.
Local secretory factors often cause bronchiolar constriction: Several substances formed
in the lungs themselves are causing bronchiolar constriction as histamine and slow reactive
substance of anaphylaxis. Both of these are released in the lung tissues by mast cells during
allergic reactions, especially those caused by pollen in the air causing the airway obstruction
that occurs in allergic asthma.
The role of Mucus and Cilia Lining the Respiratory Passageways
All the respiratory passages, from the nose to the terminal bronchioles, are kept moist by a
layer of mucus that coats the entire surface. The mucus is secreted partly by individual
mucous goblet cells in the epithelial lining of the passages and partly by small submucosal
glands. In addition to keeping the surfaces moist, the mucus traps small particles out of the
inspired air and preventing them reaching the alveoli.
The mucus itself is removed from the passages in the following manner: The entire surface
of the respiratory passages, both in the nose and in the lower passages down as far as the
terminal bronchioles, is lined with ciliated epithelium, and the cilia in the lungs moving
upward toward the pharynx. While the cilia in the nose move downward. This continual
moving cause the mucus and its entrapping particles are either swallowed or coughed to the
exterior.

Cough Reflex
The bronchi and trachea are so sensitive to light touch send afferent nerve impulses pass
through the vagus nerves to the medulla of the brain, then automatically causing the
following effect.
First, up to 2.5 L of air are rapidly inspired.
Second, the epiglottis closes, and the vocal cords shut tightly to entrap the air within the
lungs.
Third, the abdominal muscles contract forcefully, pushing against the diaphragm while other
expiratory muscles, such as the internal intercostals, also contract forcefully. Consequently,
the pressure in the lungs rises rapidly to as much as 100 mm Hg or more.
Fourth, the vocal cords and the epiglottis suddenly open widely, so that airs under this high
pressure in the lungs blow up outward.
Indeed, sometimes this air is expelled at velocities ranging from 75 to 100 miles per hour.
The noncartilaginous parts of bronchi and trachea invaginate inward during cough, so that
the exploding air actually passes through bronchial and tracheal slits.
Sneeze Reflex
The initiating stimulus of the sneeze reflex is irritation in the nasal passageways, the afferent
impulses pass in the fifth cranial nerve to the medulla, where the reflex is triggered. A series
of reactions similar to those for the cough reflex takes place; however, the uvula is
depressed, so that large amounts of air pass rapidly through the nose, thus helping to clear the
nasal passages of foreign matter.
Normal Respiratory Functions of the Nose
As air passes through the nose, three normal respiratory functions are performed by the nasal
cavities:
(1) The air is warmed by the extensive surfaces of the conchae and septum.
(2) The air is almost completely humidified even before it passes beyond the nose.
(3) The air is partially filtered by the hairs at the entrance to the nostrils.
Vocalization
Speech involves not only the respiratory system but also (1) specific speech nervous control
centers in the cerebral cortex (2) respiratory control centers of the brain; and (3) the
articulation and resonance structures of the mouth and nasal cavities. Speech is composed of
two mechanical functions: (1) phonation, which is achieved by the larynx, and (2)
articulation, which is achieved by the structures of the mouth.
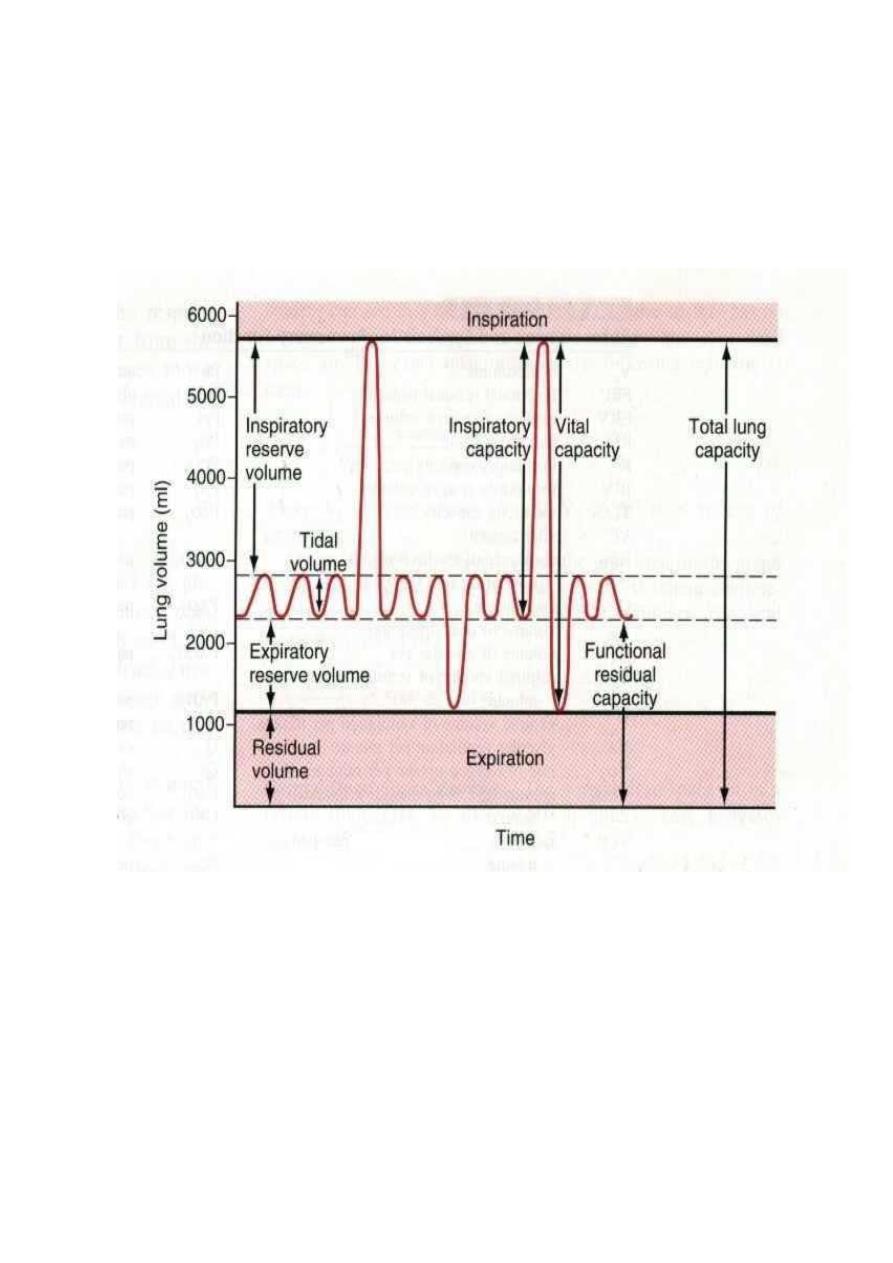
Fig-5 Diagram showing respiratory excursions during normal breathing and during maximal
inspiration and maximal expiration
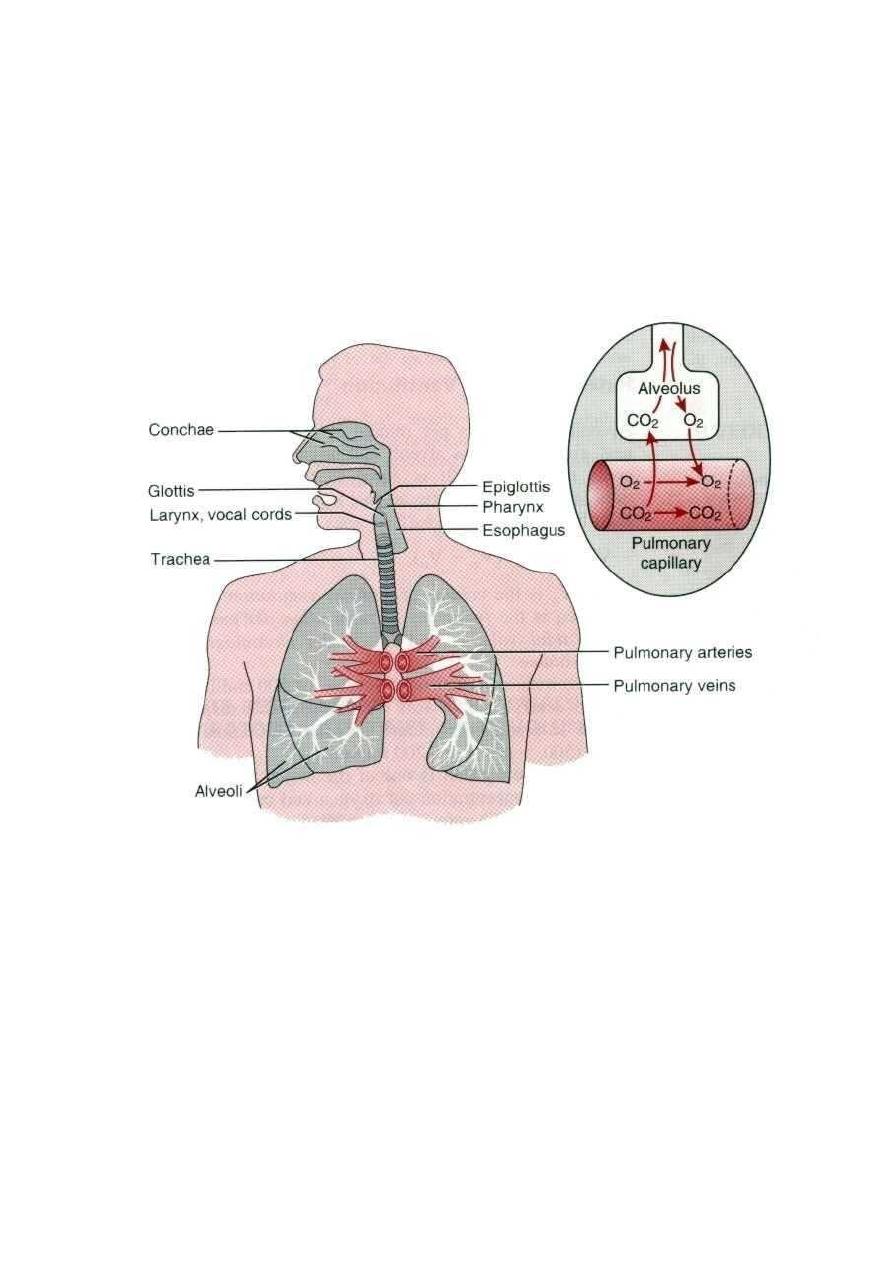
Fig -6 Respiratory passages
