Histology Dr.Luma Al-Allaf
5-11-2017Salivary Glands
Are exocrine gland, they empty their secretion into the oral cavity by their ducts. Classified into minor and major. These glands may contain serous cells or mucus-secreting cells or mixture of both.
Minor salivary glands:
found mainly in the sub mucosa of the mouth, empty their secretions into the mouth by short ducts, they are named according to their locations (buccal, labial, palatine, lingual and tonsilar).
All are characterized by:-
No capsule
Branched, tubular, acinar in type
No intercalated duct
All have the same function, secretion of saliva continuously to keep the mucous membrane of the mouth moist.
Major salivary glands:
3 large pairs of gland: Parotid, Submandibular, Sublingual.
Also called extrinsic salivary glands located outside the oral cavity, have long ducts leading to the mouth, they secrete the saliva upon non continuous stimulation, they respond to various stimulation like the presence of food in the mouth, smelling or seeing the food, the saliva represents the secretion of all the salivary glands about one and half liter per day, 90% water and contains important enzymes of different concentrations also Ig for killing the bacteria.
Parotid gland:
Are largest pair of salivary gland situated below and in front of pinna on each side of the face they are flat and well- capsulated, the facial nerve runs into the gland dividing it into superficial and deep portion, the duct of the gland open into the mouth opposite to the upper second molar teeth.
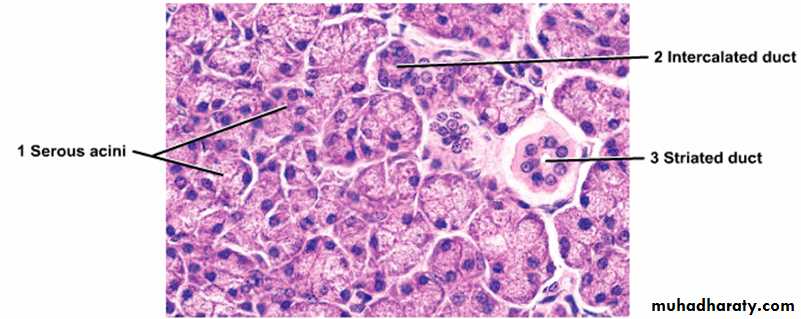
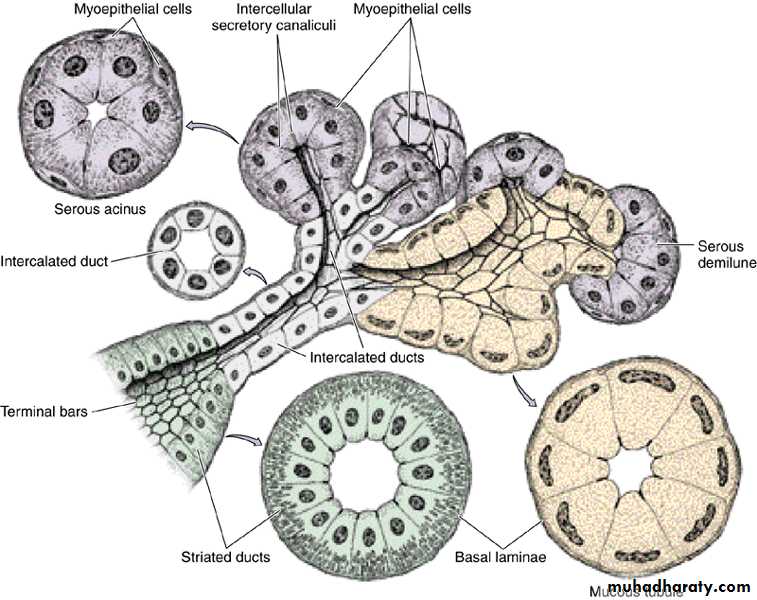
Histologically: Parotid gland surrounded by fibrous tissue capsule from which fibrous septa dividing the gland into lobes and each lobe is subdivided into many lobules, one of the characteristic feature of the gland is the presence of adipose tissue, each lobule composed of branched tubulo alveolar acini of serous type, purely secrete serous fluid. Serous cells are cubidal or pyramidal surrounding small lumen, have spherical centrally located nucleus, luminal surface of the cell cytoplasm contain zymogen granules that stain purple by using H& E stain while RER found at the basal part of the cytoplasm, the duct within the lobule called intralobular consist of intercalated and striated duct.
The intercalated duct lined with low cuboidal epithelium, striated duct lined by tall columnar epithelium showing vertical striation which is produced by large number of rod- shaped mitochondria. They leads to interlobular ducts which run in the interlobular septum then they unite to form the main excretory duct that empty into the oral cavity.
Submandibular gland:
The gland lie on each side of the neck just below the mandible, their duct open into the floor of the mouth on each side of the frenulum of the tongue just behind the lower incisor teeth. The gland is surrounded by fibrous capsule and from which fibrous septa divide the gland into lobes and lobules, no adipose tissue. The secretory part composed of tubulo- alveolar acini of serous and mucous type but majority are serous alveoli.
Mucous alveoli:
Mucous cells are polyhedral.
Surrounding large lumen.
Pale- staining cytoplasm.
Flat nucleus lie at the base of the cell (eccentric).
Clear boundries between the cells.
Serous alveoli:
Serous cells are cuboidal or pyramidal.
Surrounding narrow lumen.
Dark cytoplasm filled with zymogen granules.
Boundaries between the cells are not clear
In the sub mandibular gland the serous acini arranged as a crescent or demilune outside the end of mucous alveoli called serous demilune.
The duct system : secretory acini empty into the intercalated ducts lined by dark stained cuboidal epithelium, they merge to form striated ducts lined by tall columnar light stained cells with ertical striation which fuse to form larger interlobular duct (lined by pseudostratified epithelium), the inter lobular ducts join to form the major duct lined y stratified epithelium.
Intercalated duct
Cuboidal
Dark staining
No striation
Striated duct
Tall columnar
Pale staining
Striated basal cytoplasm
Sublingual gland
2 glands lie in the floor of the mouth on either side of the frenulum of the tongue, it is the smallest gland, no capsule and the gland is divided into many lobes which differ in size, contain mainly mucous acini some of which show serous demilune.
The duct system show intralobular ducts (lacking the striated or inter calated appearance) &interlobular ducts all drain into a single large excretory duct open in the mouth near to or with submandibular duct.
OESOPHAGUS:
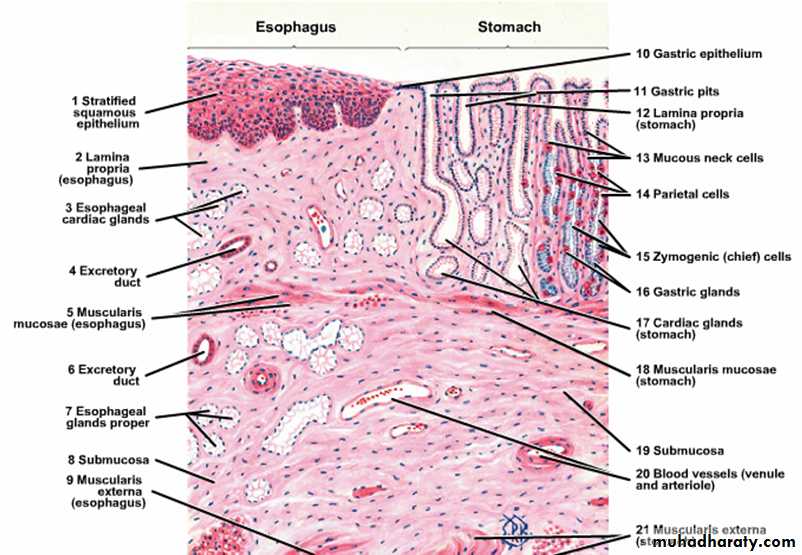
Is a striated muscular tube about 25 cm long extends from the pharynx at the level of cricoid cartilage to the stomach, consist of 4 layers:
Mucosa: is composed of stratified squamous epithelium non keratinized that is continuous above with that lining the pharynx while from below at the area of junction of the esophagus with the stomach there is an abrupt change of stratified squamous epithelium to the simple columnar epithelium.
Esophageal lamina propria consists of collagen fibers and fibroblasts with scattered lymphocytes, eosinophils, mast cells and plasma cells.
Muscularis mucosae arranged haphazardly in the upper part and longitudinally in the lower part of the esophagus.
Submucosa: composed of tubulo-alveolar mucous gland scattered along the esophagus called esophageal gland they lubricate the esophageal content during the swallowing, parasympathetic nerve plexus present in the submucosa ( called submucosal or Miessner’s plexus) that control the activity of the glands and smooth muscle in addition to lymphatic vessels, nerves and blood vessels all are found in the submucosa.
Muscular coat: consist of inner circular and outer longitudinal, in the upper third of esophagus muscles are skeletal, in the lower the muscles are smooth, in the middle third there is mixture of both skeletal and smooth muscles fibers. Myenteric plexus (Aurbach’s plexus) which is parasympathetic nerve plexus is found between the circular and longitudinal muscle layers of the muscular coat to control the activity of muscles fibers, there is thickening of the inner circular muscular layer at the cardio-esophageal junction forming the (gastro-esophageal sphincter) which prevents the content of the stomach to reflex into the esophagus at this junction
there is an abrupt transition of squamous epithelium of the esophagus to columnar epithelium of the stomach.
Fibrosa: loose connective tissue with large blood vessels & adipose tissue support the esophagus.
The lower esophagus characterized by the presence of esophageal cardiac glands in the region of lamina propria in addition to the esophageal glands in the region of submucosa which present in the upper and lower esophagus.
The Stomach
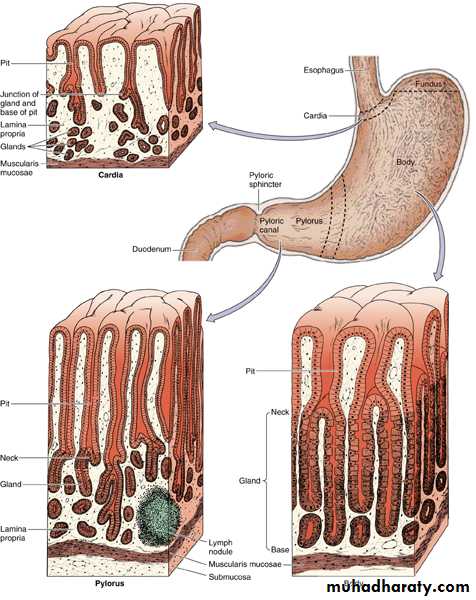
It is a dilated portion of the digestive tract, it’s main function is to continue the digestion of CHO and to change it into semi liquid mass called chyme, also initiate the digestion of protein and lipids, it is a distensible organ end at the pyloric sphincter which prevents the reflux of it’s contents until it is converted into chimeThe stomach is divided into 4 regions: Cardia, fundus, body and pylorus.
Histological structure:
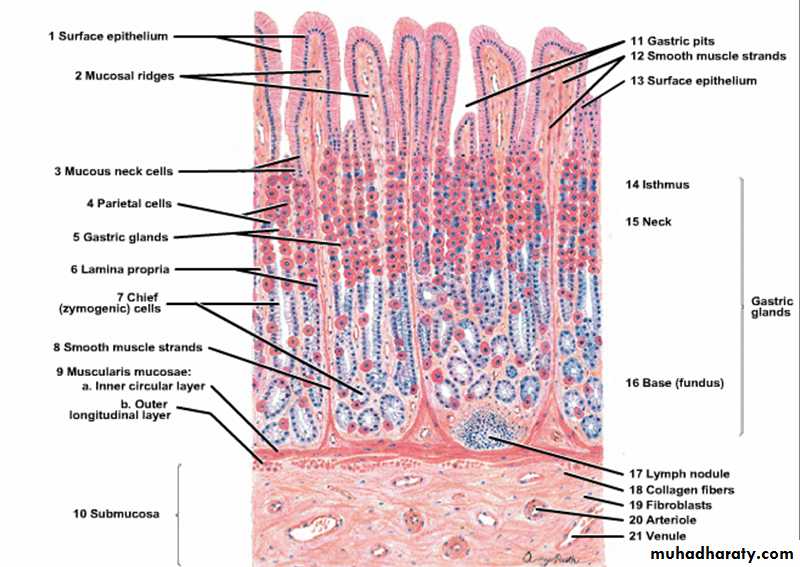
Mucosa: the gastric mucosa consists of
Surface epithelium that invaginate to form the gastric pits or crypts in which open the gastric glands.
Lamina propria composed of loose connective tissue containing lymphoid cells and blood vessels.
Muscularis mucosa- separating the mucosa from the submucosa composed of smooth muscle fibers send bundles of fibers run between the glands to reach the surface of the mucosa.
Cardia:
It is a narrow band at the transition between the esophagus and the stomach and the surface epithelium composed of mucous-secreting cells with few parietal cells.
Lamina propria contains simple or branched tubular cardiac gland some of them are coiled lined by mucous cells.
Muscularis mucosa is thick and irregular send bundles of fibers toward the surface.
Fundus and Body:
Surface epithelium is thrown into short gastric pits; the lamina propria is filled with long straight tubular gastric glands some of them open at the bottom of the gastric pits.
Types of cells in the gastric mucosa:
Stem cells:-Are columnar cells with basal nuclei, having high rate of mitosis, they are able to replace all types of epithelial cells of gastric mucosa.
Surface mucous cells:-
Are tall columnar cells with basal nuclei and clear stained cytoplasm filled with mucin which is discharged in the lumen of the stomach.Mucous neck cells:-
Lie in the neck of the gastric gland they are irregular in shape with basal nuclei and granular cytoplasm.Oxyntic (parietal )cells:-
Present in the upper part of the gastric gland characterized by:-Pyramidal cells with central spherical nuclei and eosinophilic cytoplasm.The surface area of the cell increase as a result of deep circular invaginations of plasma membrane forming intercellular canaliculus. The cytoplasm closed to the canaliculi contains clusters of vesicles while the rest of the cytoplasm contains a lot of mitochondia which is responsible for eosinophilic cytoplasm, also there is RER and Golgi apparatus. Parietal cells produce intrinsic factors which binds with vitamin B12 to make it absorbable by the digestive tract, also they secrete a diluted solution of hydrochloric acid (HCl) this metabolic activity requires energy provided by abundant mitochondria.
Chief ( peptic) cells or enzyme- producing cells:
Present in the lower part of the gastric gland, they have large basal nuclei and RER, the cytoplasm is filled with zymogene granules which contains the in active enzyme pepsinogen which is discharged into the gastric lumen where it is converted by the gastric acid into the active enzyme pepsin.
Enteroendocrine cells:-
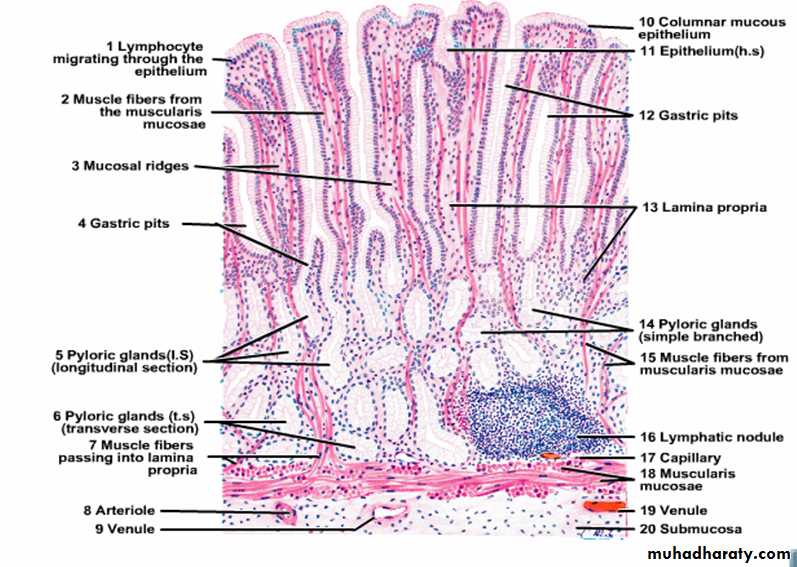
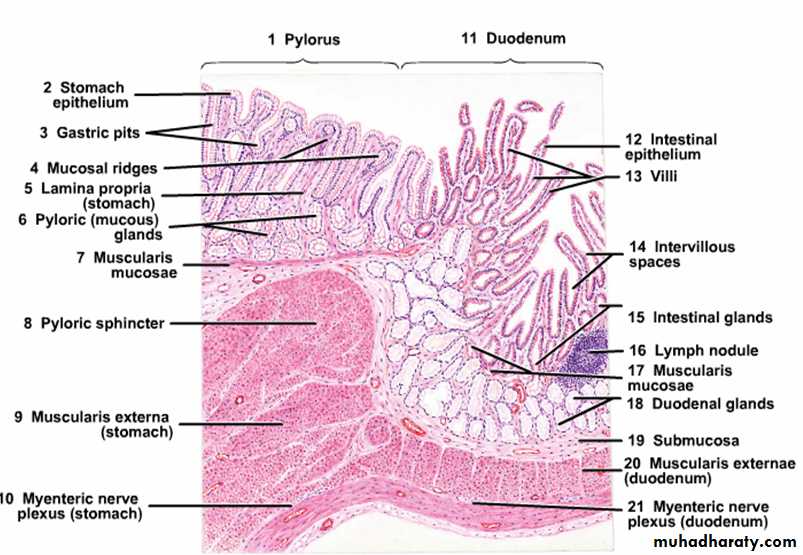
Are small rounded cells located on the epithelial basement membrane, they have central dark nucleus with a rim of clear cytoplasm.Pylorus:-
This region shows deep gastric pits into which open tubular mucous glands extending down to the muscularis mucosa similar to the cardiac glands.These glands are lined by mucous cells and scattered parietal cells particularly close to the pyloric sphincter, the glands secrete mucin and enzyme lysozyme.
Submucosa of the stomach:-
Composed of dense connective tissue, blood vessels and lymphatic vessels with scattered lymphocytes, macrophages and mast cells in addition to Meissner’s plexus.Muscular coat:-
Consists of 3 layers:
Internal oblique, middle circular and outer longitudinal, it differ from other parts of digestive tract by the presence of inner oblique muscle and this help the stomach to mix the foods with the secretions of gastric mucosa. At the pylorus the middle circular muscle is greatly thickened to form the pyloric sphincter.
Serosa:-
Thin and covered by mesothelium containing blood vessels and adipose cells.
Small intestine
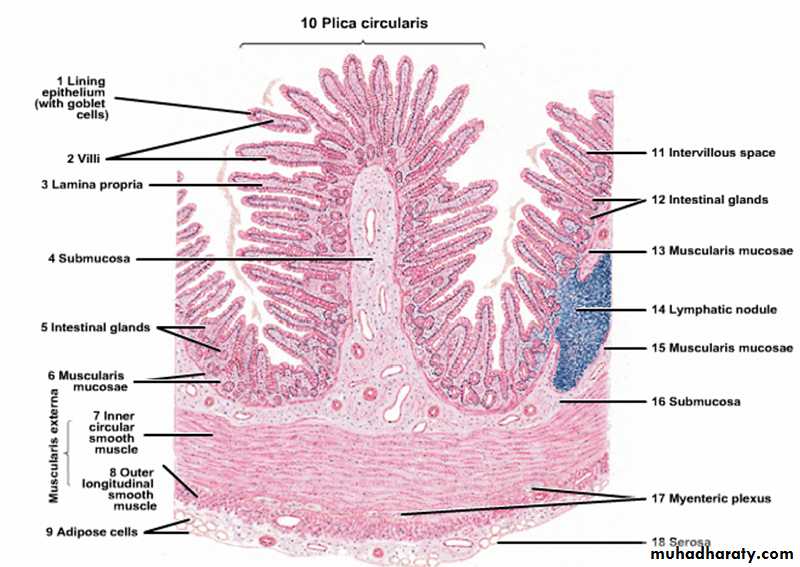
It is the site of terminal food digestion and nutrient absorption, the small intestine is the main site for the absorption of amino acids, sugars and fats and also it is the site for the secretion of enzymes to complete the digestive process, it is about 6 meters in length and divided into 3 segments, duodenum, jejunum and ileum.Histological structure:
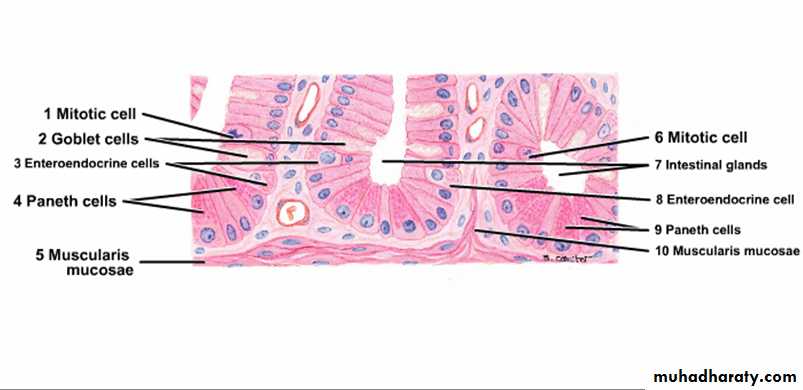
Mucosa:- the small intestine shows structural modification to increase it’s surface area for absorption, so the lining mucosa and submucosa are thrown into numbers of folds or plicae which are most prominent in the jejunum and the surface of plicae arranged into intestinal villi which are long outgrowths of the mucosa consists of epithelium and lamina propria projecting into the lumen of the small intestine, tubular glands or crypts called glands of lieberkuhn extends down from the base of the villi to the muscularis mucosa.The epithelium of the villi is continuous with that of intestinal glands and consists of 5 types of cells:-
Enterocytes ( absorptive cells) :-
Tall columnar cells with rounded basal nuclei, the apex of the cells shows brush border consists of about 3000 microvilli which act to increase the surface area of absorption and secretion of some digestive enzymes, the cytoplasm contains mitochondria, Golgi apparatus, Lysosomes and ribosoms.
Goblet cells:-
Lie between the absorptive cells and increase in number in the jejunum and ileum and most numerous in the terminal ileum. The cytoplasm is fully expanded with mucin granules, it’s mucous secretion is important to protect and lubricate lining epithelium of the intestine.
Paneth cells :-
have basal nuclei and prominent large eosinophilic granules in their apical cytoplasm, these granules secrete lysozyme which protects against infection.
Enteroendocrine cells:-
mainly lie in the lower third of the crypts, triangular in shape with broad base which in contact with the basement membrane and spherical nuclei with pale staining cytoplasm.
Stem cells:-
they multiply to replace other type of cells mostly mucous and enterocytes which shows rapid turn over.
Lamina propria:-
Consist of loose connective tissues, blood vessels and lymphatic vessels with some smooth muscle fibers which are responsible for the movement of villi during absorption, the lamina propria penetrates the core of the villi taking the blood vessels and lymphatic which are prominent in the villi, central lymphatic (lacteal) running vertically in the center of the core of the villus, lamina propria also contains lymphocytes, plasma cells, eosinophils and macrophages.
Submucosa:
loose connective tissue containing blood vessels, lymphatic and nerve plexus, in the duodenum it contains clusters of mucous secreting glands called Brunner’s glands with short ducts open into the bases of the intestinal crypts, their function they act to protect the duodenum mucous membrane against the effect of gastric acid, also bring it’s PH to the level at which pancreatic enzymes are most effective.
Muscular coat of the small intestine:- consist of inner circular and outer longitudinal.
Serosa:- (adventitia and mesothelium) contains blood vessels and adipose tissue.
Regional specialization of small intestine:-
Duodenum: entirely retroperitoneal, leaf shaped villi, Brunner’s gland in the submucosa, receive secretion from the liver and pancreas.
Jejenum: is the main absorptive site, finger like villi, plicae (most prominent).
Ileum: aggregation of lymphoid tissue to form large nodules called (Peyer’s patches) which may expands in the lamina propria , splits the muscularis mucosa and extend into the submucosa.
Doudenum: