INTRACRANIAL MASS
for 5
th
class: medical college: Al Mustansiriyah University
by
Dr Mohamed Al Tamimi
Differential diagnosis: “tumour, pus or blood”
The history is important for localizing and differentiating mass lesions
Important common features on CT (with and without contrast enhancement)
• lesions (may be isodense without contrast)
• midline shifts and herniations
• effacement of ventricles and sulci (often ipsilateral)
A. TUMOUR
1.
primary versus metastatic
2.
primary tumours (benign or malignant) rarely metastasize
their
presenting symptoms
• local effects dependent on site: focal deficits, lobe syndromes, seizures
• raised ICP acute or chronic depending on tumour growth rate
• sudden onset of symptoms after hemorrhage (5-10%)
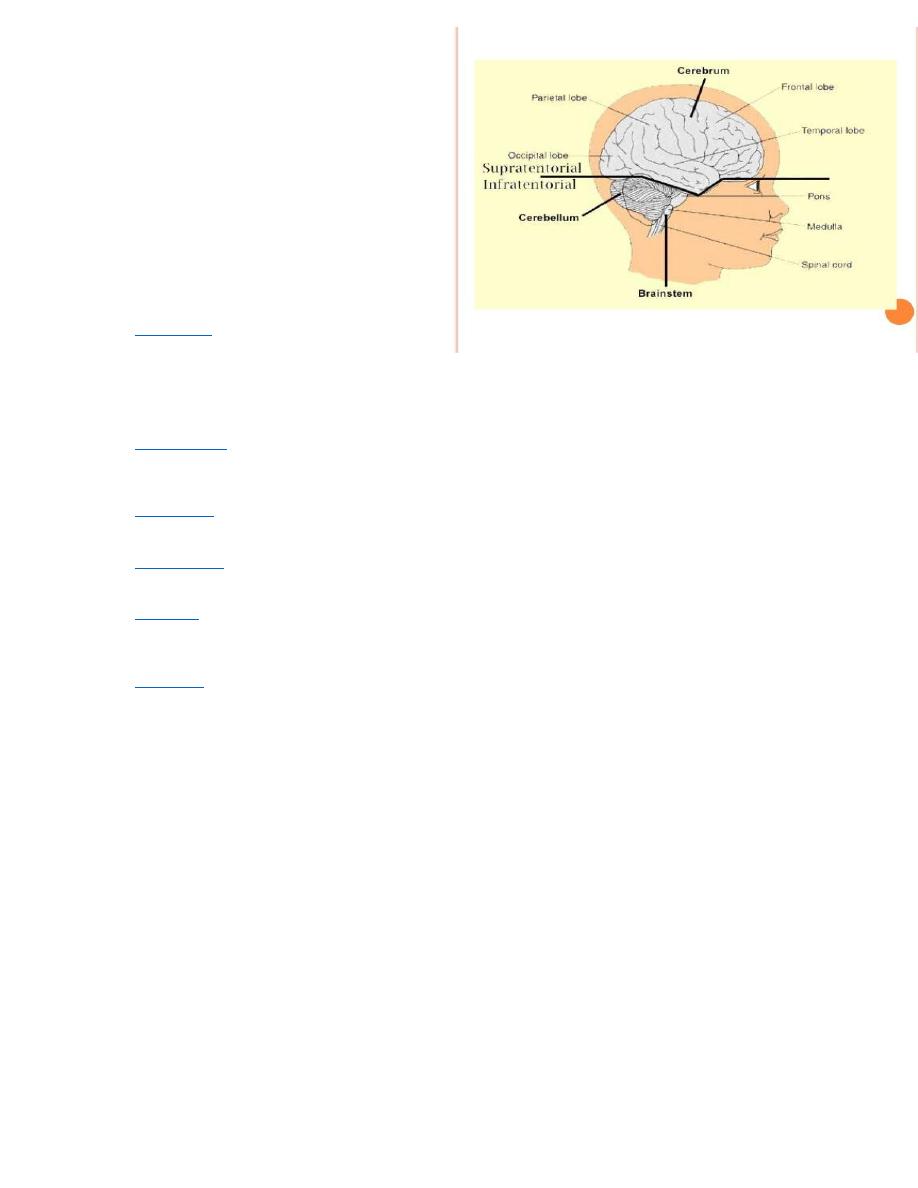
3. consider by
• location (supratentorial vs. infratentorial)
• age (adult vs. child)
Table 1. Tumour Types: Age, Location and Clinical Features
Supratentorial
Infratentorial
children (< 15 years, primarily
infratentorial - 80%)
astrocytoma - all grades e.g. optic
nerve astrocytoma
craniopharyngioma
ependymoma
other: dermoid/epidermoid,pineal
tumours, primitive neuroectodermal
tumors
cerebellar astrocytoma
medulloblastoma
ependymoma
choroid plexus papilloma
brain stem astrocytoma
adult(>15 years, primarily
supratentorial - 80%)
astrocytoma (40-50%)
metastatic (20-30%)
meningioma (15%)
pituitary ademona (5%)
oligodendroglioma (5%)
metastatic (20-30%)
schwannoma (6%)e.g. acoustic
neuroma
hemangioblastoma(5%)
medulloblastoma (5%)
signs and symptoms
raised ICP
focal or lobar effects
• seizures
• mental status changes
• personality changes
• visual field deficits
• endocrine disturbances (with
pituitary tumour)
raised ICP
local effects in posterior fossa
• extremity ataxia
• truncal ataxia
• CN palsy - often multiple
• nystagmus
• LOC
• long tract signs
Symptoms according
Position of the tumor
Changes in personality
Swearing or behaving in a way that patient normally wouldn't (loss of inhibitions)
Being irritable or aggressive
Difficulty walking
Loss of sense of smell
Forgetting words
Short term memory loss
Difficulty speaking or understanding what is said to patient
Sight problems or loss of vision on one side
Poor co-ordination
Uncontrolled movement of the eyes
Dizzine
ss
Poor co-ordination
Drooping eyelid or mouth on one side
Difficulty swallowing
Difficulty speaking
Seeing double
Investigations
CT, MRI, stereotactic biopsy (tissue diagnosis)
Management
1. medical
• steroids useful for vasogenic cerebral edema (decrease edema around tumours and decrease mass effect/ICP)
• pharmacological treatment for pituitary tumours
2. surgical
• excisional: total, partial, decompressive, palliative
• shunt if CSF flow is blocked
3.radiotherapy - external, brachytherapy, stereotactic radiosurgery (Gamma-knife, Linear Accelerator)
4.chemotherapy - alkylating agents
Metastatic Tumours
mainly from lung, breast, GI, kidney, melanoma
solitary tumour: surgical excision and whole brain radiation
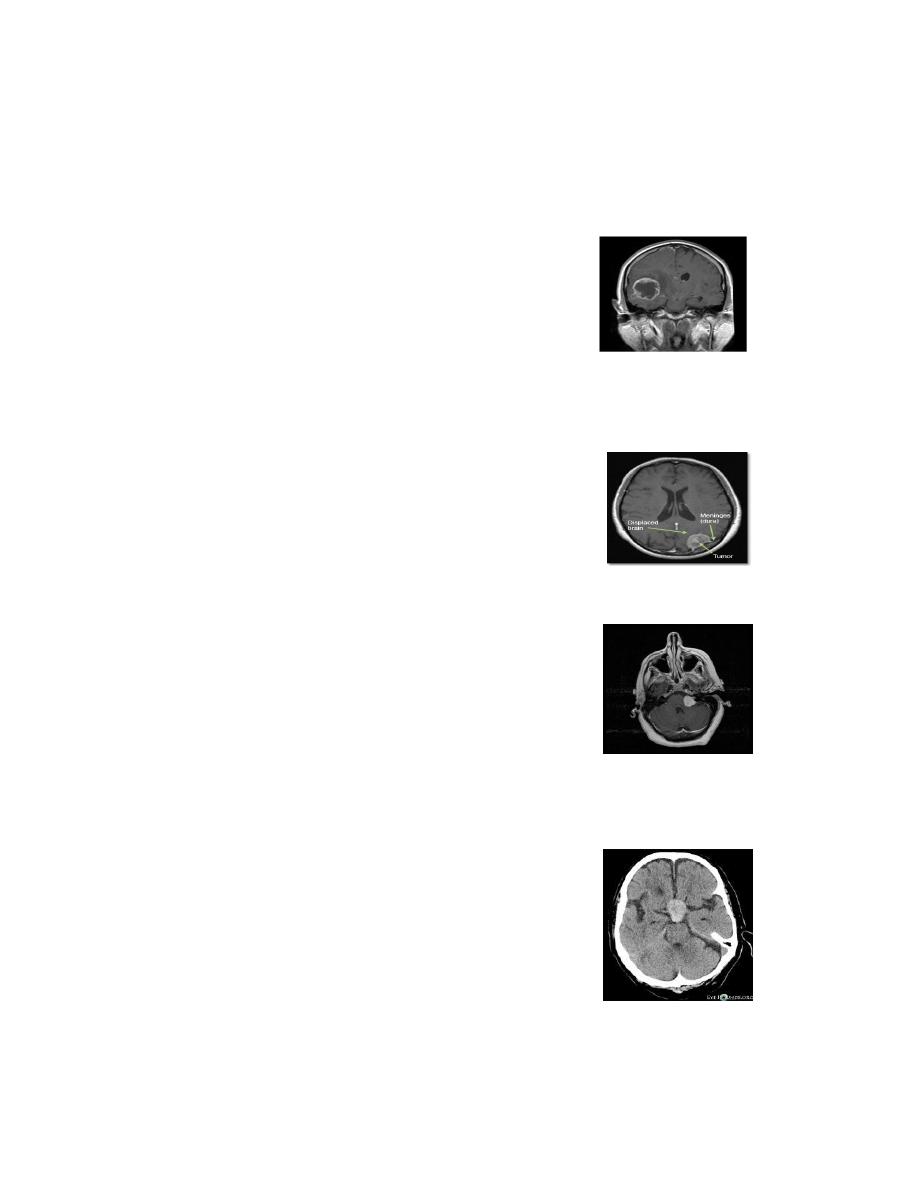
Astrocytoma
The most common primary brain tumour (45-50%)
1. low grade (grades I-II) with slower growing, peak age 40 years, median survival 2-4 years
2. high grade (grades III-IV, glioblastoma multiforme) fast growing, peak age 55 years, median survival
< 2 years, surgery not curative, aim to prolong “quality” life, radiotherapy prolongs survival)
3.
“cystic cerebellar” astrocytoma (pediatric population, infratentorial, potentially curable)
Meningioma
mostly benign (1% malignant), slow-growing
,non-infiltrative.
The
common locations: parasagittal
and falx convexity, sphenoid ridge.
It is mostly curable if complete resection possible (5 year survival > 90%)
Vestibular Schwannoma (“Acoustic Neuroma”)
progressive unilateral deafness = acoustic neuroma until proven
otherwise. It
arises from vestibular component of CN VIII at
cerebello-pontine angle (CPA). Usually presented with signs of
compression of CPA structurs
• CN V: facial numbness, loss of corneal reflex
• CN VII: facial weakness (uncommon pre-operatively)
• CN VIII: unilateral sensorineural deafness, tinnitus, vertigo
• cerebellum: ataxia, nystagmus
Generally it is curable by resection, sometimes palliative treatment with gamma-knife radiotherapy
Pituitary Adenomas
1.The usual presentation is due to its
mass effects
• H/A
• bitemporal hemianopsia (compression of optic chiasm)
• CN III, IV, V1, V2, VI palsy (compression of cavernous sinus)
2. endocrine effects
• hyperprolactinemia
• Cushing disease
• acromegaly
• infertility, amenorrhea, galactorrhea, impotence
• panhypopituitarism (hypothyroidism)

3. apoplexy and CSF rhinorrhea (rare presenting signs of pituitary tumour)
The
diagnosis endocrine function tests; MRI
Treatment is
1. medical with
• bromocriptine/dopamine agonists for prolactinoma
• endocrine replacement therapy
• somatostatin analogue (octreotide) +/– bromocriptine for acromegaly
2. surgery (+/– radiation
B. PUS
Brain Abscess
Etiology
1. local spread (adjacent infection)
• otitis media, mastoiditis, sinusitis
• osteomyelitis
• dental abscess
2. hematogenous spread
• adults: lung abscess, bronchiectasis, empyema
• children: cyanotic heart disease with R to L shunt (blood is
shunted away from lungs preventing filtration of bacteria)
• immunosuppression (AIDS - toxoplasmosis)
3. dural disruption
• surgery, trauma
• congenital defect, e.g. dermal sinus
Pathogens
• Streptococci (most common), often anaerobic or microaerophillic
• Staphylococci (penetrating injury)
• Gram negatives, anaerobes
Diagnosis
• focal neurological signs and symptoms
• mass effect, increased ICP and sequelae
• seizures
• +/– signs of systemic infection (mild fever, leukocytosis)
• blood cultures rarely helpful, LP not helpful and contraindicated
• CT scan
Management
• multiple aspiration of abscess and/or excision, and send for C&S
• antibiotics
• empirically: penicillin and metronidazole (cover Streptococci and anaerobes) +/– ceftriaxone
(cover Gram negatives)
• after sensitivity results return, revise antibiotics
• treat primary site
Other Causes of Pus...
1. subdural empyema (from sinusitis, mastoiditis - rare, 20% mortality)
2. meningitis, encephalitis, AIDS toxoplasmosis
3. osteomyelitis of skull (Pott’s puffy tumour), usually seen with sinusitis
4. granuloma (TB, sarcoid)

C. BLOOD
Hematoma/hemorrhage
1.
epidural, subdural hematoma
2.
intracerebral, intraventricular hemorrhage, SAH
Vascular Abnormality
aneurysm, AVM
Clinical Features
1.sudden onset severe headache: “worst headache of my life”
2.vomiting, nausea (increased ICP)
3.meningismus (neck stiffness, photophobia, positive Kernig’s and Brudzinski’s sign)
4.decreased level of consciousness, transient or prolonged
5.focal deficits: cranial nerve palsy (e.g. III, IV), hemiparesis
6.
ocular hemorrhage in 11-33% (due to sudden increase in ICP)
7.
occasionally exertional (straining, intercourse)
Diagnosis (see Figure 7)
differential diagnosis: migraine, tension H/A, meningitis, stroke, flu
1.
CT without contrast
2. Lumbar puncture (LP)
• contraindications
• known or suspected intracranial mass
• non-communicating (obstructive) HCP
• unconscious, focal deficit, papilledema
• coagulopathy (platelets < 50, anticoagulants, etc...)
• infection at site desired for LP (e.g. epidural abscess)
3. Cerebral angiography
Management
1.
bed rest, elevate head (30 degrees), minimal external stimulation
2.
control HTN, avoid hypotension since CBF autoregulation impaired by SAH
3.
prophylactic anticonvulsant: short course of Dilantin (2 weeks)
4.
neuroprotective agent: nimodipine
5.
early surgery to prevent rebleed or to evacuate haematoma
6.
intraventricular catheter if acute HCP present
7.
“Triple H” therapy for vasospasm: hypertension, hypervolemia, hemodilution
8.
angioplasty for refractory vasospasm
