Medically compromised patient
Ischemic Heart diseasesIschemic Heart diseases
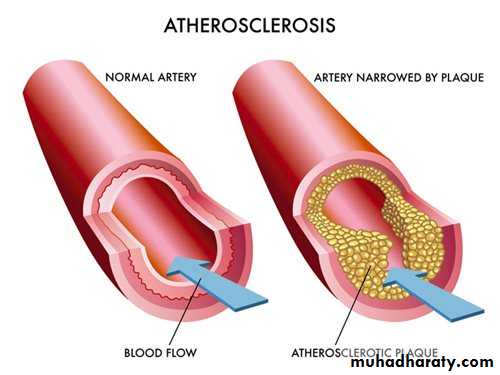
Ischemic Heart Disease (IHD) also called Coronary Artery Disease (CAD) is the most common and important cardiac disease and it is the most common cause of death. IHD is cause by Atheroma (Atherosclerosis, also called Arteriosclerosis), it is characterized by the accumulation of cholesterol and lipids in the intima of arterial walls, and can lead to thromboses, which sometimes break off and move within the vessels to lodge in and occlude small vessels (embolism).• Atheroma can thus lead to IHD with angina, myocardial infarction, cerebrovascular disease and stroke. It also affects other arteries and can cause, for example, ischemic pain in the calves whilst walking - intermittent claudication - seen especially in young smokers. Atheroma results from a combination of genetic and lifestyle factors. Irreversible (fixed) risk factors include increasing age, male gender and family history of atheroma.
Potentially reversible risk factors for atheroma include:
• Cigarette smoking. Persons who smoke 20. or more cigarettes daily have a two or three fold increase in coronary artery diseases.• Blood lipids.
• Hypertension.
• Diabetes mellitus. There is a two-eight fold higher rate of cardiovascular events. •
• Obesity and lack of exercise.
Angina pectoris
Episodes of chest pain caused by myocardial ischemia, it affects 1% of the adult population and its prevalence increases with age. The usual underlying causes are atherosclerotic plaques that rupture. Arterial spasm alone may, rarely, be responsible. The mortality rate in angina is about 4% per year, the prognosis depending on the degree of coronary artery narrowing.• The most common precipitating causes of angina pain are physical exertion (particularly in cold weather); emotion (especially anger or anxiety); and stress caused by fear or pain, leading to adrenal release of catecholamine's (epinephrine and norepinephrine) and consequent tachycardia, vasoconstriction and raised blood pressure. Consequently an increased cardiac workload is accompanied by a paradoxical drop in blood flow and myocardial ischemia occurs resulting in angina.
Clinical features of angina:
- Chest pain described as a :• pressure sensation,
• fullness
• squeezing in the mid-portion of the thorax.
• the pain lasts for less than 10-15 minutes about 2-5 minutes in most cases, relieved by rest or glyceryl tri-nitrate.
• Radiation of chest pain into the jaw/teeth, shoulder, arm, and/or back.
• Occasionally associated dyspnea or shortness of breath, epigastric discomfort or sweating.
Types of angina
• Stable angina: induced by effort, stress or sometimes eating, it is relieved by rest or Nitroglycerin.• Unstable angina: (crescendo) angina of increasing frequency or severity, occurs on minimal exertion or at rest, the pain is not readily relieved by Nitroglycerin, there is increased risk of MI.
• Decubitus angina: precipitated by lying down.
• Variant or Prinzmetal's angina: caused by coronary artery spasm.The term acute coronary syndromes (ACS) are a term used in unstable angina evolving MI which share common underling pathology; plaque rupture, thrombosis and inflammation.
Tests :
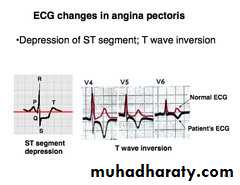
Resting ECG: ST depression, flat or inverted T wave.
Exercise ECG
THALLIUM – 201 scan: highlights ischemic myocardium.
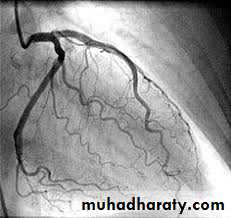
Coronary angiography.
Management:
• Identify and correct risk factors:• stop smoking.
• encourage exercise and weight loss,
• control hypertension and diabetes.
• Antiplatelet drugs like aspirin 75-150 mg/24 h and clopidogrel .
• β blockers; atenolol 50-100 mg/24h, unless contraindicated (asthma, COPD, bradycardia, coronary artery spasm).
• Nitrates; for symptoms give glyceryl triturate (GTN) spray or sublingual tablets 0.3 mg to reduce the peripheral vascular resistance and reduce oxygen demands. Also long acting nitrates isosorbide monointrate 20-40 mg twice daily or slow-releases nitrate.
• calcium antagonists; amlodipine, diltiazem, especially when β blockers are contraindicated.
• Potassium channel activator; nicorandil.
• Percutaneous transluminal coronary angioplasty (PTCA); aims to open up the coronary blood flow by inserting a balloon- tipped catheter through the groin up. into the area of arterial blockage,
• Coronary artery bypass grafts (CABG) are vascular grafts made to bridge the obstructions in the coronary blood vessels.
Myocardial Infarction (MI)
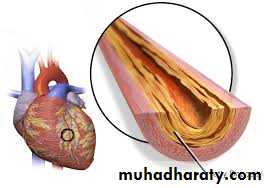
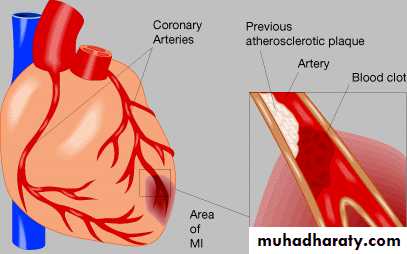
Myocardial infarction results from the complete occlusion (blockage) of one or more coronary arteries. It arises when atherosclerotic plaques rupture causing platelet activation, adhesion and aggregation with subsequent thrombus formation within the coronary circulation. Angina may progress to MI but fewer than 50% of patients with MI have any preceding symptoms.Complications of MI include weakened heart muscle, resulting in acute congestive heart failure, post-infarction angina, infarct extension, cardiogenic shock, pericarditis, and arrhythmias. Causes of death in patients who have had an acute MI include:
• ventricular fibrillation,
• cardiac standstill,
• congestive heart failure,
• embolism,
• and .rupture of the heart wall or septum
Clinical features of myocardial infarction
• Chest pain described as a pressure sensation, fullness or squeezing in the mid-portion of the thorax. 10-20% of individuals have silent (painless) MI.
• Radiation of chest pain into the jaw/teeth, shoulder, arm, and/or back.
• Associated dyspnea or shortness of breath.
• Associated epigastric discomfort with or without nausea.
• Associated diaphoresis or sweating.
• Syncope or near-syncope without other cause.
• Impairment of cognitive function without other cause
50%of the patients die within the first hour of MI and a further 10-20% within the next few days
Diagnosis of MI : is by
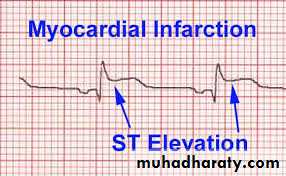
• clinical features,• ECG (large Q wave, ST elevation and T inversion),
• change in the serum levels of cardiac enzymes which include; Troponin T (TT), Creatinine Kinase MB (CK-MB), Aspartate transaminase (AST) and Lactic dehydrogenase (LDH).
Management:
• Alert emergency services (if in community) or cardiac arrest team hospital).• Aspirin (300 mg); to be chewed. Clopidogrel.
• Rest and reassurance .
• Pain relief: opioid analgesia (diamorphine) is usually necessary.
• Oxygen administration.
• Early thrombolytic therapy (Streptokinase, Urokinase, Alteplase or Reteplase),
the greatest benefit is realized when patients receive thrombolytic drugs within the first 3 hours after infarction; however, modest benefit is possible even up to 12 hours after the event. The early use of thrombolytic drugs may decrease the extent of necrosis and myocardial damage and dramatically improve outcome and prognosis.
• Primary percutaneous intervention to dissolve the coronary thrombus Provided the patient is not at risk of a life-threatening hemorrhage.
• Insulin infusion to prevent stress hyperglycemia.
• General "pharmacologic measures for patients with acute MI include the use of nitrates ,beta blockers, calcium channel blockers , ACE inhibitors and lipid – lowering agents antiplatelet drugs are significant in decreasing morbidity and mortality .
• sedative and anxiolytic medications also may be used
Dental management
Identification of patients with a history of ischemic heart diseases, and if the patient is not under medical control we have to refer him to physician for an evaluation and control.The potential problem related to the dental procedure is that, the stress and anxiety during the dental procedure, and excessive amount of vasoconstrictor in local anesthesia may precipitate the attack of angina pectoris, MI, arrhythmia, or sudden death.
In general recent MI and unstable angina are classified as clinical of major risk for perioperative complications like serious arrhythmias and re-infarction. Stable (mild) angina and past history of MI are identified as clinical predictors of intermediate risk for perioperative complications.
Patients with stable angina or past history of MI (more than 6 months) [Intermediate risk]
• Long stressful appointments should be avoided. Morning appointment with comfortable chair position is recommended.
• Pretreatment vital signs should be recorded including pulse rate and blood pressure as a base line record.
• Nitroglycerin sublingual tablets should be readily available and in some cases prophylactic preoperative nitroglycerin is advisable especially when the patient has angina more than once a week.
• Stress-reduction measures which include:
• Good communication
• Oral sedation (e.g., Diazepam 2-5 mg on the night before and 1 hour before the appointment)
• Intraoperative Nitrous oxide and oxygen but hypoxia should be avoided.
• Excellent local anesthesia
• Limited use of vasoconstrictor not more than two cartridges containing 1: 100.000 adrenalin or 1:20.000 levonordefrine, Avoid intravascular injections through the use of aspirating syringe.
• Avoidance of adrenalin-impregnated retraction cord
• Antibiotic prophylaxis not recommended for history of coronary artery bypass graft (CABG).
• Avoidance of anticholinergics (e.g., scopolamine, and atropine)
• Adequate postoperative pain control.
For patients with coronary artery stents:
• elective dental care should be deferred for 6 months.• emergency dental care should be in a hospital setting.
• It may be prudent to provide antibiotic coverage if emergency dental treatment is required during the first six weeks postoperatively.
• Patients may require long-term anticoagulant medication, but most patients are on aspirin or clopidogrel rather than warfarin.
If a patient experiences chest pain in the dental surgery:
• dental treatment must be stopped.• the patient should be given nitroglycerine sublingually and oxygen.
• and be kept sitting upright.
• Vital signs should be monitored.
• The pain should be relieved in 2-3 min.
• the patient should then rest and be accompanied home.
• If chest pain persists after three doses of nitroglycerin given every 5 min, that lasts more than 15-20 min, or that is associated with nausea, vomiting, syncope or hypertension is highly suggestive of MI, oxygen should be continued, and 300 mg of aspirin should be chewed.
Patients with unstable angina or recent MI (less than 6 months)
[Major risk]
• Avoid elective care, only emergency treatment should be provided.
• consult with physician and limit treatment to pain relief, "treatment of acute infection, or control of bleeding.
• Prophylactic nitroglycerin sublingually is advisable.
• Placement of intravenous line.
• Sedation and oxygen.
• Frequent monitoring of blood pressure, pulse oximeter and continuous electrocardiographic monitoring
• Cautious use of adrenalin in local anesthetic, local anesthesia without adrenalin can be used or not more than two cartridges containing 1: 100.000 adrenalin or 1:20.000 levonordefrine using aspirating syringes.
• In general conscious sedation and general anesthesia should be deferred for at least 3 months in patients with recent-onset angina, unstable angina or recent development of bundle- branch block and, in any case, it should be given in hospital.
• Adrenalin-impregnated retraction cords are avoided.
• If the patient "experiences pain during treatment, the management is the same as above.
The use of antiplatelet and anticoagulation drugs
• Patients who take aspirin or another platelet aggregation antagonist such as clopidogrel can expert some increase in bleeding this effect generally is not clinically significant and bleeding may be controlled through local measures ,discontinuation of these agents before dental treatment generally is unnecessary• Patients who take warfarin for anticoagulation must have a current international normalized ratio (INR) determined before any invasive procedure and they are managed after consultation with physician
The Local hemostatic measures that are used to control bleeding include the use of hemostatic agents in the sockets (gelfoam, surgicel), suturing and gauze pressure packs.