Small & Large Bowel
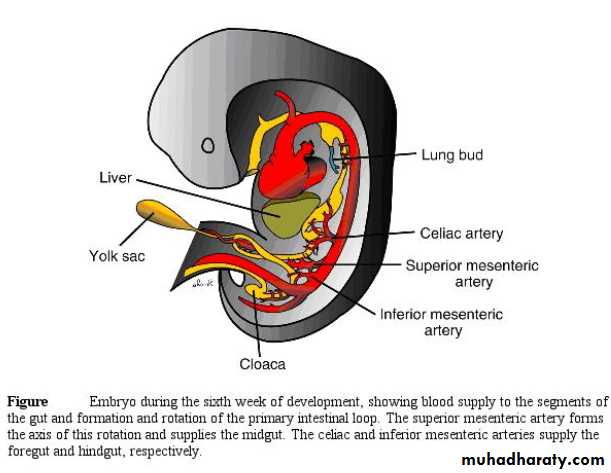
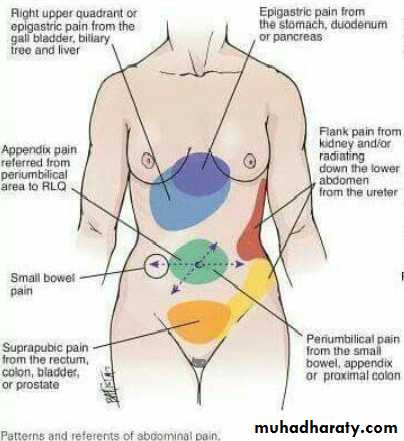
Gastrointestinal tract formed from 3 parts:Foregut: stomach and duodenum down to the Ampulla of Vater and supplied by Celiac artery and the visceral pain felt in the epigasrtic region.
Midgut: from the middle of 2nd part of duodenum till the junction of middle 3rd and the lat 3rd of transverse colon & supplied by superior mesenteric artery & its visceral pain felt around umbilicus
Hindgut remaining part colon & upper half of anal canal & supplied by inferior mesenteric artery & Pain felt.
Small Bowel
It may vary from 300 to 850 cm between the duodenojejunal (DJ) flexure to the ileocaecal valve. The proximal 40 % is referred to as the jejunum; the remainder is the ileum. There is no clear demarcation between jejunum and ileum, but the small bowel does change gradually in character from proximal to distal. The jejunum tends to have a wider diameter and a thicker wall, with more prominent mucosal folds (valvulae conniventes), while the ileum has a thicker, more fatty mesentery with more complex arterial arcades. The ileum also contains larger aggregates of lymph nodes (Peyer’s patches).
The Wall of Small intestine
Mucosa : single layer of columnar epithelium with mucus goblet cells The absorptive surface area approaches 500 m2 which achieved by the presence of mucosal folds, villi, and microvilli on the cell surface. Under the epithelium is a thin muscle layer; the muscularis mucosa.The submucosa is the strongest layer It contains lymphoid aggregates (Peyer's patches), &The Meissner's nerve plexus is present in the submucosa. Muscularis propria outer longitudinal, inner circular with Aurbach myenteric plexus. Serosa: part of visceral peritoneum.
Blood Supply:
from the superior mesenteric artery, while venous drainage is via the portal venous system, into which the superior mesenteric vein drains blood rich in nutrients after a meal. The portal vein drains in the liver . The lymphatic drainage of the small intestine follows the arterial supply. The small intestine has a rich autonomic innervation arising from the splanchnic nerves, which contribute a dense network of sympathetic fibres around the superior mesenteric artery and its branches. Referred pain from the small intestine is usually felt in the periumbilical region (T10).
Physiology Of The Small Bowel
Main function is absorption of fat, protein, carbohydrate ,vitamins and electrolytes, The jejunum is the principal site for digestion and absorption of fluid, electrolytes, iron, folate, fat, protein and carbohydrate, Resection of jujenum can be compensated by ileum but the jejunum cannot compensate resection of terminal ileum. Vit B12to be absorbed combine with intrinsic factor secreted by stomach then absorbed in the ileum therefore resection of ileum may produce vit.B12 deficiency.
Colon
Is formed of cecum, ascending colon, transverse colon, desending, and sigmoid colon, ileocecal valve is a competent valve.Cecum is a blind pouch and the appendix opens at the junction of tenia coli.Transverse colon join the ascending at hepatic flexure and the descending at splenic flexure, whih is suspended by Phrenecocolic ligament.The descending colon continues as sigmoid (pelvic) colon ends at the level of S3 where rectum begin.Cecum is completely covered with peritoneum. Transverse and (pelvic) colons completely covered with peritoneum have mese ntery and are mobile. Greater omentum attached to the antimesentric bordeer of transverse colon .
Blood Supply
Superior mesenteric artery to midgut.
Inferior mesenteric artery to hindgut.
Venous drainage :Superior and inferior mesenteric veins to portal veins
Lymphatic drainage to L.N. alongside of superior and inferior mesenteric vv.
Walls: * Mucosa columnar epithelium with goblet
Submucosa the strongest layer, connective tissue
Muscular layer inner circular& outer longitudinal Taenia coli
Serosa visceral peritoneum.
Rectum
12-15 Cm. In length starts at S3 recto sigmoid junction downward in hollow of sacrum and ends at anorectal junction at pelvic floor.
* Rectal Ampulla act as reservoir , There are 3 lateral curves in the rectum their inner aspect form a valve of Houston (on endoscope).
* The rectum has no tenia , haustration nor mesentry.
The upper 1\3 is covered with peritoneum from above & both sides.
The middle 1\3 only covered by peritoneum anteriorly.
The lower 1\3 is totally extra peritoneal.
Posteriorly the rectum is loosely bound to sacrum by connective tissue (Waldeyer Fascia) behind it is a plexus of autonomic nerves.
Anteriorly (Denoviller fascia) separate it from the base of bladder & prostate in male.
Arterial supply: Sup. rectal artery from inf.Mesenteric art. ,Middle rectal artery from internal Iliac art., Inferior rectal from Pudendal art.
Venous drainage: Sup. rectal v. to inf. Mesenteric vein to portal Middle & Inferior.rectal veins to systemic circulation.
Lower rectum and anal canal, are site for porto-systemic collaterals
Lymphatic drainage: Upper to the Inf. Mesent. lymph nodes & to para-aortic L.N.
Lower to internal Iliac L.N.
Physiology main function of the small bowel is absorption. Fat, protein, carbohydrates, vitamins, water, and electrolytes are all absorbed.
With a few exceptions (e.g. iron and calcium), the small intestine absorbs indiscriminately without regard to body composition.
To be absorbed, vitamin B12 combines with the intrinsic factor secreted by the stomach. It is then absorbed in the distal ileum. Resection of a long segment of the distal small intestine is, likely to produce vitamin B12 deficiency. intestinal secretions present a total of 5-9 L/day, but only 1-2 L pass the ileocaecal valve to the colon.
Function of colon & Rectum: Absorption of water and sodium to concentrate the waste products. This is mainly a function of the right side of the colon.
1. The left side of the colon acts as a reservoir for solid faeces till ldefaecation.
2. Mucus secreted by the mucosa acts as a lubricant. Potassium and bicarbonate are also secreted in small quantities. Excessive diarrhoea may result in potassium and bicarbonate loss and metabolic acidosis.
Preoperative preparation for elective surgery
Anastomosis in colon is liable for disruption, leakage and peritonitis, causes:
1.Highly infective contents of both aerobic and an aerobic bacteria
2.constant gaseous distension 3.incomplete serous coat
4. peculiar blood supply where terminal arteries poorly connect each other
Preoperative preparation for elective surgery Improving nutritional status
Bowel preparation : the risk of leakage & sepsis decrease much if bowel is clean .
Methods of preparation:
Mechanical preparation:
Standard preparation: 1. Non residue diet for 4 days before operation
2. Enema and mild laxative for 2-3 days before surgery.
B.Rapid preparation. Another method performed 1 day before suegery.
1.Whole gut irrigation using 2-4L/hour of a balanced crystalloid solution passed via a nasogastric tube until the patient passes clear fluid per rectum.( not for bowel obst. Or with heart disease)
2.Mannitol 1 litre of flavored mannitol given orally.
Chemical Preparation: Intestinal antiseptics administered orally help to reduce the density of colon bacteria. A combination of neomycin and metronidazole (Fiagyl) for two days will cover the Gram negative bacilli and the anaerobes which are normally resident in the large intestine.
Prophylactic Parenteral antibiotics: systemic antibiotic administered immediately before operation & continued Postoperatively for 1 day (Peri-Operative antibiotic prophylaxis) usually Cephalosporin or an Aminoglycoside with either flagyl or Clindamycin.
Operative Procedure
Resection : extent of resection is governed by art. Blood supply & disease process.
In surgery for malignancy it is essential to remove draining lymph nodes .
Divisions of peritoneal attachments allow adequate mobilization of bowel.
Anastomosis: For a successful anastomosis the two bowel ends should be adequately vascularized, and should be sutured without tension. An intestinal anastomosis can be done by one of two methods.
1-By hands two layers: 1st interrupted full thickness & seromuscular, defect in mesentery closed.
2- By stapler which is rapid and coasty.
Emergency Surgery: in patient with obst.,perforation, toxic dilatation, bleeding from colon emergency surgery might be needed
In critical ill patient with obst. Temporary colostomy done resection postponed
If patient condition permit resection ( but not prepared )&dealing with according to site: 1.ileotransverse anastomosis in right colon resection other parts of colon primary . anastomosis abandoned due to high leakage possibility,
proximal colostomy & distal end closed left in abdomen (Hartman procedure)
both ends brought to skin proximal as colostomy & distal mucus fistula .Later on after few weeks elective closure with preparation.
Intestinal Stoma
Ileostomy indications:proctocolctomy for ulcerative colitis or familial polyposis coli.
Conventional ileostomy:
The stoma is performed so that the nippl of ileostomy protrude from the skin leading to direct delivery of of irritant small bowel contents to the appliance(it is incontinent).
Continent Ileostomy:
Done by fashioning a valve with an underlying reservoir (Koch Pouch) which the patient regularly evacuate by passing a tube.
Colostomy: Opening of the colon to the skin.
Indications of Temporary Colostomy
1.To relieve large bowel obstruction in patients with:High anorectal malformations.
Hirschsprung's disease.
Inflammatory stricture.
Carcinoma of the colon.
After the obstruction is relieved, the colon is prepared and the cause is corrected. Later,the colostomy is closed. This is called three-stage
management of acute colon obstruction.
Injuries of the colon. The injured segment is either exteriorized as a colostomy, or is closed and a proximal diverting colostomy is performed.
To protect a distal doubtful colonic or rectal anastomosis.
Permanent Colostomy
After abdomino-perineal resection.
lrresectable carcinoma of the large bowel with obstruction.
Incurable cases of anal incontinence.
High anal fistulae that is not amenable to surgery.
1. Loop colostomy is usually temporary and is usually done in the right side of the transverse colon brought to the surface, fixed to the abdominal wall, opened along one of the taeniae coli, and then stitched to the skin. A rod is passed beneath the loop to prevent retraction, and is removed after one week.
2. End colostomy may be permanent or temporary. It is commonly .constructed in sigmoid colon left colon
3. Cecostomy :for temporary decompression of the colon and done by insert of wide bore tube in to the cecum.
Colostomy complications
Prolapse.
Retraction.
Necrosis of distal end.
Stenosis of the orifice.
Colostomy hernia. through the anterior abdominal all opening beside the colon end, or internal when the surgeon fails to close the space lateral to the exiting colon between it and the parietal peritoneum.
Intestinal Trauma:
The small and large intestines are frequently injured, either alone or in combination with other intra-abdominal viscera. The prognosis after treatment of intestinal injury largely depends on these associated injuries. Colon injuries are more dangerous than those of the small intestine because of the magnitude of intra-abdominal contamination.
The intestine may be injured by:
Blunt abdominal trauma as in road traffic accidents (RTA) or blows to the abdominal wall. Presence of seat belt injuries should direct attention to the possibility of intestinal injury.
Penetrating trauma as stabs and bullets. High velocity missiles are more damaging than low velocity ones and stabs. Indirect trauma, e.g., blast injuries are known to affect the colon.
Iatrogenic injury is increasing with the rising popularity of invasive investigations.
Examples:
*The duodenum may be injured during an attempt at endoscopic sphincterotormy. *The colon may also be injured with colonoscopic diatherm.
Types of Injury:
Contusion and haematoma.
Rupture which may be complete or incomplete and single or multiple.
Tears of mesentery or mesenteric vessels resulting into haematomas, and gangrene of the affected bowel segments.
Sequela:
Peritonitis occurs due to the escape of intestinal contents into the peritoneum.
Internal haernorrhage. With intestinal injuries bleeding is less of a problem than peritonitis.
Hypovolaemia and septic shock.
Paralytic ileus.
Injuries may heal by strictures and massive adhesions by intestinal obstruction.
Clinical Picture:
1-History of trauma.
2-Abdominal pain at site of trauma which spread to all abdomen.
Signs:
General : tachycardia, fever, & hypotension. And Local:
signs of injury: bruises, inlet or outlet of a bullet, stab .
Tenderness with rebound tenderness.
Loss of liver dullness due to free air in peritoneum .
Distension due to developing ileus.
Shifting dullness because of free intraperitoneal fluid.
Frank peritonitis due to perforation nearly or late.
Investigations:
1.Clinical .
2.Laboratory tests (leukocytosis , & hemodilution)
3.Radiology
Plain abdominal X-Ray may show free air under diaphragm or multiple fluid levels, due to ileus, bullet & shell or fracture may be seen.
Ultrasound or CT scan reveals hematoma or collection.
4.Needle tap, diagnostic peritoneal lavage (DPL) may show free blood, bile ,or intestinal contents.
Treatment: Surgery (laparotomy)
Preoperative:
Anti-shock measures.
Antibiotic coverage Cephalosporin & Metronidazole.
Tetanus toxoid booster dose.
Insertion of nasogastric tube & urinary catheter.
Operation:Midline incision full exploration 1st bleeing managed then bowel injury.
Priorities of multiple trauma management should be followed
Small bowel and Right side of colon :if tinny small injury suturing is enough. bigger need trimming & suturing , big wounds , big segment need resection & anastomosis .
Transverse colon and left colon: localized injury exteriorized as colostomy or injury sutured and protective proximal colostomy closed after 1 month or resection of injured segment with proximal colostomy & distal mucous fistula or Hartman's procedure, closure after month, good peritoneal irrigation with N.S.
Intstinal Fistula:
80% of external fistulae develop after an abdominal operation. The cause is either: *.Unrecognized intestinal injury.
*.Failure of an intestinal anastomosis. Causes of this failure include:
Poor vascularity.
Anastomosis under tension.
Anastomosis in the presence of sepsis.
Distal obstruction.
Lack of proper surgical technique.
Presence of a specific pathology as Crohn's disease.
Generalized diseases that impair healing, e.g., hypoproteinaemia.
Other Causes:
Congenital as patent vitello intestinal duct through the umbilicus
Abdominal trauma
Inflammatory bowel disease (Crohn's) colonic diverticulitis, radiation enteritis which produce internal and external fistula .
Malignant tumour.
Pathology:
Fistula is abnormal communication between two epithelial surfaces. It is lined by granulation tissue but sometimes it is lined by epithelium.
Intestinal fistulae are classified into:
* internal connect the intestine to hollow viscera (bladder, vagina, etc.)* external when it is connected to the skin.
External fistulae are low-output fistulae that discharge less than500 ml/day,
and high-output more than 500 ml/day. amount of fistula output has an important metabolic effect.
According to origin in intestine.& by the nature of discharge
Bile stained duodenum, jejunum.
Greenish fluid ,fecal fluid ileum, cecum.
Fecal material distal colon .
complications:
Metabolic effect: high output fistulae lead to loss of intestinal contents with
malabsorption & catabolic state, the metabolic effect include:
Dehydration.
Malnutrition, e.g., hypoalbuminaemia.
Electrolyte disturbances as hypontraemia, hypokalaemia.
Acid-base disturbance causes acidosis.
2. Sepsis If fistula track is not effectively walled off, and enteric contents escape producing an intraperitoneal abscess.
3. Skin irritation & maceration due to continuous flow of intestinal contents.
Management:
The great majority of intestinal fistulae heal spontaneously if sepsis is treated, the nutritional status is maintained and distal obstruction is relieved. 1.Resuscitation &skin protection :I.V.fluid ,blood,correct electrolyte &skin protection
2Nutritional support.: TPN for high output, entral feeding for low output fistula.
3.Investigations & treat sepsis: to know: level of fistula ,bowel disease, distal obstruction ,sepsis by:
1.clinical assessment,
2.fistulography &.Ba follow through,
3.U/S or CT scan for abscess to be treated or aspirated.
4.Suppression of intestinal secretion by Somatostatin.
5.Definitive Treatment
External Fistula:conservative treatment succeeds mostly.
Surgery :If no improvement after 6-8 weeks , Distal obstruction , Active disease Malignancy or Crohn's , Total discontinuity of bowel ends , Mucocutaneous continuity , Excision of the fistula correct pathology .
Internal Fistula: spontaneous closure rare. Many internal fistulae need no correction. Surgery indicated : Internal fistula to urinary bladder.
Fistula Bypassing long segment of bowel causing malabsorption
A is a blind pouch that is continuous with the lumen of a hollow viscus (gut or urinary bladder).
Diverticula can occur anywhere in the bowel from the duodenum down to the sigmoid colon. common ones, however, are diverticula of the colon and
Meckel's Diverticulum:
It is the most prevalent cong. Anomaly of of gastrointestinal tract .it is caused by persistant patency of proximal part of vitello intestinal duct of embryo the abnormal persistence of the duct may have anomalies as well:
A fecal fistula connecting the ileum with the umbilicus, caused by persistent patency of the whole vitello-intestinal duct
A fibrous band remaining obliteration of the duct. An enterocyst that results from the persistent patency of the middle part of the duct
A umbilical extremity of the duct is everted producing an umbilical polyp
Pathology
Meckel's diverticulum is a true diverticulum that incorporate whole layers of the bowel wall. It lies on antimesenteric border, and has its separate blood supply via a branch of sup. Mesenteric artery .It may contain ectopic mucosa and sometimes pancreatic and colonic cells. Rule of 2-3as an approximation :
It occur 2-3% of population It averages 2-3 inches in length
It situated in ileum 2-3 feet from the cecum
Symptoms are due to complications which occur in about 2-3% of affected people
Complications:
Intestinal obstruction is the commonest complication. be due to a.Intussusception: The ectopic mucosa at the base of the diverticulum acts as a foreign body and forms the apex of an ilea-ileal intussusception.
b.Pressure on an intestinal loop by a fibrous band or rotation of the ileum around its axis (volvulus).
2. Incarceration in an inguinal or a femoral hernia is called Littre's hernia.
3. Peptic ulceration and bleeding are caused by the ectopic gastric mucosa,. Bleeding from Meckel's diverticulum is the commonest cause of lower gastrointestinal bleeding in children.
4. Acute diverticulitis is similar to acute appendicitis. Gangrene and perforation may occur and leads to peritonitis .
Clinical Picture:
Accidental at surgery.
Complication like I.O.,painless rectal bleeding.
Acute abdomen like in acute appendicitis
Treatment:
Symptomatic resection is indicated.
Accidentally discovered at surgery
resection is indicated in children & young adults & in those with an attached band..
in patient over 40 years old NO need for surgery
Diverticular disease of the colon
Aetiology:Lack of fibers in nthe diet leading to chronic constipation & increased intra luminal colonic pressure,increase muscle spasm may play a role.
Pathology:it is a pulsion diverticulum of the colonic mucosa through the circular muscle layerat the points of entry of the blood vessels between the tenia coli on the anti mesenteric border.
The Sigmoid colon is the most affected part, but any part could be affected except the rectum.
Complication :
Acute Diverticulitis: Is inflammation of one or more of the diverticula secondary to obstruction of the neck.
Perforation leading to localized or generalized peritonitis.
Recurrent attacks of inflammation.
Bleeding due to erosion of blood vessels.
Stricture chronic distension I.O.
Fistula formation ( colovesical , colointestinsl.)
Clinical Picture:
Age above 40 years.
Asymptommatic recurrent attacks of lower abdominal pain, distension.& Flatulence .
Acute Diverticulitis mimic acute appendicitis but on the left side . It may be complicated by pericolic abscess & peritonitis.
Chronic diverticulitis, recurrent attacks of blood and mucus per rectum,palpable tender mass in LIF mimic colon cancer.
Fresh bleeding per rectum (massive bleeding) should be differentiated from angiodysplasia by angiography, Ca colon bleeding not massive.
Investigation:
1. Ba enema.: in early stage show saw teeth appearance ,fully developed diverticula will be visualized, In acute case Barium enema is contra-indicated .
2. Sigmoidoscopy: detect the mouth of the diverticula.
3. CT scan reveals thickenings of the wall ,peridiverticular abscess.
Treatment:
In stage of diverticulosis high fiber diet , antispasmodic for colic
Acute diverticuliculitis treated as appendicular mass.
If peri-colic abscess drainage should be done.
Generalized peritonitis laparotomy, resect the affected part with colostomy, Hartmann's procedure ,peritoneal toilet and drainage ,exteriorization of perforated segment is less successful option.
Chronic diverticulitis colectomy after adequate preparation.
Bleeding in majority of cases stop spontaneously with conservative treatment ,if continued & massive angiography and urgent colectomy.
Inflammatory Bowel Diseases:
Ulcerative Colitis ,Crohn's Disease ,(Main Diseases)
Others : schistosomal colitis, ileocecal T.B., amoebic colitis, typhoid enteritis.
Ulcerative Colitis:
Inflammatory disease of the colon characterized by ulcerations
Aetiology:
unknown, immunologic, genetic, & environmental factors could be causes.
Pathology:
The disease begins at the dentate line of the anal canal and extends proximally.Extension is continuous with no skip areas of normal bowel.
The extent of the disease varies from rectal involvement alone (proctitis), to w hole colon and rectum affection (pancolitis )
Unlike Grahn's disease, only the mucosa and submucosa are involved.
The mucosal affection varies from granularity to extensive ulceration.
The characteristic histological feature is the formation of crypt abscesses in the depths of the glandular tubules with surrounding inflammation.
The abscesses fuse to form ulcers.6Pseudopolyps are likely to be found.
Complication:
Intestinal:
1.Toxic mega colon 3-5%
2.Hemorrhage
3.Colon cancer: patient with pan colitis more than 10 years at a higher risk
Extra intestinal
include a1ihritis, uveitis, cholangitis, liver cirrhosis, and skin lesions as pyodemia gangrenosum, and erythema nodosum.
Clinical Picture:
The disease is more common in females.
Age 3rd 4th decade
Presented with watery diarrhea mixed with blood,pus,mucous & tenesmus
Pain, fever, weight loss, & dehydration'.
Remission & relapse.
Toxic mega colon
.Serious complication, severe diarrhea, with p[assage of blood & mucus,and the patient is very toxic, high fever 39 – 40c .
Abdominal examination reveals severe abdominal distension due to markedcolonic atony need urgent treatment it is Fatal
Treatment
Medical treatment:
Correction of anemia and hypokalaemiabyb proper dieting, supplementary vitamins & minerals
Sulphasalazine 2-6 gm/day according to severity. Salazopyrine is a combination of Sulpha and salicylate is an effective therapy.
Attacks of exacerbation treated by corticosteroid either systemic or by enema in localized cases to rectum.
Metronidazole also used.
Investigation
1.Laboratory finding:
Anemia, Leukocytosis, hypoproteinemia, & hypokalemia in severe cases.
2.Ba enema:
Mucosal irregularity and ulcers, colonic shortening and loss of haustration.
3.Colonoscopy:
Ulcers can be seen and biopsy taken.
Colonoscopy, biopsy ,& Ba enema are contraindicated in toxic mega colon.
Surgical treatment:
Indications:
Failure of medical treatment
Development of complications as toxic mega colon with perforation (Urgent) or cancer
Long standing pancolitis where biopsies show dysplasia.
Stricture formation.
Surgery:
Excision of whole colon and rectum [panproctocolitis] with permanent ileostomy.
Colectomywith ileo-rectal anastomosis, follow up for rectum for fear of developing cancer
Proctocolectomywith distal rectal mucosectomy with ileal pouch and ileoanal anastomosis
Crohn's Disease
It is idiopathic, chronic transmural inflammatory bowel disease that can involve any area in G.I.T.
Aetiology
Unknown, heredity can play role; focal ischemia is postulated as cause.
Pathology
The commonest site is distal ileum hence the old name is Regional Ileitis, any paet from the mouth to the anus can affected, colon next affected, followed by anal canal.
Chronic disease with granuloma formation
The affected bowel segment the wall from mucosa to serosa thickened,the mesentery thickened and contains large lymph nodes.
Skip lesion area affected between two normal areas.
In long standing cases multiple fissures occur between which the mucosa is edematous giving a coble stone appearance.
Microscopically there is non caseating granulomatous infiltration of the lymphatics of submucosa with presence of giant cells, in late cases fibrosis extends in to and obliterates the submucosa.
Complications: Intestinal:
stricture of small bowel intestinal obstruction.
Abscess & fistula to other loop, bladder, vagina, skin.
Perianal abscess, anal fistula & fissure.
Malabsorption in extensive disease.
Extra Intestinal: Ocular, joint, skin & hepatobiliary.
Clinical Picture :
Age 2nd to 4th decades, male = female.
Symptoms diarrhoea, abdominal pain, weakness, weight loss, anorectal disease.
In old standing cases the patient present with intestinal obstruction.
Signs include: Anemia, malnutrition & possibly a mass in R.I.F.
Investigations:
Ba meal & follow through for small bowel & Ba enema for colon disease.
Radiography shows stricture, skip lesion, cobble stone appearance, internal or external fistula, the finding of a narrowed terminal ileum is known as String Sign of & Kantor .
Colonoscopy & Biopsy of large bowel lesions to prove diagnosis
Biopsy of suspected anal fissures & fistula.
Treatment:
Low residue diet, high protein, high caloric diet with supplementary vitamins & minerals.
Antispasmodics for pain
Corticosteroid & antibiotic (Sulphasalazine or Flagyl) are also given.
Immunosuppression like Azathioprim drug.