Medically compromised patient
Heart failureHeart failure
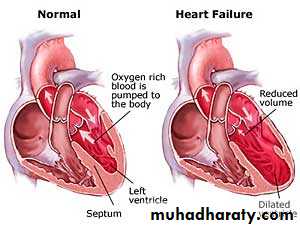
Heart failure is defined as a complex clinical syndrome that may result from any structural or functional cardiac disorder that impairs the ability of the ventricle to fill with or eject blood which leads to blood output insufficient to meet the body requirement. . Prevalence is 1-3% of the general population and 10% among the elderly population. The prognosis is poor 25-50% of the patients die within 5 years.Causes :
Heart failure is a symptom complex that is caused by many diseases such as:• ischemic heart diseases (the most common cause).
• congenital heart diseases. 9. valvular heart diseases
• hypertension. 10. endocrine diseases
• pulmonary hypertension. 11. chronic anemia
• pulmonary embolism. 12. and arrhythmias.
• myocarditis.
• infective endocarditis.
• cardiomyopathies.,,
Classification
The American Heart Association and the American College of Cardiology (AHA / ACC) classify heart failure into 4 stages:
Stage A: patients with risk factors that predispose to HF but with no left ventricular hypertrophy or dysfunction.
Stage B: patients With risk factors that predispose to HF with left ventricular hypertrophy or dysfunction but with no symptoms.
Stage C: patients with past or present symptoms of HF with structural heart disease.
stage D: patients with refractory HF who require specialized care.
Based on severity of symptoms and the amount of effort needed to elicit symptoms,
another classification was developed by the New York Heart Association (NYHA); it is complementary to the previous system.
Class I: N o limitation of physical activity, no signs or symptoms with ordinary activity.
Class II: Slight limitation of the physical activity but the patients remains comfortable at rest.
Class III: Marked limitation of activity but the patients are comfortable at rest.
Class IV: Symptoms are present at rest and physical activity exacerbates the symptoms.
Signs and Symptoms
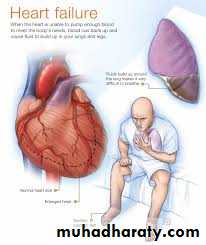
• Dyspnea (perceived shortness of breath).• Fatigue and weakness (especially muscular).
• Orthopnea (dyspnea in recumbent position)
• Paroxysmal nocturnal dyspnea (dyspnea that awakens patient from sleep)
• Acute pulmonary edema (cough or progressive dyspnea)
• Exercise intolerance (inability to climb a flight of stairs)
• Dependent peripheral edema (swelling of feet and ankles after standing or walking)
• Report of weight gain or increased abdominal girth (fluid "' " accumulation; ascites)
• Right upper quadrant pain (liver congestion) .
• Anorexia, nausea, vomiting, constipation (bowel edema)
• Cheyne-Stokes respiration (hyperventilation alternating with apnea during sleep)
• Heart murmur.
• Increased venous pressure.
• Distended neck veins.• Cyanosis
• Clubbing of fingers
Diagnosis
Heart failure is diagnosed clinically and by chest radiography (cardiomegaly), echocardiography, ECG and biochemistry. Echocardiography determines the stroke volume (SV; the amount of blood that exits the ventricles with each heartbeat), the end-diastolic volume (EDV; the amount of blood at the end of diastole), and the SV in proportion to the EDV (the ejection fraction; EF). Normally, the EF should lie between 50 and 70% but, in cardiac failure, it is < 40%.chest radiography (cardiomegaly),
Management :The management depends on the stage of the disease but the general lines of treatment are:
• General measures: rest, control of stress, salt restriction and controlling hypertension, anemia or any underlying causes.
• Angiotensin-converting enzyme inhibitors ACE-I; like enalopril and lisinopril.
• Angiotensin II receptor blockers; like losartan and valsartan.
• Vasodilators like isorbide dinitrate plus hydralazine.
• Diuretics like furosemide and spironolactone
• Digoxin may be helpful when failure 18 associated with atrial fibrillation .• Supplemental oxygen may be required.
• Heart transplantation.
Dental management
• Vital signs (i.e., pulse rate(PR) and rhythm, blood pressure (BP), respiratory rate (RR).
• For patients with symptoms of untreated or uncontrolled heart failure, defer elective dental care and refer to physician.
• Drug considerations:
• For patients taking digitalis,• avoid adrenalin. if considered essential, use cautiously (maximum 0.036 mg adrenalin or 0.20 mg levonordefrin), which is no more than 2 cartridges containing 1:100.000 adrenalin or 1: 20.000 levonordefrin with care to avoid intravascular injection.
• avoid gag reflex.
• avoid erythromycin and clarithrornycin, which may increase the absorption of digitalis and lead to toxicity.
• For patients with NYHA class III and IV congestive heart failure, avoid use of vasoconstrictors; if use is considered essential, discuss with physician.
Avoid adrenalin-impregnated retraction cord.
• Schedule short, stress-free appointments
• Use semi-supine or upright chair position.
• Watch for orthostatic hypotension, make position of chair changes slowly, and assist patient into and out of chair.
• Avoid the use of nonsteroidal anti-inflammatory drugs (NSAIDs) because they can exacerbate symptoms of heart failure.
• Watch for signs of digitalis toxicity (tachycardia, hyper salivation, visual disturbances) which if it occurs the patient must be referred to physician promptly
• Nitrous oxide / oxygen sedation may be used with a minimum of 30% .
Oral manifestations
No oral manifestations are related to heart failure but some drugs can cause:
• Dry mouth in patients taking diuretics or vasodilators.
• Angioedema of lip, face, or tongue, taste changes, burning mouth in patients taking ACE inhibitors.
• Lichenoid reactions in patients taking ACE inhibitors and Beta blockers.
• Increased gag reflex and hyper salivation in patients taking Digitalis.
• Lupus like lesions and lymphadenopathy in patients taking vasodilators.
• Cardiac Arrhythmias
Cardiac Arrhythmias
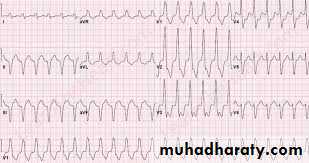
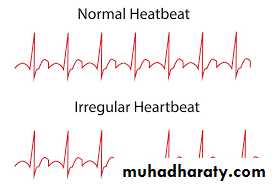
Arrhythmia is simply defined as disturbance of heartbeat including disturbance rhythm, rate or conduction pattern of the heart, in which there is abnormal electrical activity in the heart. 15% of the population may have arrhythmias and the prevalence increases with age. It has been shown that potentially fatal arrhythmias can be precipitated by strong emotion such as anxiety or anger, as well as by various drugs, both of which can be precipitated by dental treatment.Classification
They are classified according to:• Rate into: tachycardia and bradycardia.
• Mechanism into: automaticity, reentry and fibrillation.
• Site of origin into: supraventricular and ventricular arrhythmias.
Clinical features
Signs include; slow (less than 60 beat/ min) or fast (more than 100 beat / min heart rate, irregular rhythm.Symptoms include; palpitation, dizziness, syncope, angina pectoris, or dyspnea. the primary tool for diagnosis of arrhythmia is electrocardiogram (ECG).
Medical management
• Physical maneuvers. In supraventricular arrhythmias, pressure on the neck may increase parasympathetic stimulation to the heart ' inhibiting electrical conduction through the AV nodes.• Antiarrhythmic drugs; these are divided into 4 classes:
• class I are sodium channel blockers.
• class II drugs are beta blockers.
• class III drugs act on' potassium channels and prolong the duration of action potential,
• While class IV drugs are calcium channel blockers.
• Defibrillation and cardioversion .
• Pacemakers. Which Is a subcutaneously implanted generator in the left infraclavicular area, it produces an electrical impulse that is transmitted by a lead inserted into the heart Via subclavian vein to an electrode in contact with endocardial or myocardial tissue.
• Implanted cardioverter-defebrilator (ICD) which is similar to pacemaker. Both are subject to electromagnetic interferences (EMI).
• Radiofrequency catheter ablation. In which a catheter is introduced through the vein to the area Which is the source of arrhythmia, radiofrequency energy is then delivered that cause irreversible tissue destruction
• Surgery
• Anticoagulants.
Dental management
Stress associated with dental treatment or excessive amounts of injected adrenalin may lead to life threatening cardiac arrhythmias in susceptible dental patients. The keys to successful dental management of patients prone to developing a cardiac arrhythmia and those with an existing arrhythmia are identification and prevention.+Patient does not report an arrhythmia, but may beth one or more of the antiarrhythmic drugs
• Patients with cardiac arrhythmias may be identified by the following:
• Medical history to identify : type of arrhythmia, treatment, presence of pacemaker or defibrillator and stability. The dentist may need to consult with physician to obtain or verify this information• Risk for arrhythmia is increased in the presence of other cardiovascular or pulmonary disease
• Patient does not report an arrhythmia, but may be taking one or more of the antiarrhythmic drugs
• The presence of symptoms that could be caused by arrhythmias.
• Vital signs are suggestive of arrhythmia (rapid pulse rate, slow pulse rate, irregular pulse)
Refer patient to physician if signs or Symptoms are present that are suggestive of a cardiac arrhythmia or other cardiovascular disease
Cardiac arrhythmias that may be associated with major perioperative risk during dental treatment include: '
• High-grade atrioventricular (AV) block.
• Symptomatic ventricular arrhythmias in the presence of underlying heart disease.
• Supraventricular arrhythmias with uncontrolled ventricular rate.
Elective dental treatment is avoided in such cases, only urgent care is provided and preferably in hospital, the following should be considered:
• Consult with physician.
• Provide limited care only for pain control, treatment of acute infection, or control of bleeding.
• Intravenous line.
• Sedation
• Electrocardiogram (ECG) monitoring
• Pulse oximeter
• Blood pressure monitoring
• Avoid or limit adrenalin.
Other types of cardiac arrhythmias are associated with intermediate or minor perioperative risk during dental treatment in such cases elective dental treatment is allowed :
• Stress and anxiety reduction
• Establish good rapport.
• Schedule short, morning appointments.
• Ensure comfortable chair position.
• Provide preoperative sedation (short acting benzodiazepine night before and / or 1 hour before appointment).
• Administer intraoperative sedation (nitrous oxide / oxygen)
• Obtain pretreatment vital signs.
• Ensure profound local anesthesia.
• Provide adequate postoperative analgesia.
The use vasoconstrictors :
• Adrenalin-containing local anesthetic can be used With minimal risk if the dose is limited to 0.036 mg epinephrine (2 cartridges containing l:lO0,000 concentration). Higher doses may be tolerated, but the risk Of complications increases with dose
• Avoid the use of adrenalin in retraction cord.
• Patients who are taking Warfarin :
• Should have current international normalized ratio (INR) (Within 24 hours of Surgical procedure). If INR is Within the therapeutic range (INR, 2.0-3.5), dental treatment, including minor oral surgery, can be performed Without stopping or altering the drug.• Local measures include:
• gelatin sponge (Gelfoam)• Oxidized cellulose (surgeseal) in socket.
• Suturing.
• gauze pressure packs
• preoperative stents.
• and tranexamic acid or aminocaproic acid (cyclocapron) mouth rinse and / or to soak gauze.
Patients With pacemakers
• Antibiotic prophylaxis to prevent bacterial endocarditis is not recommended• Avoid the use of electro-surgery and ultrasonic scalars.
Patients taking Digoxin
• Watch for signs or symptoms of toxicity (e. g., hypersalivation)
• Avoid adrenalin or levonordefrine