INTRODUCTION
• To provide best treatment and patient satisfaction,
thorough clinical history, examination and diagnostic
aids are required. Since dental problems are not alike
in two patients, thorough examination, evaluation and
diagnosis of an individual patient guides the effective
treatment plan
• Diagnosis is defined as utilization of scientific
knowledge for identifying a diseased process and to
differentiate it from other disease process.
• In other words, literal meaning of diagnosis is
determination and judgment of variations from the
normal
PATIENT EVALUATION
• The diagnostic process actually consists of four steps:
1. First step: Assemble all the available facts gathered from
chief complaints, medical and dental history, diagnostic tests and investigations.
2. Second step: Analyze and interpret the assembled clues
to reach the tentative or provisional diagnosis
3. Third step: Make differential diagnosis of all possible
diseases which are consistent with signs, symptoms
and test results gathered
4. Fourth step: Select the closest, possible choice
History of Present Illness
• More descriptive analysis about this initial
information
– signs and symptoms
– duration, intensity of pain,
– relieving and exaggerating ( triggering )factors
Examples of
type of the questions
• How long have you had the pain?
• Do you know which tooth it is?
• What initiates pain?
• How would you describe the pain?
– Quality—Dull, Sharp, throbbing, constant
– Location—Localized, diffuse, referred, radiating
– Duration—Seconds, minutes, hours, constant
– Onset—Stimulation required, intermittent,
spontaneous
– Initiated—Cold, heat, palpation, percussion
– Relieved—Cold, heat, any medications, sleep

History of present illness
should indicate severity
and urgency of the
problem.
• If a chief complaint is toothache but
symptoms are too
vague (uncertain
) to
establish a diagnosis,
– analgesics
should be prescribed to help the
patient in tolerating the pain until the toothache
localizes.
• A history of pain which persists without
exacerbation may indicate problem of
nonodontogenic origins.
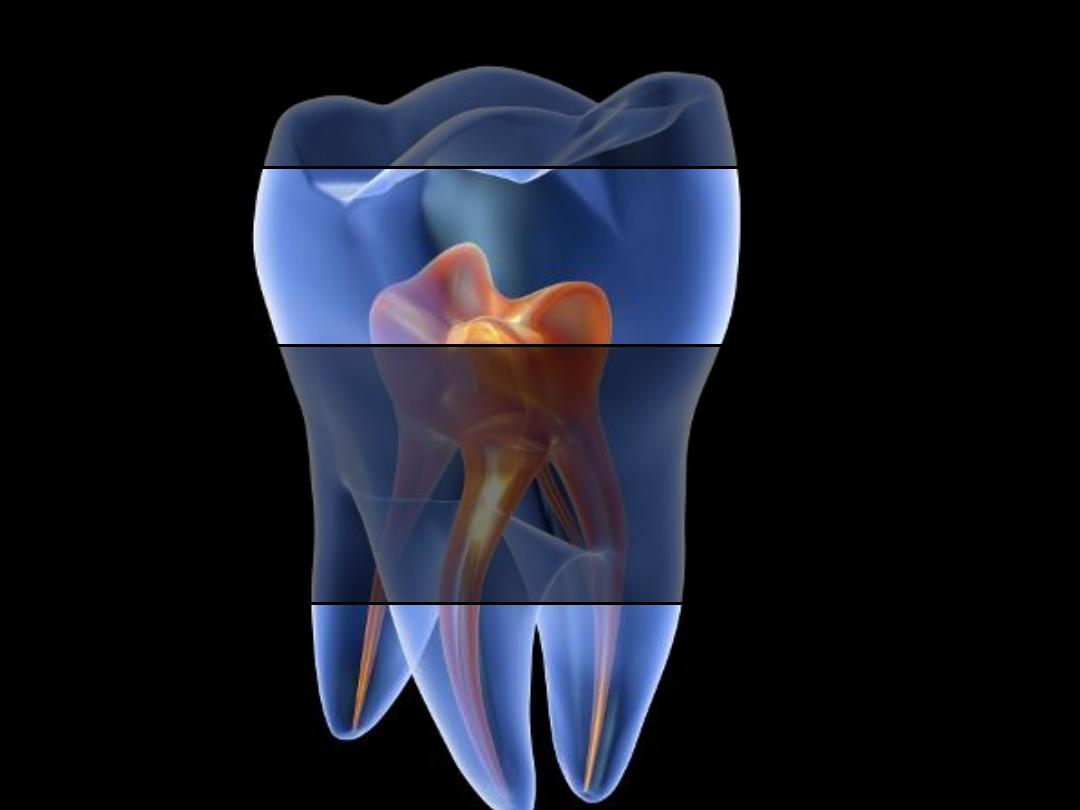
Toothache
• Pulp
• Periodontal ligament
• Pulpal pain can be sharp piercing if A-delta
fibers are stimulated.
• Dull, boring or throbbing pain occurs if there
is stimulation of C-fibers.
Pulpal Pain
Pain from periodontal ligament
• The tooth will be sensitive to;
– percussion
– chewing
– palpation.
• Mild to moderate pain
can be of
pulpal or
periodontal origin
but
acute pain
is commonly
a reliable sign that pain is of
pulpal origin
.
• Localization of pain also tells origin of pain
since pulp does not contain proprioceptive
fibers; it is difficult for patient to localize the
pain unless it reaches the periodontal
ligament
Past Dental History
• This helps to know any previous dental
experience and past restorations.
Communicable Diseases
• Immunocompromised patients
– more prone to suffer from various bacterial,
fungal and viral infections due to suppression of
immuneresponse
Physiological Changes Associated with
Aging
• Physiological changes associated with aging
should be examined properly and should not be
confused with the pathological changes. Changes
in oral cavity occurring due to aging are as
follows:
– Attrition, abrasion and wear of proximal surfaces
– Extrinsic staining
– Edematous gingivae
– Diminished salivary flow
– Gingival recession

EXAMINATION AND DIAGNOSIS
• Clinical examination: It includes both extraoral
and intraoral examination
• Intraoral examination: It includes the
examination of soft and hard tissue.
Clinical Examination
• Following sequence is followed during clinical
examinations
– Inspection
– Palpation
– Percussion
– Auscultation
– Exploration.
Inspection
• Patient should be observed for
– unusual gait and habits (may suggest underlying
systemic disease, drug or alcohol abuse)
– localized swelling,
– presence of bruises,
– abrasions, scars
– signs of trauma
Inspection
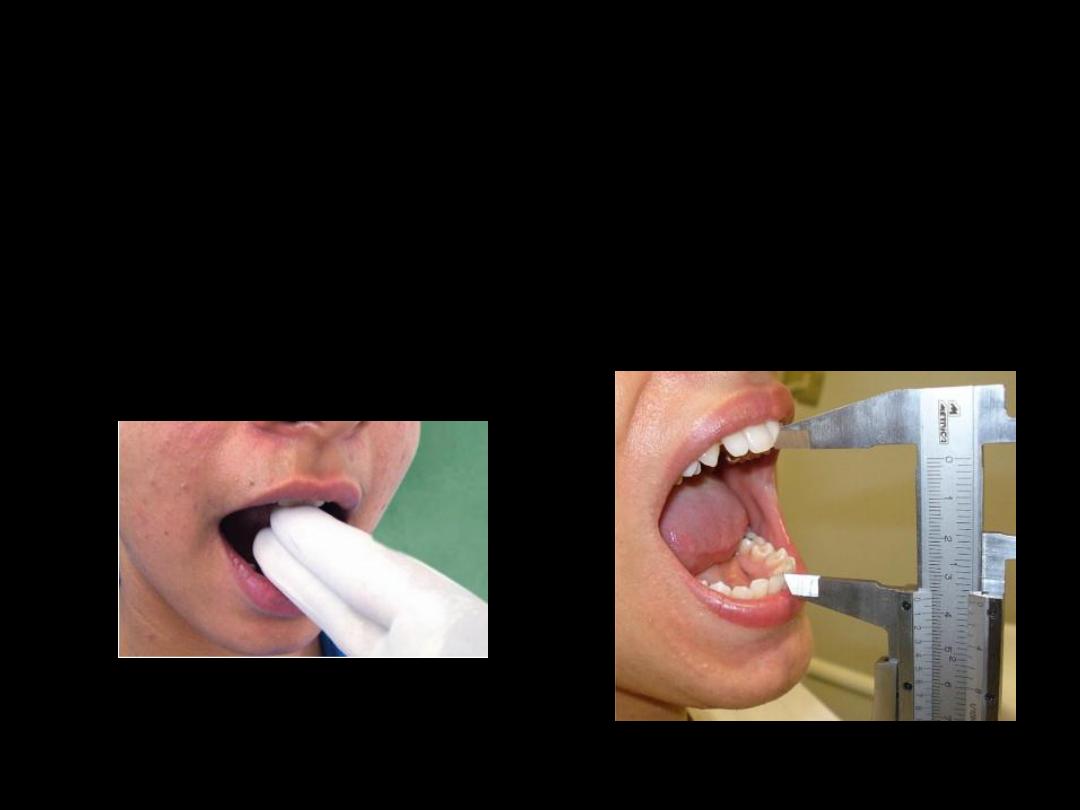
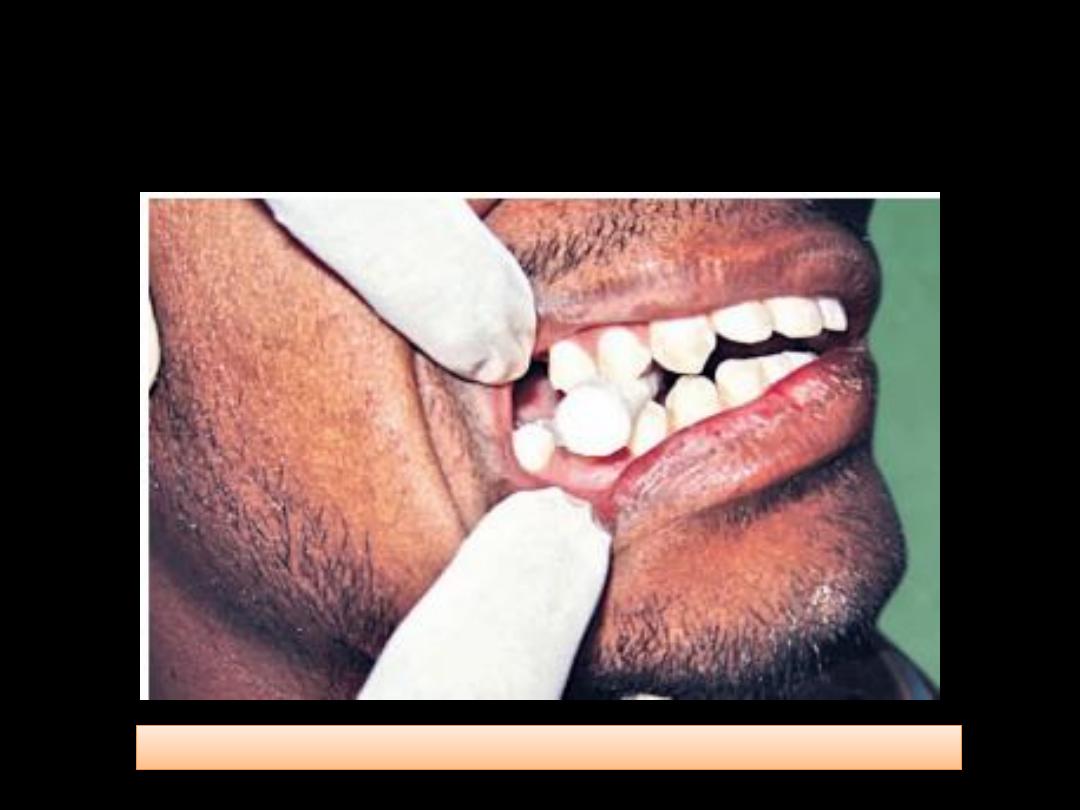
• Degree of mouth opening
– it should be at least two fingers
Inspection
• During intraoral examination, look at the
following structures systematically
– The buccal, labial and alveolar mucosa
– The hard and soft palate
– The floor of the mouth and tongue
– The retromolar region
– The posterior pharyngeal wall and facial pillars
– The salivary gland and orifices.
Inspection (general dental state)
• Oral hygiene status
• Amount and quality of restorative work
• Prevalence of caries
• Missing tooth
• Presence of soft or hard swelling
• Periodontal status
• Presence of any sinus tracts
• Discolored teeth
• Tooth wear and facets
Palpation
• Local rise in temperature
• Tenderness
• Extent of lesion
• Induration
• Fixation to underlying tissues
Percussion
• Percussion
gives information about the
periodontal status
of the tooth
• Percussion of tooth indicates
– inflammation in periodontal ligament which could
be due to
• Trauma
• Sinusitis
• PDL disease
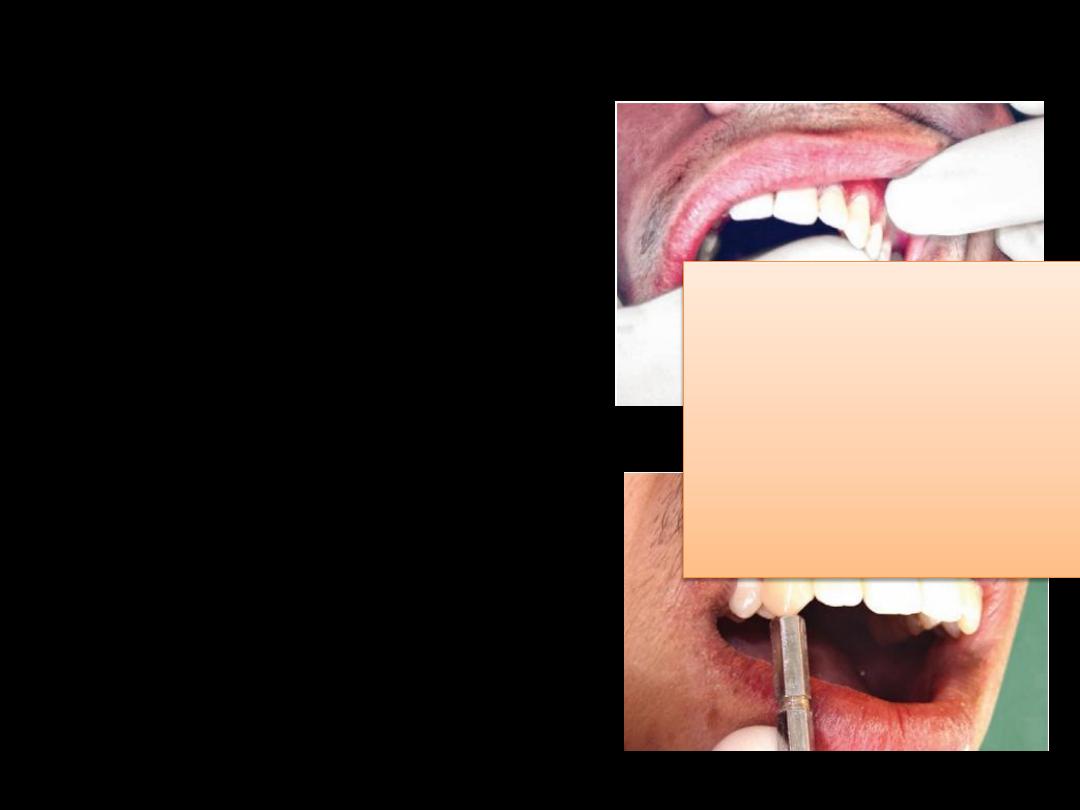
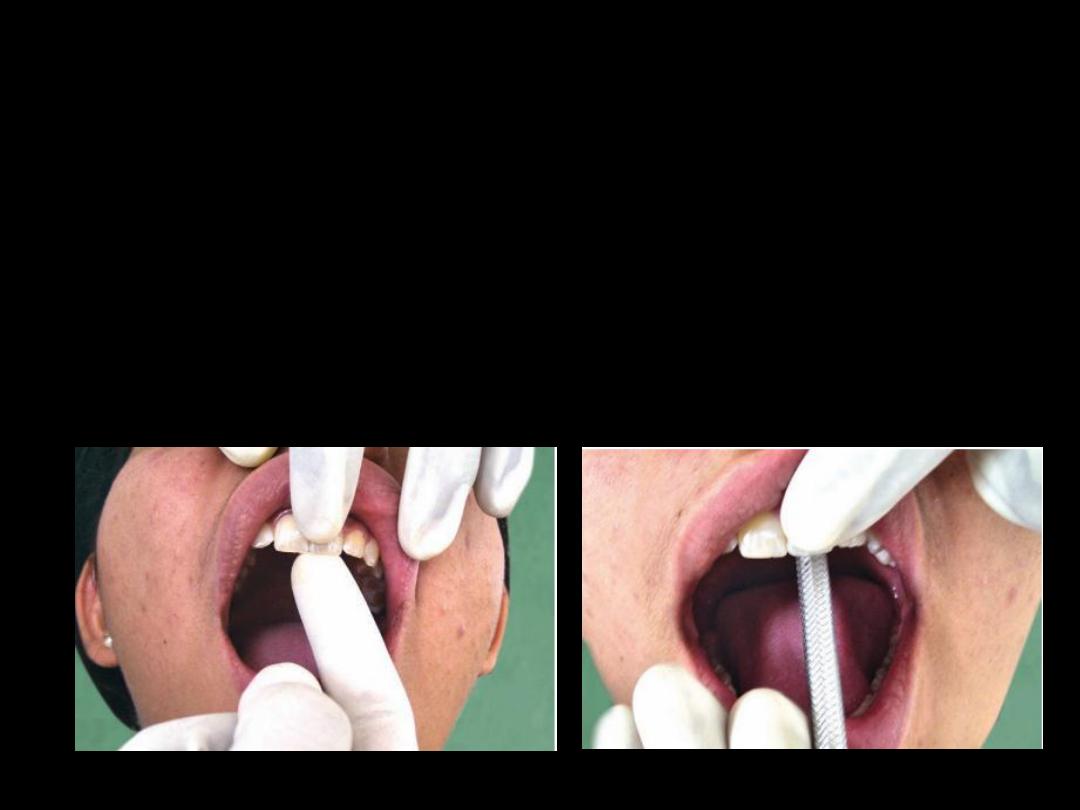
Percussion
• Percussion can be carried
out by gentle tapping
with gloved finger
• blunt handle of mouth
mirror
Each tooth should be percussed on all the
surfaces of tooth until the patient is able to
localize the
tooth with pain. Degree of response to
percussion is directly proportional to
degree of inflammation.
Periodontal Evaluation
• Periodontal examination shows change in
– color
– contour
– form
– density
– level of attachment
– bleeding tendency
Periodontal Evaluation
• The depth of gingival sulcus is determined by
systemic probing using a periodontal probe.
• A sulcus depth
greater than 3 mm
and the
sites that bleed upon probing should be
recorded in the patient’s chart
• The presence of pocket may indicate
periodontal disease
Periodontal Evaluation
• The mobility of a tooth is tested by placing a
finger or blunt end of the instrument on either
side of the crown and pushing it and assessing
any movement with other finger
Periodontal Evaluation
• Grading of mobility
– Slight (normal)
– Moderate mobility within a range of 1 mm.
– Extensive movement (more than 1 mm) in
mesiodistal or lateral direction combined with
vertical displacement in alveolus
Evaluation of Carious Lesions
• Dental caries is diagnosed by the following
– Visual changes in tooth surface
– Tactile sensation while using explorer
– Radiography
• Definite radiolucency indicating a break in the
continuity of enamel is carious enamel
– Transillumination

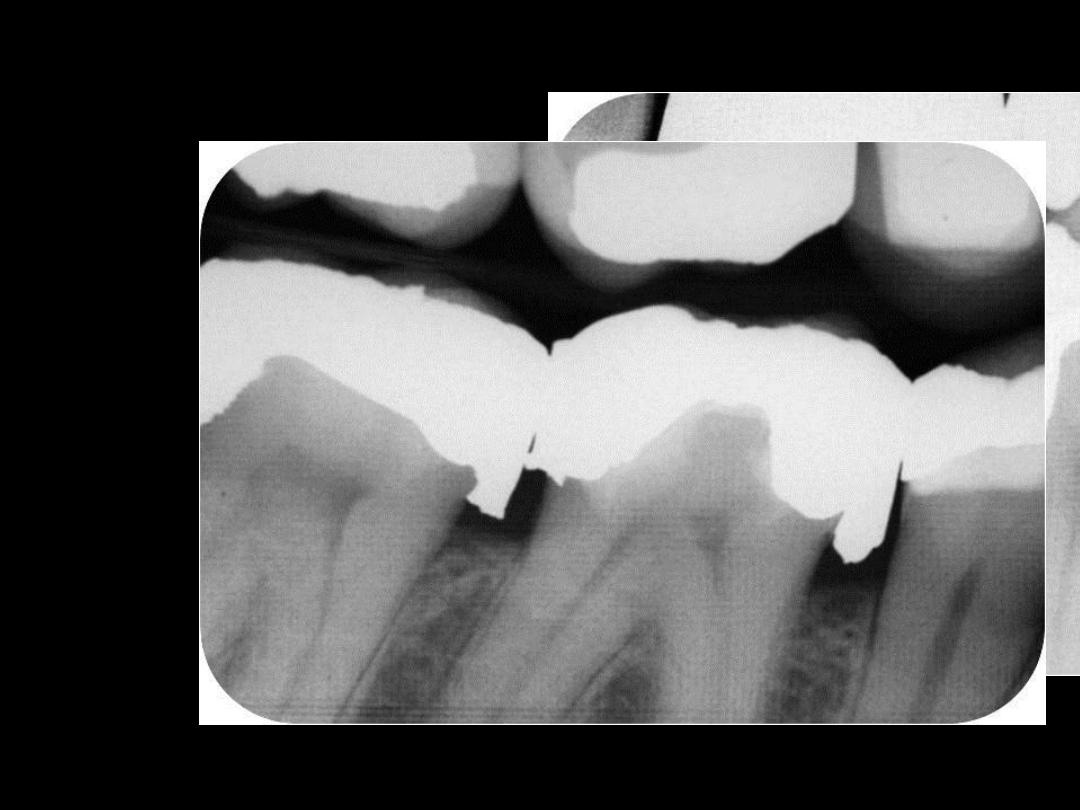
Evaluation of Existing Restorations
• Proximal overhangs
– Proximal restoration is evaluated by moving the
explorer back and forth across it. If the explorer
stops at the junction and then moves onto the
restoration, an overhang is present. This should be
corrected, as it can result in the inflammation of
the adjacent soft tissues.

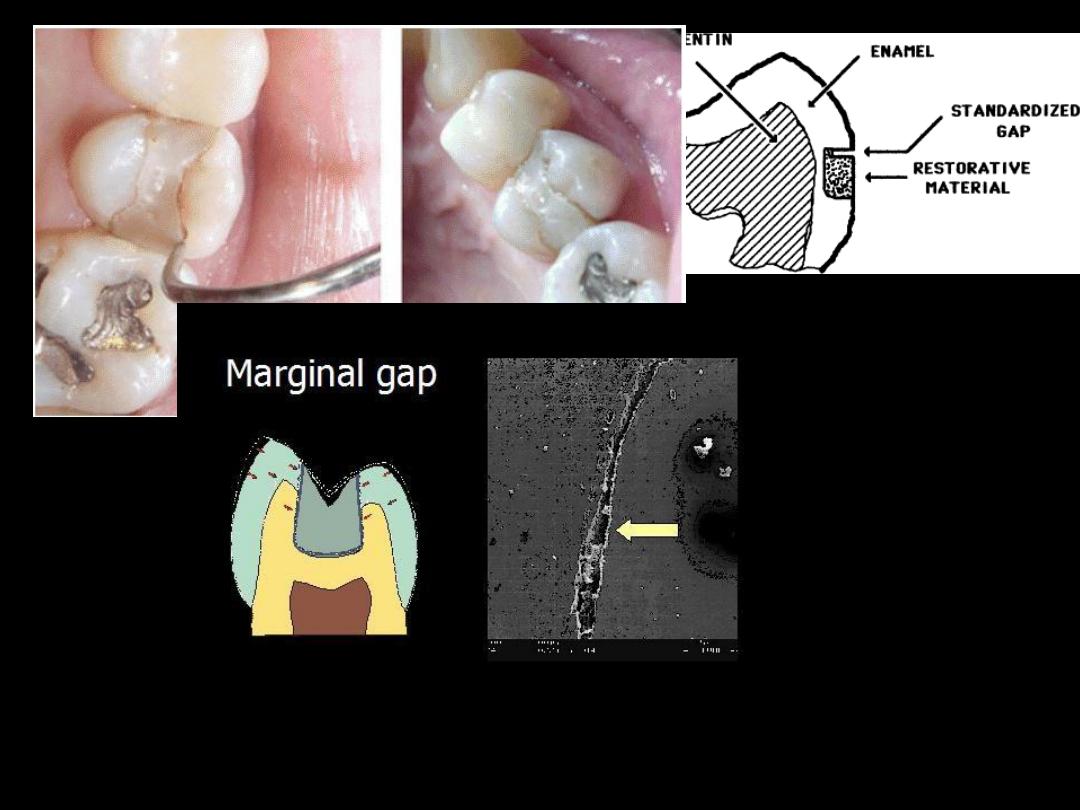
• Marginal gap or ditching:
It is the deterioration
of the restoration-tooth interface on occlusal
surfaces as a result of wear or fracture. Shallow
ditching, less than 0.5 mm deep usually requires
patchwork repair. If ditch is too deep,
restoration should be completely replaced
• Fracture line:
A fracture line that occurs in the
isthmus region generally indicates fractured
restoration which needs replacement

• Recurrent caries
at the margin of the
restoration also indicate repair or replacement
of the restoration
Radiograph
• Most important tools in making a diagnosis.
• Without radiograph, case selection, diagnosis
and treatment
would be impossible
as it helps
in examination of oral structure that would
otherwise be unseen by naked eye.
• Radiographs help to diagnose tooth related
problems like
– Caries
– Fractures
– root canal treatment
– any previous restorations
– abnormal appearance of pulpal or periradicular
tissues
– periodontal diseases and the general bone pattern
Periapical lesions of endodontic origin have
following characteristic features
• Loss of lamina dura in the apical region
• Etiology of pulpal necrosis is generally
apparent
• Radiolucency remains at the apex even if
radiograph is taken by changing the angle.
Indications of dental radiographs
• Deep carious lesion
• Large restoration
• History of pain
• History of trauma
• History of root canal
treatment
• History of periodontal
therapy
• Family history of dental
anomalies
• Impacted teeth
• Mobility of teeth
• Swelling in relation to teeth
• Presence of sinus/fistula
• Unusual tooth morphology
• Missing teeth with
unknown reasons
• Growth abnormalities.
Disadvantages of radiographs
• Radiograph gives two dimensional picture of a
three dimensional object
• Caries is always more extensive clinically
when compared to radiograph
Healthy (Normal) Pulp
• pulp is vital, without inflammation.
• asymptomatic, react to vitality tests such as
heat, carbon dioxide(CO2) snow, ice and/or
electric pulp tester (EPT)
• Once the pulp gets ‘older’ it forms increasing
amount of secondary dentin in the pulp
chamber such that its reaction to thermal test
might be diminished, but even in those cases
a healthy pulp should predictably react to EPT
Reversible Pulpitis
• The history of symptoms will most often
reveal pain or sensation on stimulation only,
such that the tooth will only bother the
patient when the tooth is exposed to a
stimulus that is hot and/or cold
• According to the classification, reversible
pulpitis should heal once the irritant is
removed or, in case of an exposed dentin
surface, the exposed dentin is adequately
sealed.
Clinical Characteristics of
Irreversible Pulpitis
• Sharp, severe pain upon thermal stimulation that continues
after stimulus removed.
• Cold is especially uncomfortable although heat, sweet or acids
can elicit (provoke) pain. Later heat intensifies and cold
relieves pain.
• Pain can be spontaneous, continuous and exacerbated when
lying down.
• Early response at low then later at higher threshold to
electrical stimulation or not at all.
• Pain localized early then more diffuse.
• Pain becomes throbbing and keeps the patient awake at night.
Clinical Characteristics of
Irreversible Pulpitis
• As with reversible pulpitis, symptoms can be
very misleading. It has been well documented
that in most cases a pulp that is irreversibly
inflamed is asymptomatic.
• It has been reported that dental pulps can
progress from vitality to necrosis without pain
in 26–60% of all cases
Chronic Hyperplastic Pulpitis
Pulp Polyp
• Uncommon form of pulpitis in which an
inflammatory hyperplasia (granulation tissue)
extrudes to fill a large cavity in the crown
• Usually seen in children or young adults
• Deciduous or permanent mandibular molar
most likely to be involved
• Apex of affected permanent tooth often
incompletely formed

Chronic Hyperplastic Pulpitis
Pulp Polyp
Periapical diagnosis
• The term apical periodontitis implies that there is
inflammation in the periapical tissues
• Like pulpal inflammation, the periapical inflammation
can be symptom free and then may only be
diagnosed on a periapical radiograph;
– however, it is very important to appreciate that a
periapical lesion is most likely caused by an infection in the
root canal system, irrespective of the patient having
history or being symptomatic
PERIAPICAL DISEASE
Classified as:
– Acute Apical Periodonitis
– Acute Apical Abscess
– Chronic Apical Periodontitis
(Suppurative Apical Periodontitis with sinus tract)
– Condensing Osteitis
Periapical Disease
Acute Apical
Periodontitis
Acute Apical Periodontitis
• Mild to severe inflammation that surrounds or
is closely associated with the apex of a tooth.
• Results from:
– Irreversible inflammation or necrotic pulp.
– Trauma or bruxism of normal or reversibly
inflamed pulpitic conditions.
• Consider vertical fractures, periodontal
abscess, and non-odontogenic pain.
Clinical Findings in
Acute Apical Periodontitis
• Visual
– Check for decay, fracture lines, swelling, sinus tracts, orientation of
tooth, and hyperocclusion
• Palpation
– Sensitive (usually on buccal surface)
• Percussion
– Moderate to severe (initially use index finger to reduce patient
discomfort)
• Mobility
– Slight to no mobility (if moderate mobility exists, check for possible
periodontal condition before continuing)
Immediate Treatment of
Acute Periapical Periodontitis
If from irreversible pulpitis:
• Pulpotomy or extraction.
If from necrotic pulp:
• Root canal therapy initiated or extraction.
If from hyperocclusion:
When the pulp is normal or reversibly inflamed, adjusting the occlusion
provides immediate relief. Always consider cracked tooth, irreversible
pulpitis, or necrotic pulp if discomfort persists.
If from bruxism:
A biteguard may be indicated.
Acute Apical Abscess
• Acute inflammation of the periapical tissue
characterized by localized accumulation of pus
at the apex of a tooth.
• A painful condition that results from an
advanced necrotic pulp.
• Patients usually relate previous painful
episode from irreversible or necrotic pulp.
• Swelling, tooth mobility, and fever are seen in
advanced cases.
Symptoms of Acute Apical Abscess
• Spontaneous dull, throbbing, persistent pain;
exacerbated by lying down.
• Percussion:
– Extremely sensitive
• Mobility:
– Horizontal / vertical; often in hyperocclusion
• Palpation:
– Sensitive; vestibular or facial swelling likely
• Thermal:
– No response
Clinical Findings of
Acute Apical Abscess
Visual:
– Check for decay, fracture lines, swelling, sinus tracts, orientation of
tooth, hyperocclusion
Palpation:
– sensitive; intraoral or extraoral swelling present
Percussion:
– Moderate to severe (initially use index finger)
Mobility:
– Slight to none; may be compressible
Perio probing:
– WNL (unless have perio disease or vertical fracture)
Periapical Disease
Chronic Apical
Periodontitis
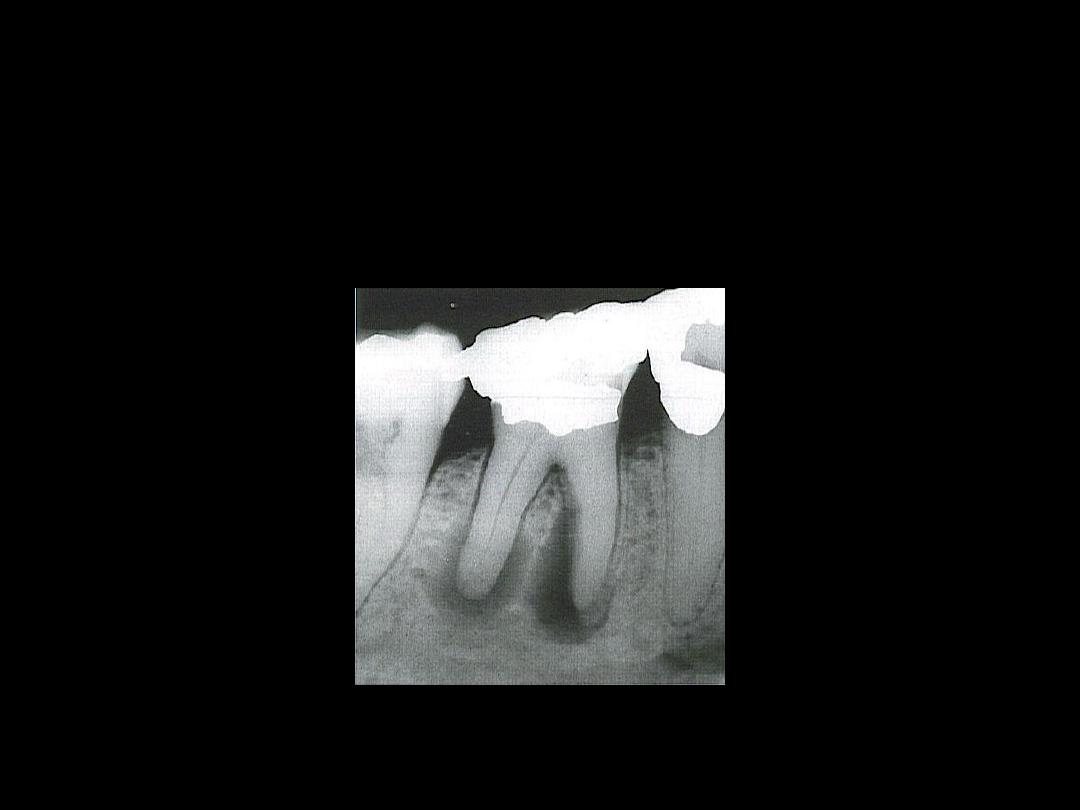
Chronic apical periodontitis. Extensive tissue destruction in the
periapical region of a mandibular first molar occurred as a result
of pulpal necrosis. Lack of symptoms together with presence of
a radiographic lesion is diagnostic.
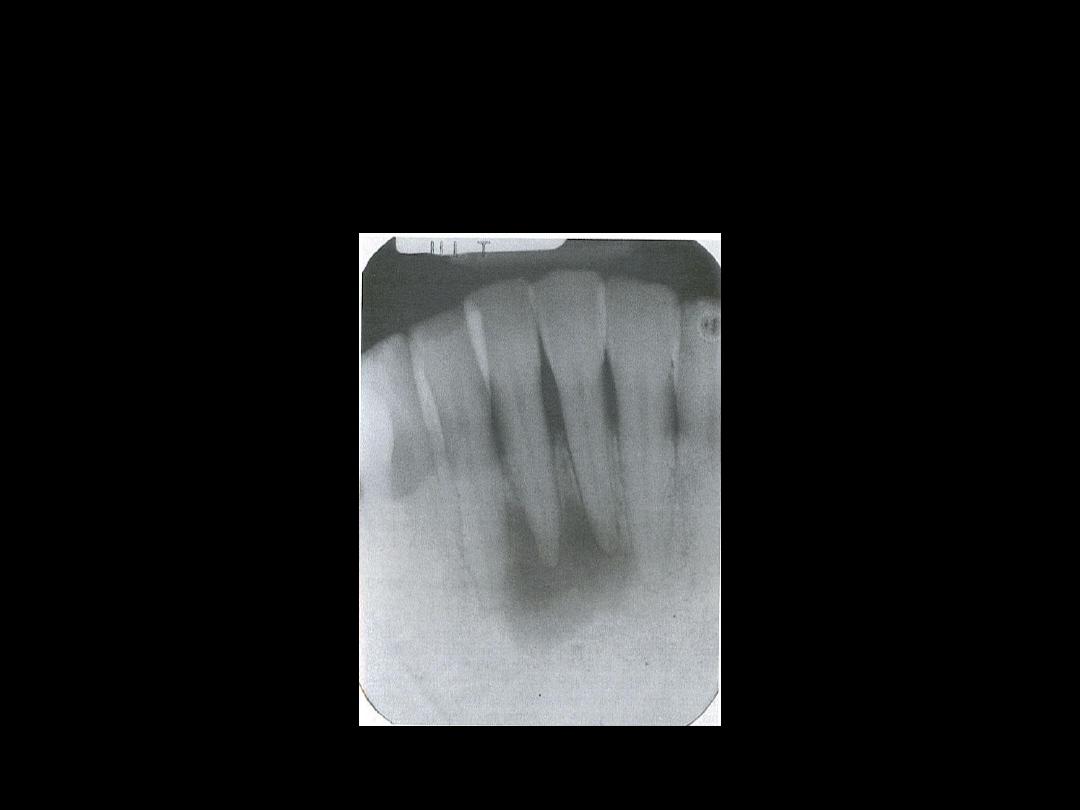
Periapical radiolucencies associated with mandibular incisors.
These teeth were vital, and a diagnosis of cemental dysplasia
was made.
Treatment of Chronic Apical
Periodontitis
(necrotic pulp)
• If asymptomatic, no immediate treatment needed;
schedule for root canal therapy
• If in acute suppurative phase, immediate treatment
same as with acute apical abscess, i.e.,
• Partial instrumentation
of canals:
– Remove all decay, evaluate restorability
– Determine working lengths of all canals
– Achieve apical patency all canals with #10 file, look for
drainage and allow to continue until it stops
– Large canals: up to #35 file, 4mm short of WL
– Smaller canals: up to #25 file, 4mm short of WL
– Alternate with #8 or 10 patency file
Pulp Vitality Tests
• Pulp testing is often referred to as vitality
testing.
• Pulp vitality tests play an important role in
diagnosis because these tests not only
determine the vitality of tooth but also the
pathological status of pulp
Pulp Vitality Tests
• Various types of pulp tests performed
• Thermal test
– Cold test
– Heat test
• Electrical pulp testing
• Test cavity
• Anesthesia testing
• Bite test.
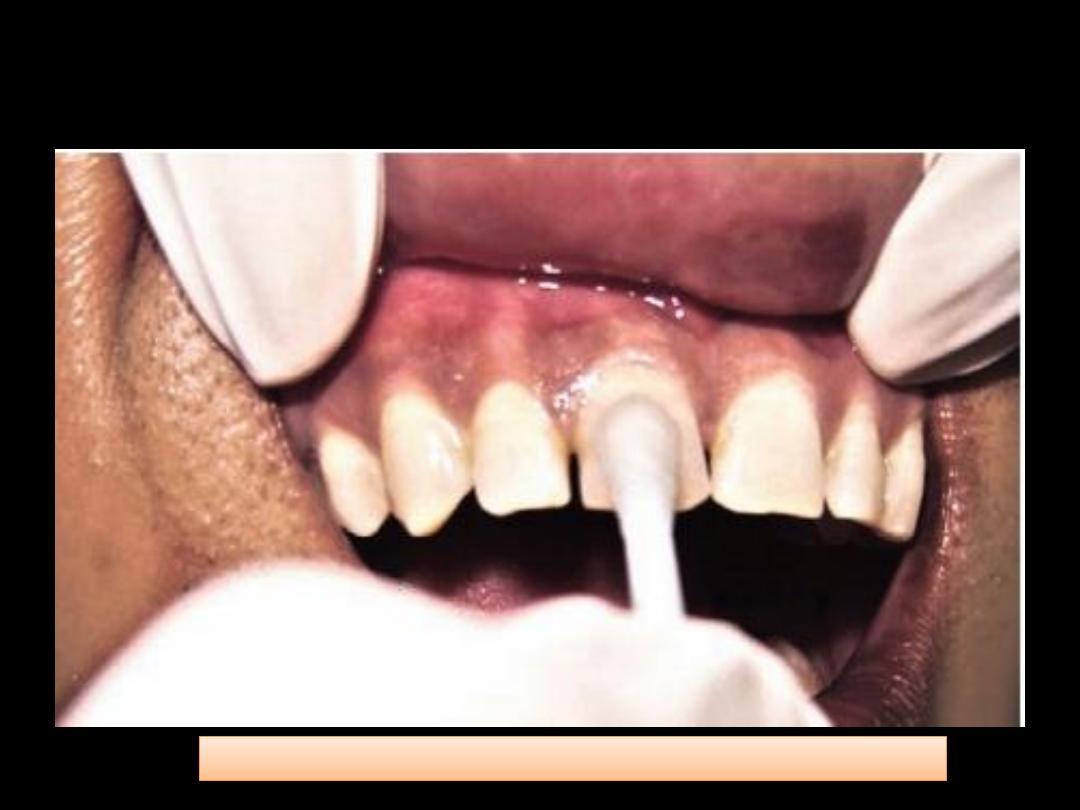
Thermal Test-Cold Test
Cold test using a cotton pellet saturated with ethyl chloride
Thermal Test-Heat test
• It is most advantageous in the condition
where patient’s chief complaint is intense
dental pain upon contact with any hot object
or liquid. It can be performed using different
techniques.
Thermal Test-Heat test
• The easiest method is to direct the warm air
to the exposed surface of tooth and note the
patient response.
• If a higher temperature is needed to illicit a
response, then other options like heated
stopping stick, hot burnisher, hot water, etc.
can be used.
Thermal Test-Heat test
• The patient may respond to heat or cold test
in following possible ways:
– Mild, transitory response to stimulation show
normal pulp.
– Absence of response in combination with other
tests indicates pulp necrosis.
– An exaggerated and lingering response indicate
irreversible pulpitis.
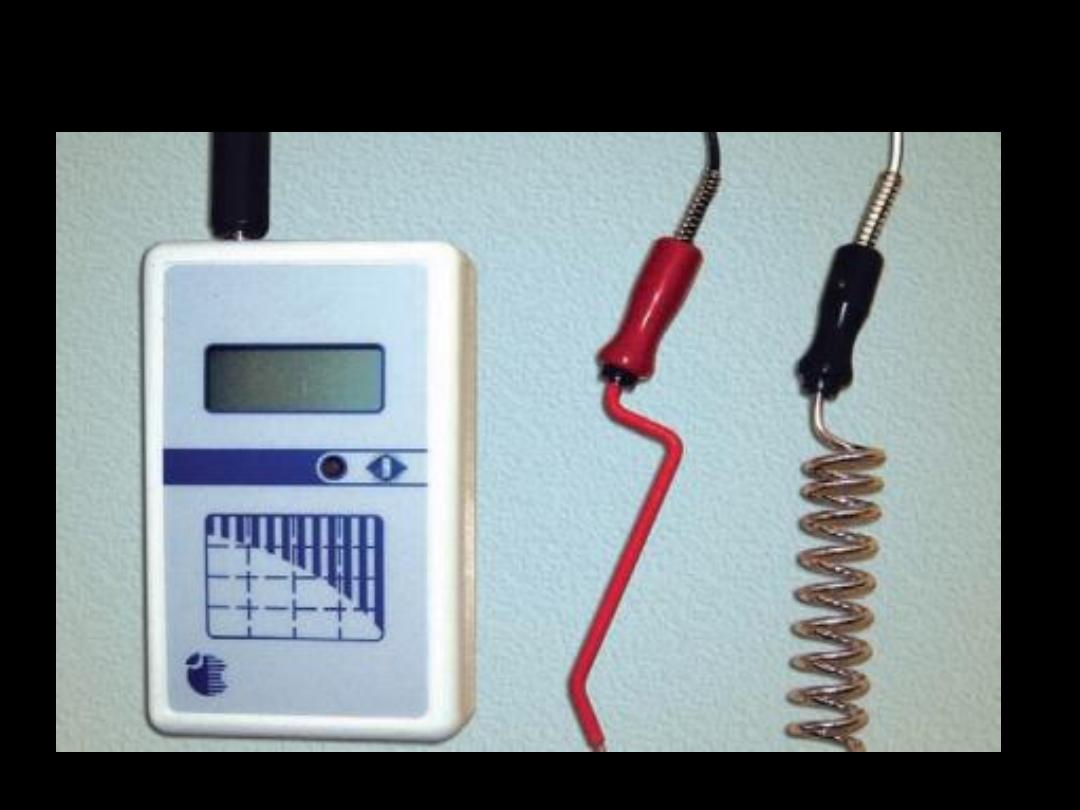
Electric Pulp Testing
• Once the circuit is complete, slowly increase
the current and ask the patient to point out
when the sensation occurs.
• Each tooth should be tested 2 to 3 times and
the average reading is noted. If the vitality of a
tooth is in question, the pulp tester should be
used on the adjacent teeth and the
contralateral tooth, as control
Bite Test
Patient is asked to bite on cotton swab or hard object for bite test
