
Lecture 10 by Prof.Dr.Alaa Fadhil Alwan
Multiple myeloma
Myeloma is a haematological malignancy affecting immunoglobulin-producing plasma cells and
is the second most common of the haematological cancers, accounting for approximately 1% of
all cancers and 10% of all haematological cancers. Myeloma is predominantly a disease of the
elderly. In Europe, the median age at diagnosis is between 65 and 70 years. The incidence rises
exponentially with age, tapering off after the age of 84 years. Only 1% of cases are diagnosed in
people younger than 40 years old. The incidence of myeloma has been increasing over the past
several decades, due in part to better diagnosis and detection. Myeloma is slightly more
common in men than women and twice as common in black African-American populations than
in Caucasians
The major clinical features of myeloma result from:
1.Abnormal accumulation of malignant plasma cells within the bone marrow and other tissues
causing disruption of normal bone marrow function resulting in anemia, low white cell count
(leucopenia) and low platelet count (thrombocytopenia).
2.Destruction of bone caused by localized stimulation of osteoclast function.
3.Synthesis of monoclonal immunoglobulin (M Protein) by the myeloma cells which accumulates
in the blood and urine, causing increased blood viscosity and renal failure
4.Impairment of normal immune function, due to reduced normal immunoglobulin synthesis,
leucopenia and the release of inhibitory cytokines by the myeloma cells.

Clinical Presentation of Myeloma
Patients typically present with symptoms attributable to:
1.Accumulation of malignant plasma cells within the bone marrow and other tissues Destruction
of bone.
2. Accumulation of monoclonal immunoglobulin (M-Protein) with increased blood viscosity and
renal failure
3.Impairment of normal immune function
Investigation of Suspected Myeloma
Patients whose medical history and physical examination indicate the possibility of myeloma
need further investigation to confirm the diagnosis and evaluate the extent of disease.
Diagnostic procedures for evaluation of multiple myeloma typically include : laboratory tests,
bone marrow aspiration and biopsy, and imaging studies.
The initial diagnostic workup in all patients should include a history and physical examination
and the following baseline blood studies:
1.Hematological tests including full blood count (FBC) with skeletal survey with other imaging
studies as required.
2.Bone marrow aspirate and biopsy.
3.Serum protein electrophoresis (SPEP), urine protein electrophoresis (UPEP) and
immunofixation
Once a diagnosis of myeloma has been confirmed, several other tests can provide useful
supplementary information, including:
1.serum β microglobulin,
2.serum C-reactive protein,
3.serum lactic dehydrogenase (LDH) and
4.detection of chromosomal abnormalities using standard cytogenetics or fluorescence in situ
hybridization (FISH
In some patients, supplementary tests may be needed to confirm the diagnosis or to provide
more detailed information to guide treatment:
1.Magnetic resonance imaging (MRI) may be useful if spinal cord compression is suspected.
2.Imaging studies may help to identify plasmacytomas and tissue biopsy may be required for
confirmation
3.Bone marrow immunohistochemistry may be required in some cases to demonstrate clonality
of the plasma cells.
4.Assay for serum free light chains (FREELITE™; FLC’s) is useful for detecting non-secretory
myeloma and AL amyloidosis (National Comprehensive Cancer Network(NCCN) 2008
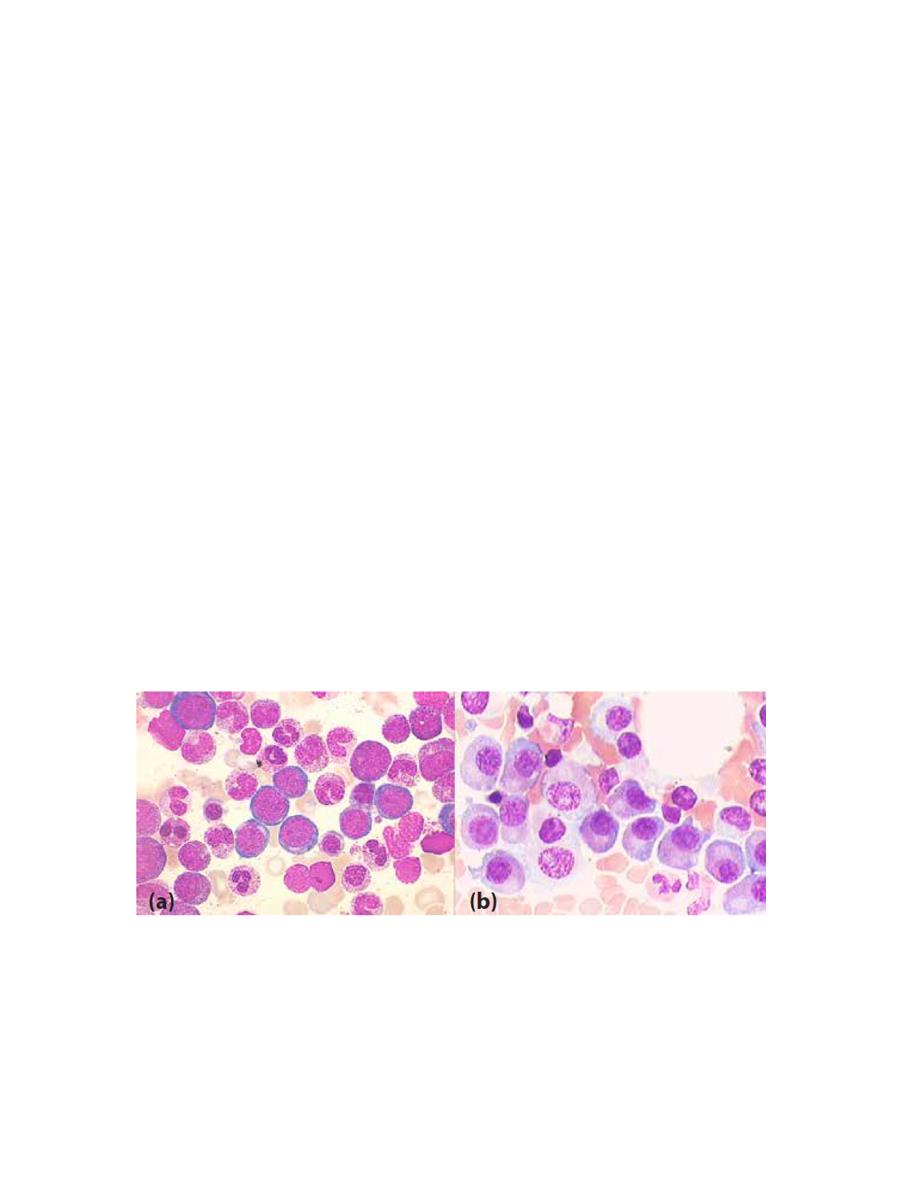
Normal BMA BM with myeloma
M protein is found in serum and/or urine in 98% of myeloma patients and its identification and
quantitation is a central component of the diagnosis of myeloma. In addition, quantitation of M
protein is an important indicator of the success of treatment and progress of the disease:
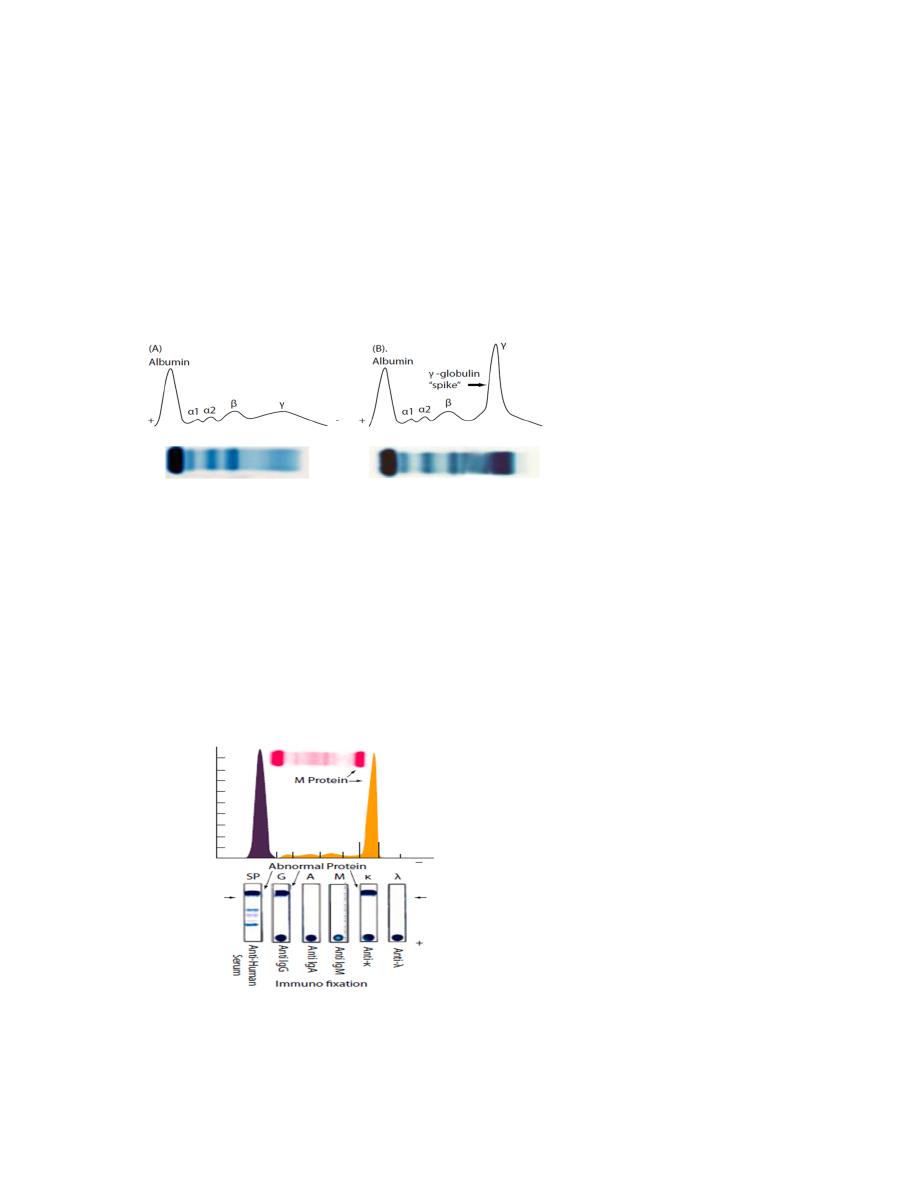
1.Serum and urine protein electrophoresis (SPEP or UPEP): Protein electrophoresis is a
laboratory test that separates different proteins from a sample of blood or urine, based on size
and electrical charge. The proteins are separated into five major groupings called albumin, α1,
α2, β and γ globulins. Albumin, which is produced in the liver, accounts for about 60% of the
protein in the blood
2.Immunoelectrophoresis (IEP): Immunoelectrophoresis (IEP) is a much more sensitive
technique than SPEP and UPEP and provides more specific quantitative information about the
types and amounts of M protein present
3.Immunofixation (IFE): Immunofixation electrophoresis (IFE) is the most sensitive type of
electrophoresis. With this test, a monoclonal antibody is placed in contact with the gel after the
proteins have been separated by electrophoresis. The resulting protein antibody complexes are
then stained for visualisation after being precipitated out. With this technique, a specific
immunoglobulin spike can be identified and classified. Both the heavy and light chains of the M
protein can be identified with IFE
4.Bence Jones protein assay: Bence Jones proteins are free monoclonal immunoglobulin light
chains. They can be detected in the urine using the Bence Jones reaction or UPEP and further
characterised by IEP or IFE. In the Bence Jones reaction, urine is heated to 45–70°C, and any

Bence Jones protein present precipitates. If the urine is heated above or below this range, the
protein goes back into solution. Other clumping procedures use salts, acids and other chemicals
to precipitate the Bence Jones proteins.
5.Serum free light chain assay
6.Laser nephelometer
Standard diagnostic criteria:
The International Myeloma Working Group (IMWG) and Mayo Clinic have established almost
identical criteria for the diagnosis of the plasma cell proliferative disorders.
It’s important to differentiate between MM and MGUS:
MGUS: Monoclonal Gammopathy of Undetermined Significance
1.M-protein in serum < 3 g/dL.
2.Less than10% bone marrow plasma cells
3.Absence of end organ damage
Smoldering multiple myeloma (also referred to asymptomatic multiple myeloma)
Both criteria must be met:*
1.serum M protein (IgG or IgA) ≥3 g/dL) and/or
2.the presence of 10% or more plasma cells in the bone marrow.
3.no evidence of related organ or tissue impairment (ROTI) or CRAB symptoms
Fulfilment of three criteria is required for a diagnosis of symptomatic myeloma:
The identification of an M protein in serum and/or urine (no specific level is required for a
diagnosis, although 60% of patients have a serum M protein >30g/L (Kyle 2003A)).
Clonal bone marrow plasma cells ≥10%
Evidence of end-organ damage which can be attributed to the underlying plasma cell
proliferation, specifically:
1.Hypercalcemia: serum calcium ≥11.5 mg/dL
2.Renal insufficiency: serum creatinine >2 mg/dL
3.Anaemia: normochromic, normocytic with haemoglobin >2 g/dL below the lower limit of
normal or <10 g/dL
4.Bone lesions: lytic lesions, severe osteopenia or pathologic fractures
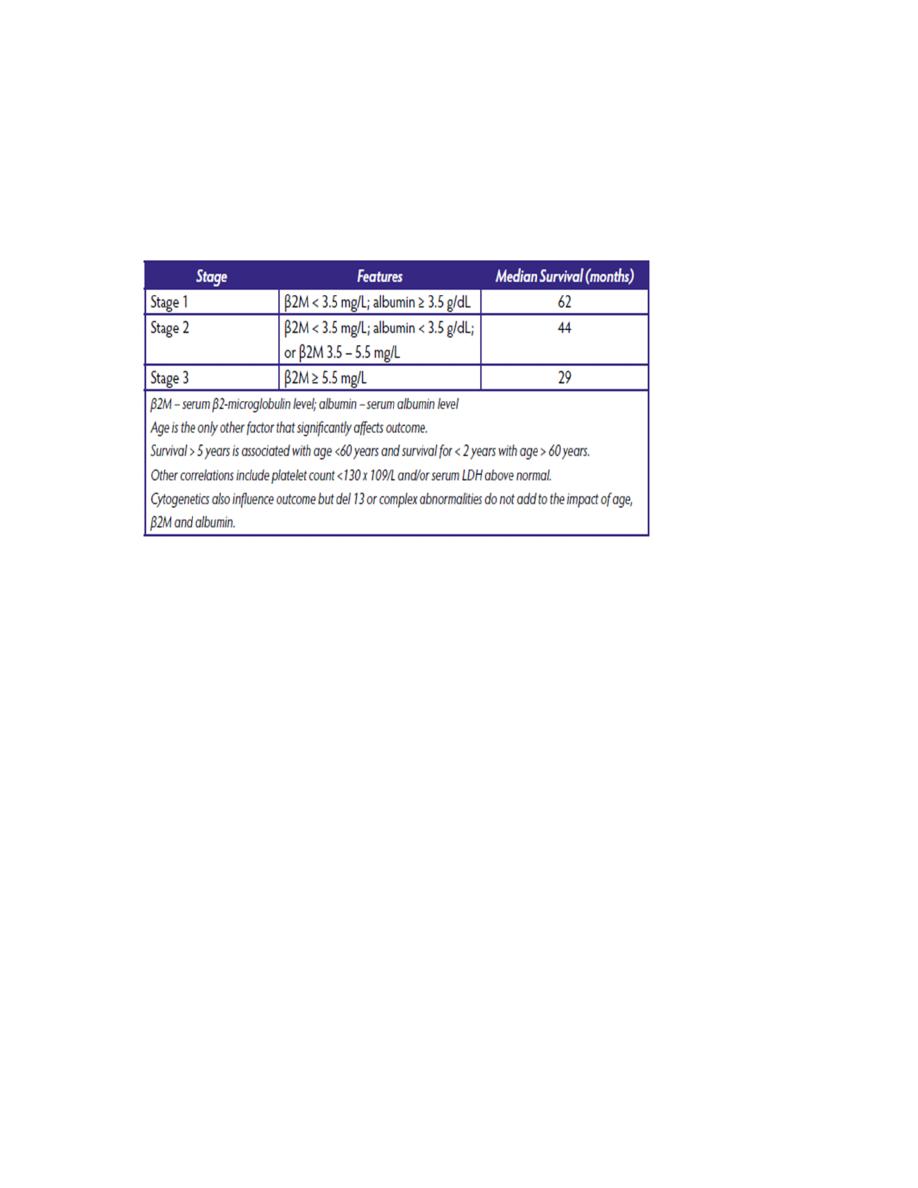
Staging system
1.Durie–Salmon staging system
2.International staging system
Complications of MM
The course of myeloma is often accompanied by clinical complications including:
1.Renal impairment
2.Haematological complications
3.Infection
4.Bone disease
5.Pain
6.Hypercalcaemia
7.Neurological complications
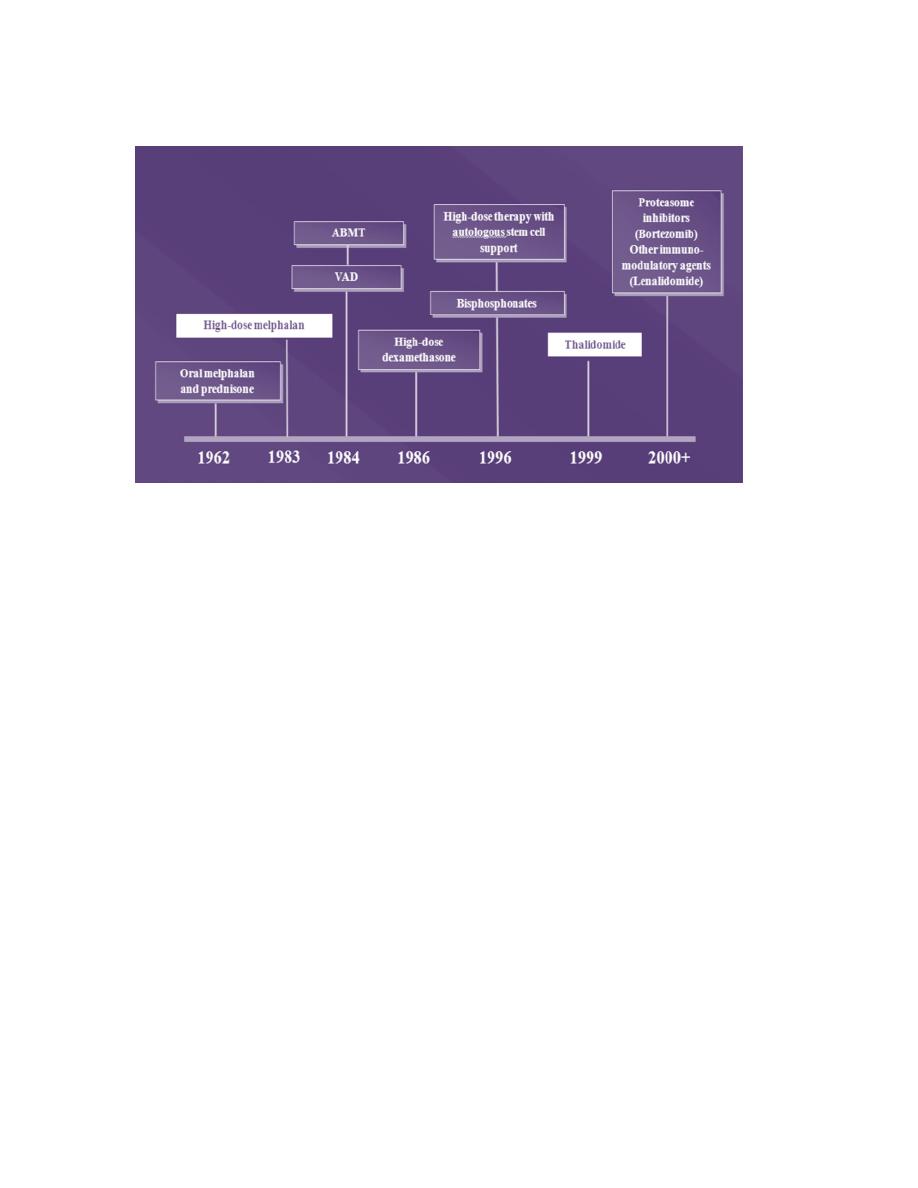
Treatment
The current treatment for eligible transplant patients consists of Bortizomib + thalidomide+
Dexamethasone or Bortizomib + lenalidomide+ Dexamethasone
For not eligible transplant pt Bortizomib + melphalan+ Dexamethasone
