Anesthesia
Bydr .abeer mansour
Definition of Anesthesia: is a reversible state of central nervous system (CNS)depression, resulting in loss of response to and perception of external stimuli.
or state of being unaware and unresponsive to painful stimuli
Concomitant use of drugs
Multiple adjunct agents: surgical patients receive oneor more of the following preanesthetic medications:
H2 blockers,
such as famotidine or ranitidine to reduce gastric acidity; benzodiazepines,
such as midazolam or diazepam to allay anxiety and facilitate
amnesia;
opioids such as fentanyl for analgesia;
antihistamines such
as diphenhydramine
for prevention of allergic reactions;
antiemetics
such as ondansetron to prevent nausea and the possible aspiration
of stomach contents;
and/or anticholinergics such as glycopyrrolate
to prevent bradycardia and secretion of fluids into the respiratory
tract .These agents facilitate smooth induction of anesthesia
and, when administered concurrently, also lower the dose of
anesthetic required to maintain the desired level of surgical anesthesia.
However, such coadministration can also enhance undesirable
anesthetic effects (for example, hypoventilation), and may produce
negative effects that are not observed when each drug is given
individually
STAGES AND DEPTH OF ANESTHESIA
General anesthesia can be divided into three stages:
induction, maintenance, and recovery.Induction is defined as the period of time from the
onset of administration of the potent anesthetic to the development of effective surgical anesthesia in the patient.
Maintenance provides a sustained surgical anesthesia.
Recovery is the time from discontinuation ofadministration of anesthesia until consciousness and protective physiologic reflexes are regained. .
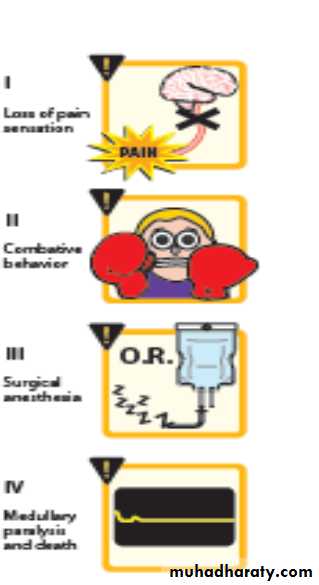
1. Stage I—Analgesia: Loss of pain sensation results from interference with sensory transmission in the spinothalamic tract. The patient progresses from conscious and conversational to drowsy. Amnesia and reduced awareness of pain occur as Stage II is approached.
2. Stage II—Excitement: The patient experiences delirium and possibly combative behavior. There is a rise and irregularity in blood pressure and respiration as well as a risk of laryngospasm. To shorten or eliminate this stage of anesthesia, a rapid acting agent, such as propofol, is given intravenously before inhalation anesthesia is administered.
3. Stage III—Surgical anesthesia: There is gradual loss of muscle tone and reflexes as the CNS is further depressed. Regular respiration and relaxation of skeletal muscles with eventual loss of spontaneous movement occur in this stage. This is the ideal stage of anesthesia
for surgery. Continuous careful monitoring is required to prevent
undesired progression into Stage IV.
4. Stage IV—Medullary paralysis: Severe depression of the respiratoryand vasomotor centers occur during this stage. Death can rapidly ensue unless measures are taken to maintain circulation and
respiration
Depth of anesthesia
Types of anesthetics
I. Inhalation anesthetics
II. Intravenous anestheticsIII. Local anesthetics
Inhalation anesthetics
Mechanisms of action :Activate K+ channels
Block Na+ channels Action
Disrupt membrane lipids
In general, all general anesthetics increase the cellular threshold for firing, thus decreasing neuronal activity.
I. Inhalation anesthetics
Nitrous OxideRapid onset
Good analgesia
Used for short procedures and in combination with other anesthetics
Supplied in blue cylinders
Halothane (Fluothane)
Volatile liquid
Narrow margin of safety
Less analgesia and muscle relaxation
Hepatotoxic
Reduced cardiac output leads to decrease in mean arterial pressure
Increased sensitization of myocardium to catecholamines
Enflurane (Ethrane)
Similar to Halothane
Less toxicities
Isoflurane (Forane)
Volatile liquid
Decrease mean arterial pressure resulting from a decrease in systemic vascular resistance
Inhalation anesthetics(Pharmacokinetics)
The concentration of a gas in a mixture of gases is proportional to the partial pressure
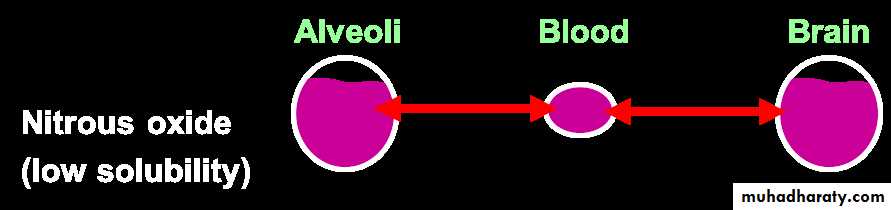
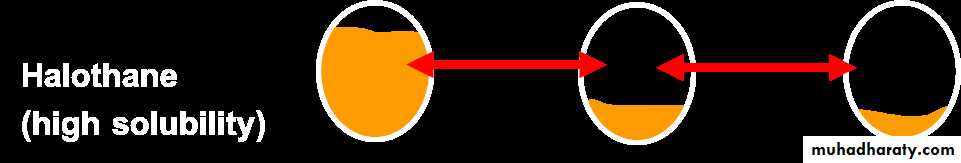
Inverse relationship between blood: gas solubility and rate of induction
Side Effects
Reduce metabolic rate of the brainDecrease cerebral vascular resistance thus increasing cerebral blood flow = increase in intracranial pressure
Malignant Hyperthermia
Rare, genetically susceptibleTachycardia, hypertension, hyperkalemia, muscle rigidity, and hyperthermia
Due to massive release of Ca++
Treat with dantrolene (Dantrium), lower elevated temperature, and restore electrolyte imbalance
Inhalation anesthetics
II. Intravenous anesthetics
Ketamine (Ketaject, Ketalar)Block glutamate receptors
Dissociative anesthesia:
Catatonia, analgesia, and amnesia without loss of consciousness
disorientation, sensory and perceptual illusions, vivid dreams
Cardiac stimulant
Propofol :works by increasing GABA-mediated inhibitory tone in the CNS. Propofol decreases the rate of dissociation of the GABA from the receptor, thereby increasing the duration of the GABA-activated opening of the chloride channel with resulting hyperpolarization of cell membranes. At supra clinical concentrations, it may directly activate the receptor’s chloride channel.
Rapid onset and recovery
Mild hypotension
Antiemetic activity
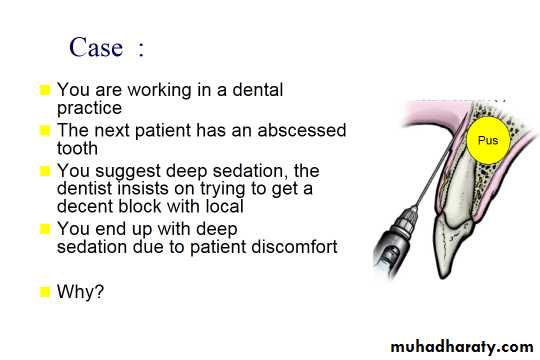
Local anesthetics
Blockade of sensory transmission to brain from a localized area
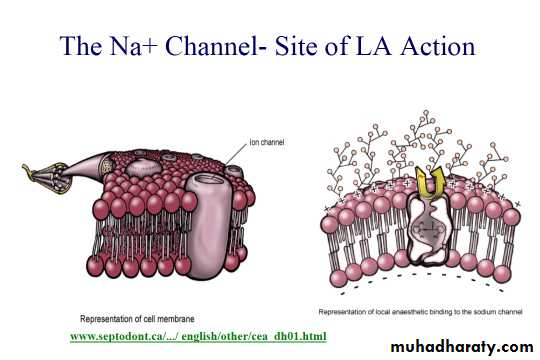
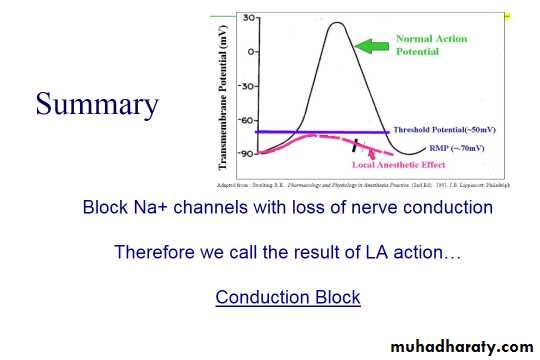
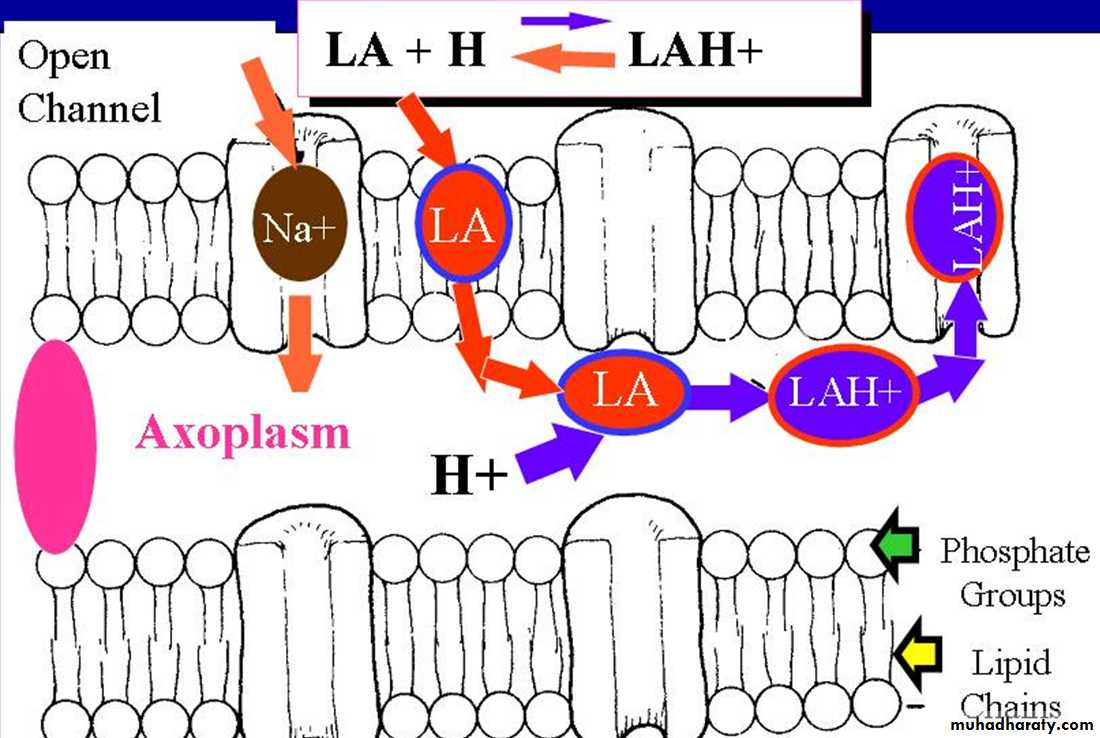
Blockade of voltage-sensitive Na+ channels
Use-dependent block
Administer to site of action
Decrease spread and metabolism by co-administering with adrenergic receptor agonist (exception….cocaine) local anesthetic is a drug that causes reversible local anesthesia and a loss of nociception. When it is used on specific nerve pathways (nerve block),
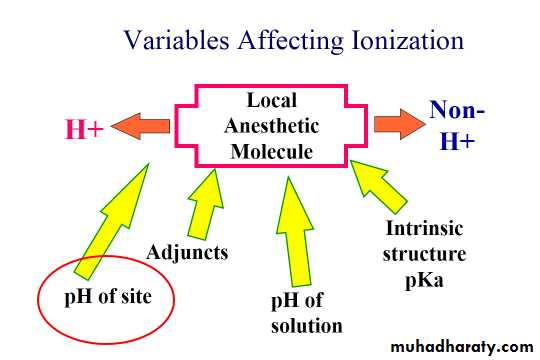
Local anesthetics
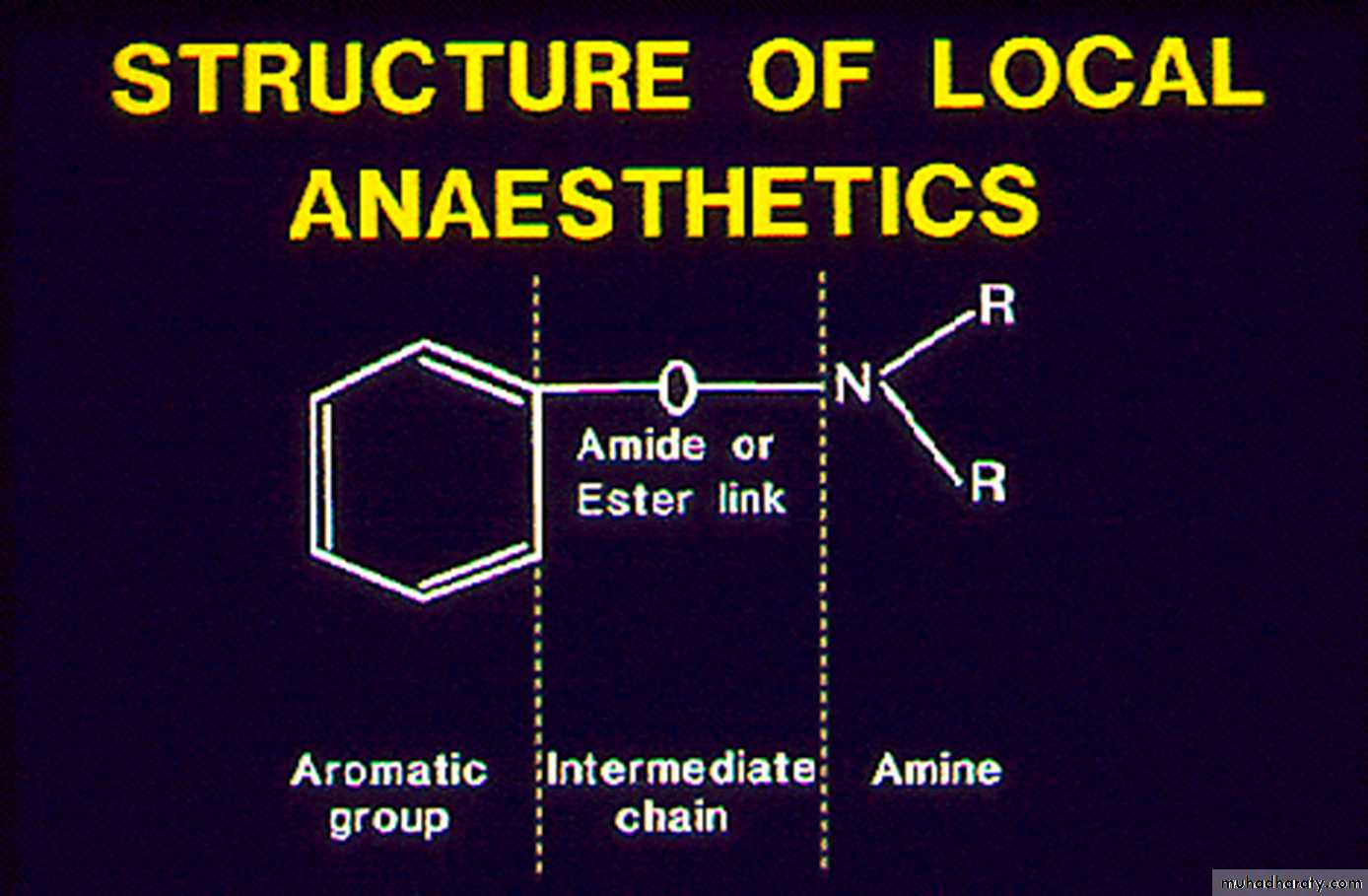
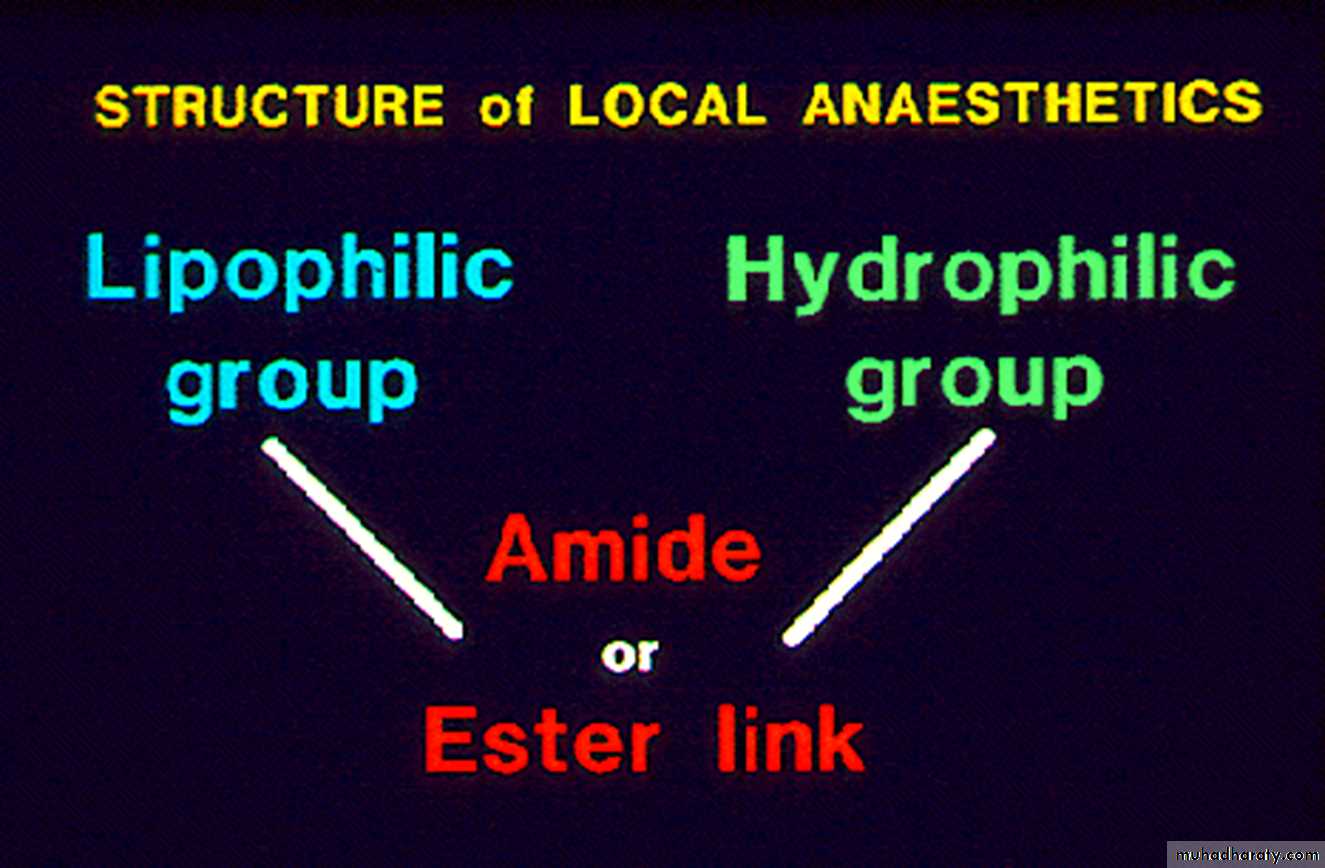
Local anesthetics - esters or amides
a lipophilic aromatic groupto a hydrophilic, ionizable amine.
Most are weak bases
Mechanism of action
Local anesthesia
The most widely usedof the local anesthetic compounds are bupivacaine
lidocaine mepivacaine procaine
ropivacaine
and tetracaine .
Of these,
lidocaineis probably the most commonly used.
Bupivacaine is noted for its
cardiotoxicity.
Mepivacaine should not be used in obstetric anesthesia due
to its increased toxicity to the neonate.
Add to LA vasoconstrictors
Vasoconstrictors
Epinephrine/Phenylephrine/ Levonordefrin
Prolong duration
Minimize effect of LA vasodilatation
toxicity
intensity of block
bleeding
Practical procedure
New Zealand white rabbit , clinically healthy, Were used, the animal study protocol was approved by the ethics committee for animalexperiments in the faculty of dentistry, Mosul University.
The animals were housed in wire mesh cages with standered condition food and water were provided at libitum,
Rabbits were anesthetized with injection of 50mg/kg ketamine hydrochloride (Ketamine, Hameln, Germany)and
xylazine 5 mg /kg (Xyla,Interchemie, Holland) respectively, and atropine sulfate injection (50) microgram / kg intra
muscularly in femur was routinely asepsis and montair the stages of anesthesia