The Respiratory System د.رند عبداللطيف
Lecture 3
1
Paranasal sinuses:
Are closed cavities in the frontal, maxillary, ethmoid & sphenoid bones. They
are lined with thin respiratory epithelium that contains few goblet cells. Their
lamina propria contains only few small serous and mucous glands. Those sinuses
communicate with the nasal cavity through small openings & the mucous
produced in the sinuses is drained into the nasal cavity by the action of the ciliated
epithelial cells, these sinuses help to increase the surface area for moistening &
warming the inhaled air, also the sinus cavities play a role in the nature of the
sounds produced. Sinusitis is an inflammatory process in the sinuses that may
persist for long period occur due to obstruction of the sinus openings.
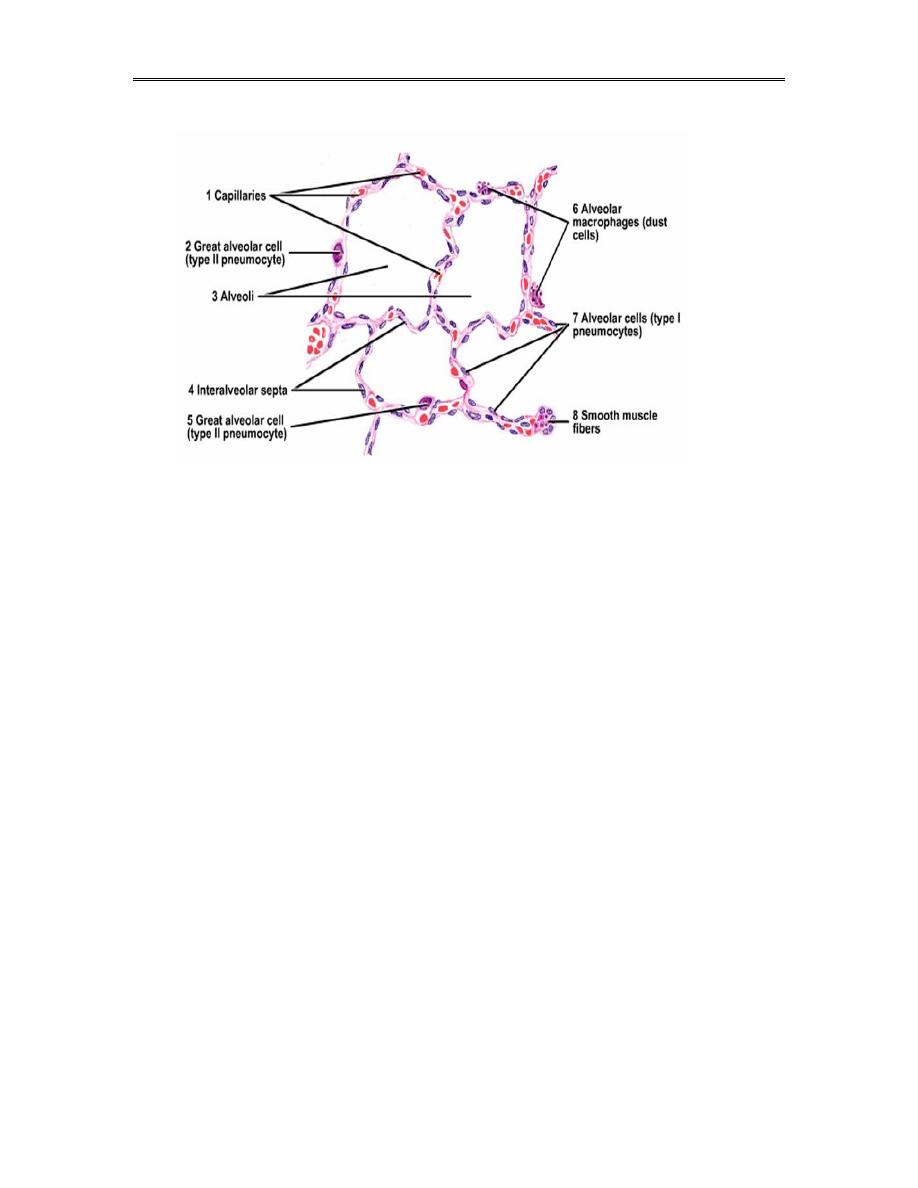
Alveoli
Are sac like structures (about 200µm in diameter), around 350 million
alveoli are present in each lung. They are the terminal portion of the
bronchial tree & are responsible for the spongy structure of the lungs, within
these alveoli O2 & CO2 will be exchanged between the blood & the air &
the structure of the alveolar wall will enhance this exchange greatly.
The Respiratory System د.رند عبداللطيف
Lecture 3
2
Generally the alveolar wall lie between two adjacent alveoli called
interalveolar septum, this septum consist of two thin squamous epithelial
layers between which lie capillaries, fibroblasts, elastic & reticular fibers &
also macrophages, these structures lie within a connective tissue stroma
called “interstitium” which contains the most vascular capillary network in
the body.
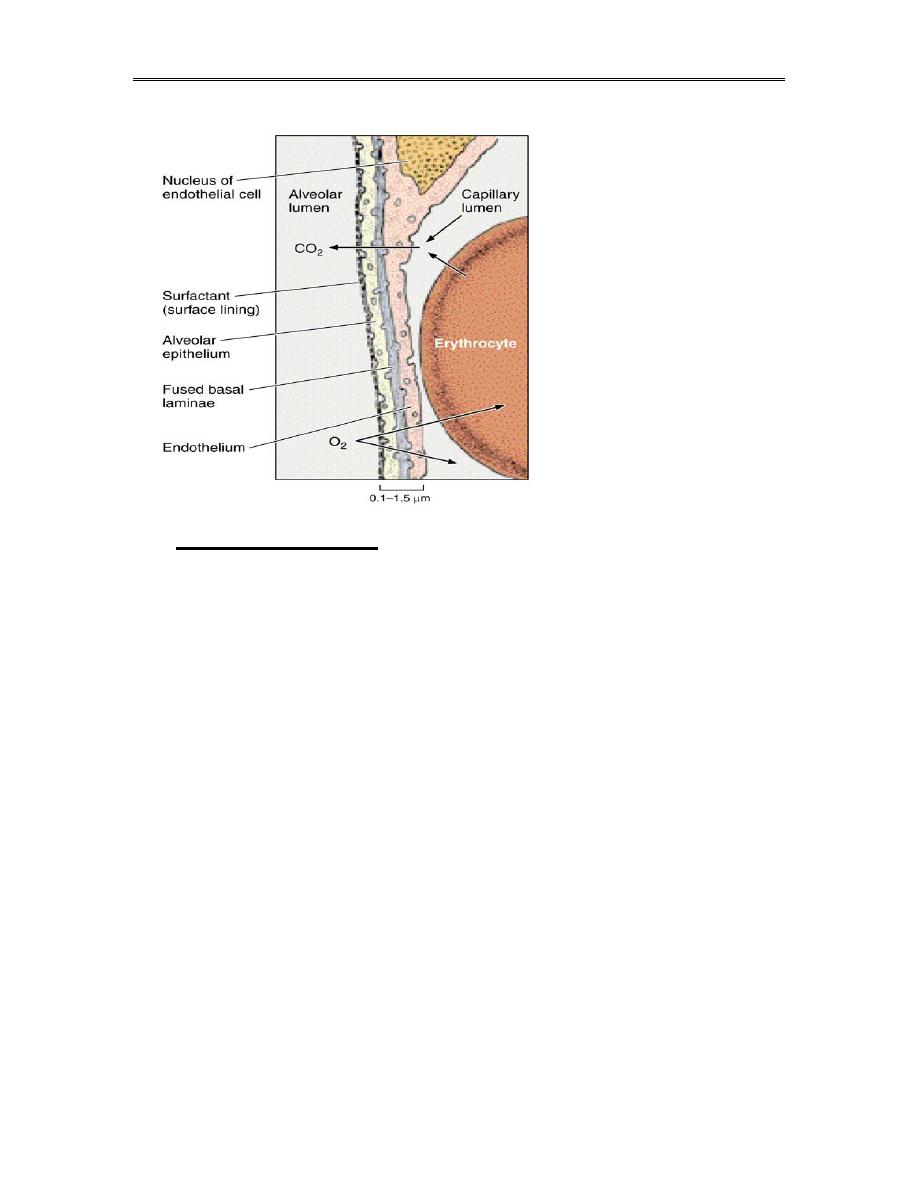
Air in the alveoli is separated from blood in the capillaries by three
components referred to as the blood – air barriers, the total thickness of
this barrier varies from (0.1-1.5) µm. & these are:
cells of the alveolar wall (type I & type II squamous alveolar cells).
basement membrane of the alveolar cells.
endothelial cells of the pulmonary capillaries.
The Respiratory System د.رند عبداللطيف
Lecture 3
3
Inter-alveolar septum:
The interalveolar septum is composed of 5 main cell types:
a) capillary endothelial cells (30%).
b) type I squamous alveolar cells (8 %).
c) type II septal (great alveolar) cells (16 %).
d) alveolar macrophages (10 %).
e) interstitial cells including fibroblasts & mast cells (36%).
within the interalveolar septum the anastomosing pulmonary capillaries &
different types of cells are supported by a meshwork of reticular and elastic
fibers that provide structural support to the alveoli.
The Respiratory System د.رند عبداللطيف
Lecture 3
4
1. Capillary endothelial cells:
These are extremely thin cells, the clustering of the nuclei & other
cellular organelles allows the remaining areas of the cell to become
extremely thin thus increasing the efficacy of gaseous exchange.
The capillary endothelium is continuous not fenestrated type
the most prominent feature in these cells is the numerous
pinocytotic vesicles.
2. Type I pneumocytes:(squamous alveolar cells)
These cells will make up to 97% of the alveolar surface area &
they are also extremely thin cells, flattened nucleus.
all the cellular organelles are grouped around the nucleus reducing
the thickness of the rest of the cell, thus decreasing the thickness of

The Respiratory System د.رند عبداللطيف
Lecture 3
5
the blood –air barrier by leaving large areas of the cytoplasm free
of organelles.
The main function of these cells is to provide a barrier of minimal
thickness through which gaseous exchange take place, the
cytoplasm of these cells contains many pinocytotic vesicles which
may play a role in the turn over of surfactant & in the removal of
small particles on the surface of the alveoli.
All type I pneumocyte cells have occluding junctions that prevent
the leakage of tissue fluid into the alveolar air space
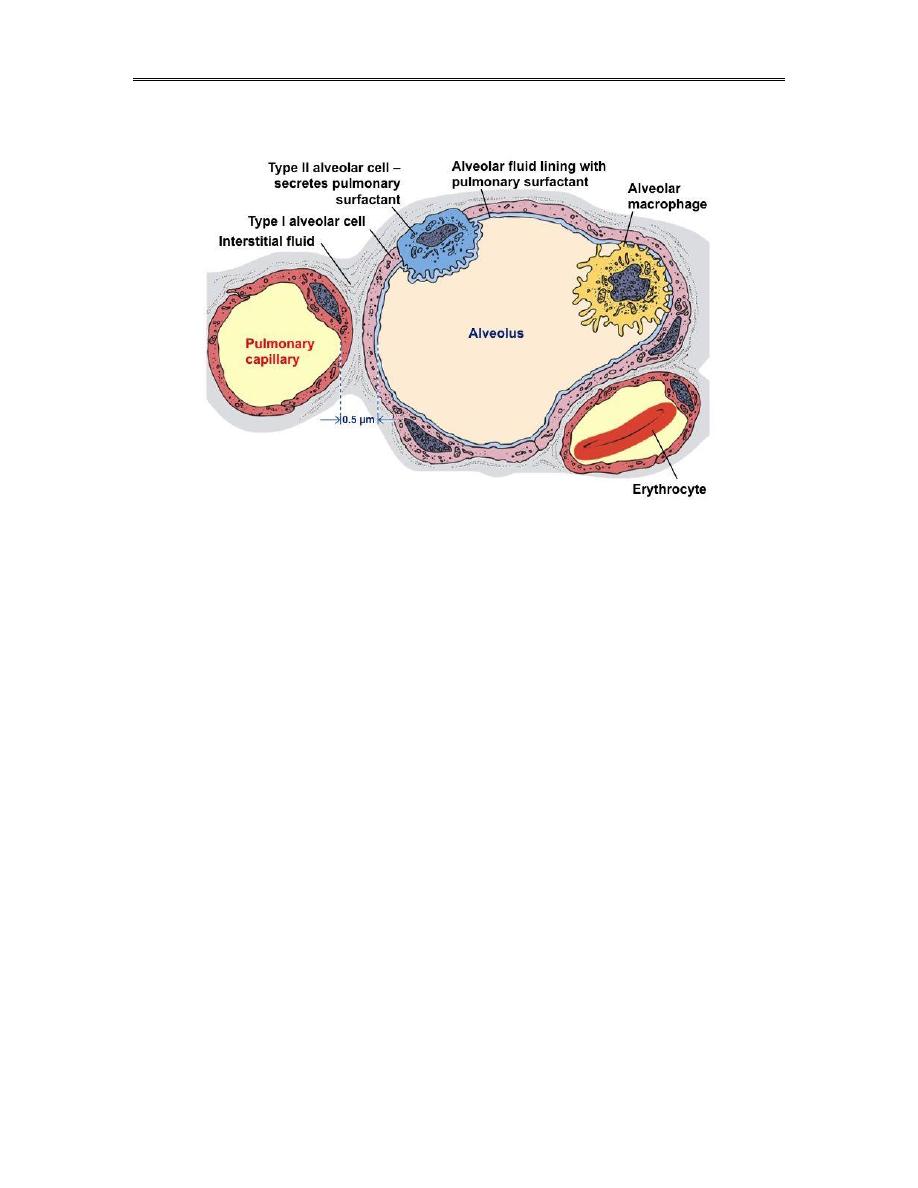
3. Type II pneumocytes: (great alveolar, septal cells)
They are found in between type I pneumocytes, they are cuboidal
in shape with large rounded nucleus and are usually found singly
scattered or in small groups of 2-3 cells along the alveolar wall,
they are found mainly where the alveolar walls unite & form an
angles.
These cells divide by mitosis to form another type II pneumocytes
and also to form type I cells but the main function of type II
pneumocytes is the production of surfactant which is a substance
released from the cell produce reduction of the surface tension
thus preventing collapse of the alveoli during expiration &
facilitate expansion during inspiration.The reduction in the surface
tension means that less inspiratory force is needed to inflate the
alveoli at the same time alveoli without surfactant would tend to
collapse during expiration.

The Respiratory System د.رند عبداللطيف
Lecture 3
6
Type II pneumocytes are first detectable in the alveolar wall at
about 28 week gestation after this time the premature babies are
capable of respiratory survival, however between 28 week
gestation and term the amount of surfactant may be inadequate
leading to alveolar collapse and type I pneumocyte damage and in
this case some artificial respiratory assistance may be needed and
the condition is known as “respiratory distress syndrome”.
Recently surfactant has also been suggested to have bactericidal
effect aiding in the removal of potentially dangerous bacteria that
reach the alveoli.
4. Alveolar macrophages:
These cells are found within the interalveolar septum and are often seen
on the surface of the alveoli. These cells also called Dust cells they often
contain phagocytosed materials, particularly inhaled carbon particles, they
are also important defense mechanism against inhaled bacteria. after
phagocytosis these cells will enter the respiratory bronchioles or terminal
bronchioles where they are either pass into the lymphatic vessels and then
removed to the regional lymph node or they adhere to the ciliated mucous
coated epithelium which will eventually carried up to the trachea & cleared
by coughing. The phagocytosed debris within these cells was most likely
passed from the alveolar lumen to the interstitium by the pinocytotic activity
of type I pneumocytes.
5. Interstitial cells:
The interstitium of the interalveolar septum also contains fibroblasts, mast
cells & other connective tissue cells.The fibroblasts will synthesize collagen

The Respiratory System د.رند عبداللطيف
Lecture 3
7
& elastic fibers which are important factors in giving resilience & elasticity
to the lung.
Alveolar pores:
The interalveolar septum contain many pores (10-15 µm. in diameter), they
connect the neighboring alveoli so will equalize air pressure in the alveoli
and also promote the collateral circulation of air when a bronchiole is
obstructed.
Defense mechanisms:
the respiratory system has a large surface area that is exposed to both
blood and the external environment so it is very susceptible to
invasion by bacteria and other non-infective agents.
particles larger then (10 µm.) are retained in the nasal passages,
particles of (2-10 µm.) are trapped by the mucous coated ciliated
epithelium and the cough reflex can eliminate these particles by
expectoration or swallowing. smaller particles are removed by
alveolar macrophages.
in addition to the above mechanisms we have many lymphoid tissues
containing both B & T lymphocytes are found in association with the
bronchi, this important part of the immune system is called BALT
(bronchus- associated lymphatic tissue).
