د.ساجدة فسلجة 21\11\2017
عدد الاوراق ( 28 ) م\2\موصلLEC: 1+2+3+4+5+6+7+8+9+10+11
PHYSIOLOGY OF THE ENDOCRINE SYSTEM
You should now be familiar with:
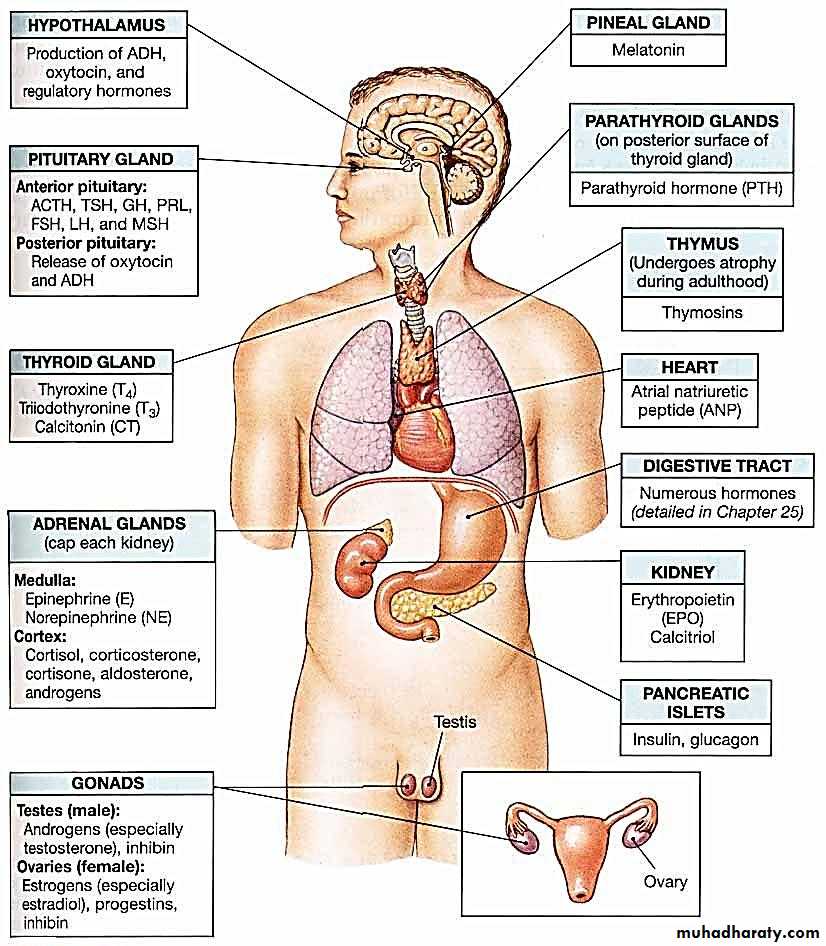
The major chemical classes and general mechanisms of hormones.
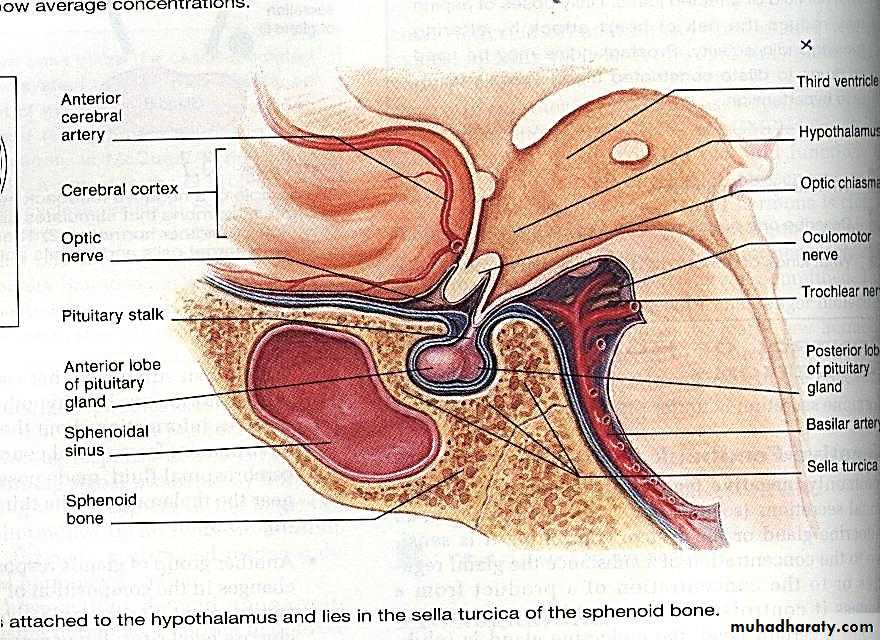
The location and structure of the pituitary gland, and its structural and functional relationships with the hypothalamus.
The location and structure of each of the endocrine glands.
The hormones produced by each of the endocrine glands, and the functions of those hormones.
How hormones interact to produce coordinated physiological responses.
What is endocrinology?
Endocrinology =Intercellular Chemical Communication
Endocrinology is about communication systems & information transfer.
What are endocrine systems for?
Endocrine FunctionsGrowth and development
Homeostasis (the internal balance of body systems)
Metabolism (body energy levels)
Reproduction
Response to stimuli (stress and/or injury)
Endocrinology
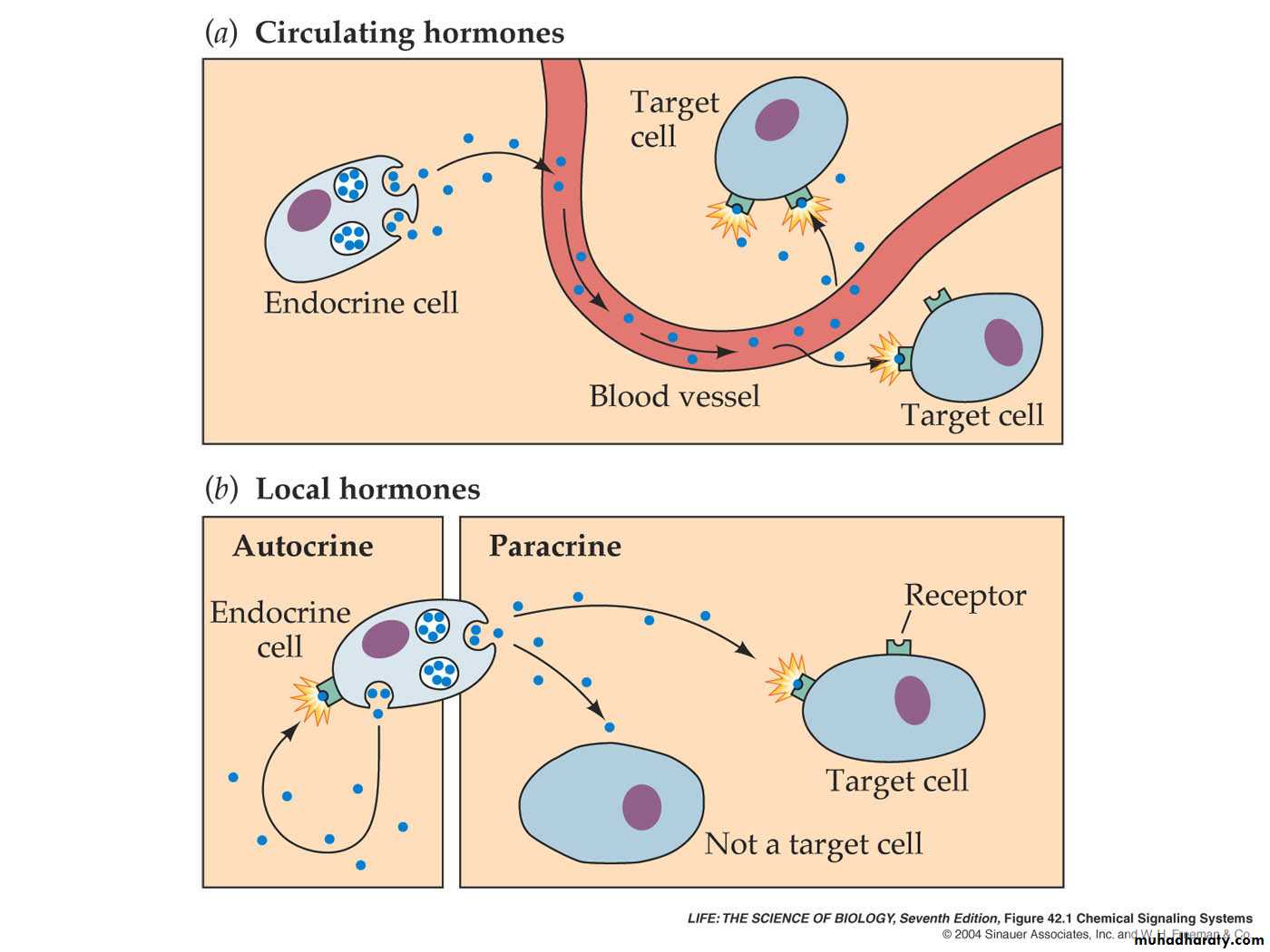
Endocrine: glands or specialized cells release into the circulating blood hormones that influence the function of cells at another location in the body.
Paracrine: in which cells secrete substances that diffuse into the extra cellular fluid & affect neighboring cells.
Autocrine: in which a cell secrets substances that affect the function of the same cell by binding to the same surface receptor.
There are three classes of hormones:
Proteins& polypeptides including hormones secreted by the anterior & posterior piuitary gland,insulin&glucagon,the parathyroid hormone.
Steroids as cortisol & aldosterone,estrogen, progesterone and testosterone.
Derivatives of the amino acid tyrosine as thyroxine& triiodothyronine, epinephrine&norepinephrine.
Transport of hormones in the blood
Water-soluble hormones ( peptides & catecholamines ) are dissolved in the plasma & transported from their sites of synthesis to target tissues where they diffuse out of the capillaries into the interstitial fluid & then to target cells.Steroids & thyroid hormones , circulate in the blood bound to plasma proteins. Usually
less than 10 per cent of steroid or thyroid hormones in the plasma exist free in solution. For example, more than 99 per cent of the thyroxine in the blood is bound to plasma proteins. These can not diffuse easily across the capillaries ,so they are inactive until they dissociate from plasma proteins .The relatively large amounts of hormones bound toproteins serve as reservoirs, replenishing the concentration of free hormones when they are bound to target receptors or lost from the circulation., binding of hormones to plasma proteins greatly slows their clearance from the plasma.
Clearance of hormones from blood
Two factors can increase or decrease the concentration of a hormone in blood. One of these is the rate of hormone secretion in blood. The second is the rate of removal of the hormone in blood. which is called the (metabolic clearance rate= rate of disappearance of hormone from the plasma/ concentration of hormone in each milliliter of plasma.Hormones are cleared from the plasma in several ways, including:
Metabolic destruction by the tissues.
Binding with the tissues.
Excretion by the liver .
Excretion by the kidneys..
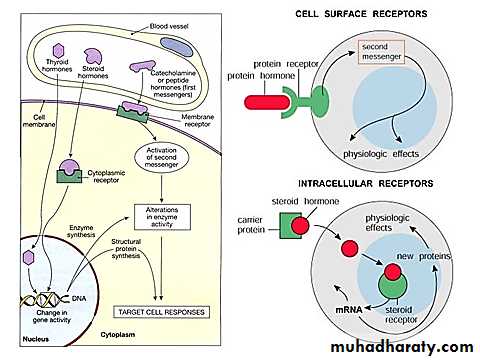
Mechanism of action of hormones
The first step of hormone action is to bind to specific receptors at the target cells.
Receptor located :
In or on the surface of cell membrane as for protein ,peptide &catecholamine hormones.
In the cell cytoplasm as for steroid hormones.
In the cell nucleus as for thyroid hormones.
After binding with the receptor some change the membrane permeability for ions , some activate intracellular enzymes ,some activate gens.
What is a hormone receptor?
Hormone Receptors are cellular proteins that bind with high affinity to hormones & are altered in shape & function by binding; they exist in limited numbers.
Binding to hormone is reversible.
Peptide Hormones
Peptide hormones do not enter the cell directly. These hormones bind to receptor proteins in the cell membrane.When the hormone binds with the receptor protein, a secondary messenger molecule initiates the cell response.
Because peptide hormones are water soluble, they often produce fast responses.
Steroid Hormones
Steroid hormones enter through the cell membrane and bind to receptors inside of the target cell.These hormones may directly stimulate transcription of genes to make certain proteins.
Because steroids work by triggering gene activity, the response is slower than peptide hormones.
Hypothalamus
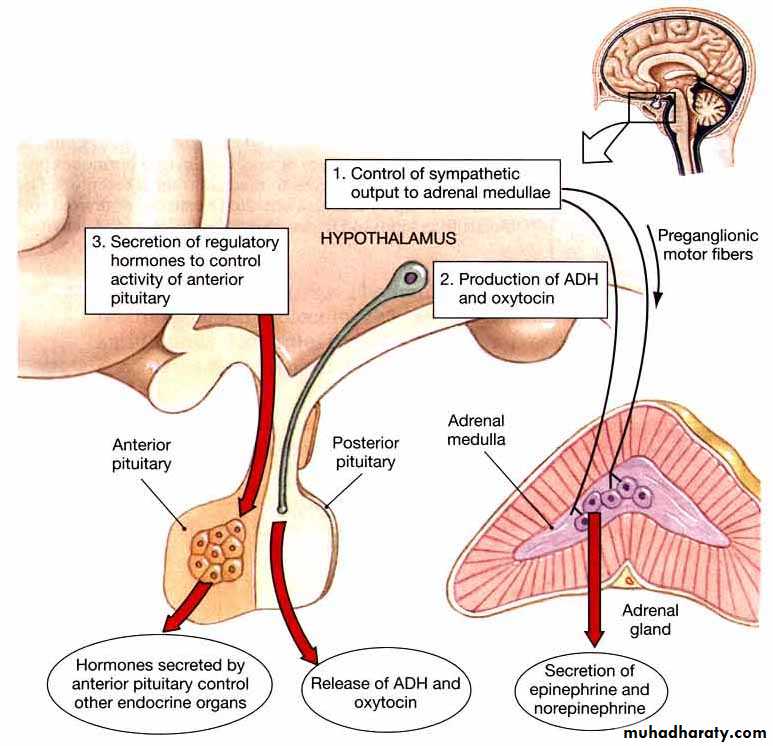
The portion of the brain that maintains the body’s internal balance (homeostasis).The hypothalamus is the link between the endocrine and nervous systems.
The hypothalamus produces releasing and inhibiting hormones, which stop and start the production of other hormones throughout the body.
The hypothalamus is involved in many functions of the autonomic nervous system, as it receives information from nearly all parts of the nervous system
Anatomy of the Hypothalamus
The hypothalamus is located below the thalamus (a part of the brain that relays sensory information) and above the pituitary gland and brain stem. It is about the size of an almond.
Hormones of the Hypothalamus
The hypothalamus is highly involved in pituitary gland function. When it receives a signal from the nervous system, the hypothalamus secretes substances known as neurohormones that release and inhibit the secretion of pituitary hormones.Primary hormones secreted by the hypothalamus include:
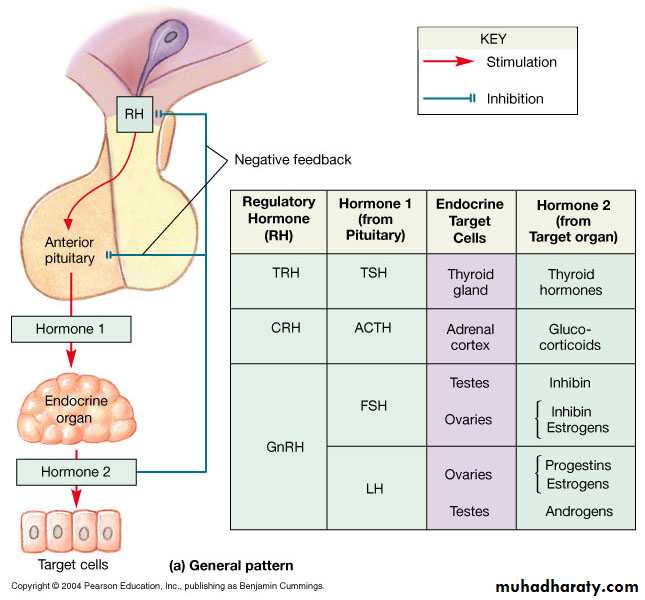
Anti-diuretic hormone (ADH): This hormone increases water absorption into the blood by the kidneys.Corticotropin-releasing hormone (CRH): CRH sends a message to the anterior pituitary gland to stimulate the adrenal glands to release corticosteroids, which help regulate metabolism and immune response.
Gonadotropin-releasing hormone (GnRH): GnRH stimulates the anterior pituitary to release follicle stimulating hormone (FSH) and luteinizing hormone (LH), which work together to ensure normal functioning of the ovaries and testes.
Hormones of the Hypothalamus
Growth hormone-releasing hormone (GHRH) or growth hormone-inhibiting hormone (GHIH) (also known as somatostain): GHRH prompts the anterior pituitary to release growth hormone (GH); GHIH has the opposite effect. In children, GH is essential to maintaining a healthy body composition. In adults, it aids healthy bone and muscle mass and affects fat distribution.Oxytocin: Oxytocin is involved in a variety of processes, such as orgasm, and the release of breast milk.
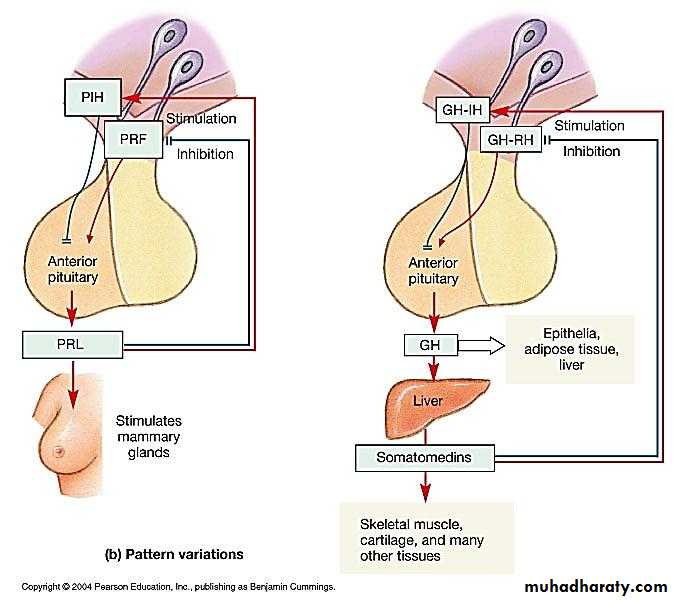
Prolactin-releasing hormone (PRH) or prolactin-inhibiting hormone (PIH) (also known as dopamine): PRH prompts the anterior pituitary to stimulate breast milk production through the production of prolactin. Conversely, PIH inhibits prolactin, and thereby, milk production. Thyrotropin releasing hormone (TRH): TRH triggers the release of thyroid stimulating hormone (TSH), which stimulates release of thyroid hormones, which regulate metabolism, energy, and growth and development.
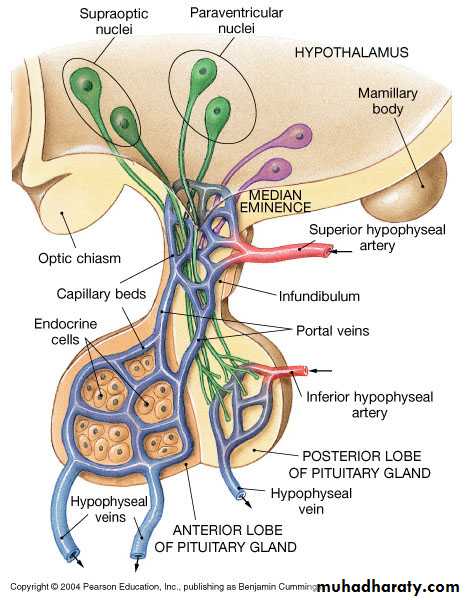
All or most of hypothalamic hormones are secreted at nerve endings in the median eminence before being transported to the anterior pituitary gland.
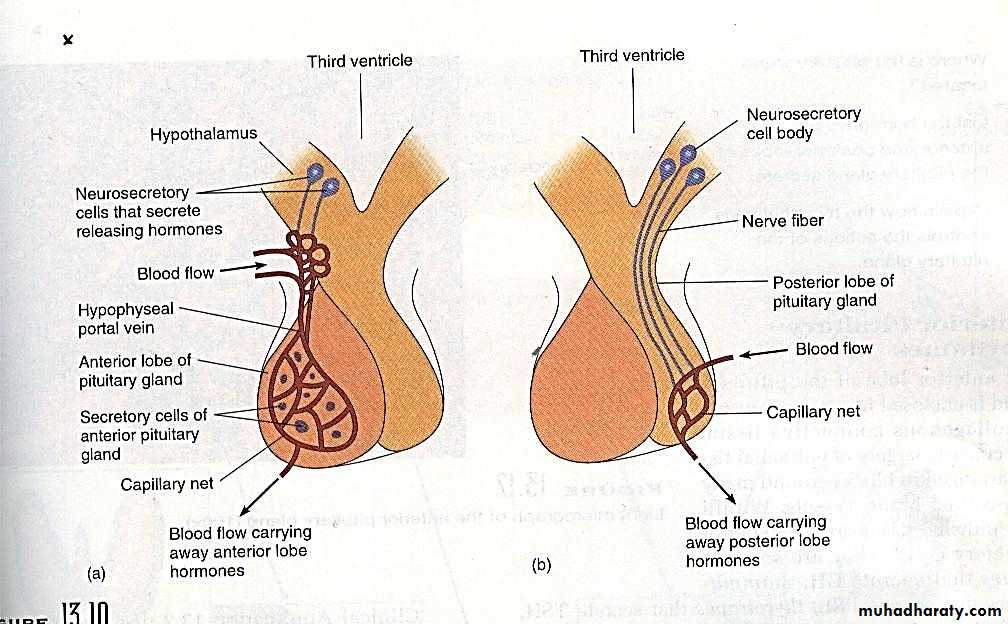
Hypophyseal portal system
All blood entering the portal system will reach the intended target cells before returning to the general circulationFigure 18.8 Feedback control of Endocrine Secretion
Figure 18.8 Feedback control of Endocrine Secretion
The pituitary gland
The anterior pituitary secrets six hormones : growth hormone (GH), adrenocorticotropin (ACTH) , thyroid stimulating hormone (TSH) , luteinizing hormone (LH) , follicle stimulating hormone (FSH) , prolactin (PRL) ..
There are five cell types in the anterior pituitary:
Somatotropes---human growth hormone.
Corticotropes----ACTH.
Gonadotropes—FSH&LH.
Thyrotropes------TSH.
Lactotropes------PRL.
The Posterior Pituitary Gland
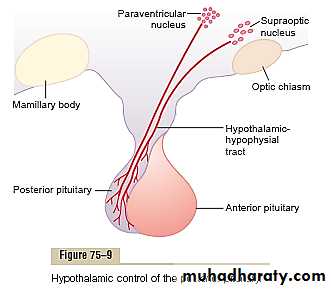
Its also called the neurohypophysis or pars nervosa, contains the axones of some hypothalamic neurons. Neurons within the supraoptic & paraventricular nuclei manufacture :
Antidiuretic hormone (ADH) also called vasopressin
- Oxytocin
The posterior pituitary is made up of the endings of the axons that arise from the cell bodies in the supraoptic & the paraventricular nuclei & pass to the posterior pituitary via the hypothalamo-hypophysial tract , the portal hypophysial vessels form a direct vascular link between the hypothalamus & the anterior pituitary.
The hormones of the posterior pituitary gland , oxytocin & vasopressin are nonapeptides synthesized in the cell bodies of the magnocellular neurons in the supraoptic & paraventricular nuclei & transported down the axons of these neurons to their endings in the posterior lobe, where they are secreted in response to the electrical activity in the endings.
Vasopressin secreting neurons are found in the suprachiasmatic nuclei , & vasopressin & oxytocin are also found in the endings of neurons that project from the paraventricular nuclei to the brain stem & the spinal cord . These neurons appears to be involved in the cardiovascular control.
Chemical structures ADH and oxytocin
Both oxytocin and ADH are polypeptides , each containing nine amino acids. These two hormones are almost identical except that in vasopressin, phenylalanine and arginine replace isolucine and leucine of the oxytocin molecule .Ejection of milk (function of oxytocin)
When baby suckles the breast , nerve signals transmitted to the spinal cord & then to the hypothalamus cause oxytocin secretion which result in contraction of myoepithelial cells surrounding the alveoli & ejection of milk . Generalized sympathetic stimulation inhibit oxytocin secretion & milk ejection .Other actions: oxytocin causes contraction of smooth muscle of the uterus. The sensitivity of uterine musculature to oxytocin is enhanced by estrogen & inhibited by progesterone , the inhibitory effect of progesterone is through direct effect on oxytocin receptors in the uterus . Oxytocin may also act on non- pregnant uterus to facilitate sperm transport .
Circulating oxytocin is increased at time of ejaculation in males & it is possible that this increase causes increased contraction of smooth muscle of the vas deferens , propelling the sperm toward the urethra.
.
Physiologic functions of ADH
ADH decrease the excretion of water by the kidneys.
1.In the absence of ADH , the collecting tubules and ducts become almost impermeable to water , which prevents significant reabsorption of water and therefore allows extreme loss of water into the urine and causes dilution of urine .
2.In the presence of ADH , the permeability of collecting ducts and tubules to water increases greatly and allows most of the water to be re absorbed as the tubular fluid passes through these ducts , thereby conserving water in the body and producing very concentrated urine. .
Regulation of ADH Production
1. Osmotic regulationSomewhere in or near the hypothalamus are modified neuron receptors called osmoreceptors . When the extracellular fluid becomes too concentrated , fluid is pulled by osmosis out of the osmoreceptor cell , decreasing its size and initiating nerve signals in the hypothalamus to cause ADH secretion . Conversely , when the extra cellular fluid becomes too dilute , water moves by osmosis in the opposite direction into the cell & this decreases signal for ADH secretion.
So concentrated body fluid stimulate the supraoptic nuclei , whereas dilute body fluids inhibit them .
Higher concentrations of ADH have a potent effect of vasoconstricting the arterioles throughout the body , therefore increasing the arterial pressure . For this reason it is also called vasopressin .
2. One of the stimuli for causing ADH secretion is decreased blood volume , this occurs especially when the blood volume decreases 15-25 % , the secretory rate then sometimes rises to as high as 50 times normal .
3. The atria especially the right atrium have stretch receptors that are excited by overfilling , they signals to the brain to inhibit ADH secretion .
4. Decreased stretch of baroreceptors of the carotid , aortic & pulmonary regions , increases ADH secretion .
Growth Hormone
also known as somatotropin (or as human growth hormone [hGH] in its human form), is a peptide hormone that stimulates growth, cell reproduction, and cell regeneration in humans and other animals. It is thus important in human development. Growth hormone is a 191-amino acid, single-chain polypeptide that is synthesized, stored, and secreted by HYPERLINK "https://en.wikipedia.org/wiki/Somatotropic_cell" somatotropic cells within the anterior pituitary gland.Growth Hormone: Physiologic Effects
Metabolic effects: (1) increased rate of protein synthesis in most cells of the body(2) increased mobilization of fatty acids from adipose tissue,
increased free fatty acids in blood, & increased use of fatty acids for energy.
(3) decreased rate of glucose utilization throughout the body.
Thus, in effect, growth hormone enhances body protein, uses up fat stores, and conserves carbohydrates.(stress hormone)
Promotes Growth
Increases cell number in organs
Skeletal growth
Cartilage formation
Collagen biosynthesis (epiphysal plates)
Muscle cell growth
Growth Hormone Action
Growth Hormone Action
GH may act directly on tissues, but much of its effect is mediated by stimulation of the liver and other tissues to produce and release insulin-like growth factors, primarily insulin-like growth factor 1 (IGF-1; formerly called somatomedin). The term insulin-like growth factor is derived from the ability of high concentrations of these factors to mimic the action of insulin, although their primary action is to stimulate growth. Serum IGF-1 concentrations increase progressively with age in children, with an accelerated increase at the time of the pubertal growth spurt. After puberty the concentrations of IGF-1 gradually decrease with age, as do GH.Regulation of GrowthHormone Secretion
The secretion of GH is not stable over time . Adolescents have the highest level of circulating GH , followed by children,& finally adults .levels decline in old age.Growth hormone is secreted in a pulsatile pattern, increasing & decreasing.
several factors related to a person’s state of nutrition or stress are known to stimulate secretion:
(1) starvation, especially with severe protein deficiency; (2) hypoglycemia or low concentration of fatty acids in the blood; (3) exercise; (4) excitement; and (5) trauma.
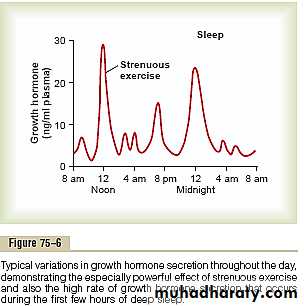
Growth hormone also characteristically increases during the first 2 hours of deep sleep, as shown in the figure.
Control of GrowthHormone Secretion
Growth hormone secretion is controlled by two factors secreted in the hypothalamus and then transported to the anterior pituitary gland through the hypothalamic hypophysial portal vesselsGrowth hormone–releasing hormone (GHRH)
2.growth hormone inhibitory hormone (also called somatostatin)
Most of the control of growth hormone secretion is probably mediated through GHRH rather than through the inhibitory hormone somatostatin.
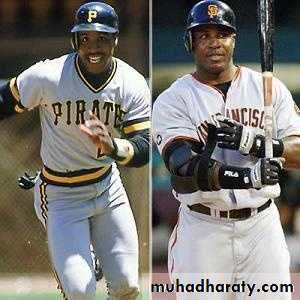
Abnormalities of GrowthHormone Secretion
Acromegaly Over-secretion of growth hormone during adulthood usually from tumorrefers to the enlargement of the distal parts of the body, including the hands, feet, chin, and nose. The enlargement is due to the overgrowth of cartilage, muscle, subcutaneous tissue, and skin. Thus, patients with acromegaly have a prominent jaw, a large nose, and large hands and feet, as well as enlargement of most other tissues, including the tongue, heart, liver, and kidneys.
Gigantism Over-secretion of growth hormone prior to puberty.
Excessive growth of long bones
Acromegaly
Over-secretion of growth hormone during adulthoodusually from tumor
Enlargement of the extremities and/or face
Treatment: drug therapy to inhibit GH release
Gigantism
Over-secretion of growth hormone prior to puberty.Excessive growth of long bones
Treatment: drug therapy to inhibit GH release
Dwarfism
Most instances of dwarfism result from generalized deficiency of anterior pituitarysecretion(panhypopituitarism)during childhood.A person with panhypopituitary dwarfism does notpass through puberty and never secretes sufficient quantities of gonadotropic hormones to develop adult sexual functions.
In one third of such dwarfs, however,
Only growth hormone is deficient; these persons do mature sexually and occasionally reproduce.
Prolactin
Prolactin (PRL) is a peptide hormone secreted by anterior pituitary and is critical for lactation and breast development in women.Prolactin is synthesized and secreted by lactotrophs of the anterior pituitary. Synthesis and secretion of pituitary PRL is under control of the hypothalamus via releasing and inhibitory hormones. Hypothalamic TRH acts as the releasing hormone whereas hypothalamic dopamine acts as an inhibitory hormone, although inhibition by dopamine is likely the dominant control mechanism. Additionally, prolactin secretion appears to be under negative feedback control as high levels of prolactin induce hypothalamic secretion of dopamine.
Prolactin is only found at significant levels in pregnant or lactating women. During pregnancy, the levels of PRL steadily increase, reaching a peak immediately before delivery. Following birth of the child, PRL levels decline to their low, pre-pregnancy levels; however, they then display rapid peaks whenever suckling at the nipple occurs.
Physiological Effects of Prolactin
- Breast Development: Together with estrogen and progesterone, prolactin induces proliferation and growth of mammary glands during puberty and again during pregnancy.
Lactation: Prolactin stimulates mammary glands to synthesize milk.
Inhibition of ovulation: Prolactin inhibits hypothalamic release of GnRH, resulting in decreased ovulation. This explains why breast-feeding tends to promote reversible infertility.
Prolactin deficiency results in defective lactation during pregnancy. Prolactin deficiency may arise within a context of generalized hypopituitarism especially when Sheehan Syndrome is the etiology
PHYSIOLOGY OF THE ENDOCRINE SYSTEM
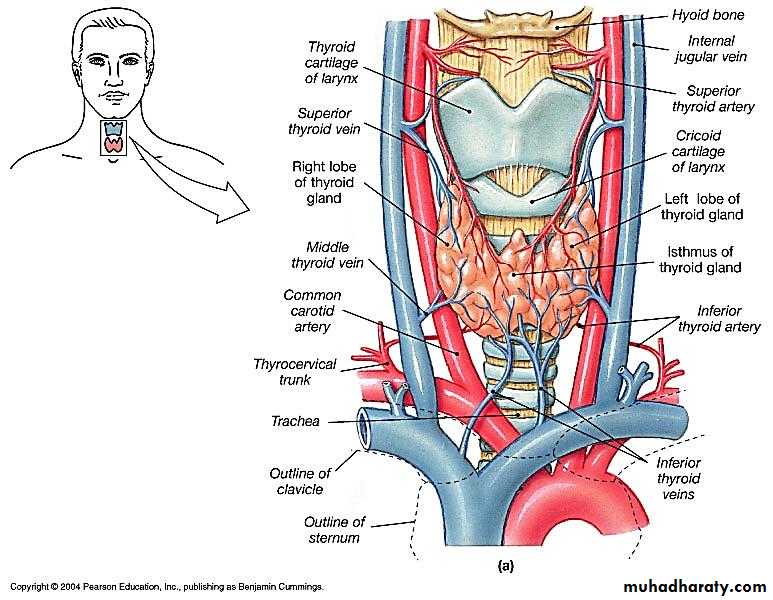
The Thyroid GlandLies near the thyroid cartilage of the larynx
Two lobes connected by an isthmus
The thyroid gland
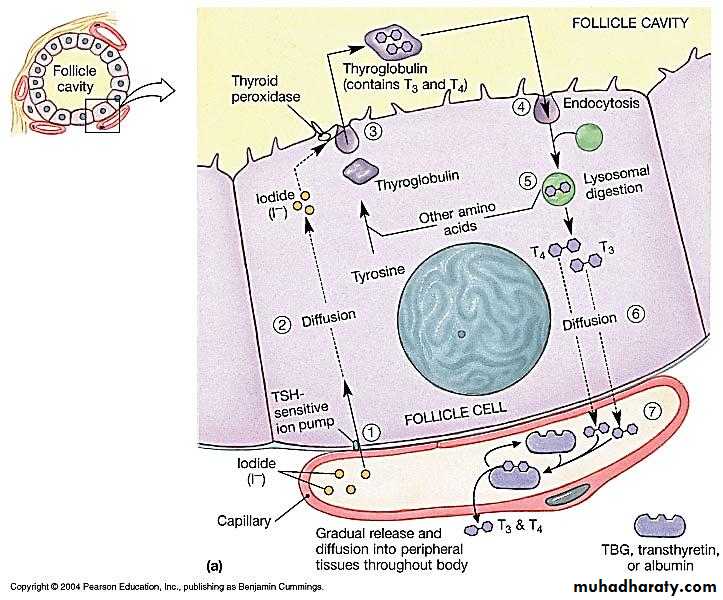
Formation & secretion of thyroid hormones :The main hormones secreted by the thyroid are thyroxine(T4) &triiodothronine(T3) T3 is also formed in the peripheral tissues by deiodination of T4.both hormones are iodine containing amino acids.T3 is more active than T4.
Iodied pump :
The first stage in the formation of thyroid hormones is transport of iodieds from the blood into the thyroid glandular cells & follicles this is called iodied trapping , in normal gland the iodied pump concentrates the iodied to about 30 times its concentration in blood. the rate of iodide trapping is influenced by several factors , the most important is the concentration of TSH.
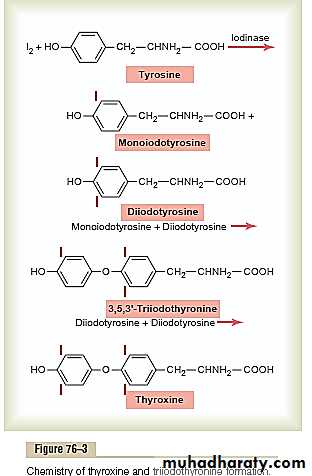
Thyroglobulin & chemistry of thyroxin & triiodothyronin formation
Thyroglobulin is a large glycoprotein molecule has a molecular weight of about 335,000.the molecule of thyroglobulin contains 70 tyrosine amino acids &they are the major substrates that combine with iodine to form thyroid hormones .thus thyroid hormones form within the thyroglobulin molecule .
Thyroglobulin is synthesized in the thyroid cells & secreted into the colloid . the first step in the formation of thyroid hormones is conversion of iodide ions to an oxidized form of iodine , this oxidation of iodine is promoted by the enzyme peroxidase . tyrosine is first iodized to monoiodotyrosine (MIT) this is next iodinated to form diiodotyrosin (DIT).
Two DIT molecules then undergo an oxidative condensation to form T4.or one molecule of MIT couples with one molecule of DIT to form triiodothyronine
Each thyroglobulin molecule contains 30 thyroxin molecules & a few triiodothyronine molecules.in this form thyroid hormones are stored in the follicles for 2-3 months.
Release of thyroxin & triiodothyronine from the thyroid
gland :The human thyroid secrets about 80µg (103 nmol)T4,& 4µg T3(7nmol).the thyroid cells ingest colloid by endocytosis .in the cells the globules of the colloid merge with lysosomes .the peptide bonds between the iodinated residuse & the thyroglobulin are broken by the proteases in the lysosomes &T4, T3,MIT,DIT are librated into the cytoplasm. the iodinated tyrosins are deiodinated by deiodinase enzyme ,T4&T3 pass into the circulation.
Figure 18.12 The Thyroid Follicles
Physiologic functions of thyroid hormones
Thyroid hormones increase cellular metabolic activity the BMR increase to 60-100% above normal when large quantities of hormone are released .the rate of utilization of foods for energy is accelerated ,the rate of protein synthesis is increased . thyroid hormones increase the number& activity of the mitochondria .thyroid hormones increase active transport of ions through cell membranes.
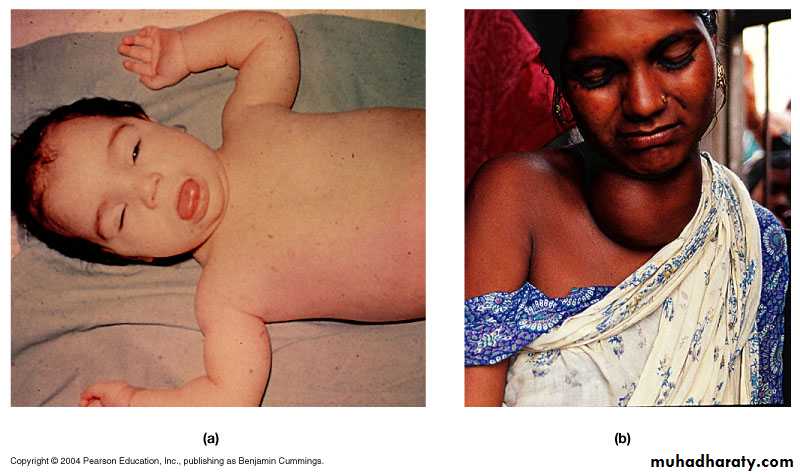
1.Effect of thyroid hormones on growth:
The effect of thyroid hormones on growth manifest in growing children.
In those who are hypothyroid the rate of growth is retarded.
In those who are hyperthyroid excessive skeletal growth occur causing the child to become taller at an earlier age.
An important effect is to promote growth & development of the brain during fetal life &for first few years of
postnatal life.
2.effects of thyroid hormones on specific bodily mechanisms:
Stimulation of carbohydrate metabolism , it causes rapid uptake of glucose by cells , increased glycolysis , enhanced gluconeogenesis , increased insulin secretion.
Stimulation of fat metabolism, decreases the concentrations of cholesterol,phospholipids, and triglycerides in the plasma
Increased requirement for vitamins.
Increased BMR.
Decreased body weight.
3.Effect of thyroid hormones on cardiovascular system
Increased blood flow and cardiac output . Increased metabolism in the tissues causes more utilization of oxygen than normal & releases greater than normal metabolic end products from the tissues , these effects cause vasodilatation so it increase blood flow & as a consequence cardiac output is increased .Increased heart rate thyroid hormone seems to have a direct effect on the excitability of the heart.
Increased heart strength ,The increased enzymatic activity caused by increased thyroid hormone production apparently increases the strength of the heart when only a slight excess of thyroid hormone is, but when increased markedly the strength of heart muscle decrease because of long-term excessive protein catabolism..
Normal arterial pressure : The mean arterial pressure usually remains about normal after administration of thyroid hormone. Because of increased blood flow
through the tissues between heartbeats, the pulse pressure is often increased, with the systolic pressure elevated in hyperthyroidism 10 to 15 mm Hg and the diastolic pressure reduced a corresponding amount.
4. Increased respiration : the increase in utilization of oxygen & formation of co2 increases the rate & depth of respiration .
5. Increased G.I.T motility : thyroid hormone increases both the rate of secretion of digestive juices & the motility of G.I.T . Diarrhea often result from hyperthyroidism while constipation from hypothyroidism .
6. Excitatory effects on the C.N.S : the hyperthyroid subject have extreme nervousness , anxiety .
7. Effect on the function of the muscles : increased thyroid hormone weakens the muscles because of protein catabolism , while hypothyroidism causes the muscle to become relax slowly after contraction .
Muscle Tremor. One of the most characteristic signs of
hyperthyroidism is a fine muscle tremor.
8. Effect on sleep : Because of the exhausting effect of thyroid hormone on the musculature and on the central nervous system, the hyperthyroid subject often has a feeling of constant tiredness, but because of the excitable effects of thyroid hormone on the synapses, it is difficult to sleep..
9. Effect on other endocrine glands : increased thyroid hormones increase the rate of secretions of most endocrine glands . Increased thyroxin secretion increases the rate of glucose metabolism
everywhere in the body and therefore causes a corresponding need for increased insulin secretion by the pancreas.
Effect on other endocrine glands
Also, thyroid hormone increases man metabolic activities related to bone formation and, aa consequence, increases the need for parathyroid hormone. Thyroid hormone also increases the rate at which adrenal glucocorticoids are inactivated by theliver. This leads to feedback increase in adrenocorticotropic hormone production by the anterior pituitary and, therefore, increased rate of glucocorticoid secretion by the adrenal glands.
Effect of Thyroid Hormone on Sexual Function
For normal sexual function, thyroid secretion needs to be approximately normal. In men, lack of thyroid hormone is likely to cause loss of libido; great excesses of the hormone, however, sometimes cause impotence.In women, lack of thyroid hormone often causes menorrhagia and polymenorrhea— that is, respectively, excessive and frequent menstrual bleeding.
In the hyperthyroid woman, oligomenorrhea, which means greatly reduced bleeding, is common, and occasionally amenorrhea results.
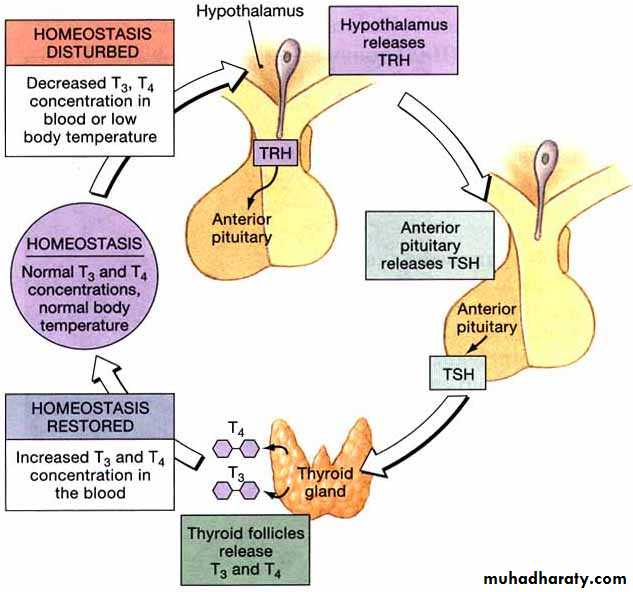
Regulation of thyroid hormone secretion
The anterior pituitary secretion of TSH is controlled by TRH which secreted by nerve endings in the median emninence of the hypothalamus , then TRH is transported to the anterior pituitary by way of hypothalamic – hypophysial portal blood .TRH is a tripeptide amide , it stimulates the anterior pituitary to secrete TSH .
TSH also called thyrotropin , is a glycoprotein with a molecular weight of about 28000 , this hormone increases the secretion of thyroxin & tri-iodothyronine by the thyroid gland .
increased thyroid hormone in body fluids , decreases secretion of TSH by the anterior pituitary .
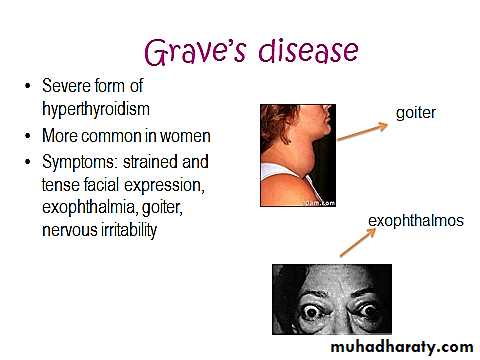
Diseases of the thyroid gland
Hyperthyroidism :
The thyroid gland is increased 2 – 3 times normal size and increase thyroid secretion .
Symptoms :
Excitability .
Intolerance to heat .
Increase sweating .
Weight loss .
Diarrhea .
Muscle weakness .
Nervousness .
Fatigue .
Tremor of hands .
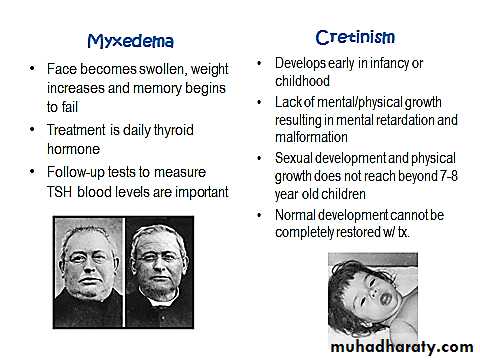
Hypothyroidism :
Decreased thyroid hormone secretion .symptoms :
Fatigue and sleep up to 12 -14 h / day .
Slow heart rate and decreased cardiac output , decreased blood volume .
Increased body weight .
Constipation .
Mental sluggishness .
Husky voice .
Decreased hair growth .
Thyroid Disorders
PHYSIOLOGY OF THE ENDOCRINE SYSTEM
parathyroid glandcalcium & phosphate regulation in the extra cellular fluid & plasmaECF calcium normal value 9.4 mg / dl (2.4 mmol / L ) .
Calcium plays a key role in many physiological processes including :
Contraction of skeletal ,cardiac and smooth muscle .
Blood clotting .
Transmission of nerve impulses .
Only 0.1% of total body Ca is in the ECF , 1% is in the cells and the rest is stored in the bones .
About 85% of the body s phosphate is stored in bones , 14 – 15 %is in the cells and less than 1% is in the ECF.
The calcium in the plasma is present in three forms :
1. About 41%( 1mmol / L) of calcium is combined with the plasma proteins and in this form is non-diffusible through the capillary membrane.
2. About 9% ( 0.2 mmol / L) is combined with an ionic substances ( citrate & phosphate ) . is diffusible through the capillary membrane
3. 50 % is ionized . is diffusible through the capillary membrane, the plasma and interstitial fluids have a normal calcium ion concentration of about 1.2 mmol/L (or 2.4 mEq/L) This ionic calcium is the form that is important for
most functions of calcium in the body.
Inorganic phosphate in extra cellular fluid
Inorganic phosphate in the plasma is mainly in two forms: HPO4and H2PO4 The concentration of HPO4 is about 1.05 mmol/L, and the concentration of H2PO4 - is about 0.26 mmol/L.
when the pH of the extracellular fluid becomes more acidic, there is a relative increase in H2PO4 and a decrease in HPO4-, whereas the opposite occurs when the extracellular fluid becomes alkaline.
The average total quantity of inorganic phosphorus represented by both phosphate ions is about 4 mg/dl, varying between normal limits of 3 to 4 mg/dl in adults and 4 to 5 mg/dl in children.
Non –bone physiologic effect of altered Ca & phosphate concentrations in the body fluids.
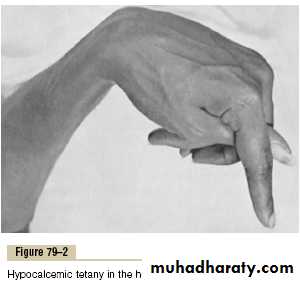
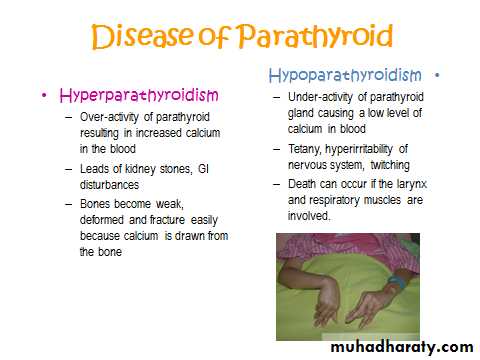
Hypocalcemia causes nervous system excitement & tetany .
Hypercalcemia decreases nervous system & muscle activity .
When ECF concentration of Ca ions falls below normal the nervous system becomes more excitable , because this causes increased neural membrane permeability to Na ions allowing easy initiation of action potential .
At plasma Ca 50% below normal , the peripheral nerve fibers become so excitable that they discharge spontaneously initiating nerve impulses that pass to the peripheral skeletal muscles to cause tetanic muscle contraction .
It also causes seizures because of its action of increasing excitability of the brain .
this pic. Shows carpopedal spasm .
Tetany occurs when the blood concentration of Ca falls from 9.4 mg / dl to about 6 mg / dl , which is only 35% below normal & is usually lethal at about 4 mg / dl .
When calcium level in the body fluids rises above normal , the nervous system becomes depressed & reflex activities of the nervous system are sluggish , also decrease the QT interval of the heart , constipation and lack of appetite .
These effects occur when the level of calcium rises above 12 mg / dl .
when the level of calcium rises above 17mg /dl in blood , calcium , phosphate crystals precipitate throughout the body .Absorption & excretion of calcium and phosphate
Intestinal absorption & fecal excretion .
the usual rates of intake are about 1000 mg / day for calcium & phosphate , Ca ions are poorly absorbed from the intestine , vitamin D promotes its absorption by the intestine. about 35%( 350 mg / day ) of ingested calcium is usually absorbed , the remaining is excreted in the feces .
an additional 250 mg of calcium enters the intestine via secreted G.I.T. juices thus90% ( 900 mg / day ) of daily intake of calcium is excreted in feces .
Intestinal absorption of phosphate occurs very easily. Except for the portion of phosphate that is excreted in the feces in combination with nonabsorbed calcium, almost all the dietary phosphate is absorbed into the blood from the gut and later excreted in the urine.
Renal excretion of calcium & phosphate
About 10% ( 100 mg / day ) of ingested calcium is excreted in urine .About 41%of plasma calcium is bound to plasma proteins and therefore not filtered by the glomerular capillaries . The rest is combined with anions such as phosphate ( 9% ) or ionized 50% and is filtered through the glomeruli into the renal tubules .
Normally renal tubules absorb 99% of the filtered calcium & about 100mg / day is excreted in urine . About 90%of calcium in the glomerular filtrate is reabsorbed in the proximal tubules , loop of Henle and early distal tubules , then in the late distal tubular and early collecting ducts ,reabsorption of remaining 10% is very selective , depending on calcium ion concentration in blood .
When concentration is low , this reabsorption is great , so that almost , no calcium is lost in urine . Conversely , even a minute increase in blood calcium ion concentration above normal increases excretion markedly.
Renal phosphate excretion is controlled by an overflow mechanism that is when phosphate concentration in the plasma is below the critical value of about 1 mmol / L, all the phosphate in the glomerular filtrate is reabsorbed & no phosphate is lost in the urine .
But above this critical concentration , the rate of phosphate loss is directly proportional to the additional increase .
Vitamin D
Vitamin D3 ( cholecalciferol ) is found in the skin .
This is activated &converted to 25-hydroxycholecalciferol in the liver & this has a negative feedback effect on the conversion reactions .
25-hydroxycholecalciferol in the proximal tubules of the kidneys is converted to 1, 25-dihydroxycholecalciferol .this is the most active form of vitamin D .this conversion requires PTH .
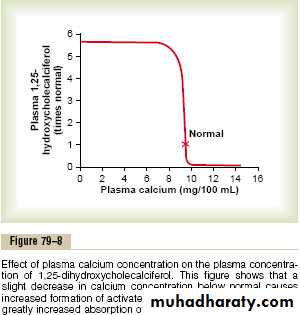
This demonstrates that plasma concentration of 1, 25-dihydroxycholecalciferol is inversely affected by the concentration of calcium in the plasma.
There are 2 reasons for this :
First : the calcium ion itself has a slight effect in preventing the conversion of 25-hydroxycholecalciferol to 1, 25-dihydroxycholecalciferol .Second : the rate of secretion of PTH is greatly decreased when plasma calcium ion concentration rises above 9 – 10 mg / 100ML , therefore , at calcium concentration below this level ,PTH promotes the conversion of 25-hydroxycholecalciferol to 1, 25-dihydroxycholecalciferol in the kidneys .
At higher plasma calcium concentration when PTH is decreased , the 25-hydroxycholecalciferol is converted to 24, 25-dihydroxycholecalciferol that has no vitamin D effect .
Actions of vitamin D
It promotes intestinal calcium absorption .It promotes phosphate absorption by the intestines .
It decreases renal calcium and phosphate excretion .
It plays an important role in both bone absorption & bone deposition .
Parathyroid hormone
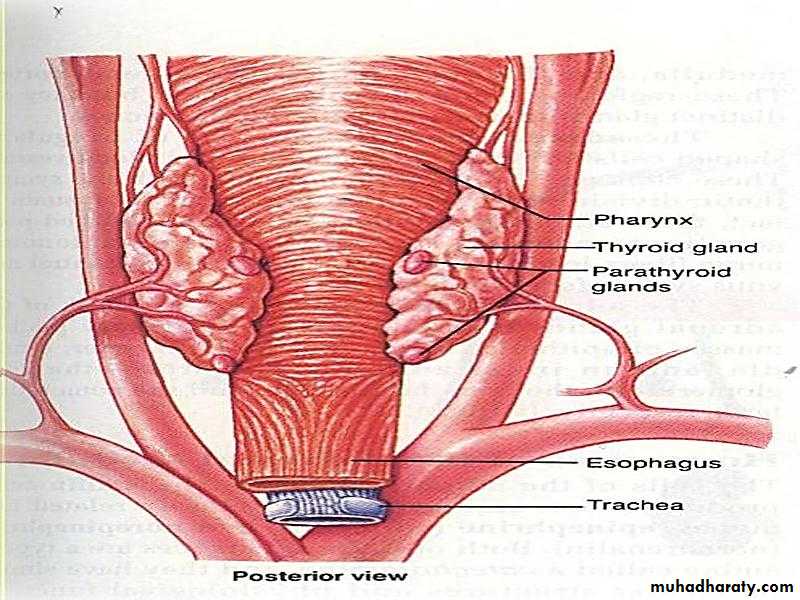
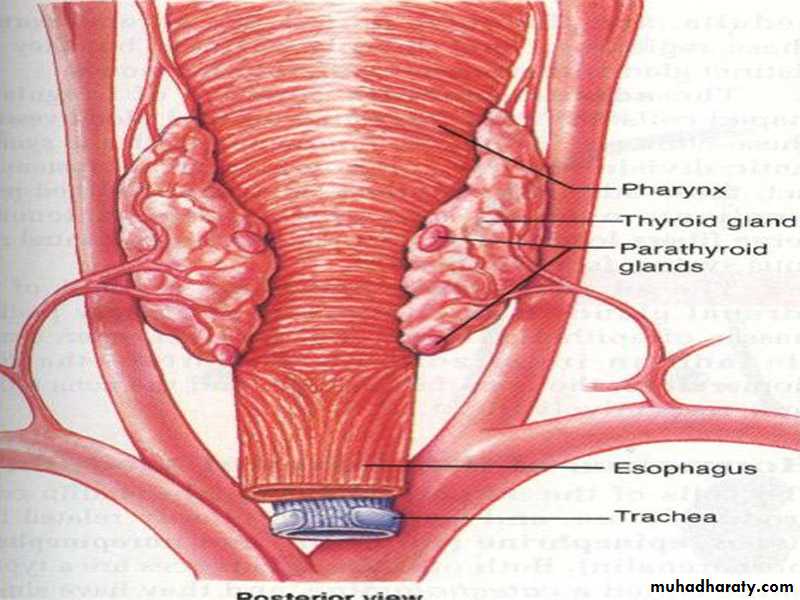
Normally there are 4 parathyroid glands in humans , they are located immediately behind the thyroid gland and behind each of the upper &each of the lower poles of the thyroid.
The parathyroid gland contains mainly chief cells which secret PTH .PTH is a polypeptide with 84 amino acids .
Effect of PTH on calcium & phosphate concentration in ECF
1. PTH increases calcium &phosphate absorption from the bone .2. It decrease the excretion of the calcium by the kidney .
3. It increases renal phosphate excretion .
Effect of PTH on bone .
PTH has 2 effects on bone in causing absorption of calcium & phosphate ;One Is rapid phase that begins in minutes & increasing progressively for several hours , this phase results from activation of the already existing bone cells to promote calcium and phosphate absorption .
The second phase is a much slower one requiring several days or even weeks , it result from proliferation of the osteoclasts followed by increased osteoclastic reabsorption .
Effect of PTH on renal tubules .
PTH increases renal tubular reabsorption of calcium , at the same time it decreases phosphate reabsorption .
The increase of calcium absorption occurs mainly in the late distal tubules , the collecting tubules & the ascending loop of Henle to a lesser extent.
Effect of PTH on intestine .
PTH increases intestinal absorption of calcium & phosphate by increasing the formation of 1, 25-dihydroxycholecalciferol in the kidneys for vitamin D .
Control of PTH secretion by calcium ion concentration
Even the slightest decrease in calcium ion concentration in ECF causes the parathyroid glands to increase their rate of secretion within minutes , if the decreased calcium continue , the glands will hypertrophy , sometimes five folds .The parathyroid glands enlarge in rickets , in pregnancy and in lactation .
Conversely conditions that increase Ca ion concentration above normal cause decreased activity & reduced size of parathyroid gland such condititions include :
Excess calcium in the diet .
Increased vit.D in the diet .
Bone absorption caused by disuse of bones .
Calcitonin
It is a peptide hormone secreted by the thyroid gland , it decreases plasma calcium concentration &has effects opposite to those of PTH .
synthesis & secretion of calcitonin occur in the Para follicular cells or C cells , lying in the interstitial fluid between the follicles of the thyroid gland .
The primary stimulus for calcitonin secretion is increased calcium ion concentration in plasma .
The reduction of Ca ions concentration caused by calcitonin leads within hours to a powerful stimulation of PTH secretion which over rides the calcitonin effect .
PHYSIOLOGY OF THE ENDOCRINE SYSTEM
Adrenal Gland
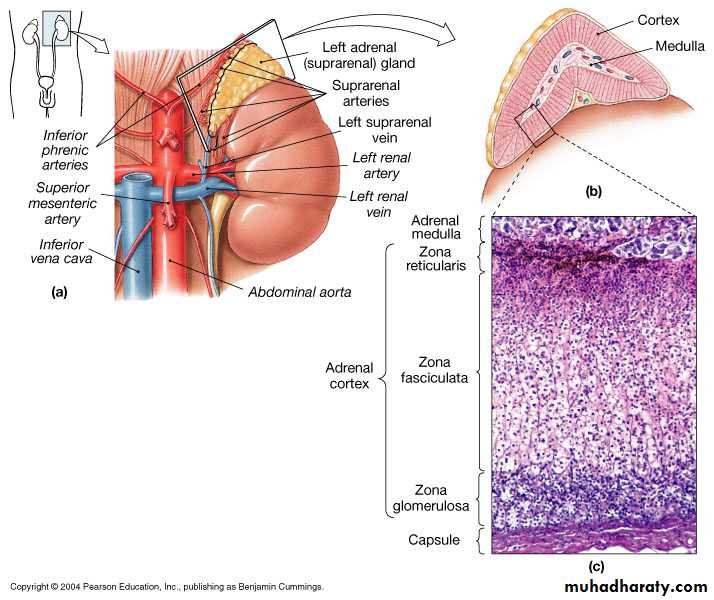
The two adrenal glands , each of which weighs 4 gm , lie at the superior poles of the kidneys
The Adrenal Gland
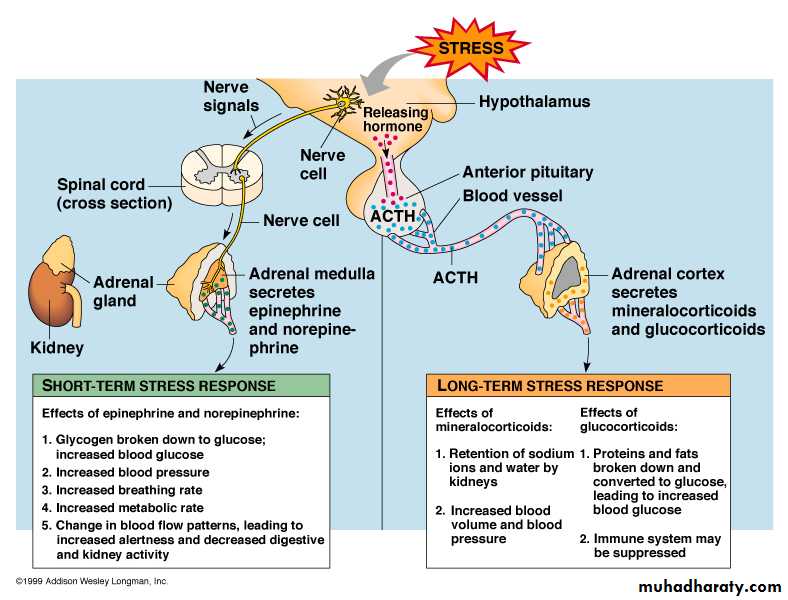
Each gland is composed of 2 parts , the adrenal medulla and adrenal cortex. The adrenal medulla ,central 20% of the gland , is functionally related to the sympathetic nervous system , it secrets the hormones epinephrine & norepinephrine in response to sympathetic stimulation .
In turn these hormones cause almost the same effect as direct stimulation of the sympathetic nerves in all parts of the body .
The adrenal cortex secretes corticoids . These hormones synthesized from the steroid cholesterol ,and they all have the similar chemical formulas .
The corticoids , mineralocorticoids ,glucocorticoids and androgens
Two major types of adrenocortical hormones , the mineralocorticoids & the glucocorticoids, are secreted by the adrenal cortex . In addition small amount of hormones are secreted , especially androgenic hormones which have the same effect of testosterone ( male sex hormone ) .
Mineralocorticoids affect the electrolytes ( minerals ) of the ECF , sodium & potassium .
Glucocorticoids they increase blood glucose concentration .
The steroids include aldosterone & cortisols which are the principal glucocorticoids .
Synthesis and secretion of the adrenocortical hormones
The adrenal cortex has 3 distinct layers .Zona glomerulosa:
a thin layer of cells that lies just underneath the capsule , constitutes about 15% of the adrenal cortex . These cells secrete aldosterone because they contain the enzyme aldosterone synthase . The secretion of these cells is controlled by the ECF concentration of angiotensin II & potassium , both of which stimulates aldosterone secretion .
Zona fasiculata :
the middle and widest layer , constitutes about 75% of the adrenal cortex and secretes the glucocorticoids , cortisole and corticosterone as well as small amounts of androgens and estrogens . The secretion of these cells is controlled by the hypothalamic – pituitary axis via ACTH .
Zona reticularis :
the deep layer of the cortex , secretes the adrenal androgens dehydroepiandrosterone (DHEA) and androstenedione , as well as small amounts of estrogens and some glucocorticoids. ACTH also regulates secretion of these cells .Mineralocorticoids include :
Aldosterone (very potent account for 90 % of all mineralocorticoids activity).Deoxycorticosterone (1 / 30 as a potent as aldosterone , but very small quantities secreted).
Corticosterone ( slight mineralocorticoid activity )
9 - Fluocorisol ( Synthetic, slightly more potent than aldosterone ) .
Cortisol ( very slight mineralocorticoid activity, but large quantity secreted ).
Cortisone ( Synthetic, slight mineralocorticoid activity ) .
Glucocorticoids :
Cortisol ( very potent, account for about 95% of all glucocorticoids activity ).Corticosterone ( provides about 4% of total glucocorticoids activity, but much less potent than cortisol ).
Cortisone ( synthetic, almost as potent as cortisol ).
Prednisone (synthetic, four times as potent as cortisol).
Methyl prednisone ( synthetic, five times as potent as cortisol)
Dexamethasone ( synthetic, 30 times as potent as cortisol ).
Approximately 90-95% of cortisol in the plasma binds to plasma proteins , especially globulin called cortisol-binding globulin or transcortin & to a lesser extent to albumin .
Cortisol has half life of 60-90 minutes .
Only about 60% of the circulating aldosterone combinds with the plasma proteins, so about 40% in the free form . Aldosterone has short half life of about 20 minutes .
Aldosterone’s mineralocorticoid activity is about 3000 times greater than that
of cortisol, but the plasma concentration of cortisol is nearly 2000 times that of aldosteroneThe concentration of aldosterone in blood is about 6nanograms/100 ml .
The concentration of cortisol in the blood averages 12 mg /100 ml.
Functions of the mineralocorticoids – aldosterone
Renal & circulatory effects of aldosterone :
Aldosterone increases absorption of sodium and secretion of potassium by the renal tubular epithelial cells especially in the principal cells of the collecting tubule and to a lesser extent in the distal tubules and the collecting ducts. Therefore, aldosterone causes sodium to be conserved in the ECF while increasing potassium excretion in the urine .
Excess aldosterone increases ECF volume and arterial pressure but has only small effect on the plasma sodium concentration, although, has a potent effect in decreasing the rate of sodium excretion by the kidneys, the concentration of sodium in the extra cellular fluids often rises only a few milliequievelants.
The reason for this is that when sodium is reabsorbed , there is simultaneous osmotic absorption of almost equivalent amount of water also small increase in ECF sodium concentration stimulate thirst and increased water intake .
Therefore the ECF volume , increases almost as much as the retained sodium , but without much change in sodium concentration .
An aldosterone – mediated increase in ECF volume last for 1-2 days also leads to an increase in arterial pressure , this increases kidney excretion of both salt and water called pressure natriuresis and pressure diuresis . This return to normal of salt and water excretion by the kidneys as a result of pressure diuresis and natriuresis is called aldosterone escape .
Conversely , when aldosterone secretion becomes zero , large amounts of salt are lost in the urine , decreasing the ECF volume , the result is circulatory shock .
3. Excess aldosterone causes hypokalemia and muscle weakness . Too little aldosterone causes hyperkalemia and cardiac toxicity .
Excess secretion of aldosterone causes serious decrease in plasma potassium concentration , sometimes from the normal value of 4.5 mg / L to as low as 2 mg / L this condition is called hypokalemia . When potassium ion concentration falls below about ½ normal severe muscle weakness often develops .
Conversely , when aldosterone is deficient , the ECF potassium ion concentration can rise above normal , when it rises 60 – 100 % above normal cardiac toxicity occur , causes weakness of heart contraction and development of arrhythmia .
4. Excess aldosterone increases tubular hydrogen ion secretion , with resultant mild alkalosis .
Aldosterone causes secretion of hydrogen ions in exchange for sodium in the intercalated cells of the cortical collecting tubules , this decrease the hydrogen ion concentration in the ECF . This effect usually causes a mild degree of alkalosis .
Aldosterone stimulates sodium and potassium transport in sweat glands , salivary glands & intestinal epithelial cells
Aldosterone has almost the same effects on sweat glands and salivary glands as it has on the renal tubules . Both these glands form a primary secretion that contains large quantities of sodium chloride , but much of this is reabsorbed by excretory ducts ,whereas potassium and bicarbonate ions are secreted .
The effect on the sweat glands is important to conserve body salt in hot environment and the effect on salivary glands is necessary to conserve salt when excessive quantities of saliva are lost .
Aldosterone also greatly enhances sodium absorption by the intestines especially in the colon which prevents lose of sodium in the stools . The absence of aldosterone leads to diarrhea , with loss of salt from the body .
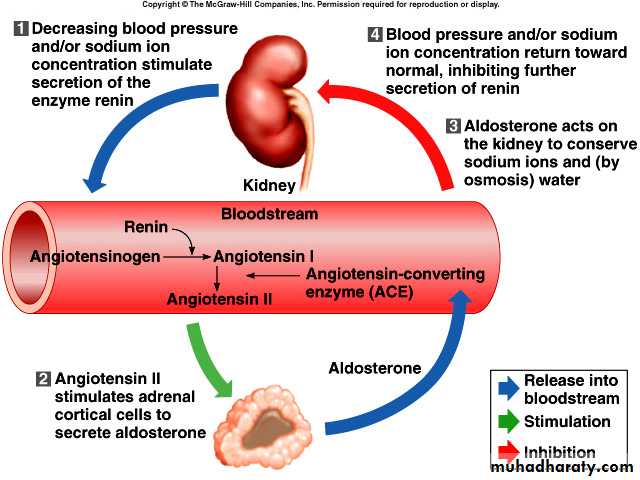
Regulation of aldosterone secretion
Four factors play essential roles in the regulation ;Increased potassium ion concentration in the ECF greatly increases aldosterone secretion .
Increase activity of the rennin – angiotensin system greatly increases aldosterone secretion .
Increased sodium ion concentration in the ECF may slightly decrease aldosterone secretion .
ACTH from the anterior pituitary gland is necessary for aldosterone secretion , but has little effect in controlling the rate of secretion .
Of these factors , K + concentration & the rennin – angiotensin system are the most potent in regulating aldosterone secretion .
Activation of rennin – angiotensin system cause several fold increase in aldosterone secretion .
In turn , the aldosterone acts on the kidneys ;
To help the excrete the excess potassium ions .
To increase blood volume & arterial pressure thus returning rennin – angiotensin system toward normal , these feedback control mechanisms are essential for maintaining life .
Functions of the Glucocorticoids
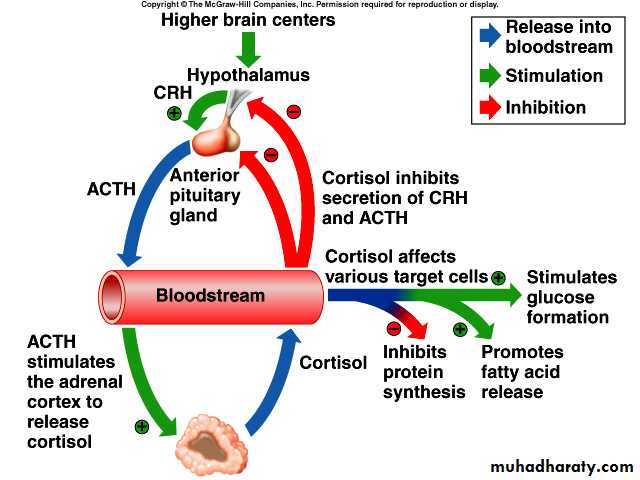
95% of the glucocorticoid activity of the adrenocortical secretion results from the secretion of cortisol , known also as hydrocortisone , in addition small but significant amount of glucocorticoid activity is provided by corticosterone .Effect of cortisol on carbohydrate metabolism
Stimulation of gluconeogenesis .
that is formation of carbohydrate from proteins & other substances by the liver this result mainly from two effects of cortisol :
a. Cortisol increases the enzymes required to convert amino acids into glucose in the liver cells .
b. cortisol causes mobilization of amino acids from the extra hepatic tissues mainly from muscle .
2. Decreased glucose utilization by the cells .
3. Elevated blood glucose concentration & adrenal diabetes .
Effect of cortisol on fat metabolism
Mobilization of fatty acids , this helps shift the metabolic system of the cells in times of starvation or other stresses from utilization of glucose for energy to utilization of fatty acids .Many people with excess cortisol secretion develop type of obesity , with excess deposition of fat in the chest & head regions of the body giving a buffalo like tor so and a rounded “ moon face “ this obesity result from excess food intake .
Cortisol is important in resisting stress & inflammation
Almost any type of stress causes an immediate & marked increase in ACTH secretion by the anterior pituitary followed by increased adrenocortical secretion of cortisol .Some different types of stress that increase cortisol release are the following ;
Trauma , infection , intense heat or cold , injection of norepinephrine ,surgery , injection of necrotizing substances beneath the skin , any debilitating disease .
Glucocorticoids cause rapid mobilization of amino acids & fats from their cellular stores making them immediately available both for energy & for synthesis of other compounds including glucose needed by different tissues of the body .
Anti-inflammatory effect of high levels of cortisol
When tissues are damaged by trauma ,by infection with bacteria , they almost become inflamed , the administration of cortisol can usually block this inflammation by ;
1. It can block the early stages of inflammation process .
2. If inflammation has already begun , it causes rapid resolution of the inflammation & increased rapidity of healing .
Cortisol prevents shock or death in anaphylaxis .
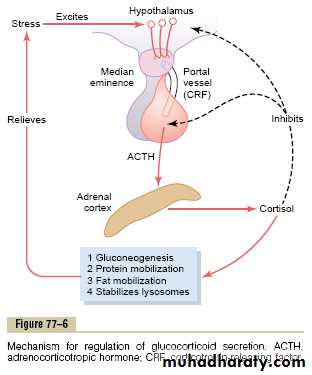
Regulation of cortisol secretion by ACTH from the anterior pituitary
ACTH is a large polypeptide , has 39 amino acids .it is controlled by Corticotropin –releasing factor ( CRF) from the hypothalamus .ACTH act on adrenocortical cells to produce steroids ,
Stress stimuli activate the entire control system to cause rapid release of cortisol & the cortisol in turn initiates a series of metabolic effects .there is direct feedback of the cortisol to both the hypothalamus & the anterior pituitary to decrease the concentration of cortisol in plasma .The secretory rate of CRF, ACTH & cortisol are high in early morning but low in the late evening .
Adrenal Androgens
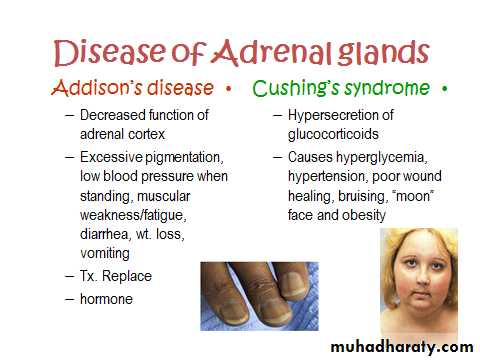
The most important male sex hormone is dehydroepiandrosterone secreted by the adrenal cortex , also female sex hormones are secreted in small quantities as estrogen & progesterone some of the adrenal androgens are converted to testosterone in the extra-adrenal tissues.Abnormalities of adrenocortical secretion
1. Hypoadrenalism __ Addison s disease is failure of adrenal cortex to produce adrenocortical hormones .
2. Hyperadrenalism __ cushing s syndrome .
3. Primary aldosteronism __ conn s syndrome , tumor of zona granulosa.
PHYSIOLOGY OF THE ENDOCRINE SYSTEM
PancreasThe pancreas is a nodular organ occupying a space between the stomach & small intestine. It contains both exocrine & endocrine cells. The exocrine pancreas secretes an enzyme-rich fluid into the lumen of the digestive tract. Cells of the endocrine pancreas form clusters called pancreatic islets (islets of Langerhans).
Each islet contains 4 cell types:
alpha cells produce glucagon;
beta cells secrete insulin
delta cells secrete somatostatin (growth hormone-inhibiting factor).
F- cells secrete pancreatic polypeptide.(10% of the cells).
Β- cells account for 60-75% of the cells in the islet.
Α- cells account for 20% of cells of islet.
Insulin and its metabolic effects
Insulin was first isolated from the pancreas in 1922 .It is a small protein , has a molecular weight of 5808 .
It is composed of two amino acid chains connected to each other by disulfide linkages .
Insulin is synthesized in the beta cells , when insulin is secreted in the blood , it circulates in an unbound form , it has a plasma half life about 6 minutes , so that it is cleared from the circulation within 10-15 minutes .
Insulin is degraded by the enzyme insulinase mainly in the liver & to a lessor extent in the kidneys & muscles , except that portion of insulin that combines with receptors in the target cells.
Effect of Insulin on CarbohydrateMetabolism
Insulin Promotes Muscle Glucose Uptakeand Metabolism
under two conditions the muscles do use large amounts of glucose. One of these is during moderate or heavy exercise.This usage of glucose does not
require large amounts of insulin, because exercising muscle fibers become more permeable to glucose even in the absence of insulin because of the contraction process itself.
The second condition for muscle usage of large amounts of glucose is during the few hours after a meal. At this time the blood glucose concentration is
high and the pancreas is secreting large quantities of insulin. The extra insulin causes rapid transport of glucose into the muscle cells.
Effect of Insulin on CarbohydrateMetabolism
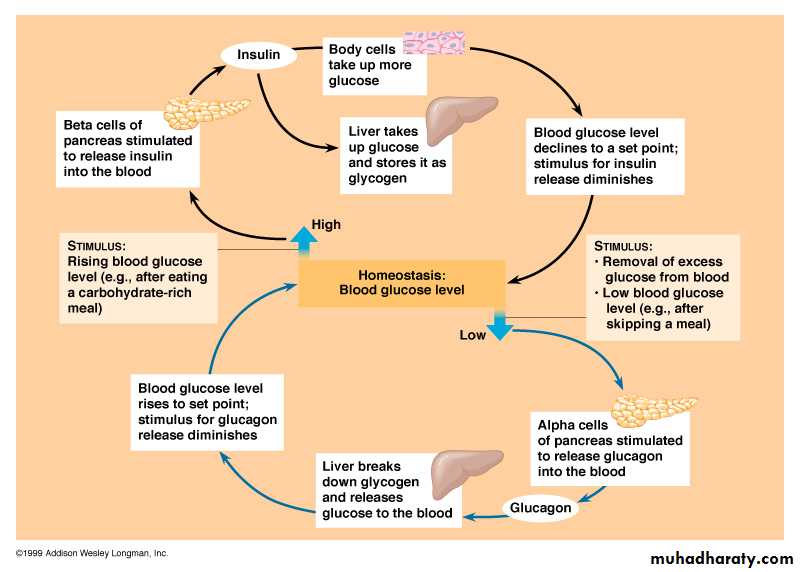
2.Insulin Promotes Liver Uptake, Storage, and
Use of Glucose
One of the most important of all the effects of insulin is to cause most of the glucose absorbed after a meal to be stored almost immediately in the liver in the form of glycogen. Then, between meals, when food is not available and the blood glucose concentration begins to fall, insulin secretion decreases rapidly and the liver glycogen is split back into glucose, which is
released back into the blood to keep the glucose concentration from falling too low.
Effect of Insulin on CarbohydrateMetabolism
Lack of Effect of Insulin on Glucose Uptakeand Usage by the Brain
The brain is quite different from most other tissues of the body in that insulin has little effect on uptake or use of glucose. Instead, the brain cells are permeable to glucose and can use glucose without the intermediation
of insulin.
Effect of Insulin on Fat Metabolism
Insulin Promotes Fat Synthesis and StorageInsulin has several effects that lead to fat storage in adipose tissue. First, insulin increases the utilization of glucose by most of the body’s tissues, which automatically decreases the utilization of fat, thus functioning as a fat sparer. However, insulin also promotes fatty acid synthesis. This is especially true when more carbohydrates are ingested than can be used for immediate energy, thus providing the substrate for fat synthesis.
Effect of Insulin on ProteinMetabolism and on Growth
Insulin Promotes Protein Synthesis and Storage1. Insulin stimulates transport of many of the amino
acids into the cells.
2.Insulin increases the translation of messenger RNA, thus forming new proteins.
3.Insulin inhibits the catabolism of proteins, thus decreasing the rate of amino acid release from the cells, especially from the muscle cells.
4.In the liver, insulin depresses the rate of gluconeogenesis. It does this by decreasing the activity of the enzymes that promote gluconeogenesis.
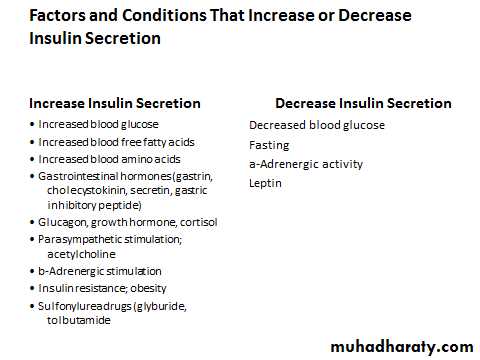
Control of Insulin Secretion
Increased Blood Glucose Stimulates Insulin SecretionAt the normal fasting level of blood glucose of 80 to 90 mg/100 ml, the rate of insulin secretion is minimal
If the blood glucose concentration is suddenly increased to a level
two to three times normal and kept at this high level thereafter, insulin secretion increases markedly in two stages
1. Plasma insulin concentration increases almost 10-fold within 3 to 5 minutes after the acute elevation of the blood glucose; this results from immediate dumping of preformed insulin from the beta cells of the islets of Langerhans. However, the initial high rate of secretion is not maintained; instead, the insulin concentration decreases about halfway back toward normal in another 5 to 10 minutes.
2. Beginning at about 15 minutes, insulin secretion rises a second time and reaches a new plateau in 2 to 3 hours, this time usually at a rate of secretion even greater than that in the initial phase. This secretion results both from additional release of preformed insulin and from activation of the enzyme system that synthesizes and releases new insulin from the cells.
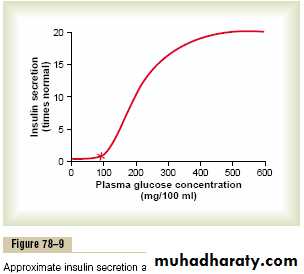
Feedback Relation Between Blood Glucose Concentration andInsulin Secretion Rate
As the concentration of blood glucose rises above 100 mg/100 ml of blood, the rate of insulin secretion rises rapidly, reaching a peak some10 to 25 times the basal level at blood glucose concentrations between 400 and 600 mg/100 ml, as shown
Glucagon and its function
Is a hormone secreted by the alpha cells of the islet of langerhans when the blood glucose concentration falls , has several functions that opposed to those of insulin . Most important of these functions is to increase the blood glucose concentration .Glucagon is a large polypeptide , is composed of 29 amino acids . glucagon is also called the hyperglycemic hormone.
Effect of glucagon on glucose metabolism
The major effects of glucagon on glucose metabolism are:-
Breakdown of liver glycogen ( glycogenolysis ).
Increased gluconeogenesis in the liver .
Both of these effects enhance the availability of glucose to the other organs of the body .
Other effects of glucagon occur only when its concentration rises well above the maximum normally found in blood. The most important effect is that glucagon activates adipose cell lipase , making increased quantities of fatty acids .
Glucagon in very high concentration also :-
Enhance the strength of the heart .Increase blood flow in some tissues .
Enhances bile secretion .
Inhibit gastric acid secretion .
Regulation of glucagon secretion
Increase blood glucose inhibits glucagon secretion :the blood glucose concentration is the most potent factor that controls glucagon secretion . That the effect of blood glucose concentration on glucagon secretion is exactly the apposite direction from the effect of glucose on insulin secretion .
The decrease in the blood glucose concentration to hypoglycemic levels can increase the plasma concentration of glucagon several fold , conversely the blood glucose to hyperglycemic levels decreases plasma glucagon.
2. Increased blood amino acids stimulate glucagon secretion , it is the same effect on insulin secretion .
glucagon promotes rapid conversion of amino acids to glucose .
3. Exercise stimulates glucagon secretion , in exhaustive exercise , the blood concentration of glucagon increase four fold to five fold .
Somatostatin inhibits glucagon & insulin secretion
The delta cells of the islet of Langerhans secrete somatstatin , which is a polypeptide containing 14 amino acids , it has short half life of 3 minutes .
Almost all factors related to the ingestion of food stimulate somatostatin secretion .
They include :
Increased blood glucose .
increased amino acids .
Increased fatty acids .
Increased concentrations of several of G.I.T. hormones.
In turn , somatostatin has multiple inhibitory effects :
1. somatostatin acts locally within the islets of Langerhans themselves to decrease the secretion of both insulin & glucagon .2. somatostatin decreases the motility of the stomach , dudenum & gallbladder .
3. it decreases both secretion & absorption in the G.I.T.
Diabetes Mellitus
Diabetes mellitus is a syndrome of impaired carbohydrate, at, and protein metabolism caused by either lack of insulin secretion or decreased sensitivity of the tissues to insulin. There are two general types of diabetesmellitus:
1. Type I diabetes, also called insulin-dependent diabetes mellitus (IDDM), is caused by lack of insulin secretion.
2. Type II diabetes, also called non–insulin-dependent diabetes mellitus (NIDDM), is caused by decreased sensitivity of target tissues to the metabolic effect of insulin. This reduced sensitivity to insulin is often called insulin resistance
Diabetes Mellitus
In both types of diabetes mellitus, metabolism of all the main foodstuffs is altered.The basic effect of insulin lack or insulin resistance on glucose metabolism is to prevent the efficient uptake and utilization of glucose by most cells of the body, except those of the brain. Asa result, blood glucose concentration increases, cell utilization of glucose falls increasingly lower, and utilization of fats and proteins increases.
Pineal gland
Of the endocrine organs, the function of the pineal gland was the last discovered.Located deep in the center of the brain, the pineal gland was once known as the “third eye.”because of its location deep in the center of the brain to its connection to light.
The pineal gland produces melatonin, which helps maintain circadian rhythm and regulate reproductive hormones.
Anatomy of the Pineal Gland
Located near the center of the brain, the pineal gland is a very small organ shaped like a pine cone (which is where it gets its name). It’s reddish-gray and about 1/3 inch long. Pineal cells and neuroglial cells (which support the pineal cells) mainly comprise the gland.The pineal gland often appears calcified in x-rays, which is usually due to fluoride, calcium, and phosphorus deposits that build up with age.
Melatonin: The Pineal Gland Hormone
The pineal gland secretes a single hormone—melatonin (not to be confused with the pigment melanin). This simple hormone is special because its secretion is dictated by light. Researchers have determined that melatonin has two primary functions in humans—to help control your circadian (or biological) rhythm and regulate certain reproductive hormones.
Circadian Rhythm
Your circadian rhythm is a 24-hour biological cycle characterized by sleep-wake patterns. Daylight and darkness help dictate your circadian rhythm. Light exposure stops the release of melatonin, and in turn, this helps control your circadian rhythms.
Melatonin secretion is low during the daylight hours and high during dark periods, which has some influence over your reaction to photoperiod (the length of day versus night). Naturally, photoperiod affects sleep patterns, but melatonin’s degree of impact over sleep patterns is disputed.
Reproduction
Melatonin blocks the secretion of gonadotropins (luteinizing hormone and follicle stimulating hormone) from the anterior pituitary gland. These hormones aid in the proper development and functioning of the ovaries and testes.The pineal gland’s full purpose is still a bit of a mystery. But research suggests that we’re getting closer to understanding the pineal gland—and more about the endocrine system as a whole.