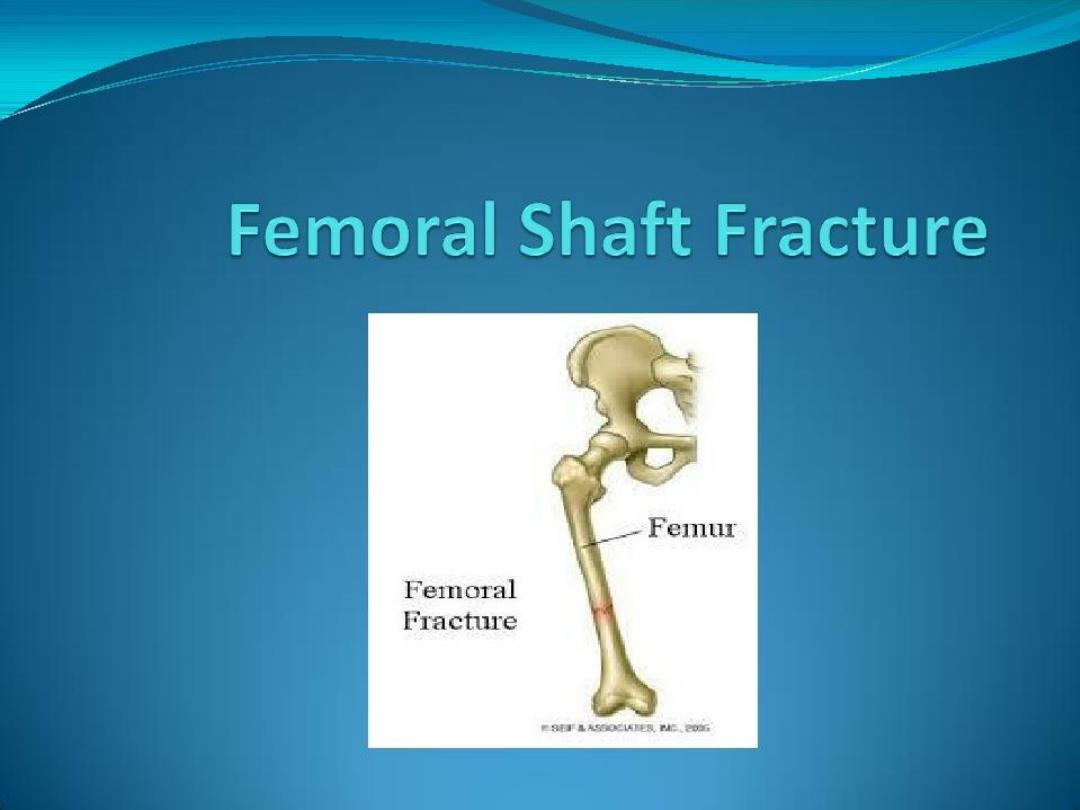

Femoral Shaft Fracture
The femoral shaft is well padded with muscles(an
advantage in protecting the bone from all but the most
powerful forces)but the disadvantage is that fractures
are often severely displaced by muscle pull ,making
reduction so difficult.

Femoral Shaft Fracture
Special Features:-
1.
It is essentially a fracture of young adults and usually
results from a high energy injury.
2.
Diaphyseal fracture in elderly patients should be
considered pathological unless proved otherwise.
3.
In children under 4 years of age ,the possibility of
physical abuse must be kept in mind.

Femoral Shaft Fracture
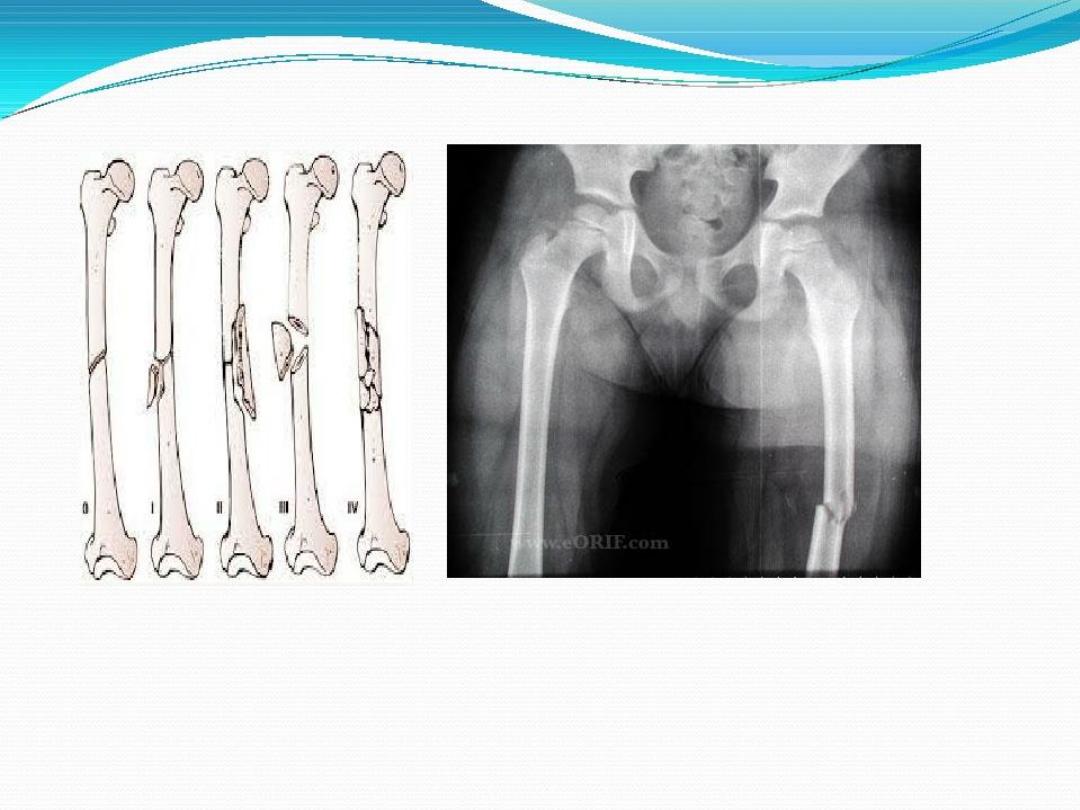
X-ray :-
A.
Most fractures of femoral shaft have some degree of
communication ,it is the reflection of the amount of
force involved in these injuries .
B.
Displacement may be in any direction.
C.
Sometimes there are two fracture lines separated by an
unbroken length of bone “the segmental fracture”.
D.
The pelvis and knee must always be x-rayed to avoid
missing a fracture in them.
Femoral Shaft Fracture
Treatment:-
The risk of systemic complications can be largely
reduced by early stabilizing of the fracture.
1.
General:-assessment of blood loss and resuscitation
of patient.

Femoral Shaft Fracture
2. Traction and bracing :-
The main indications of traction are :-
A.
Fractures in children.
B.
Contra-indications to anesthesia.
C.
Lack of suitable skill or facilities for internal fixation
.
The chief drawback is the length of time spent in
bed(10-14) weeks for adults with its attendant
problems.
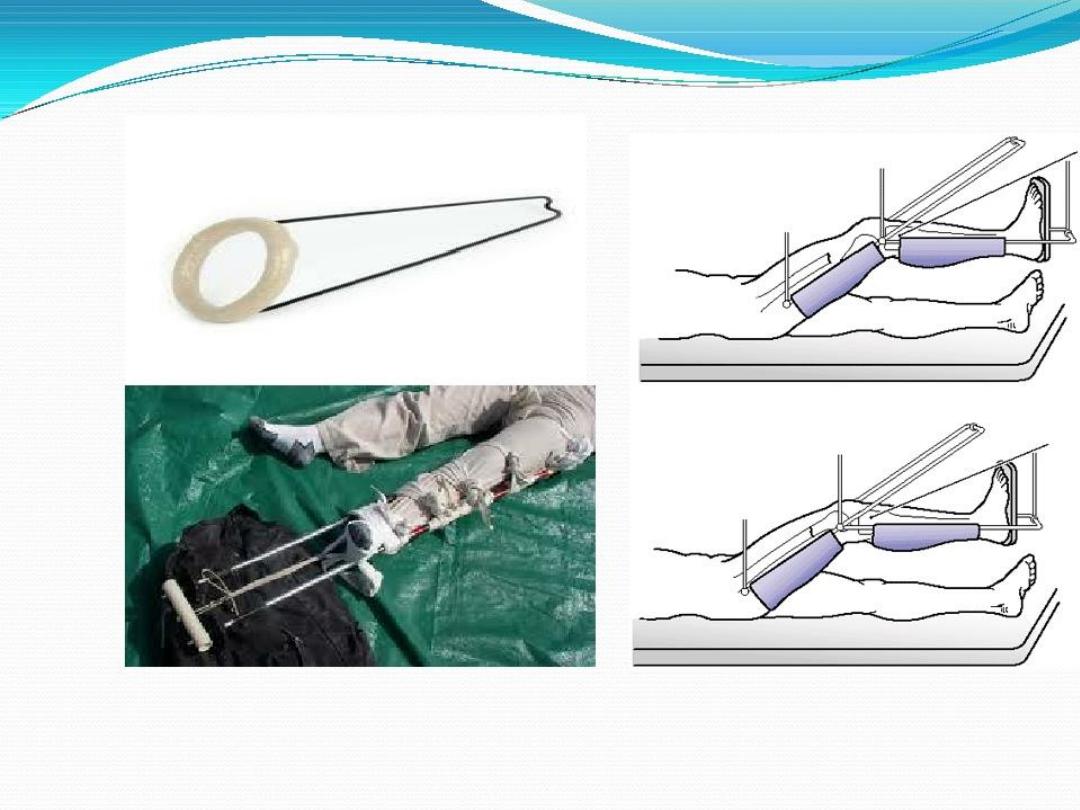

Femoral Shaft Fracture
Some of the difficulties are overcome by reducing the
time in traction and then changing to a plaster spica or
(in case of lower third fracture) functional bracing for
6-8 weeks.
While the patient in traction ,joint mobility must be
preserved by encouraging movement and exercise.

Femoral Shaft Fracture
3. Open reduction and plating :-
Fixation with plates and screw was popular but now it is
limited due to complications including implant
failure.
The main indications are :-
A.
Combination of femoral neck and shaft fractures.
B.
A shaft fracture with associated vascular injury.
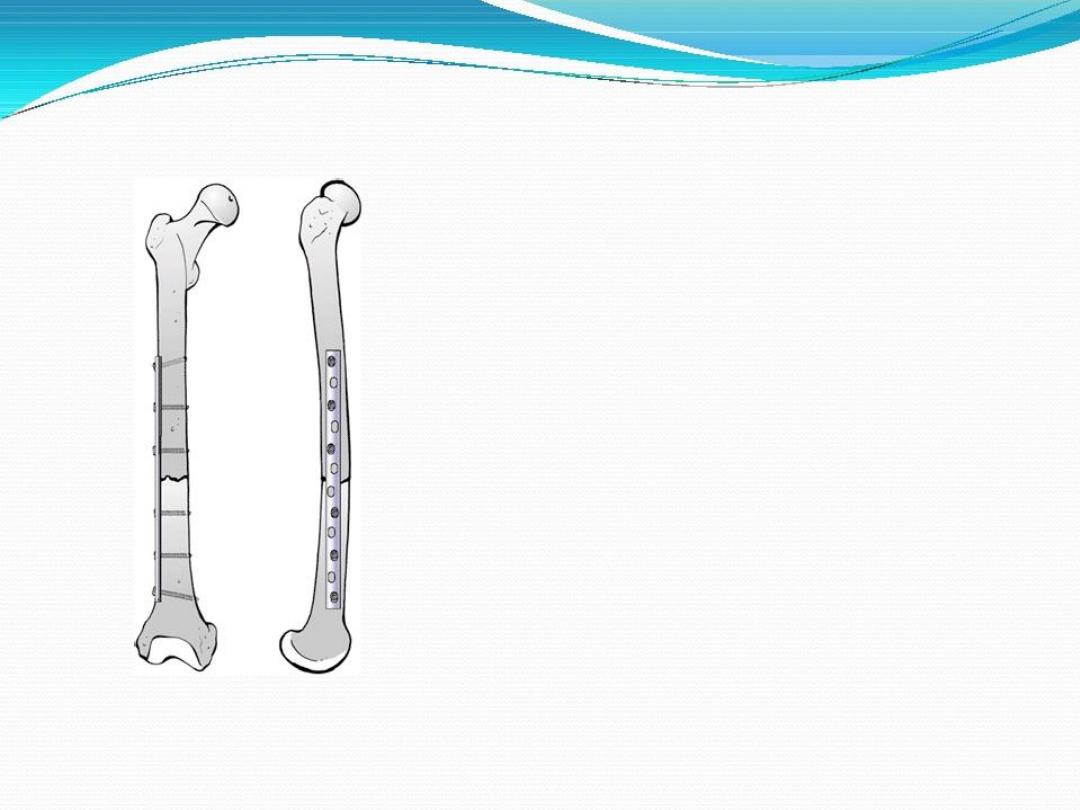

Femoral Shaft Fracture
4. Intra-medullary nailing:-
Is the method of choice for most femoral shaft fractures.
it controls rotation and ensure stability even for sub-
trochantric and distal third fractures.


Femoral Shaft Fracture
5. External fixation :-
Indication:-
A.
The treatment of severe open injuries.
B.
Management of patients with multiple injuries when
there is need to reduce operating time.
C.
Dealing with severe bone loss by bone transport.
D.
Treating femoral fractures in adolescents.


Femoral Shaft Fracture
Open fractures:-
open femoral fractures should be carefully examined for
:-
1.
Skin loss.
2.
Wound contamination.
3.
Muscle ischemia .
4.
Injury to vessels and nerves.

Femoral Shaft Fracture
The immediate treatment is similar to that of closed
wounds :-
1.
Antibiotics ,wound cleansing and debridement.
2.
With little skin loss or small clean wound ,the
fracture can be treated as closed.
3.
With massive skin loss large wound ,contaminated
wound ,tissue destruction ,the internal fixation
should be avoided and the wound left open and do
external fixation.

Femoral Shaft Fracture
Femoral fracture in children :
1.
Infants: 1-2 weeks in balanced traction followed be
spica for another 3-4 weeks .
2.
Children : up to 10 years can be treated in similar
manner but with 2-4 weeks of traction and 6 weeks
in spica.
3.
Teenagers: may required longer duration of traction
and spica . If satisfactory reduction can’t be obtained
or healed ,internal fixation with plate and screws is
justified especially in those with multiple injuries.

Femoral Shaft Fracture
Complications of femoral shaft fractures:
1.
General :- severe blood loss ,shock, fat embolism ,
and acute respiratory distress , are common in high
energy fractures.
2.
Vascular injuries :- the vascular lesion take priority
and the vessels must be repaired or grafted without
delay. At the same operation the fracture is secured
by internal fixation.
3.
Thrombo-embolism:- due to prolong traction in bed
.movement and exercise are important to prevent it.

Femoral Shaft Fracture
4.
Infection:- in open injuries and following internal
fixation , there is always a risk of infection. so give
prophylactic antibiotics and pay careful attention to
principle of surgery .
5.
Delayed union and non union:- it’s said that fractured
femur must be united in 100 days plus/minus 20 days.
6.
Malunion:- fractures treated by traction and bracing
often develop some deformity, no more than 15 degrees
angulation.
7.
Joint stiffness:- the knee joint is affected and may be
injured at the same time of insult, or it’s stiffness is due to
soft tissue adhesion during treatment.
Supracondylar femur fractures:
The supracondylar femur account for approximately 7% of all femur
fractures. They occur just proximal to the knee joint, in the terminal 9 cm
of the femur between the metaphyseal-diaphyseal junction and the
femoral condyles. Supracondylar femur fractures have a bimodal
distribution within the population. They present in younger patients due
to high-energy injuries, such as from motor vehicle collisions or falls
from height. In elderly patients, these fractures are often due to low-
energy injury mechanisms such as simple falls due to underlying
osteoporosis. Supracondylar femur fractures may extend proximally into
the diaphysis (patients presented with deformity & swelling of thigh with
external rotation of leg) or extend distally in the knee joint (patients
presented with severe swelling & deformity of the knee joint). Regardless
of injury mechanism, supracondylar femur fractures often require surgical
treatment for the restoration of limb alignment and fracture stability.


Complications:
1-Early: vascular injury.
2-Late :joint stiffness & non – union.
there are four bones that come together at the knee, only the
femur (thighbone) and the tibia (shinbone) form the joint itself.
The head of the fibula (strut bone on the outside of the leg)
provides some stability, and the pattella (kneecap) helps with
joint and muscle function. Movement and weight-bearing occur
where the ends of the femur called the femoral condyles match
up with the top flat surfaces of the tibia (tibial plateaus)
Knee Joint Injury
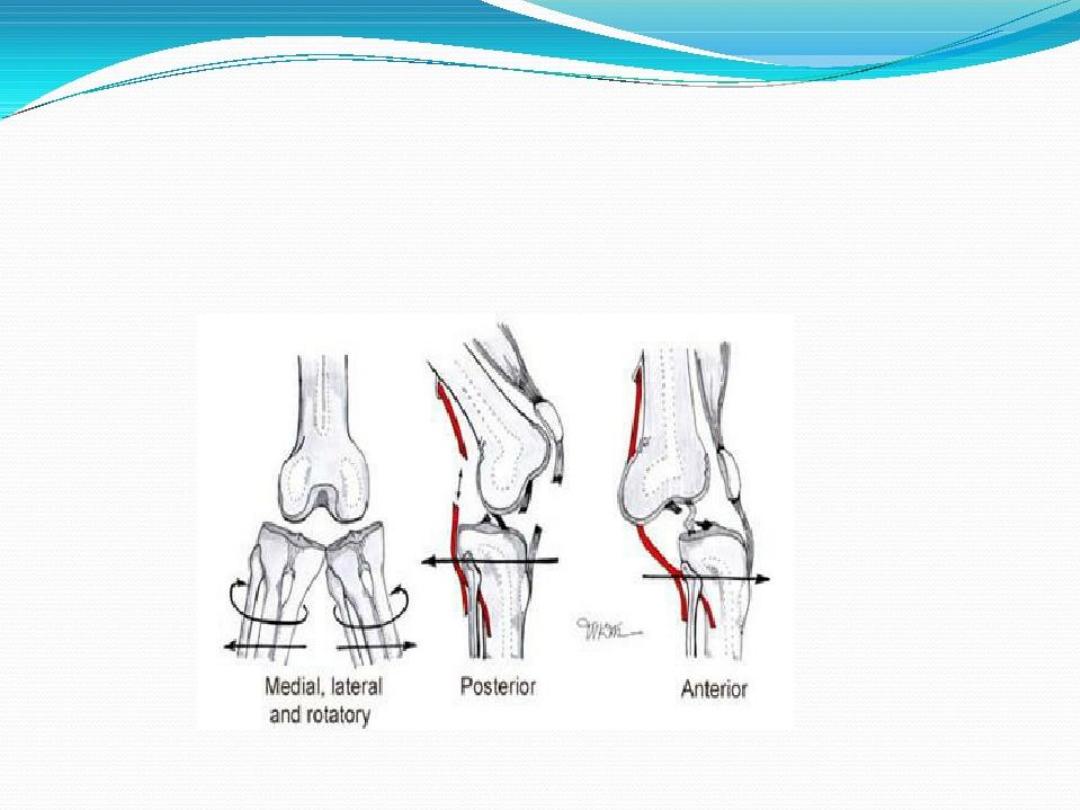
The stability of the knee joint is maintained by four ligaments, thick
bands of tissue that stabilize the joint. The medial collateral ligament
(MCL) and lateral collateral ligament (LCL) are on the sides of the knee
and prevent the joint from sliding sideways. The anterior cruciate
ligament (ACL) and posterior cruciate ligament (PCL) form an "X" on
the inside of the knee and prevent the knee from sliding back and
forth. These limitations on knee movement allow the knee to
concentrate the forces of the muscles on flexion and extension.
Inside the knee, there are two shock-absorbing pieces of cartilage
called menisci (singular
meniscus
) that sit on the top surface of the
tibia. The menisci allow the femoral condyle to move on the tibial
surface without friction, preventing the bones from rubbing on each
other. Without this cartilage covering, the friction of bone on bone
would cause inflammation, or arthritis.
Acute knee injuries can cause pain and swelling with difficulty
bending the knee and weight-bearing. Pain can also be felt with
specific activities. Pain while climbing stairs is a symptom of
meniscus injury, where the cartilage is being pinched in the joint as
the joint space narrows with knee bending. Pain with walking down
stairs suggests patellar pain, where the kneecap is being forced onto
the femur. If the swelling occurs immediately, it may suggest a
ligament tear or fracture. If the swelling arises over a period of many
hours, meniscal or cartilage injuries may be the cause. Giving way or
a feeling of instability of the knee, or popping or grinding in the knee
is associated with cartilage or meniscus tears. Locking is the term
used when the knee joint refuses to completely straighten, plain X-
rays may not be initially needed and imaging of the knee may wait
until a later date. Standing X-rays of the knees may be obtained. An
MRI might be considered to evaluate the ligaments and cartilage
within the knee joint
In Strains of ligament: RICE (rest, ice, compression, and elevation)
with some strengthening exercises and perhaps physical therapy will be
needed. Sometimes the decision for surgery is delayed to see if the
RICE and physical therapy will be effective. Each injury is unique, and
treatment decisions depend on what the expectation for function will
be. As an example, a torn ACL (anterior cruciate ligament) would
usually require surgery in a young athlete or a construction worker, but
the ACL may be treated nonoperatively with physical therapy in an 80-
year-old who is not very active. IN chronic pain during walking uphill
or climbing upstairs & swelling & signs of giving way which are signs of
meniscus injury usually need Arthroscopic menisectomy.MCL,LCL &
PCL alone rarely need surgery in acute stage unless associated with
meniscal or ACL injuries .
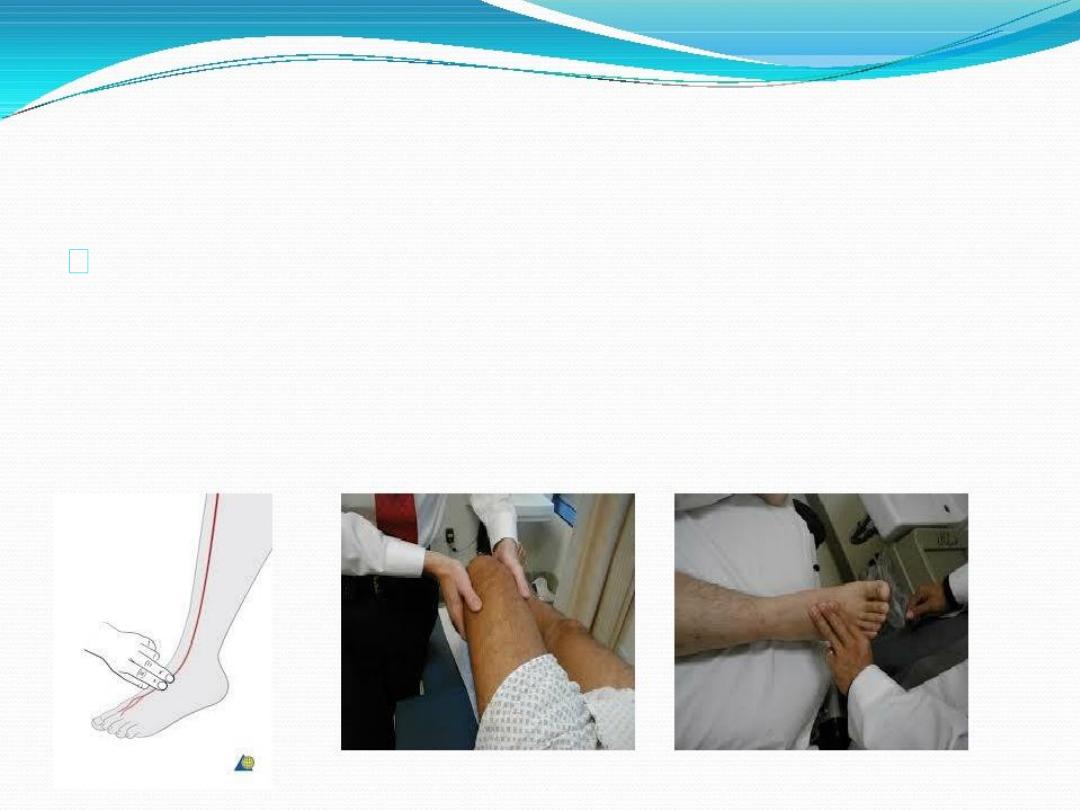
Treatment
X-ray: will be taken to make sure there are no breaks in the bone.
Examination of pulses: Injury to the arteries in the knee is common
with this injury. The doctor will make sure there are pulses in the foot.
An arteriogram (X-ray of the artery): This X-ray may need to be done to
detect injuries to the artery. Some medical centers may also use special
Ultrasound or Doppler (sound wave) machines to assess the blood flow
in the arteries.
Examination of nerves: Nerves also run through the knee, so it is
possible that they may have been damaged. The ability to feel touch
and to move certain muscle groups are the main ways nerves are tested.
Specifically, the ability to move the foot up and down and to turn the
foot inside (inversion) and outside (eversion) are important muscle
movements to examine. Any feeling of numbness is concerning for
nerve injury.
. They usually happen only after major trauma , including falls,
car crashes, and other high-speed injuries. Knee dislocation will
always cause severe pain in the knee. Sometimes, there will be no
feeling below the knee. If the knee relocates, it will become
swollen from fluid in the knee and be painful with any
movement. Very serious symptoms include loss of a pulse below
the knee or loss of feeling or movement below the knee. If a
dislocated knee joint is suspected, there is likely severe ligament
injury. Go to the nearest hospital's emergency department.
Relocation by closed reduction is usually done in emergency
unit by orthopedic doctors.
If an arterial injury is determined to be present, immediate
surgery by a trauma or vascular surgeon to repair the injured
vessel(s ). Immobilization: the entire knee joint will be kept in a
splint or immobilizer. This will keep the knee from bending and
help the tissues to start healing. A knee dislocation almost always
has severe tears and sprains of the ligaments and sometimes has
breaks in the bones of the knee. After swelling has gone down,
the knee may need reconstruction surgery to regain function
1-vascular injury: popliteal artery
2-nerve injury: mostly common peroneal or tibial nerves.
3-Associated fracture femural condyles or shaft or tibial palateu.
4-ligaments injuries .

Late:
1- joint instabilitg
2-joint stiffness
3- Osteoarthritis
Thank you for listening
