Cardiac Lectures Dr. Ahmed Moyed Hussein
Supraventricular tachycardias:The term ‘supraventricular tachycardia’ (SVT) is commonly used to describe regular tachycardia that have a similar appearance on ECG. These are usually associated with a narrow QRS complex and are characterized by a re-entry circuit or automatic focus involving the atria.
Atrioventricular nodal re-entrant tachycardia (AVNRT):
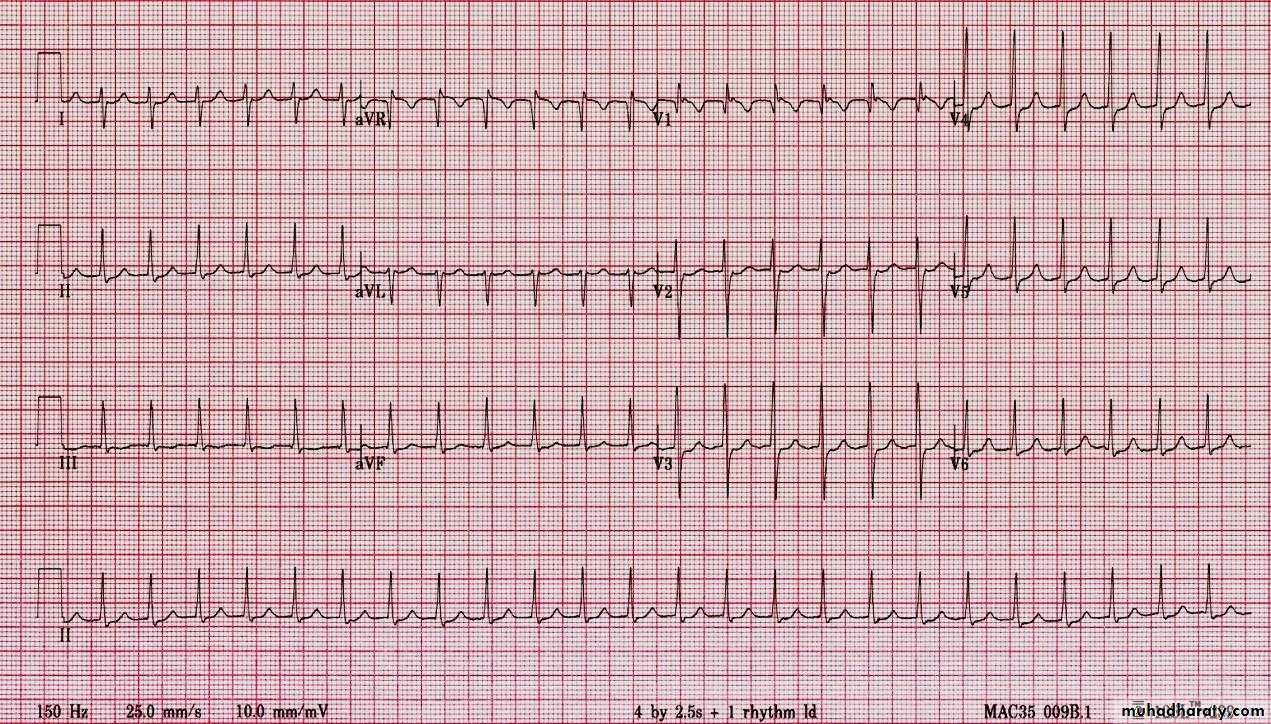
is due to re-entry in a circuit involving the AV node, This produces a regular tachycardia with a rate of 120–240/min. It tends to occur in the absence of structural heart disease and episodes may last from a few seconds to many hours. The patient is usually aware of a rapid, very forceful, regular heart beat and may experience chest discomfort, lightheadedness or breathlessness. Polyuria, mainly due to the release of atrial natriuretic peptide, is sometimes a feature. The ECG usually shows a tachycardia with normal QRS complexes.Fig: SVT
Management:Episode may be terminated by carotid sinus pressure or by the Valsalva manoeuvre (vagal stimulation). Adenosine (3–12 mg rapidly IV) or verapamil (5 mg IV over 1 min) will restore sinus rhythm in most cases. Intravenous β-blocker or flecainide can also be used. In rare cases, when there is severe hemodynamic compromise, the tachycardia should be terminated by synchronized DC cardioversion.
In patients with recurrent SVT, catheter ablation is the most effective therapy and will permanently prevent SVT in more than 90% of cases. Alternatively, prophylaxis with oral β-blocker, verapamil or flecainide may be used.
Wolff–Parkinson–White syndrome(WPW) and atrioventricular re-entrant tachycardia:
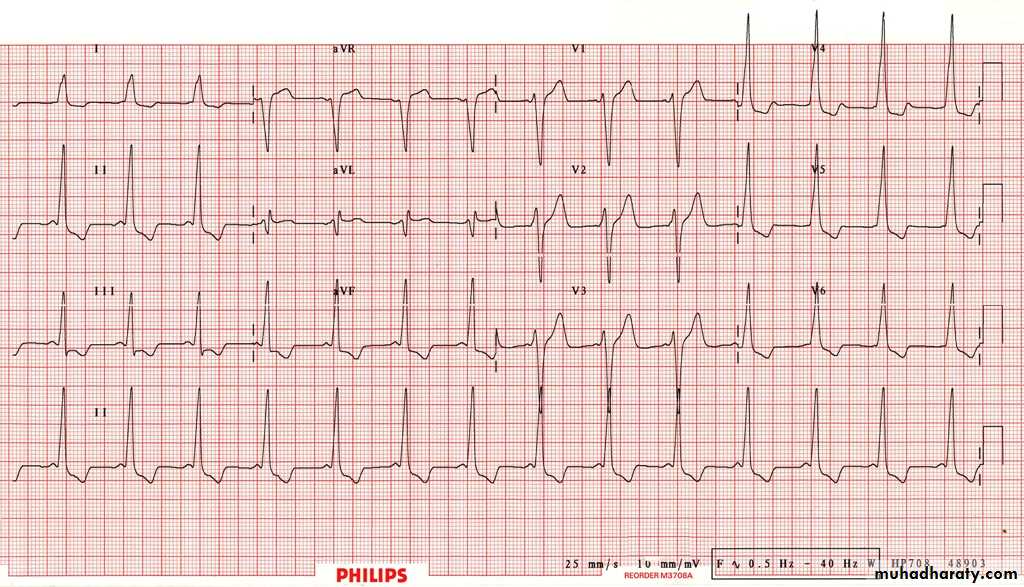
Here, an abnormal band of conducting tissue connects the atria and ventricles. This ‘accessory pathway’ comprises rapidly conducting fibers which resemble Purkinje tissue. Premature ventricular activation via thepathway shortens the PR interval and produces a ‘slurred’ initial deflection of the QRS complex, called a delta wave. As the AV node and accessory pathway have different conduction speeds and refractory periods, a re-entry circuit can develop, causing tachycardia, The ECG during this tachycardia is almost indistinguishable from that of AVNRT.
Carotid sinus pressure or intravenous adenosine can terminate the tachycardia. Catheter ablation is first-line treatment in symptomatic patients and is nearly always curative. Alternatively, prophylactic anti-arrhythmic drugs, such as flecainide or propafenone, can be used to slow conduction in the accessory pathway.
Fig: WPW syndrome, show short PR interval and Delta wave (arrow)
Ventricular tachyarrhythmias:Ventricular ectopic beats (extrasystole , premature beats):
The QRS complexes of ventricular ectopic beats (VEBs) are premature, broad and bizarre. The complexes may be unifocal (identical beats arising from a single ectopic focus) or multifocal (varying morphology with multiple foci). Ectopic beats produce a low stroke volume because left ventricular contraction occurs before filling is complete. The pulse is therefore irregular, with weak or missed beats.
Patients are usually asymptomatic but may complain of an irregular heart beat, missed beats or abnormally strong beats (due to the increased output of the postectopic sinus beat). The significance of VEBs depends on the presence or absence of underlying heart disease.
VEBs are frequently found in healthy people and are more prominent at rest and disappear with exercise. Treatment is not necessary,
unless the patient is highly symptomatic, in which case β-blockers or, in some situations, catheter ablation can be used.
In patients with underlying heart disease VEBs is decreased by management of heart disease.
Fig: multiple PVCs (bigeminy)
Ventricular tachycardia (VT):occurs most commonly in the settings of acute MI, chronic coronary artery disease, and cardiomyopathy. It occurs when there is extensive ventricular disease, such as impaired left ventricular function or a left ventricular aneurysm. It is caused by abnormal automaticity or triggered activity in ischemic tissue, or by re-entry within scarred ventricular tissue.
Patients may complain of palpitation or symptoms of low cardiac output, e.g. dizziness, dyspnea or syncope.
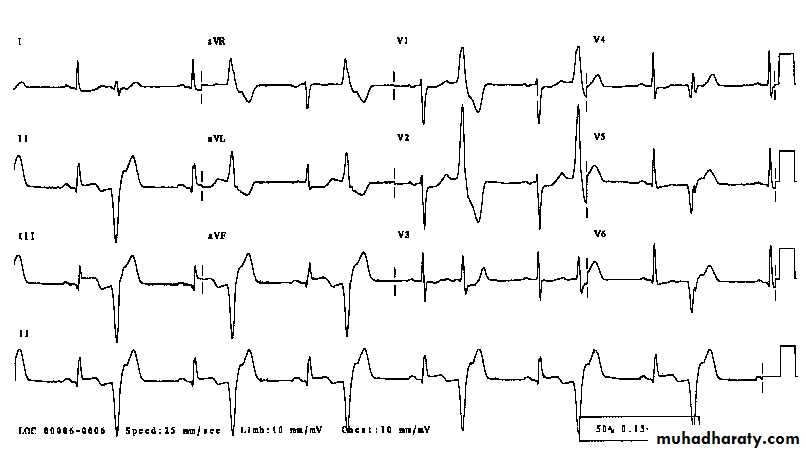
The ECG shows tachycardia and broad, abnormal QRS complexes with a rate of more than 120/min.
Fig: VT
VT may be difficult to distinguish from SVT with bundle branch block or pre-excitation (WPW syndrome). Features in favour of a diagnosis of VT are:History of MI
AV dissociation (pathognomonic)
Capture/fusion beats (pathognomonic)
Extreme left axis deviation
Very broad QRS complexes (> 140 ms)
No response to carotid sinus massage or IV adenosine
Management:
Synchronized DC cardioversion is the treatment of choice if systolic BP is less than 90 mmHg. If the arrhythmia is well tolerated, intravenous amiodarone may be given as a bolus, followed by a continuous infusion. Intravenous lidocaine can be used but may depress left ventricular function, causing hypotension or acute heart failure. Hypokalaemia, hypomagnesaemia, acidosis and hypoxaemia should be corrected.
In patients at high risk of arrhythmic death (e.g. those with poor left ventricular function, or where VT is associated with haemodynamic compromise), the use of an implantable cardiac defibrillator is recommended.
Torsades de pointes (Polymorphic ventricular tachycardia):
This form of polymorphic VT is a complication of prolonged ventricular repolarisation (prolonged QT interval). The ECG shows rapid irregular complexes that oscillate from an upright to an inverted position and seem to twist around the baseline as the mean QRS axis changes.The arrhythmia is usually nonsustained and repetitive, but may degenerate into ventricular fibrillation. During periods of sinus rhythm, the ECG will usually show a prolonged QT interval (> 0.43 s in men, > 0.45 s in women when corrected to a heart rate of 60/min).
Treatment should be directed at the underlying cause. Intravenous magnesium (8 mmol over 15 mins, then 72 mmol over 24 hrs) should be given in all cases.
Fig: polymorphic VT
Ventricular fibrillation and pulseless ventricular tachycardia:
These are the most common and most easily treatable cardiac arrest rhythms. Ventricular fibrillation produces rapid, ineffective, uncoordinated movement of the ventricles, which therefore produces no pulse. The ECG shows rapid, bizarre and irregular ventricular complexes.Defibrillation will restore cardiac output in more than 80% of patients, if delivered immediately. However, the chances of survival fall by at least 10% with each minute’s delay, and by more if basic life support is not given; thus provision of these is the key to survival.