12/6/2017
1

Etiology
Pathogenesis
Clinical manifestation
Investigation
D.Dx.
Treatment
Prognosis
OBJECTS:
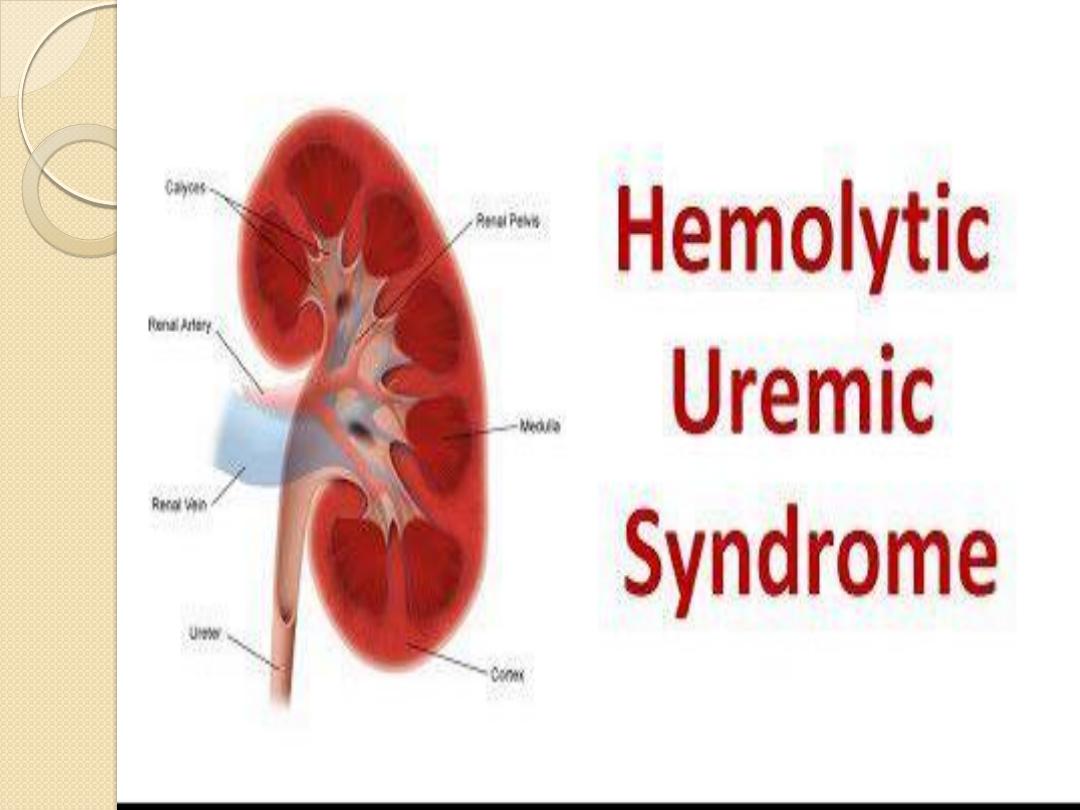
HUS is a common cause of community-
acquired ARF in young children. It is
characterized by the triad of:
microangiopathic
hemolytic anemia
thrombocytopenia,
and renal insufficiency.
12/6/2017
3
Etiology:
HUS can be classified according to etiology as follows:-
• Infection-induced (most common); it include: Verotoxin-producing
E coli (most common 057:H7 type), Shiga toxin-producing Shigella
dysentereriae type 1 (common), Streptococcus pneumoniae (rare),
and HIV (rare).
• Genetic (Atypical) HUS include: Familial AR & AD of undefined
etiology, recurrent, undefined etiology without diarrhea prodrome.
• Diseases associated with microvascular injury include: SLE,
Following BM transplantation, Malignant hypertension.
• Medication-induced include: some immunosuppressant & cytotoxic
medications
12/6/2017
4
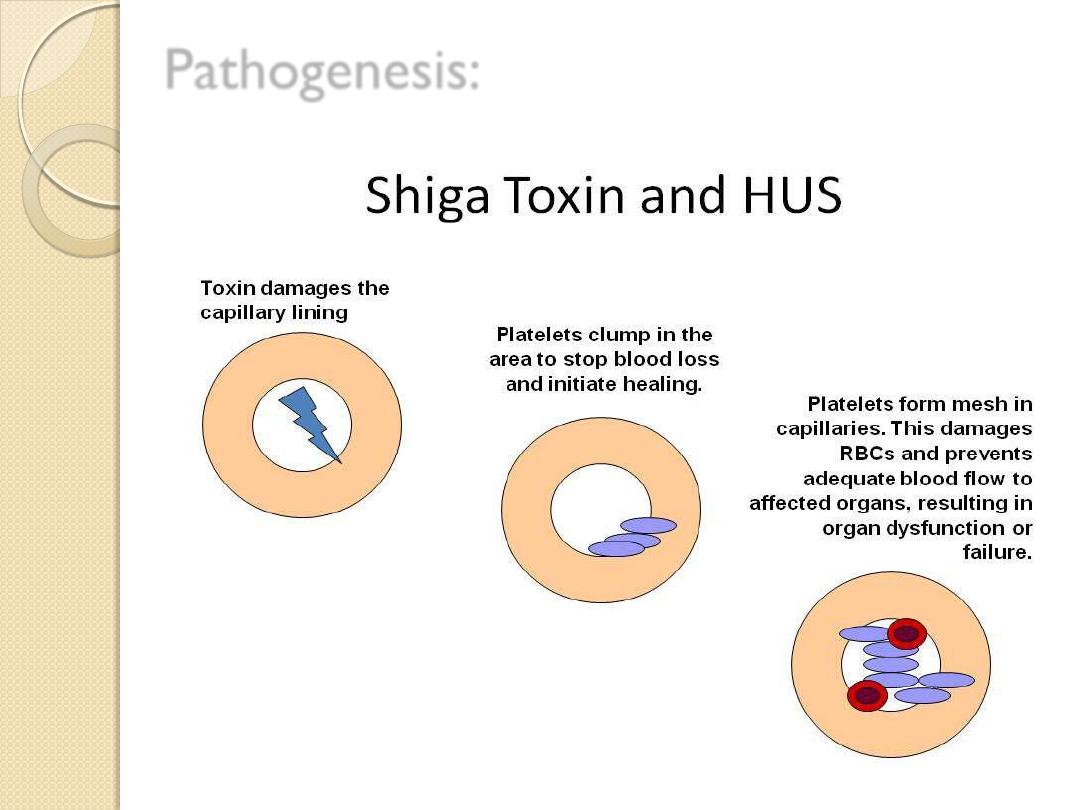
Microvascular injury with
endothelial cell
damage is characteristic of all forms of HUS,
capillary and arteriolar endothelial injury in
the kidney particularly in glomeruli, leads to
localized thrombosis causing a direct decrease
in GFR.
Progressive platelet aggregation in the areas of
microvascular injury results in consumptive
thrombocytopenia.
Microangiopathic hemolytic anemia results
from mechanical damage to red blood cells as
they pass through the damaged and
thrombotic microvasculature
12/6/2017
5
Pathogenesis:
12/6/2017
6
Clinical manifestation:
HUS is most common in
preschool and school-aged
children.
In HUS caused by exotoxin-producing E. coli, onset
of HUS occurs a few days
(as few as 3 days) up to 3
wk. after onset of gastroenteritis with fever, vomiting,
abdominal pain, and diarrhea which is often bloody,
but not necessarily, especially early in the illness.
Following the prodromal illness, a
sudden onset of
pallor, irritability, weakness, lethargy and Oliguria
12/6/2017
7

Patients can develop
petechiae
, but significant or
severe bleeding is rare despite very low platelet
counts.
Patients with pneumococcus-associated HUS
usually are ill with pneumonia and empyema when
they develop HUS.
E.coli is usually transmitted by undercooked
meat, unpasteurized milk , contaminated apple
cidar or bathing in contaminated swimming pool
12/6/2017
8
Investigation:
1.
CBP shows
Hb
is in the range of 5-9gm/dl.
2.
Thrombocytopenia
is an invariable finding in
the acute phase
3.
Leukocytosis
is present
4.
Blood film
:microangiopathic hemolytic anemia
with schistocytes, burr cells, helmet cells and
fragmented RBCs.
5.
Coombs test
is negative.
6.
PT & PTT
are usually normal.
7.
RFT
: Renal insufficiency can vary from mild
elevations in BUN to ARF.
12/6/2017
9
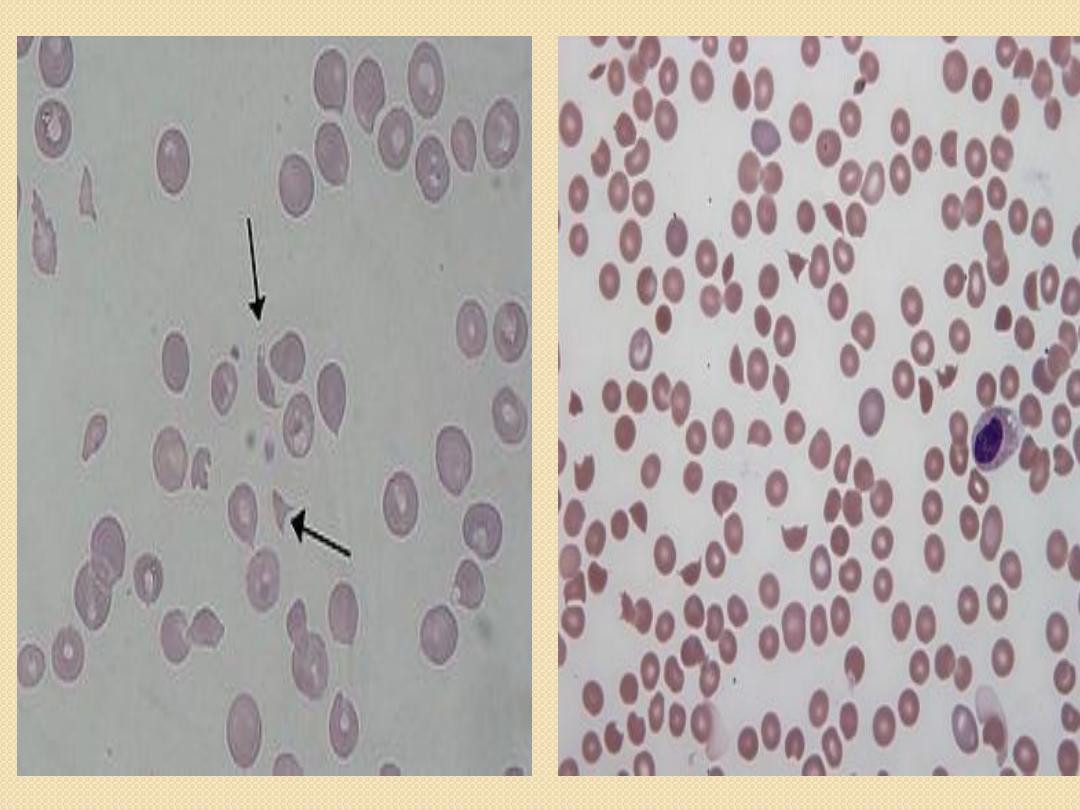
s
schistocytes
12/6/2017
10
D.Dx.
Thrombotic Thrombocytopenic Purpura (TTP)
SLE
malignant hypertension
bilateral renal vein thrombosis
12/6/2017
11
Treatment
I.
Careful management of fluid and electrolytes
e.g. correction of volume deficit, control of
hypertension, and early institution of dialysis if
the patient becomes anuric .plasmapheresis
or FFP has been recommended.
II.
Red cell transfusions are usually required
because hemolysis can be brisk and recurrent
until the active phase of the disease has resolved.
12/6/2017
12
III.
Platelets
should not be administered
,
regardless of platelet count because they are
almost immediately consumed by the active
coagulation and can theoretically worsen the
clinical course.
IV.
Antibiotic therapy
is not recommended
as it
result in increased toxin release, potentially
exacerbating the disease.
12/6/2017
13

PROGNOSIS:
The mortality rate for diarrhea-associated
HUS after careful supportive care has
declined to <5%. Most recover renal
function completely, but of surviving
patients, 5% remain dependent on
dialysis,.
The prognosis for HUS that not
associated with diarrhea is more severe,
with mortality reported ≈20%. The familial
forms of HUS have a poor prognosis
12/6/2017
14

12/6/2017
15
