
Dr.Basma Adel
Fifth grade
2017-2018
12/3/2017
1
At the end of this lecture you
should know:
Epidemiology
Etiology
Pathology
Risk factors of UTI
Clinical manifestation
Investigations
Complications
Treatment
Vesico ureteral reflux
12/3/2017
2
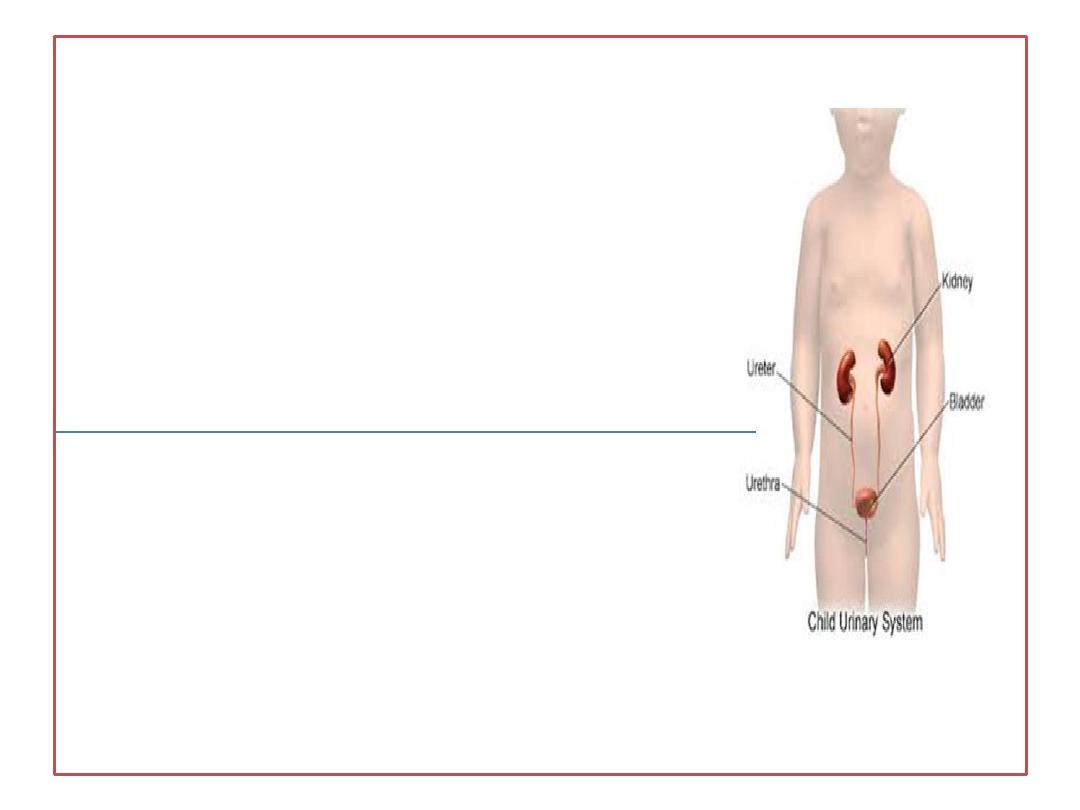
• UTI are
the most common genitourinary
disease of childhood.
The prevalence of UTI at all ages is :
1-3% of girls
1% of boys
.
Below 1 year
≈
male: female 4:1
, especially
among uncircumcised males
but after 1 year
male: female ratio is 1:10.
12/3/2017
3
Etiology:
• UTI is mainly caused by colonic bacteria e.g.
E coli
,
followed by
Klebsiella and Proteus
. Infrequently it caused
by Staphylococcus saprophyticus and enterococcus as
well as to viral infection e.g. adenovirus
Pathology
• Virtually all UTIs are
ascending infections
. The bacteria
arise from the fecal flora and enter the bladder via
urethra.
•
Rarely, in some neonates, renal infection may occur by
hematogenous spread.
12/3/2017
4

12/3/2017
5
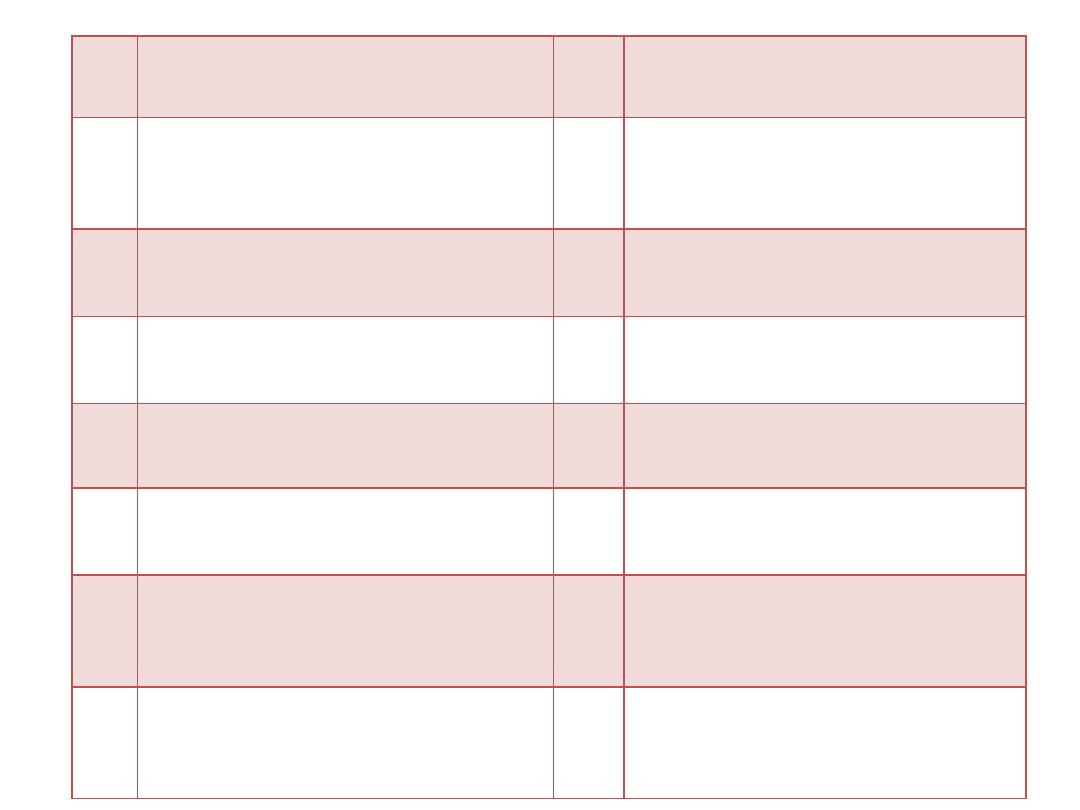
1
Female gender
2
Uncircumcised male
3
Vesicoureteral reflux
4
Voiding dysfunction
5
Obstructive uropathy
6
Neuropathic bladder
7
Urethral instrumentation
8
Constipation
9
Bacteria with P fimbriae
10
Pinworm infestation
11
Tight clothing
12
Toilet training
13
Anatomic abnormality (labial
adhesion)
14
Wiping from back to front in
females
15
Bubble bath
16
Sexual activity& Pregnancy.
12/3/2017
6
Clinical manifestations:
• The symptoms and signs of UTI vary with age:
•
Neonate
:commonly presents with
FTT
feeding problem
diarrhea, vomiting
Fever
hyperbilirubinemia
12/3/2017
7
•
1month-2 year infant
• usually has
non
urinary tract manifestations
• FTT
• feeding problems
• diarrhea
• unexplained fever
• gastrointestinal illness
such as colic, irritability, screaming periods.
12/3/2017
8
•
2-6 years old child
may have GIT symptoms
and classic signs of UTI such
as urgency, dysuria, frequency
and abdominal pain.
•
6-18years old
most commonly
• will have urgency,
• frequency,
• abdominal or flank pain.
12/3/2017
9
There are 3 main types of UTI
• 1. Asymptomatic Bacteriuria
refers to a condition that results in a positive
urine culture without any manifestations of
infection. It is most common in girls.
12/3/2017
10
2. Cystitis (infection of bladder lower UTI)
→
dysuria, urgency, frequency,
suprapubic pain, incontinence,
and malodorous urine.
It
does not
cause fever or
renal injury.
3. Pyelonephritis (upper UTI)
is clinically manifested as
abdominal or flank pain,
fever,
malaise,
nausea,
vomiting,
and
occasionally diarrhea.
12/3/2017
11

Chronic recurrent UTI →
renal scarring
which result in
chronic hypertension
& renal insufficiency
.
12/3/2017
12

Investigations
UTI may be suspected based on :
• symptoms
• urinalysis,
• and urine culture
• Imaging studies
12/3/2017
13
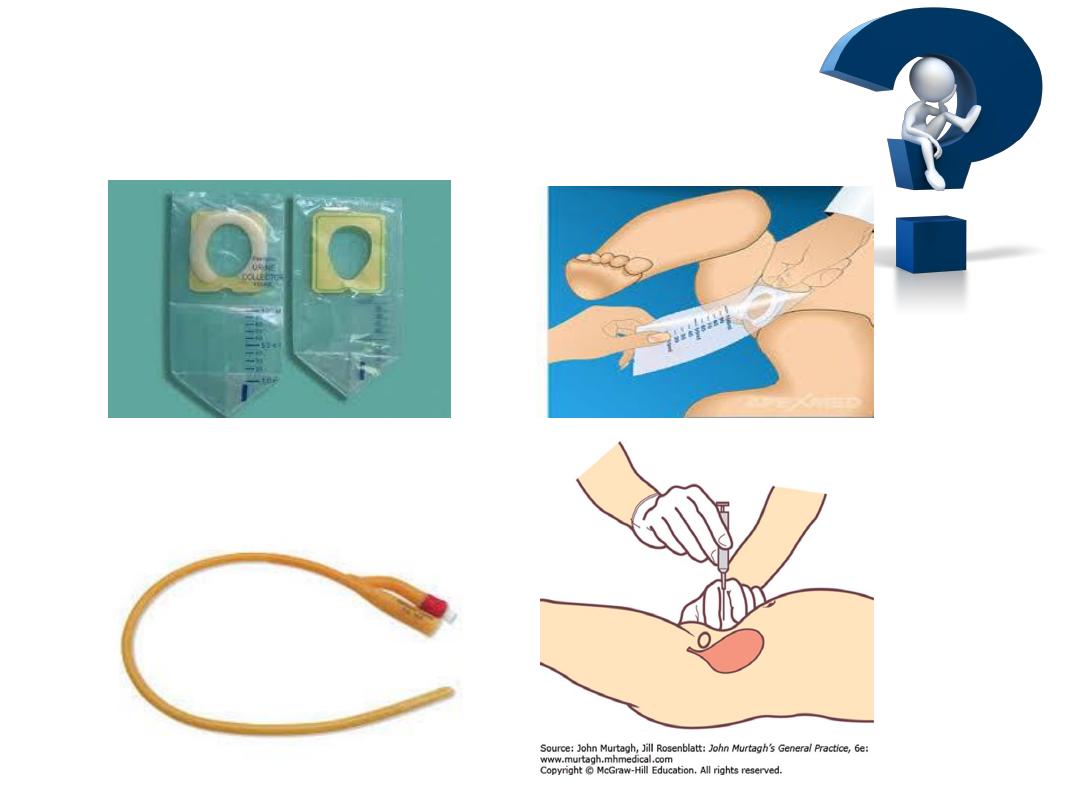
•
In toilet-trained children:
a midstream urine sample usually is satisfactory;
the area should be cleaned before obtaining the
specimen
.
• Children 2-24 months:
a catheterized or suprapubic aspirate urine sample
should be obtained.
Alternatively, the application of an adhesive sealed,
sterile urine bag after disinfection of the skin
can be useful
only if the culture is negative or if a
single uropathogen is identified.
• However, a positive culture can result from skin
contamination
12/3/2017
14
How to obtain a urine sample
12/3/2017
15
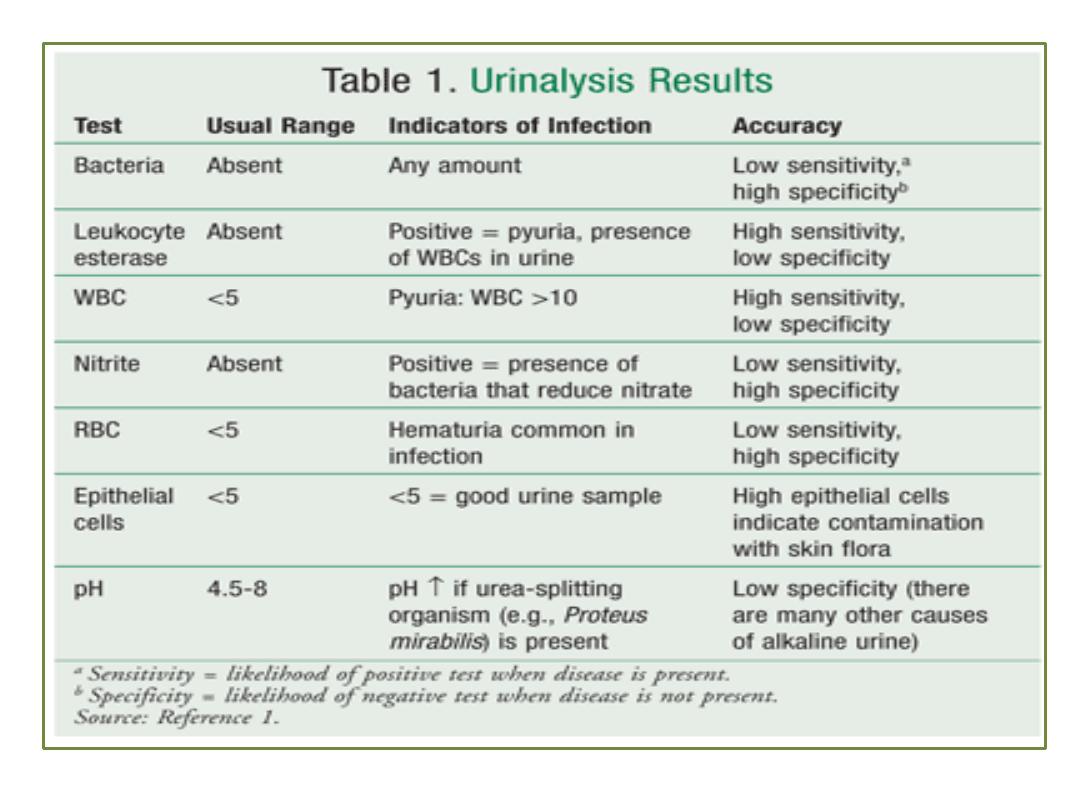
• Pyuria (leukocytes on urine microscopy)
suggests infection, but infection can occur in
the absence of pyuria; this finding is more
confirmatory than diagnostic.
• Nitrites and leukocyte esterase usually are
positive in infected urine.
• Microscopic hematuria is common in acute
cystitis, but microhematuria alone does not
suggest UTI
12/3/2017
16
12/3/2017
17

Sterile pyuria (positive leukocytes, negative
culture) may occur in:
• partially treated bacterial UTIs
• viral infections
• renal tuberculosis
• renal abscess
• urinary obstruction
• inflammation near the ureter or bladder
eg.appendicitis
12/3/2017
18
Urine culture
If the culture (suprapubic or catheter
sample) shows
>50,000
colonies of a single
pathogen regardless of symptoms, or if
there are
10,000
colonies with symptoms,
the child is considered to have a UTI.
In (bag sample), if the urinalysis result is
positive, the patient is symptomatic, and
there is a single organism cultured with a
colony count >
100.000
there is a presumed
UTI
12/3/2017
19
B-CBP in upper UTI, there is leukocytosis
(neutrophilia), ↑ ESR & CRP
C- blood cultures should be drawn before
starting antibiotics if possible as sepsis is
common in pyelonephritis, particularly in infants
and any child with obstructive uropathy
12/3/2017
20
D
-
Imaging studies are used to identify the
anatomical abnormalities ,these include
:-
1. Ultrasound of kidney
is indicated
initially for all
infants
with UTI To exclude obstruction and determine
the size of the kidney, rule out hydronephrosis, renal
abscess .
2.
VCUG
is indicated if the
U/S study is abnormal, the
patient has atypical features, or after a recurrent
febrile UTI.
The timing of VCUG 2-6 wk. after treatment (to
allow inflammation in bladder to resolve to reduce the
incidence of VUR
12/3/2017
21
3.IV pyelography
to evaluate kidney size ,
calyceal blunting ,urethral dilatation.
4.Renal scanning using DMSA
(di-mercapto-
succenic acid) is used to detect renal scars that
usually develop after severe or recurrent upper
UTI.
5.CT scan
can also detect renal scars
12/3/2017
22
Treatment:
• Acute cystitis
should be treated promptly to prevent progression
to pyelonephritis,
a 3-5 day
course of
1) trimethoprim-sulfamethoxazole (TMP-SMX) or
trimethoprim
is effective against many strains of
E. coli.
2)
Nitrofurantoin (5-7 mg/ kg/24 hr. in 3-4 divided
doses)
has the advantage of being active against
Klebsiella and Enterobacter organisms.
3) Amoxicillin (50 mg/kg/24 hr.)
.also is effective as
initial treatment but has a high rate of bacterial
resistance.
12/3/2017
23
• Acute pyelonephritis, a 7-14 day
course of
broad-spectrum antibiotics is preferable.
Children should be admitted to the hospital for IV
rehydration and IV antibiotic therapy
:
i.
dehydrated,
ii. vomiting,
iii. unable to drink fluids,
iv. 1 mo. of age or younger,
v. have complicated infection, or in whom urosepsis is
a possibility
.
12/3/2017
24
1) Ceftriaxone (50-75 mg/kg/24 hr., Not to
exceed 2 g)
2) Cefotaxime (100 mg/kg/24 hr.),
3) Ampicillin (100 mg/ kg/24 hr.) With an
aminoglycoside such as gentamicin (3-5
mg/kg/24 hr. in 1-3 divided doses) is
preferable.
Treatment with aminoglycosides
is particularly effective against Pseudomonas
spp .
• Parenteral treatment with:
12/3/2017
25
4. Oral third-generation cephalosporins such as
cefixime
are as effective as parenteral ceftriaxone
against a variety of Gram-ve organisms other than
Pseudomonas, and these medications are
considered to be the treatment of choice for oral
outpatient therapy.
5.
Ciprofloxacin
is an alternative agent for resistant
microorganisms, particularly Pseudomonas, in
patients older than age 17 yr.
• In some children with a febrile UTI,
intramuscular
injection of a loading dose of ceftriaxone
followed by oral therapy with a third-generation
cephalosporin is effective
12/3/2017
26
Note
:
A urine culture 1 wk. after the termination of
treatment of a UTI ensures that the urine is sterile
• Urologic conditions for recurrent UTIs that might
benefit from long-term prophylaxis include :
neuropathic bladder
urinary tract stasis and obstruction and urinary calculi.
severe vesicoureteral reflux
In a child with recurrent UTIs.
Antimicrobial prophylaxis using
trimethoprim or
nitrofurantoin at 30% of the normal therapeutic dose
once a day. TMP-SMZ, amoxicillin, or cephalexin can also
be effective
12/3/2017
27
Vesico ureteral reflux:
• VUR is a condition in which urine flows from the
bladder into the ureters/kidneys.
• Most children with VUR are asymptomatic
• Reflux increases risk of urinary tract infection or
acute pyelonephritis, so testing for reflux may be
performed after a child has one or more
infections.
• May be congenital or acquired like in Posterior
urethral valves; urethral or meatal stenosis,
bladder instability, neurogenic bladder . UTI may
cause reflux due to the elevated pressures
associated with inflammation.
12/3/2017
28
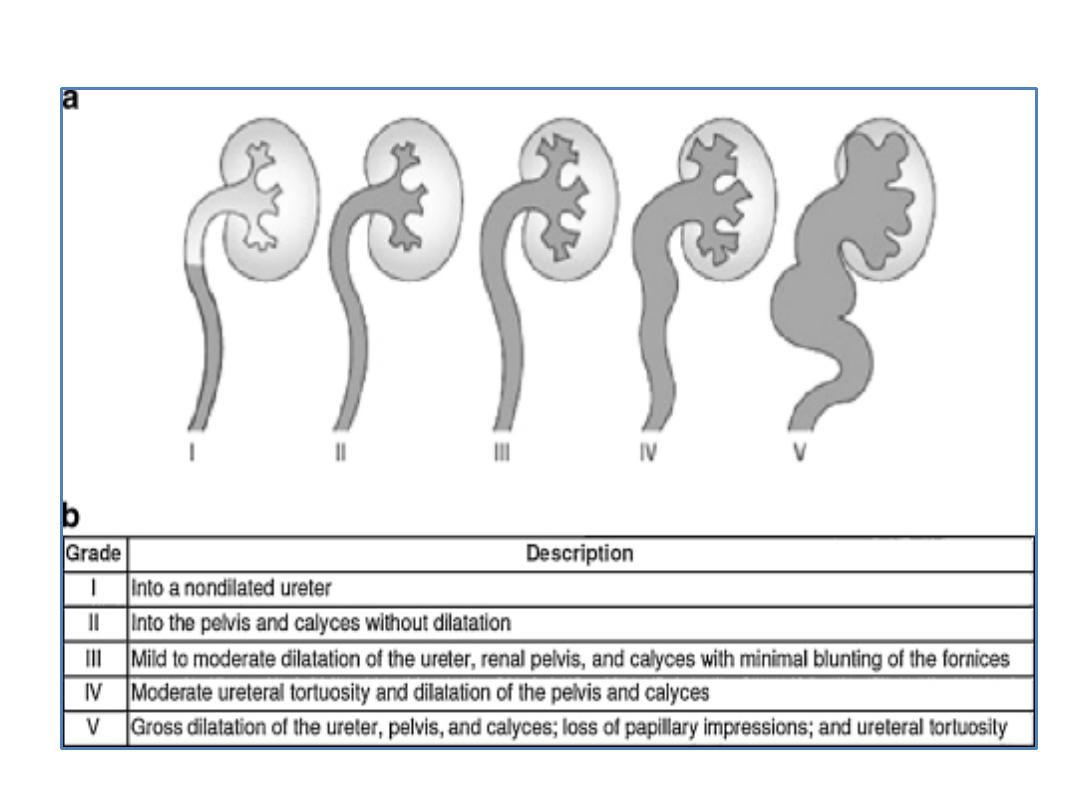
International Classification of Vesicoureteral Reflux
12/3/2017
29
Treatment:
85% of grade I & II cases of VUR will resolve spontaneously.
50% of grade III cases and a lower percentage of higher grades
will also resolve spontaneously
• The goal of treatment is to minimize infections by
prophylactic antibiotics, as it is infections that cause renal
scarring and not the vesicoureteral reflux
• When medical management fails to prevent recurrent UTI,
or if the kidneys show progressive renal scarring then
surgical interventions may be necessary
• Medical management is recommended in children with
Grade I-III VUR. A trial of medical treatment is indicated in
patients with Grade IV VUR . Of the patients with Grade V
VUR surgery is the only option .
12/3/2017
30
1.Types of urine casts and its clinical
significance?
2. Causes of albumin in urine?
12/3/2017
31

12/3/2017
32
