Fetal monitoring during pregnancy and labour
Dr Hiba Ahmed SuhailM.B. Ch. B./F.I.B.O.G.College of medicineUniversity of MosulAntepartum fetal assessment
The goals of antepartum fetal surveillance includePrevention of fetal death.
Avoidance of unnecessary intervention.
• Current techniques employed to forecast fetal well-being , a negative, that is, normal test result is highly reassuring, because fetal deaths within 1 week of a normal test are rare
• Antenatal fetal assessment methods include :
• Clinical assessment
• Maternal perception of fetal movement
• Cardiotocography to assess fetal heart rate pattern
• Ultrasound for Biophysical profile
• Doppler ultrasound study for the fetal and maternal vessels
#CLINICAL ASSESSMENT
Clinical examination in each antenatal visit is the primary and main assessment of fetal wellbeing. This includes detection of :fetal heart sound
- fetal size
- fundal level
- amount of amniotic fluid.
#FETAL MOVEMENTS
Passive un stimulated fetal activity start as early as7 weeks and becomes more sophisticated and coordinated by the end of pregnancy
Physiological factors affect fetal movement
.An important determinant of fetal activity is sleep-awake cycles, which are independent of the maternal sleep-awake state.
If amnionic fluid volume is decreased fetal activity with diminished amnionic volumes restricted uterine space so physically limit fetal movements.
Beyond 36 weeks, there is less rapid movement but normal slow movement
• Pathological diminished of fetal movement is caused by conditions associated with fetal hypoxia
Methods of detection of fetal movement
Maternal subjective perceptionstocodynamometer
visualization with sonography
fetal movement counting protocols
Fetal movement counting protocols have been used perception of 10 fetal movements in up to 2 hours is considered normal The counting can be discontinued for that day after 10 movements.
Or if 10 or more fetal movement per 12-hour period in normal pregnancies.
The decrease or cessation (no fetal movement) of fetal movements has an ominous implication and may be associated with fetal distress or death.
Advantages:
1- Informative and non-invasive.2- Pregnant woman can monitor herself.
3- No cost.
4- Accurate gestational age not required.
Drawbacks:
1. Awareness of the fetal movement is differ from a mother to another.2. Cessation of fetal movement may occur due to intrauterine sleep.
3. Sedation of the fetus occurs if the mother is taking sedatives.
4-Sudden death of the fetus may occur without preceding slowing of the fetal movement
as in abruptio placenta or it may be preceded by increased flurry movements.
#ANTEPARTUM CARDIOTOCOGRAPHY
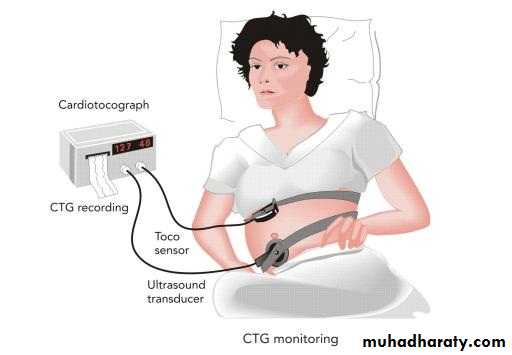
Cardiotocography is a machine used for continuous fetal heart rate tracing to assess fetal well being ,it consist of external ultrasound fetal transducer to monitor fetal heart and external tocodynometer to record uterine activity and applied over the uterusRecording made over 20min
The out put trace consists of 2 lines one trace for fetal heart rate activity and the other for uterine activity
1. Non-stress Test:
Indications:1. Decrease fetal movement( <10/12 hours) or its cessation.
2. Intrauterine growth retardation especially with a major cause as pre-eclampsia.
3. Fetal danger as in antepartum haemorrhage.
4. Biochemical evidence of placental insufficiency
Procedure:
- It is done starting from the 30 weeks of pregnancy.- The electronic fetal monitor is used during pregnancy to record the pattern of fetal heart rate (FHR) and its response to the fetal movements reported by the
mother by pressing a button in her hand.
- The test is carried out for 20 minutes. If fetal movement did not occur the test is
extended for another 20 minutes during which the fetus is stimulated mechanically
Results:
1-Reactive test: 2 or more fetal movements are accompanied by acceleration ofFHR of 15 beats/ minute for at least 15 seconds’ duration.
Reactive test means that the fetus can survive for one week, so the test should be repeated weekly
.2- Non -reactive test: no FHR acceleration in response to fetal movements so
contraction stress test is indicated
2-Contraction Stress Test ( Oxytocin Challenge Test):
It is done after 32 weeks of pregnancy.
- Two transducers are applied to the mother’s abdomen; one to record the FHR
pattern and the other to record the uterine activity.
- Three uterine contractions per 10 minutes are induced by:
IV oxytocin drip starting with 0.5mU/ minute and doubled gradually
Contractions stress test interpretation
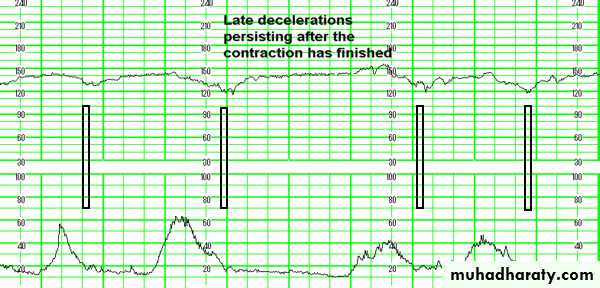
Negative: no late or variable decelerations( in healthy fetus )• Positive: late decelerations following contractions
( in uteroplacental insufficiency).
The tests repeated on a weekly basis.
Disadvantage it required 90 minutes to complete.
Results:
Positive test: consistent and persistent late deceleration of FHR, so placentalinsufficiency is diagnosed and delivery by caesarean section is indicated..
Negative test: late deceleration does not occur with uterine contractions. It denotes that the fetus can survive safely for one week when it should be
repeated
Contraindications
1- Threatened preterm labour.2- Placenta praevia.
3- Rupture of membranes.
4- Previous classical C.S.
5- Multiple pregnancy
#BIOPHYSICAL PROFILE
Biophysical components assessed, which include:
(1) Fetal heart rate acceleration
(2) Fetal breathing
(3) Fetal movements
(4)Fetal tone
(5) Amnionic fluid volume.
Normal variables were assigned a score of 2 each and abnormal variables, a score of 0.
The high score possible for a normal fetus is 8- 10.
Below 6 consider abnormal .
These tests require 20 to 30 minutes of examiner time.
It is valid after 26 weeks.
Score 0
Score 2Variable
Less than 30 seconds in 30 minutes of
observation
Last for 30 seconds in 30 minutes of observation.
Fetal breathing
movements
Less than 3 movements
3 or more discrete body or limb movements within
30 minutes
Fetal movements
Not observed
One or more episodes of limb extension with return
to flexion within 30 minutes.
Fetal tone
Non-reactive
Reactive.
Non-stress test{FHR}
Largest pocket measures less than 1 cm in 2
perpendicular planes
One or more amniotic fluid pockets measures 1 cm
or larger in 2 perpendicular planes
Amniotic fluid volume
# DOPPLER VELOCIMETRY
Doppler ultrasound is a noninvasive technique to assess blood flow
Three fetal vascular circuits.
■ Umbilical Artery Velocimetry(fetal )
Doppler ultrasound flow of the umbilical artery is reduced in pregnancies complicated with fetal growth restriction.
■ Middle Cerebral Artery(fetal )
Doppler velocimetry of the middle cerebral artery (MCA) is useful for detection and management of fetal anemia as it increase in fetal anaemia
■ Ductus Venosus(fetal )
The use of Doppler ultrasound to assess the fetal venous circulation is predictor of perinatal hypoxemia(reduce flow ).
■Maternal Uterine Artery
Doppler of uterine artery most helpful in assessing pregnancies at high risk of complications related to uteroplacental insufficiency assessment at 22 to 24 weeks. detect the risk of development of abruption, preeclampsia, or fetal-growth restriction
Intrapartum fetal assessment
A healthy term fetus is usually able to withstand the journey of a normal labourWith each contraction, placental blood flow and oxygen transfer are temporarily interrupted and a fetus that is already compromised before labour will become increasingly so.
Insufficient oxygen delivery to the fetus causes a switch to anaerobic metabolism and results in the generation of lactic acid and hydrogen ions.
In excess, these saturate the buffering systems of the fetus and cause a metabolic acidosis which, in the extreme, can cause neuronal damage and permanent neurological injury, even intrapartum fetal death
Fetal assessment in labour
1-Observation of the colour of the liquor - fresh meconium staining and heavy bleeding are markers of potential fetal compromise2. Auscultation of the fetal heart either by
intermittent auscultation of the fetal heart using a Pinard stethoscope or a hand-held Doppler ultrasoun
Continuous external fetal monitoring (EFM) using cardiotocography (CTG).
3. continuous internal fetal monitoring using fetal electrode .
4 . fetal scalp blood sampling (FBS).
1. Monitoring of the fetal heart rate.
2. Monitoring of the uterine contractions.
3. Fetal blood sampling
Intermediate auscultation
In the low risk situation, Intermittent auscultation, is often advocated.employing either by:
• Auscultation of fetal heart rate by Pinnard fetal stethoscope.
• hand-held Doppler (sonocaid).
• CardioTocoGraphy (CTG)
• Early on in the initial assessment. It should be listened for a minute, immediately after a contraction. This should be repeated every 15 minutes during first stage, and every 5 minutes in second stage.
Continuous auscultation
Fetal electrocardiography (ECG):1. External: by external electrodes applied to the mother’s abdomen
2-Internal: - by an internal electrode applied to the fetal scalp after rupture of membranes while the cervix should be one or more cm dilated
• Most of woman will also have continuous electronic fetal monitoring (EFM) throughout labour, using the CTG. intermittent auscultation maybe change to continuous EFM if the following events occur during labour:
• Meconium stain in liquror
• Abnormal fetal heart rate detected by auscultation
• Maternal pyrexia
• Fresh vaginal bleeding
• Augmentation of contraction with oxytocin
MONITRORING OF UTERINE CONTRACTIONS
(TOCOGRAPHY)
(I) External
An external transducer is applied to the mother’s abdomen close to the fundus transmitting the strength,
frequency and duration of uterine contractions onto a paper strip record.
(II) Internal
A fluid-filled catheter is introduced into the uterus after rupturing the membranes. The intrauterine
pressure is transmitted to the catheter then to a transducer giving electrical signals expressing the exact
pressure in mmHg.
1- External fetal heart monitoring
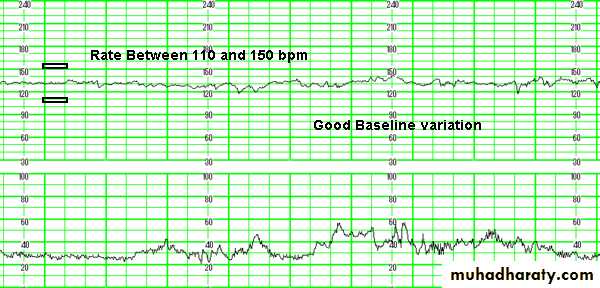
(Intrapartum Cardiotocography)features of a normal fetal heart rate pattern
The features of a normal fetal heart rate pattern include(features )A baseline rate of between 110 and 150bpm (beats per minute),
A baseline variability of between 5 and 25 bpm,
The absence of decelerations.
Presence of acceleration
Classification of CTG
Each feature can be described as 'reassuring', 'non-reassuring' or 'abnormal'Normal CTG all four features are reassuring then the CTG is considered ‘reassuring '
Suspicious CTG If one feature is non-reassuring (and the other three are reassuring) nonreassuring
Abnormal if there are two or more non-reassuring features, or any abnormal features, then the CTG is 'pathological'.
A- Base line fetal heart rate activity
With increasing fetal maturation, the heart rate decreases. approximately one beat/min per week . corresponds to maturation of parasympatheticThe average fetal heart rate is considered the result of balance between accelerator sympathetic system and decelerator parasympathetic system influences on pacemaker cells of the fetal heart .
At term it is ranging from 110-150 bpm
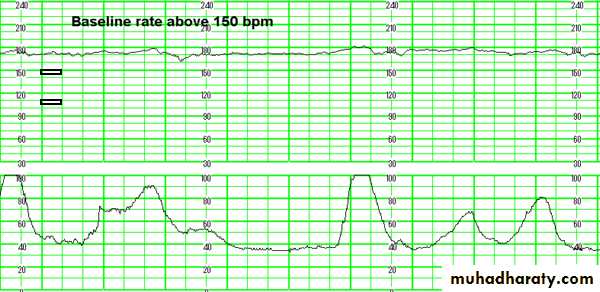
Tachycardia
Fetal tachycardia is defined as a baseline heart rate is greater than 150 bpm maternal causesFever from infections
Chorioamnionitis
Thyrotoxicosis
Drugs parasympathetic (atropine )or symmpathomemic drugs (salbutamol )
Fetal causes
Prematurity
Fetal compromise
Cardiac arrhythmias
Fetal sepsis.
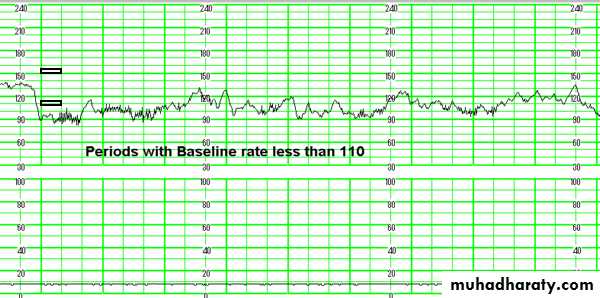
Bradycardia
If the baseline fetal heart rate less than 110 beats/minFetal hypoxia
• Causes of fetal bradycardia
• FETALfetal acidemia.
Cardiac Arrhythmia
congenital heart block.
fetal hydrops.
Hypothermia
• MATERNAL
analgesic drugs given during labor narcotics, betablocker barbiturates.
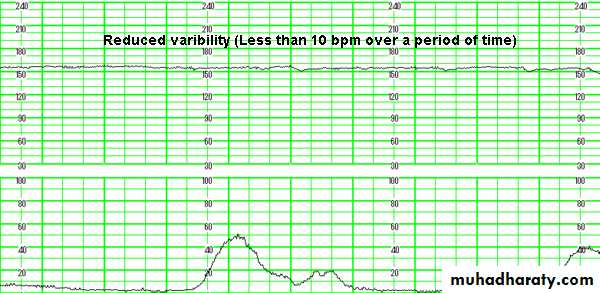
B-Beat-to-Beat Variability( baseline variability)
It regulated by the autonomic nervous system that is, a sympathetic and parasympathetic mediated via the sinoatrial node
Is defined as fluctuation in the fetal heart rate base line
The mean FHR of baseline variability is between 5 -25bpm during a 10-min
Reduced baseline heart rate variability is the single most reliable sign of fetal compromise. it is considered abnormal when there is loss of variability which appears as a smoothing out or flattening of the FHR trace, which could be due to:
• Drug suppressing fetal CNS (narcotic and anesthetic drugs).
• Prolonged fetal hypoxia.
• severe fetal anaemia.
• preterm fetus variability is normally reduced
C-Acceleration
• A visually apparent increase in the heart rate basal line —15 bpm above baseline, with a duration of _ 15 secPresence of 2 or more acceleration in 20 -30 min trace define it as reactive ( non hypoxic fetus )
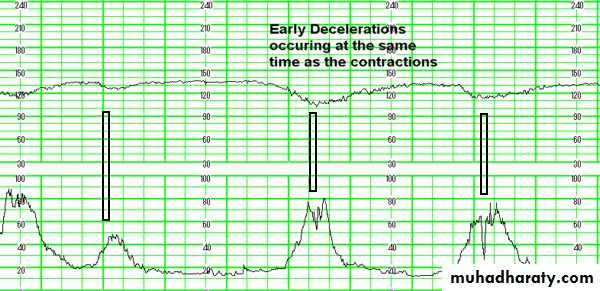
D-Deceleration
Transiet reduction in the fetal heart rate base line of 15 beat or more of more than 15 seconds it divided in to :Early deceleration caused by head compression during labour
Late deceleration due to uteroplacental insufficiency
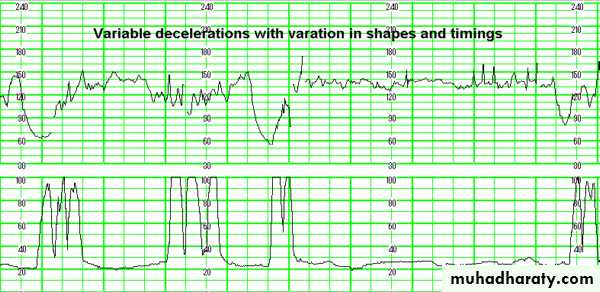
Variable deceleration caused by umbilical cord occlusion.
Poor quality of a CTG recording is sometimes occur because of
• fetal position interfere with correct application of the abdominal conductor on the correct site for better auscultation• Maternal obesity.
• Change in maternal position during labour
Management of abnormal CTG
Any reversible causes of that fetal abnormality must be considered and treated eg severe uterine contraction , change in maternal positionThen further assessment of the fetus made with fetal blood sampling.
If fetal blood sampling difficult or there is an ominous sign of fetal distress by fetal blood sampling then the baby should be delivered without delay.
2-Internal fetal monitoring (fetal electrode)
2-Internal fetal monitoring (fetal electrode)
A fetal scalp electrode may overcome this problem. It is fixed into the skin of the fetal scalp and picks up the fetal heart rate directly.to assess fetal heart rate and uterine contraction
It is not affected by change in maternal position
It rarely causes any harm to the fetus but
It requires:
certain degree of cervical dilatation to be fitted
the membranes to be ruptured
Contraindications to internal fetal heart rate monitoring.
Certain maternal infections, including human immunodeficiency virus (HIV), herpes simplex virus, hepatitis B virus, and hepatitis C virus,Fetal bleeding tendency.
Complications of Electronic
Fetal MonitoringInjury to the fetal scalp or breech by the electrode is rarely the eye in case of a face presentation— a fetal vessel in the placenta may be ruptured by catheter placement
Severe cord compression from entanglement with the catheter.
Penetration of the placenta, causing hemorrhage uterine perforation during catheter insertion,
Both the fetus and the mother may be at increased risk of infection as the consequence of internal monitoring. Scalp wounds infection and Puerperal infection
3- Fetal Scalp Blood Sampling
3- Fetal Scalp Blood Sampling
Measurements of the pH in capillary scalp blood help to identify the fetus in serious distress. After rupturing the membrane, a special guarded needle is introduced through an amnioscope to take adrop of scalp blood for detection of its pHThe pH of fetal capillary scalp blood is usually greater than 7.25,
If the pH is between 7.20 and 7.25, the pH measurement is repeated within 30 minutes.
If the pH is less than 7.20 or less denotes acidosis, and the mother should be delivered
The benefits for scalp pH testing are fewer cesarean deliveries for fetal acidemia.