Neonatology
The neonate
The baby in the first 4 weeks of life is called a neonateResuscitation
Babies fall into one of three categorieswithin a minutes of birth:
Well, healthy and vigorous. The child has a good respiratory effort, is pink centrally, and the heart rate is >100 bpm.
This infant can be wrapped up in a warm towel and given back to his mother. Do not suck him out; this risk producing a vagal bradycardia and cools him.
Cyanosed, poor respiratory effort, with or without a heart rate <100 bpm:
Dry the baby and place him under a radiant heat source wrapped in a warm, dry towel. Drying often provide enough stimulation to induce breathing, but gentle rubbing can also be used. If there is no response, begin active resuscitation using inflation breath via a bag and mask
Pale, apnoeic or terminal gasp, with absent heart beat or profound bradycardia (<60 bpm):
These babies are usually completely floppy. This baby is in need of prompt resuscitation and will not recover without it.
Dry him quickly, place him on the resuscitation surface in a warm, dry towel and call for help.
Initiate basic resuscitation with mask ventilation.
If the heart rate remains < 60 bpm, commence chest compressions.
If there is not a rapid response, proceed to intubation as soon as a person with a necessary skill arrives
The functional status and grade of maturity of the newborn are evaluated with:
Apgar score.Ability to maintain the stable temperature.
Presence of the newborns reflexes.
Sufficient levels of movement activity and emotional reactions.
Newborns maturity signs according to clinical features and special tables.
6
The Apgar score
Assessment (and reassessment) is vital to a successful outcome.Apgar score are carried out at 1 minute and 5 minutes of life. Further score may be carried at 5 minute intervals depending on subsequent progress
Five factors are used to evaluate the baby's condition and each factor is scored on a scale of 0 to 2, with 2 being the best score:
• activity and muscle tone
• pulse (heart rate)
• grimace response (medically known as "reflex irritability")
• appearance (skin coloration)
• respiration (breathing rate and effort)
• Apgar Scoring
•• Apgar Sign
• 2• 1
• 0
• Heart Rate(pulse)
• Normal (above 100 beats per minute)
• Below 100 beats per minute
• Absent(no pulse)
• Breathing(rate and effort)
• Normal rate and effort, good cry
• Slow or irregular breathing, weak cry
• Absent (no breathing)
• Grimace (responsiveness or "reflex irritability")
• Pulls away, sneezes, or coughs with stimulation
• Facial movement only (grimace) with stimulation
• Absent (no response to stimulation)
• Activity(muscle tone)
• Active, spontaneous movement
• Arms and legs flexed with little movement
• No movement, "floppy" tone
• Appearance(skin coloration)
• Normal color all over (hands and feet are pink)
• Normal color (but hands and feet are bluish)
• Bluish-gray or pale all over
Normally the Apgar score is of 7 to 10. Infants with a score between 4 and 6 have moderate depression of their vital signs while infants with a score of 0 to 3 have severely depressed vital signs and are at great risk of dying unless actively resuscitated.
WHAT CAUSES A LOW APGAR SCORE?
• Fetal distress due to hypoxia• Maternal anaesthesia or recent analgesia.
• Preterm infant.
• Difficult or traumatic delivery.
• Excessive suctioning of the pharynx after delivery.
• Severe respiratory distress.
Note that fetal distress due to hypoxia during labour is only one of the many causes of neonatal asphyxia.
It is important to always try and find the cause of a low Apgar score.
There is good evidence that prolonged depression of the Apgar score is associated with death or major neurological disability
Deliveries at which a trained neonatal resuscitator should be present
• Preterm deliveries• Vaginal breech deliveries
• Thick meconium staining of the amniotic fluid
• Significant fetal distress
• Significant antepartum haemorrhage
• Serious fetal abnormality (e.g. hydrops, diaphragmatic hernia)
• Rotational forceps or vacuum deliveries
• Caesarean section – unless elective and under regional anasthesia
• Multiple delivery
Care of the normal term newborn baby
A suggested order of examination is as follows
• Ask the mother about any antenatally diagnosed problems that may need follow up, and any family problems (deafness, dislocation of hips). Check for risk factors that predispose to neonatal sepsis, such as pyrexia in labour.• Remove the baby clothes except the nappy; look at the skin.
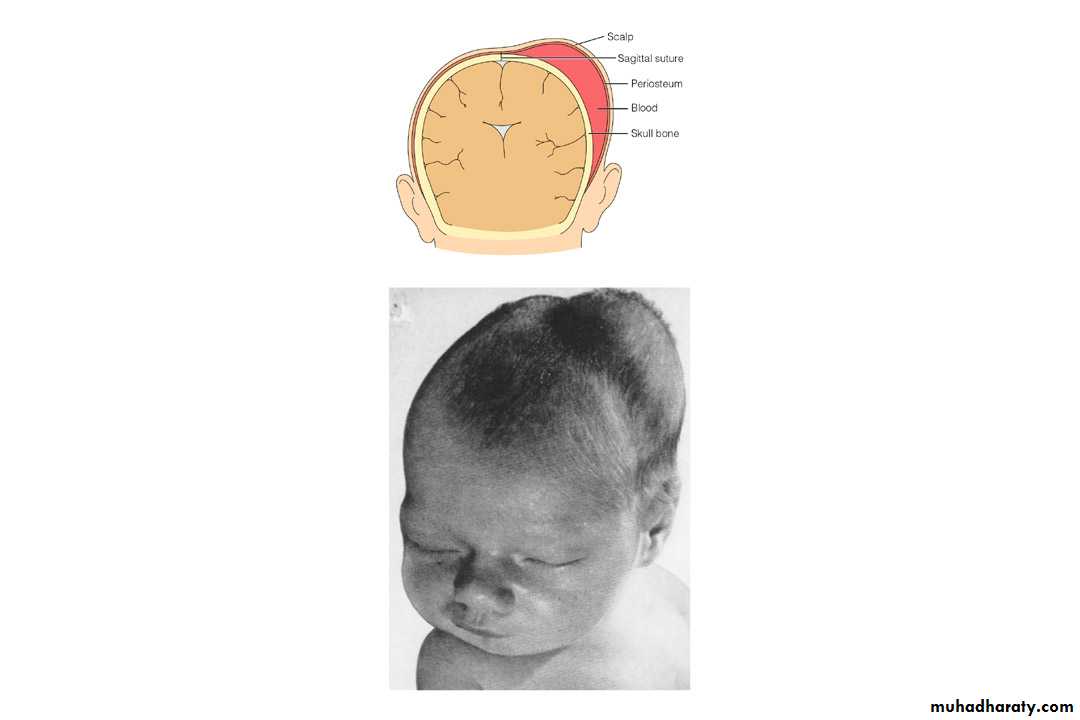
• Feel the anterior fontanel for tension; palpate the sutures (craniosynostosis is a disorder with premature fusion of the sutures); check the scalp for swellings (a cephalhaematoma is the most common).
Cephalhematoma is a collection of blood between the surface of a cranial bone and the periosteal membrane.
Not crossing suture line
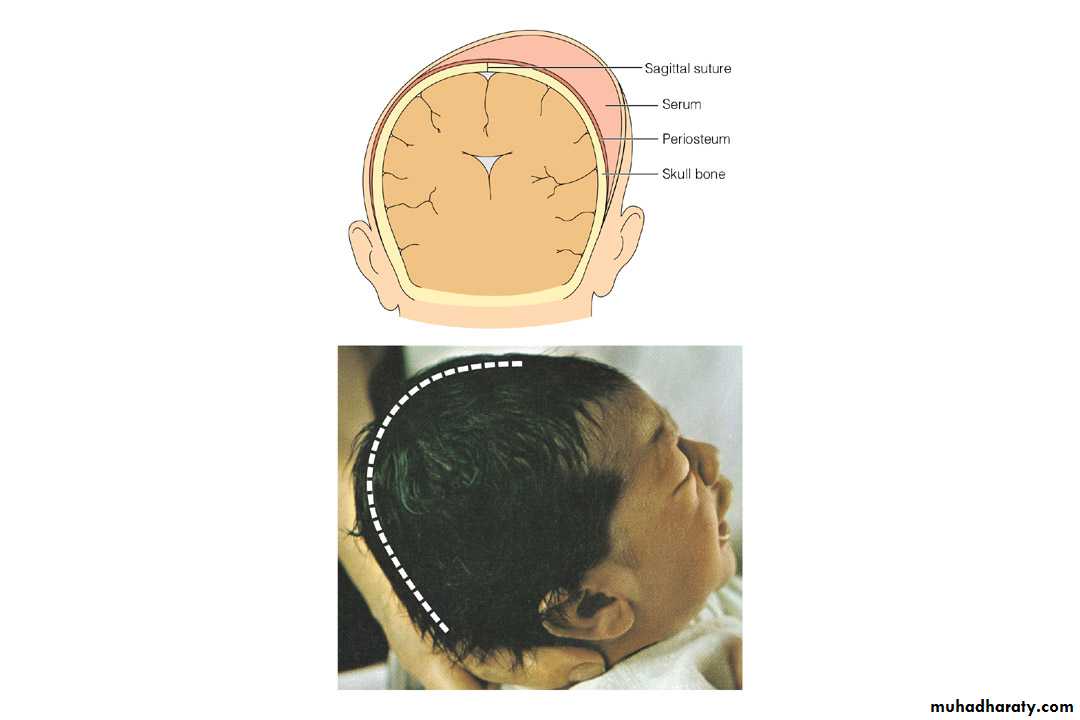
Caput succedaneum is a collection of fluid (serum) under the scalp.
Crossing suture line• Measure the head circumference
17
Look at the face for colour (cyanosis/ pallor / jaundice).
Listen to the heart and estimate the heart rate – normally 110 – 150 bpm, but can drop to 80 bpm in sleep.Count the respiratory rate – normally <60 breaths per minute.
Palpate the abdomen, feeling for masses, including large bladder or kidneys.
Examine the eyes, checking that it is possible to obtain a red reflex using an ophthalmoscope to exclude cataract.
19
Congenital Cataracts
Examine the ear, nose and mouth (cleft palate).
Examine the neck including clavicleExamine the arms, hand, legs and feet.
Remove the nappy.
Feel for femoral pulses.
Examine the genitalia and anus
Turn the baby to the prone position and examine his back and spine; assess tone.
Return the infant to the supine position and evaluate the central nervous system.
Examine the hips
The aims of the neonatal examination
Diagnosis of congenital malformations (present in about 10 – 15 per 1000 babies).
Diagnosis of common minor problem with advice about management or appropriate reassurance if no intervention is indicated (e.g. Mongolian blue spot, jaundice, naevi)
Continuing screening, begin antenatally, to identify those babies who should be offered specific intervention, e.g. hepatitis vaccination.
Health education advice, e.g. regarding breast feeding, cot death prevention, immunization
General parental reassurance
Danger signs in the well baby nursery
Temperature instability.A change in activity, including refusal to feed or having to be wakened for feeds.
Unusual skin colour, mottling.
An abnormal heart rate or respiratory rate, including grunting or fast breathing.
Apnoea.
Excessive jitteriness or abnormal stereotyped, repetitive movement patterns.
Delayed stooling (beyond 48 hours) or completely dry nappies.
Abdominal distension, green vomit
Odd lumps or swelling
Lethargy, floppiness; paucity of movement, excessive sleeping.
Common neonatal complications presenting in the first 24 hours
Transient tachypnoea of the newborn:
Is the commonest respiratory disease of term infant.
The disease is due to delayed clearance of lung liquid and is much more common after caesarean section delivery, particularly without labour.At term, the incidence falls between 37 and 40 weeks.
The baby will have grunting (noise made by forced expiration against closed epiglottis) and tachypnoea
These signs usually appear within the first few hours after birth and settle within 24 – 48 hours.
It must be remembered that this is a diagnosis of exclusion. More serious condition such as sepsis or pneumothorax should be excluded.
Fortunately, the disease is usually mild, but sometimes requires intubation and ventilation, with the associated risk of complications.
• Hypoglycemia
• The importance of hypoglycemia is to identify and treat the ‘at –risk’ infant. Examples include:• Infants with intrauterine growth restriction
• Infants of diabetic mothers
• Preterm infants
• Infants who have suffered fetal distress in labour (infants with perinatal asphyxia)
• Infants who are ‘large for dates’ - possibility of undiagnosed maternal gestational diabetes
• In these groups, a blood glucose <2.6 mmol/L is generally accepted to indicate hypoglycemia.
• Signs of hypoglycemia in the newborn are vague and include apathy/ floppiness, apnoea, excessive jitteriness. These non specific signs can also be due to sepsis.
• Hypothermia:
• This can be defined as a rectal temperature <36°C.• It is most commonly seen in:
Growth restricted babies
Preterm small infants
As part of the clinical features in the sick infants
The septic infant may also present with hypothermia rather than pyrexia
• Hypothermia can cause significant morbidity:
• Infants are lethargic and feed poorly• More seriously, hypothermia is associated with hypoglycemia, metabolic acidosis and respiratory distress
Perinatal asphyxia
• Neonatal asphyxia is defined as failure of the infant to cry or breath well after delivery.• Perinatal asphyxia occurs when a lack of oxygen and acidosis cause organ impairment.
• Deprivation of the oxygen to the brain can occur in two ways:
• hypoxaemia – a reduction in the amount of oxygen in the blood.• Ischaemia – a reduction in the amount of blood perfusing the brain.
• The majority of cases occur in the intrapartum period.
Features include
• Fetal distress
• Birth depression (low Apgar score require ressuscetation
• Metabolic acidosis on cord blood or early neonatal sample
• Seizures (the hallmark of this condition)
• Renal impairment (blood in the urine and a low urine output)
• Alteration of central nervous system state – the baby is not normally conscious between seizures, but is irritable or lethargic with abnormal primitive reflex
Criteria that define an acute intrapartum event sufficient to cause cerebral palsy
Essential criteria (must meet all four):• metabolic acidosis in fetal umbilical artery: pH < 7.0 and base deficit > 12 mmol/L
• early onset of neonatal encephalopathy born at or > 34 weeks’ gestation
• CP of the spastic quadriplegic or dyskinetic type
• exclusion of other identifiable etiologies
Criteria that collectively suggest intrapartum timing but are non-specific to asphyxial insults:
• Sentinel (signal) hypoxic event immediately before or during labor.
• Sudden and sustained fetal bradycardia or absence of FHR variability with persistent late or variable decelerations, when pattern was previously normal.• Apgar 0–3 beyond 5 minutes.
• Onset of multisystem organ involvement within 72 hours.
• Early neuroimaging with evidence of acute non-focal cerebral abnormality
35
Thank you