Anatomy of small
Small intestine1-pylorus------ ileocaecal valve
2-7 m length( duodenum, jejunum, ileum)
3-anteriorly omentum and ant abdominal wall, posteriorly it is fixed to vertebral column by mesentry
4-jejunum 2/5, thicker wider, more vascular, circular fold of mucous membrane (valvulae coniventes). Ileum contains peyer,s patches
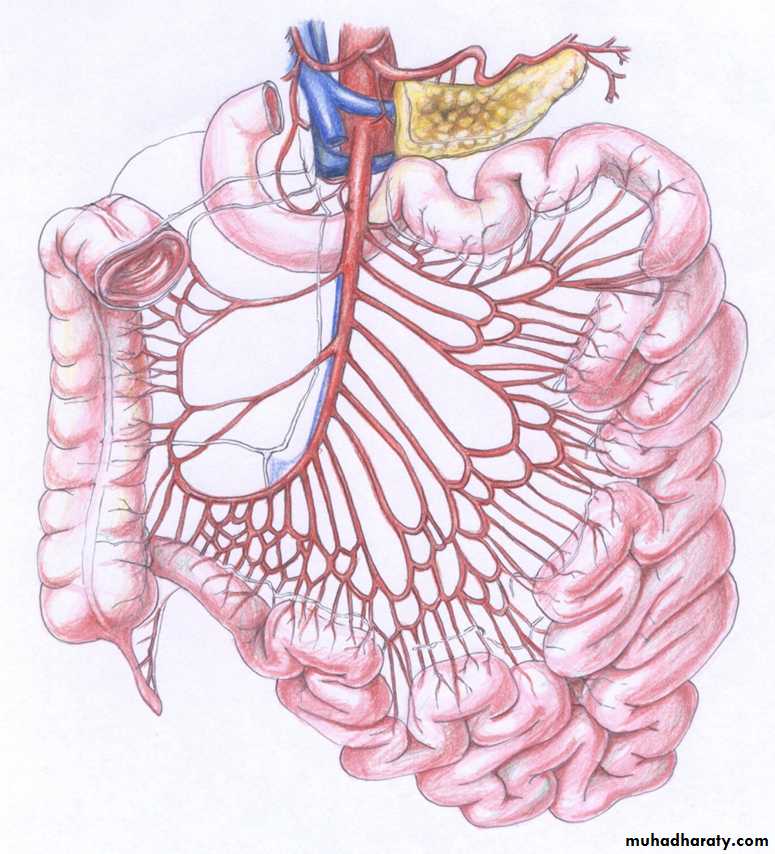
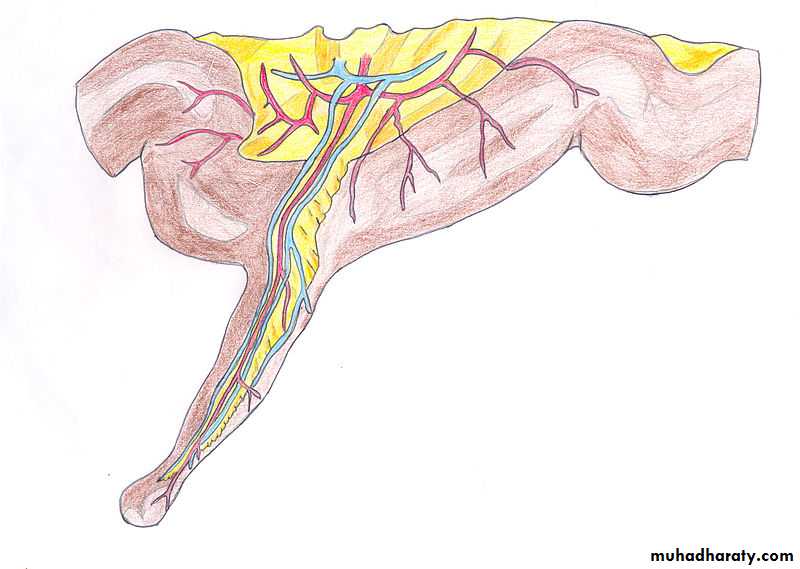
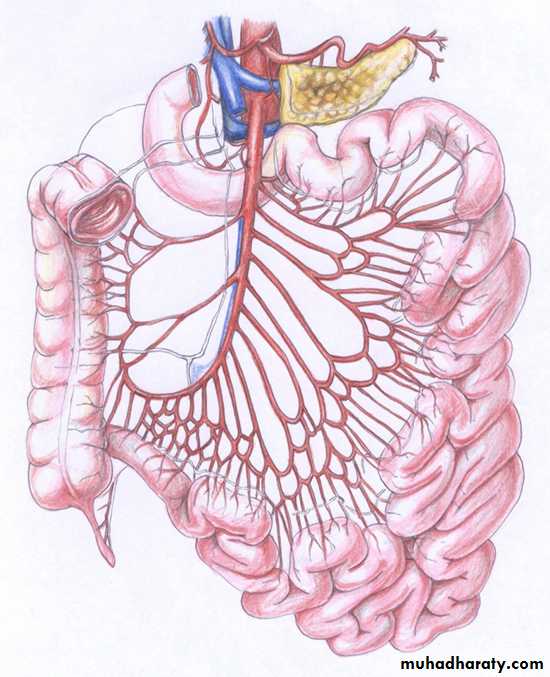
5-Art sup duodenum RG, SPDA and IPDA jeju and ileum from SMA
Anatomy of small bowel
Blind loop syndrome
PathogenesisStasis causing bacteria flora over growth preventing proper breakdown of food especially fat and vitamins
Type of blind loop syndrome
1-self –filling :deficiency occurs 2-self emptying no deficiency
3-long afferent loop stasis in polya gastrectomy 4-jejunal diveticula5-intestinal stricture 6-stenosis –anastomosis loop syndrome
Diverticular diseaseTypes1-congental 2- acquired
Jejuna diverticulaVariable in size and number
1-asymtomatic 2-abdominal pain
3-produce a malabsorption 4- as acute abdomen
5- more common in patient with connective tissue disorder 6-major malabsorption problems giving rise to anemia , steatorrhoea, hypoproteinaemia, or vit B12 deficiency
6-resection of affected segment can be effective
Meckel, s diverticulum
1-2% on ati-mesenteric borderof small intestine
2-2 feet from ileocaecal valve
3-2 inches length
4-it is true diverticulum
5-20% contain heterotopic
epithelium ( gastric ,colonic, or pancreatic)
Symptoms
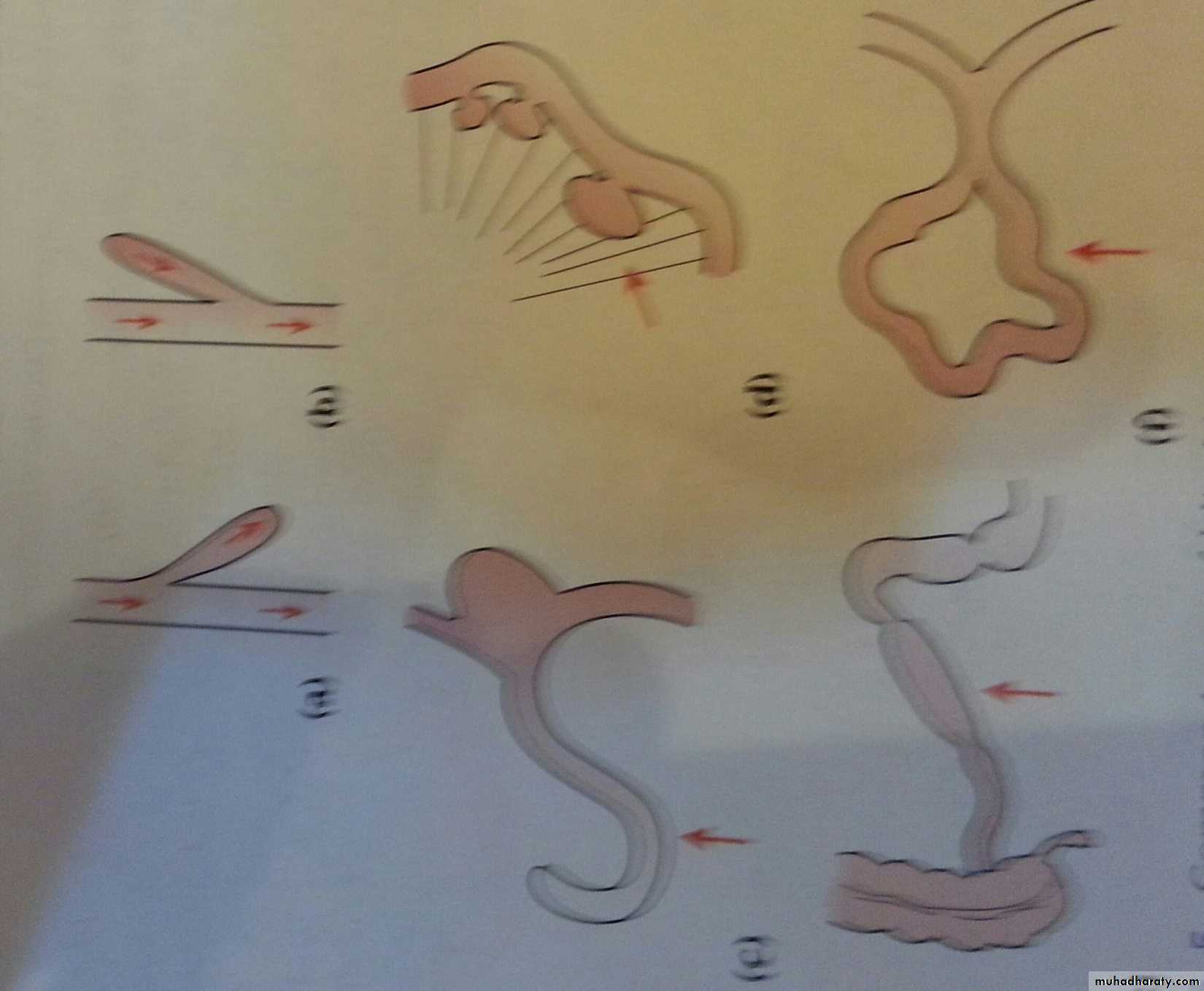
1-sever hemorrhage 2- intussuscepption
3-diverticulitis 4-chronic peptic ulcer pain around umbilicus
5-intestinal obstruction by band
Investigation
1-difficult to be seen by contrast study but small bowel enema would be the most accurate investigation2-Tc -99m scaning
Silent Meckel,s diverticulum
No need for surgery if the
1-if it is wide mouthed
2-if the wall of diverticulum does not feel thickenened
3-where there is doubt and can be removed without appreciable additional risk
TB of the intestine
-any part of GIT can affected but the terminal ileum, proximal colon and peritoneumType
A-ulcerative TB
-2nd to pulmonary TB
-multiple transversely ulcer in the terminal ileum
-overlying serosa is thick , reddened, and covered by tubercles
Clinical features
-diarrhoea and wt loss
-history for antiTB for pulmonary TB
Radiology
B-meal and follow through or small bowel enema shows absence of filling of lower ileum, caecum and proximal ascending colon
Treatment
B-hyperplastic TB
1-solitary or multiple lesion in the terminal ileum
2-caused by ingestion of M-tuberculosis with high resistance to the organism
3-thickening the wall and narrowing the lumen
4-early regional LN which may caseate is involvement
Clinical feature
1-bdominal pain with attach of diarrhoea
2-anemia and loss of wt
3-RIFmass
4-B-meal and follow through showed long narrow filling defect of terminal ileum
Treatment
Actinomycosis of the ileocaecal region
1-it is rare2-narrowing of the lumen of the intestine does not occur
3-mesenteric nodes do not involved
4-local abscess spread to retroperitoneal tissue and adjacent abdominal wall forming multiple indurated discharging sinuses
5-liver may be involved
Clinical features
1-history of appendectomy
2-3wks after surgery mass at RIF then wound discharge after wound healing
3-thin watery discharge then become thick
4-fecal fistula may develop
5-sulphur granule
Treatment
Pencillin or cotrimoxazole treatment should be prolonged and high dose
Tumors of small bowel
it is rare compared to large bowel and this due
benign tumor
(adenoma, lipomas, haemangiomas, and neurogenic tumours)
clinically presented as intussusceptions, bleeding, usually delayed DX as overlooked at barium radiology, endoscope and even surgery
peutz-jeghers syndrome
a-autosomal dominant disease ( gene STK11 on chromosome 19-intestinal hamartomatosis polyposis affect whole small and large bowel and causing hemorrhage and often intussusceptions
-melanosis of the oral mucous membrane and lip( melanin spot some time on digit and perianal spot
-long follow up is indicated may change to malignant and a wide range of cancer
-endoscope or contrast study every 3 ys
-female patient attend cervical and breast screening program
Histology
Polyps like tree
Treatment
adenocarcinoma
1-more found in the jejunum2-more common in patient with Crohns disease, coeliac, FAP and Peutz-Jeghers syndrome
3-clinical picture
4-treatment
Carcinoid tumor
a-common sit appendix, ileum, rectum
b-origin from neuroendocrine cell at the base of intestinal crypt
c-primary small while 2nd is large, multiple and more yellow when this has occurred , the carcinoid syndrome will become evident
d-clinical syndrome consist reddish –blue cyanosis, flushing attacks ,diarhhoea, asthmatic attack, some time pulmonary and tricuspid stenosis
treatment
a-resection the tumor and enucleation of hepatic metastases
b-octreotide for preparation who has syndrome for surgery and for symptom of syndrome
lymphoma
Mediterrannean
primary lymphoma
western
North africa , middle
East
Burkitts lymphoma
: regarded as T-cell lymphoma in patient with celiac disease there is worsening of the patient diarrhoea, with pyrexia of unknown origin together with local obstruction
type: annular ulcerating lesion may be multiple thought to be non-Hodgkin,s lymphoma in origin
(obstruction and bleeding, perforation, anorexia and wt loss)
Criteria for DX of primary lymphoma
:Lack of peripheral or mediastinal lymphadenopathy.
Normal WBC count and differential on peripheral smear.
Tumor involvement primarily in GI tract.
No involvement of liver or spleen.
No history of previously treated nodal lymphoma.
gastrointestinal stromal tumor
benign and malignantmalignant is sarcoma occur in 50-70 ys
patient with neurofibromatosis have increase risk
symptom
lethargy, pain, nausea, hematemesis or melaena
treatment
surgery with imitinib is effective in advanced cases
Intestinal trauma
Aetiology
A-blunt abdominal trauma
B-penetrating trauma
C- iatrogenic
1-ERCP
2-laparoscope
Types of injury
A-contusion and haematomaB-rapture complete or incomplete , single or multiple
C- tears of mesentery or
mesentery bd vessel resulting
in haematoma and gangrene
of the affected bowel segment
sequelae
A-peritonitisb-internal bleeding
C-hypovolaemia and septic shock
D-paralytic ileus
E-intestinal obstruction later due stricture or adhesion
Clinical feature
Symptoms
1-history of traum
2-abdominal pain
Signs
A-general signs
B-local signs(inj sign, tenderness, liver dullness, shifting dullness, ileus, peritonitis may delayed
investigations
DX depend on clinical basesA-lab tests: WBC count and Hb
B-radiology
1-plain X-ray of abdomin may show
a-air under the diaphragm
b-multiple fluid level
c-bullet
d-fracture
2-us or CT-scan
C--DPL
treatment
All bowels inj need laparotomyA-preoperative preparation
1-anti-shock measures
2-antibiotic
3-tetanus toxoid boosting dose
4-NGT and urethral catheter
Conte treatment
B-Laparotomy
1-Tidy inj are sutured
2-Raged inj
3-intestinal resection for ischemic or gangrenous segment or severe contused segment and for multiple perforation close together
Intestinal fistulae
A fistula is abnormal communication between two epithelialized surface , formed by granulation tissue but some case it may lined by epitheliumAetiology
80% of external fistulae after laparotomy due to
A-unrecognized intestinal inj
B- failure of an intestinal anastomosis
1-poor vascularity 2-anastomsis under tension
3-distal obstruction 4-lack of proper surgical technique 5-presence of sp path as Crohn
Cont aetiology
6-generralized diseases that impair healing e.g hypoproteinaemiaC-other causes
1-congenital anomalies
2-abdominal trauma
3- inflammatory conditions
4-malignant tumors
pathology
Classification
A-internal fistula
B-external fistula
1-low- output(less than 500ml/d)
2-high-output (more than 500/d)
C-according to origin in intestine
complications
1-metabolic effectsa-dehydration
b-malnutrition e.g hypalbuminaemia
c- electrolyte disturbance
d-acid –base disturbance cause acidosis
2-sepsis
3-skin irritation and maceration
management
1-resuscitation and skin protectiona-correct the dehydration, and electrolyte balance. Blood transfusion may be needed
b-skin protection start as early as possible by adhesive cover and a disposable collection bag are applied to skin around fistula
2-nutritional sport
a-TPN for high output and proximal fistula
b-enteral feeding for low output and distal fistula
Conte management
3-investigation and eradication of sepsis:
(detect the level of fistula, presence of bowel disease, distal obstruction, and the presence of intraperitoneal sepsis
Investigations
a-clinical assessment
b-fistulography and B-meal follow through
c-us or CT-scan
4-Suppression of intestinal secretions by somatoststin 0,1mg s.c every 8 hr for 2-3 wks
Conte management
5-definitive treatmentA-external fistula start as nutritional support
Indication of surgery
1-no improvement over 4-6 wks
2-distal obstruction
3-active disease at sit of fistula e.g malignancy
4-total discontinuity of the bowel end
5-mucocutaneous continuity
Conte management
B-internal fistula: spontaneous closure is rare and many do not need to be closedIndications of surgery
1-patient with nutritional problem where fistula bypasses along segment of intestine producing malabsorption
2-internal fistulae to the urinary tract
Thank you