THE HYPOTHALAMUS ANDTHE PITUITARY GLAND
By:Dr. Wael Thanoon Younis
C.A.B.M.,Mosul college of medicine.
Functional anatomy, physiologyand investigations:
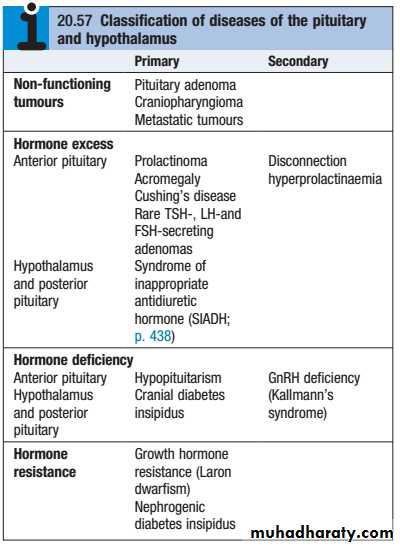
The pituitary gland is enclosed in the sella turcica and bridged over by a fold of Dura mater called the diaphragma sellae, with the sphenoidal air sinuses below and the optic chiasm above. The cavernous sinuses are lateral to the pituitary fossa and contain the 3rd, 4th and 6th cranial nerves and the internalcarotid arteries. The gland is composed of two lobes, anterior and posterior, and is connected to the hypothalamus by the infundibular stalk, which has portal vessels carrying blood from the median eminence of the hypothalamus to the anterior lobe and nerve fibers to the posterior lobe .Diseases of the hypothalamus and pituitary are classifed in Box.
By far the most common disorder isan adenoma of the anterior pituitary gland.
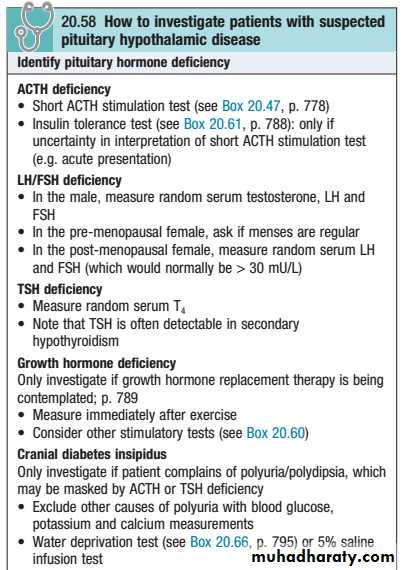
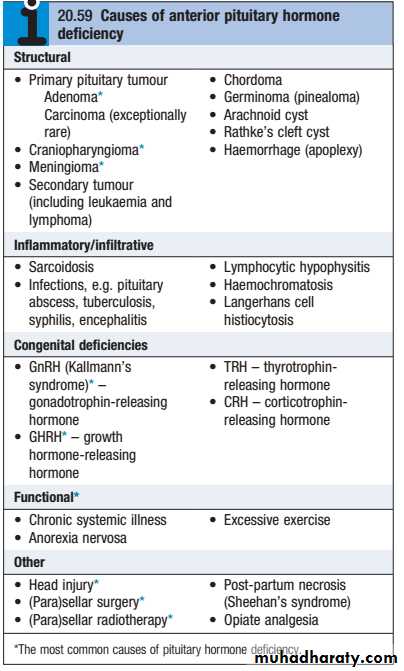
Investigation of patients with pituitary disease :
The most common local complication of a large pituitary tumor is compression of the optic pathway. The resulting visual field defect can be documented using a Goldman’s perimetry chart.MRI reveals ‘abnormalities’ of the pituitary gland in as many as 10% of ‘healthy’ middle-aged people.It should therefore be performed only if there is a clear biochemical abnormality or in a patient who presents with clinical features of pituitary tumour .A pituitary tumour may be classifed as either a macroadenoma (> 10 mm diameter) or a microadenoma(< 10 mm diameter).
Surgical biopsy is usually only performed as part of a therapeutic operation. Conventional histology identifes tumours as chromophobe (usually non-functioning), acidophil (typically prolactin- or growth hormonesecreting) or basophil (typically ACTH-secreting);immunohistochemistry may confrm their secretory capacity but is poorly predictive of growth potential of the tumour.
Presenting problems in hypothalamicand pituitary disease:
Younger women with pituitary disease most commonly present with secondary amenorrhoea or galactorrhoea (in hyperprolactinaemia). Post-menopausal women and men of any age are less likely to report symptoms of hypogonadism and so are more likely to present late with larger tumors causing visual field defects.Nowadays, many patients present with the incidental finding of a pituitary tumor on a CT or MRI scan.
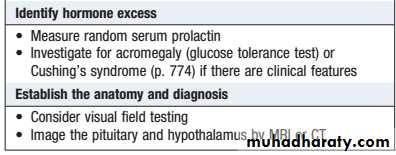
Hypopituitarism:
Hypopituitarism describes combined deficiency of any of the anterior pituitary hormones. The clinical presentation is variable and depends on the underlying lesionand the pattern of resulting hormone deficiency. The
most common cause is a pituitary macroadenoma but
other causes are listed below
Clinical assessment :
The presentation is highly variable. For example, following radiotherapy to the pituitary region, there is a characteristic sequence of loss of pituitary hormone secretion.Growth hormone secretion is often the earliest to be lost.In adults, this produces lethargy, muscle weakness and increased fat mass but these features are not obvious in isolation.
Next, gonadotrophin (LH and FSH) secretion becomes impaired with, in the male, loss of libido and, in the female, oligomenorrhoea or amenorrhoea. Later, in the male there may be gynaecomastia and decreased frequency of shaving. In both sexes, axillary and pubic
hair eventually become sparse or even absent and the skin becomes characteristically finer and wrinkled.
Chronic anemia may also occur. The next hormone to be lost is usually ACTH, resulting in symptoms of cortisol insufficiency (including postural hypotension and a dilutional hyponatraemia).
In contrast to primary adrenal insufficiency ,angiotensin II-dependent zona glomerulosa function is not lost and hence aldosterone secretion maintains normal plasma potassium. In contrast to the pigmentation of Addison’s disease due to high levels of circulating ACTH acting on the skin melanocytes, a striking degree of pallor is usually present.
Management:
1-Cortisol replacement:Hydrocortisone should be given if there is ACTH defciency. Suitable doses are described in the section on adrenal disease on.
Mineralocorticoid replacement is not required.
2-Thyroid hormone replacement: Levothyroxine 50–150 µg once daily should be given , Unlike in primary hypothyroidism, measuring TSH is not helpful in adjusting the replacement dose because patients with hypopituitarism often secrete glycoproteins which aremeasured in the TSH assays but are not bioactive. Theaim is to maintain serum T4 in the upper part of the reference range. It is dangerous to give thyroid replacementin adrenal insuffciency without frst giving glucocorticoid therapy, since this may precipitate adrenal crisis.
3-Sex hormone replacement:
This is indicated if there is gonadotrophin defciency in women under the age of 50 and in men to restore normal sexual function and to prevent osteoporosis .4-Growth hormone replacement:
Growth hormone (GH) is administered by daily subcutaneous self-injection to children and adolescents with GH defciency and, until recently, was discontinuedonce the epiphyses had fused. However, although hypopituitary adults receiving ‘full’ replacement with hydrocortisone, levothyroxine and sex steroids are usuallymuch improved by these therapies, some individuals remain lethargic and unwell compared with a healthy population. Some of these patients feel better, and haveobjective improvements in their fat :muscle mass ratios and other metabolic parameters, if they are also given GH replacement. Treatment with GH may also help young adults to achieve a higher peak bone mineraldensity.The principal side-effect is sodium retention, manifest as peripheral oedema or carpal tunnel syndrome.