PROGNOSIS
Jafar Naghshbandi D.D.S;M.S
Diplomate of the American Board of Periodontology
CONTENTS
Defination
Determination of prognosis
Type of prognosis
Factors affecting prognosis
Relationship between diagnosis and prognosis
Reevaluation of prognosis after phase I
therapy
Conclusion
References

Prognosis is
the prediction of the
probable
course, duration, and outcome of a disease
based on a general knowledge of the
pathogenesis of the disease and the presence of
risk factors for the disease.
Goodman et al
MADE BEFORE TREATMENT PLAN IS
ESTABLISHED
Based on:
Specific information about disease
Previous experience
Confused with risk
Risk : Likelihood that an individual will get a
disease in a specified period
DETERMINATION OF PROGNOSIS:
1
>
Excellent
2
>
Good
3
>
Fair
4
>
Poor
5
>
Questionable
6
>
Hopeless
(Mc Guire et al 1991
)
EXCELLENT
No bone loss
Excellent gingival condition
Good patient cooperation
No systemic / environmental factors
GOOD
Adequate remaining bone support
Adequate possibilities to control etiologic
factors and establish a maintainable dentition
Adequate patient cooperation
factors
or if
No systemic / environmental
present well controlled
FAIR
Less than adequate remaining bone
support
Some tooth mobility
Grade I furcation involvement
Adequate maintenance possible
Acceptable patient cooperation
Limited systemic / environmental factors
POOR
Moderate to advanced bone loss
Tooth mobility
Grade I and II furcation involvement
Difficult to maintain areas
Doubtful patient cooperation
Presence of systemic / environmental factors
QUESTIONABLE
Advanced bone loss
Grade II and III furcation involvements
Tooth mobility
Inaccessible areas
Presence of systemic / environmental factors
HOPELESS
Advanced bone loss
Non-maintainable areas
Extractions indicated
Uncontrolled systemic / environmental
conditions
OVERALL VERSUS INDIVIDUAL TOOTH PROGNOSIS
INDIVIDUAL TOOTH
PROGNOSIS
Determined after the
overall prognosis and is
affected by it.
OVERALL PROGNOSIS
Factors that may
influence the overall
prognosis include
Patient age
Current severity of
disease
Systemic factors
Smoking
Presence of plaque &
calculus
Patient compliance

Should treatment be undertaken?
Is it likely to succeed ?
.
When prosthetic replacements are needed, are the
remaining teeth able to support the added burden
of the prosthesis?
Overall
Clinical
Factors
Systemic/
Environmental
Factors
Local Factors
Prosthetic/
Restorative
Factors
Patient age
Disease
severity
Plaque
control
Patient
compliance
Smoking
Systemic
disease/conditio
n
Genetic factors
Stress
-
Plaque/calculus
-
Subgingival restorations
-
Anatomic factors:
Short, tapered roots
Cervical enamel
projections
Enamel pearls
Bifurcation ridges
Root concavities
Developmental grooves
Root proximity
Furcation involvement
-
Tooth mobility
Abutment
selection
Caries
Nonvital teeth
Root resorption
OVERALL CLINICAL
FACTORS
1.PATIENT AGE
Comparable CT attachment and alveolar
bone –
prognosis better for older
Younger patient – shorter time – more
periodontal destruction

2. DISEASE SEVERITY
Determination of :
Pocket depth
Level of attachment
Degree of bone loss
Type of bony defect
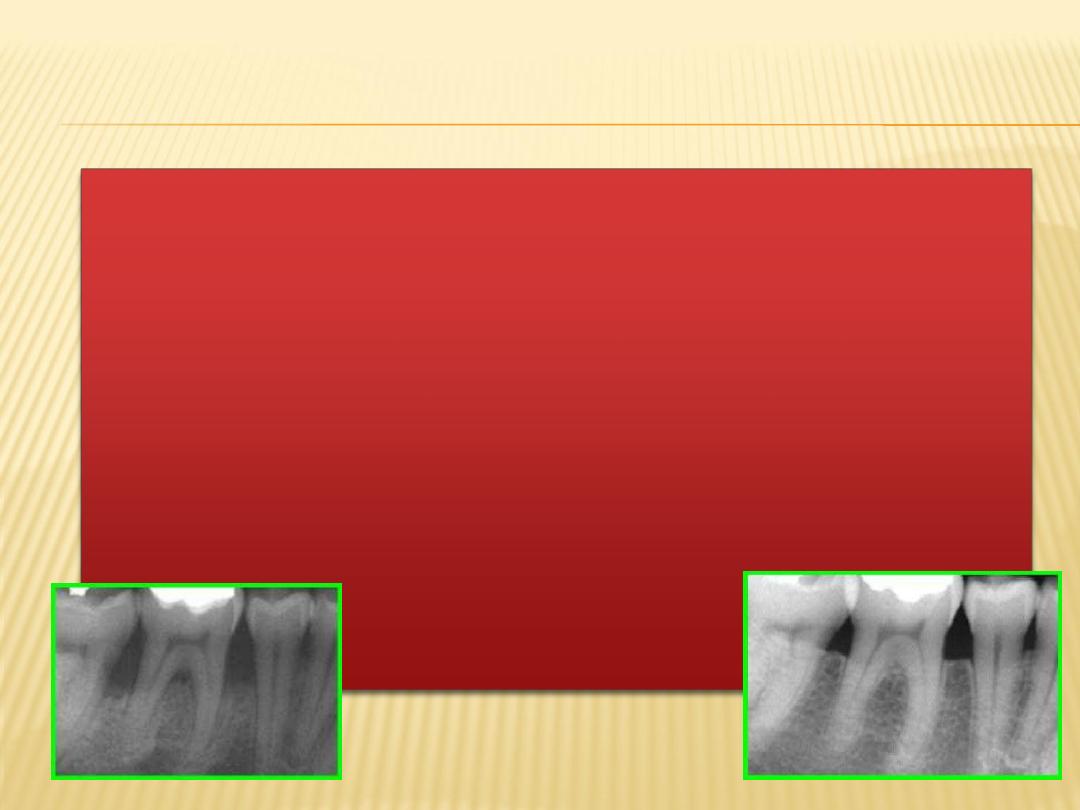
Prognosis for horizontal bone loss depends
on the height of the existing bone.
Angular defects - if the contour of the
existing bone & the number of osseous
walls are favorable, there is an excellent
chance that therapy could regenerate
bone to approximately the level of the
alveolar crest.
When greater bone loss has occurred on one surface
of a tooth, the bone height on the less involved
surfaces should be taken into consideration when
determining the prognosis.
3
. PLAQUE CONTROL
Bacterial plaque - primary etiologic factor
associated with periodontal disease.
Effective removal of plaque on a daily basis by
patient.
4
. PATIENT COMPLIANCE
&
COOPERATION
Refuse to accept the patient for treatment
Extract teeth with hopeless or poor prognosis and
perform scaling and root planing on remaining
teeth
SYSTEMIC/
ENVIRONMENTAL
FACTORS
1
. SMOKING
Direct relationship - smoking and the
prevalence and incidence of periodontitis
Affects severity
Affects healing
Slight to moderate periodontitis - fair to
poor
Severe periodontitis - poor to hopeless

2. SYSTEMIC DISEASE/
CONDITION
Prevalence and
severity of
periodontitis -
significantly higher - type I and II diabetes
Prognosis dependent
on patient compliance
relative to both dental and medical status
Well controlled patients - slight to moderate
periodontitis - good prognosis

4
. GENETIC FACTORS
Genetic polymorphism in IL-1 genes resulting in
overproduction of IL-1
- associated with significant
increase in risk for severe, generalized, chronic
periodontitis.
Genetic factors also influence serum IgG2 antibody
titers and the expression of Fc-
RII receptors on the
neutrophil - significant in aggressive periodontitis.
IDENTIFICATION OF GENETIC FACTORS CAN
LEAD TO TREATMENT ALTERATIONS –
ADJUNCTIVE ANTIBIOTIC THERAPY &
FREQUENT MAINTENANCE VISITS.

LOCAL FACTORS

1
. PLAQUE AND CALCULUS
calculus -
most
plaque
local
and
factor
in periodontal
Bacterial
important
diseases.
Good prognosis- depends on ability of
patient and clinician to remove etiological
factor.
2
. SUBGINGIVAL RESTORATIONS
Contribute to
Increased plaque accumulation
Increased inflammation
Increased bone loss
Subgingival margins - poor prognosis.
3
. ANATOMIC FACTORS
Short, tapered roots with large crowns, cervical
enamel projections (ceps) and enamel pearls,
intermediate bifurcation ridges, root concavities,
and developmental grooves - predispose
periodontium to disease
Teeth with short, tapered roots and relatively
large crown – Poor prognosis
CEPs
are flat, ectopic extensions of enamel extending
beyond the normal contours of the cementoenamel
junction.
Enamel pearls
are larger, round deposits of enamel
that can be located in furcations or other areas on the
root surface
Developmental grooves
– create accessibility problems
plaque-retentive area - difficult to instrument
Root concavities
exposed through loss of attachment
can vary from shallow flutings to deep depressions.
They appear more marked on maxillary first
premolars, the mesiobuccal root of the maxillary first
molar.
Although these concavities increase the attachment
area and produce a root shape that may be more
resistant to torquing forces but they are inaccessible
to clean.
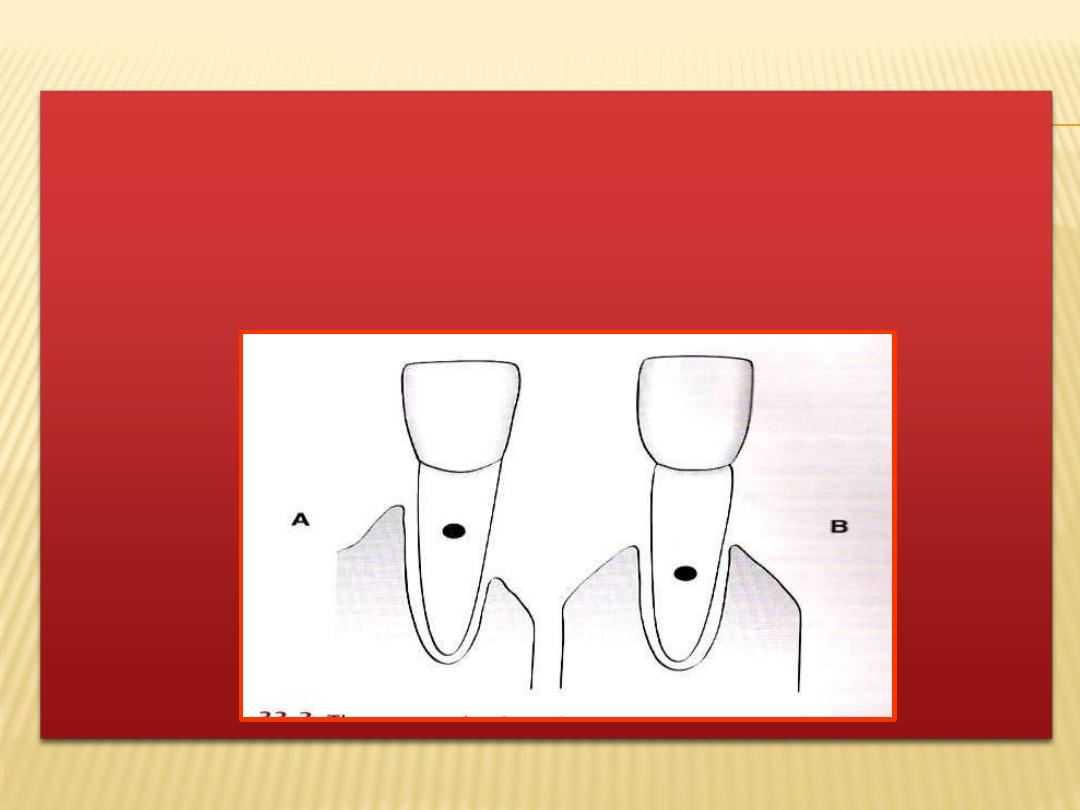
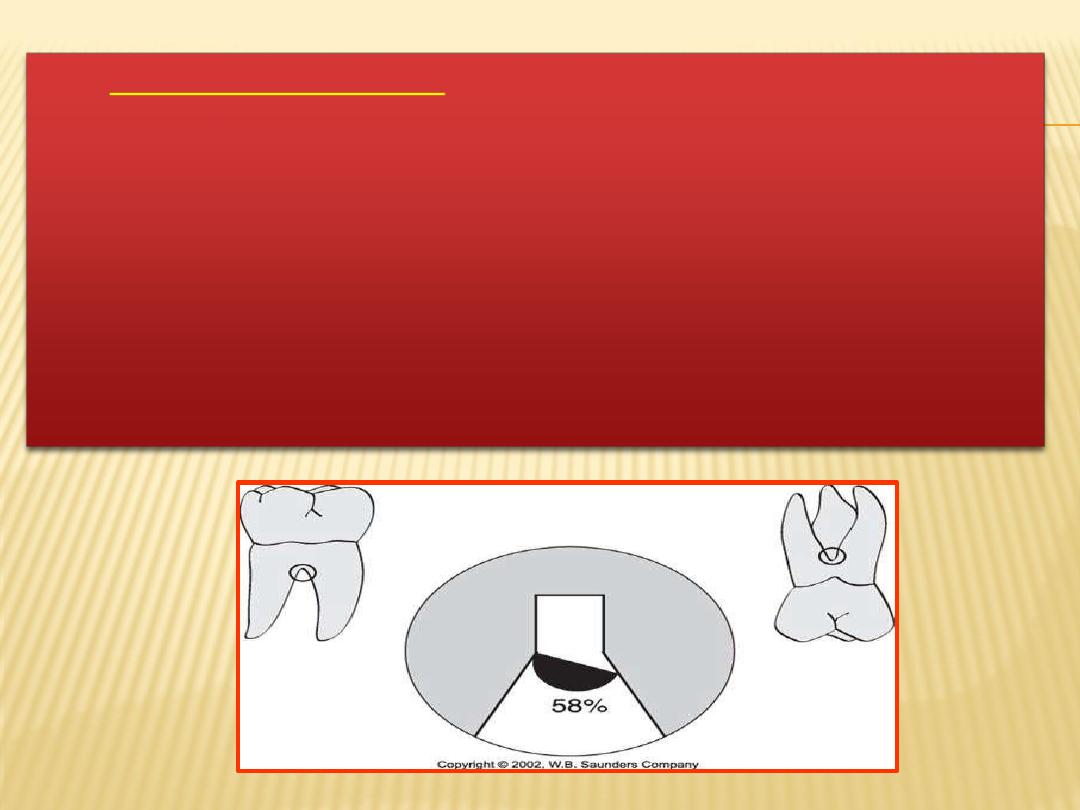
4
. TOOTH MOBILITY
Principal causes-
Loss of alveolar bone
in the
Inflammatory changes
periodontal ligament
Trauma from occlusion.
stabilization by use of splinting
the
tooth
- beneficial impact on
overall and individual
prognosis.
Correctable
Non correctable
PROSTHETIC/REST
ORATIVE
FACTORS
THE OVERALL PROGNOSIS REQUIRES A GENERAL
CONSIDERATION
OF
BONE
LEVELS
AND
ATTACHMENT LEVELS TO ESTABLISH WHETHER
ENOUGH TEETH CAN BE SAVED EITHER TO
PROVIDE A FUNCTIONAL AND AESTHETIC
DENTITION OR TO SERVE AS ABUTMENTS FOR A
USEFUL PROSTHETIC REPLACEMENT OF THE
MISSING TEETH.
THE OVERALL PROGNOSIS AND THE
PROGNOSIS FOR INDIVIDUAL TEETH
OVERLAP BECAUSE THE PROGNOSIS FOR
KEY INDIVIDUAL TEETH MAY AFFECT THE
OVERALL PROGNOSIS FOR PROSTHETIC
REHABILITATION.
WHEN
FEW
TEETH
REMAIN,
THE
PROSTHODONTIC
NEEDS
BECOME
MORE
IMPORTANT, AND SOMETIMES PERIODONTALLY
TREATABLE
TEETH
MAY
HAVE
TO
BE
EXTRACTED IF THEY ARE NOT COMPATIBLE
WITH THE DESIGN OF THE PROSTHESIS.
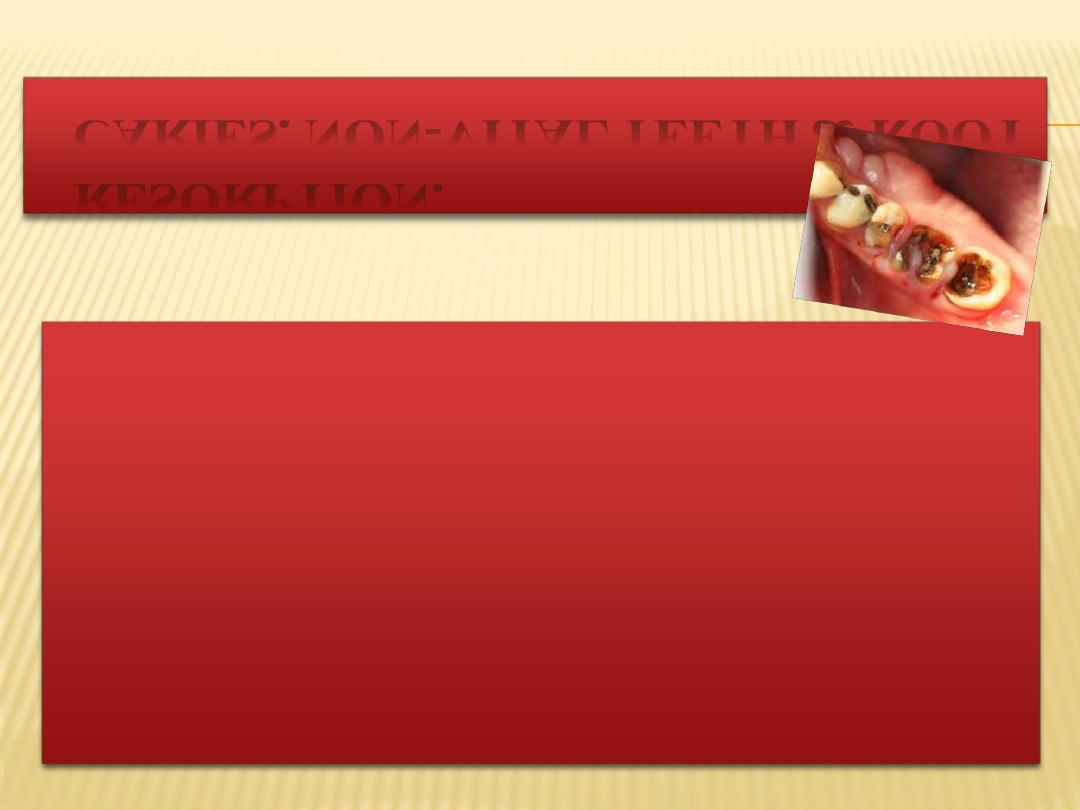
CARIES, NON-VITAL TEETH & ROOT
RESORPTION.
For teeth mutilated by extensive caries, the feasibility
of adequate restoration and endodontic therapy should
be
considered
before
undertaking
periodontal
treatment.
Extensive idiopathic root resorption or root resorption
that has occurred as a result of orthodontic therapy,
risks the stability of teeth and adversely affects the
response to periodontal treatment.
RELATIONSHIP BETWEEN
DIAGNOSIS AND PROGNOSIS
Factors such as patient age, severity of
disease, genetic susceptibility, and presence of
systemic disease are important in developing
both diagnosis as well as prognosis.
PROGNOSIS FOR PATIENTS WITH GINGIVAL
Reversible
Prognosis - good provided all local irritants are
eliminated & patient cooperates by maintaining
good oral hygeine.
DISEASE
I. DENTAL PLAQUE INDUCED GINGIVAL DISEASES

B) PLAQUE INDUCED GINGIVAL DISEASES
MODIFIED
by systemic factors
The inflammatory response to bacterial plaque can be
influenced by systemic factors, such as endocrine
related changes associated with puberty, pregnancy
and diabetes.
Long term prognosis depends - control of bacterial
plaque along with correction of the systemic factors.
C) PLAQUE INDUCED GINGIVAL DISEASE
modified by medications
•
Drug induced gingival enlargement often seen with
phenytoin, cyclosporin, nifedipine and in oral
contraceptive associated gingivitis.
•
Plaque control alone does not prevent the
development of lesions, and surgical intervention is
usually necessary to correct the alteration of gingival
contours.
D) GINGIVAL DISEASES MODIFIED
BY
malnutrition
Exception - vitamin C deficiency (gingival
inflammation and bleeding on probing independent
of plaque levels present)
Prognosis of these patients depend upon the
severity and duration of the deficiency and on the
likelihood of reversing the deficiency through dietary
supplements.
II. NON PLAQUE INDUCED
GINGIVAL LESIONS
Seen in patients with a variety of bacterial, fungal
and viral infections.
Dermatologic
lichen
planus,
pemphigoid,
disorders such as
pemphigus
vulgaris,
erythema
multiforme, and lupus erythematosus can also
manifest in oral cavity as atypical gingivitis.
Allergic, toxic, and foreign body reactions, as well as
mechanical and thermal trauma, can result in
gingival lesions.
PROGNOSIS OF PATIENTS WITH
PERIODONTITIS
Chronic periodontitis
In cases where clinical attachment loss and bone
loss are not very advanced (slight to moderate
periodontitis) - prognosis - good.
The inflammation - controlled through good oral
hygiene and the removal of local plaque retentive
factors.

AGGRESSIVE PERIODONTITIS
Poor prognosis
Localized aggressive periodontitis
–
Occurs around puberty
Localized to first molars and incisors
Patient exhibits strong serum antibody response to the
infecting agent contributing to localization of lesions.
DIAGNOSED EARLY
- CAN BE TREATED CONSERVATIVELY WITH
ORAL HYGIENE INSTRUCTION AND SYSTEMIC ANTIBIOTIC
THERAPY - EXCELLENT PROGNOSIS.
Advanced diseases
, prognosis can be good if the
lesions are treated with debridement, local and
systemic antibiotics, and regenerative therapy
GENERALIZED FORM
– FAIR, POOR OR
QUESTIONABLE PROGNOSIS DUE TO
GENERALIZED INTERPROXIMAL LOSS, POOR
antibody response and thus poor response to
conventional periodontal therapy.

PERIODONTITIS AS A MANIFESTATION
OF SYSTEMIC DISEASES
It can be
divided into two categories
:
- periodontitis associated with
hematologic
disorders such as leukemia and
acquired
neutropenia.
- periodontitis associated with genetic disorders
such as familial and cyclic neutropenia, down
syndrome and hypophosphatasia.
Primary etiologic factor
- bacterial plaque
Systemic diseases
affect the
progression
of disease
and thus
prognosis.
NECROTIZING PERIODONTAL
DISEASES
Necrotizing ulcerative gingivitis (NUG)
Necrotizing ulcerative periodontitis (NUP.)
In NUG - primary predisposing factor - bacterial plaque.
Disease - complicated by presence of secondary
factors such as acute psychological stress, tobacco
smoking, poor nutrition leading to immunosuppression.
With control of both bacterial plaque and secondary
factors prognosis
(NUG) - good
although tissue
destruction is not reversible.
NUP is similar to that of NUG, except the necrosis extends
from the gingiva into the periodontal ligament and
alveolar bone.
Many
patients
presenting
with
NUP
are
immunocompromised through systemic conditions, such
as HIV infection.
REEVALUATION OF PROGNOSIS
AFTER PHASE I THERAPY
inflammatory
changes not
controlled or
If the
reduced
by phase I therapy- overall prognosis -
unfavorable.
In these patients the prognosis can be directly
related to the severity of inflammation.
Reduction in pocket depth and inflammation after
Phase I therapy indicates a favorable response to
treatment and may suggest a better prognosis than
previously assumed.
CONCLUSION
Prognosis help us in planning the customized
treatment for each patient thus help in
providing overall care to patient. So it should
be given due importance in general clinical
practice
REFERENCES
Carranza’s Clinical Periodontology 10th Edition.
Lindhe- 5th edition