
Ass.
Prof.
Zaid
W.Al-Shahwanii
Consultant Orth. Surgeon
2016

Osteomyelitis is inflammation of the bone caused by an
infecting organism. Although bone is normally resistant to
bacterial colonization, events such as trauma, surgery, the
presence of foreign bodies, or the placement of prostheses
may disrupt bony integrity and lead to the onset of bone
infection..
Early and specific treatment is important in osteomyelitis,
and identification of the causative microorganisms is
essential for antibiotic therapy. Infection of bones and joints
is associated with considerable morbidity, and can be a
challenging to treat.

The principles
& goals of treatment are;-
1) Prompt diagnosis.
2) Aggressive eradication of infection. Using
appropriate antibiotic &surgical debridement.
3) Restoration of function
Routes of infection:
-
Micro-organisms may reach the
musculoskeletal tissues by
(a)
direct introduction of bacteria
through the
skin
trauma
(a pinprick, an injection, a stab wound, a
laceration, an open fracture or an operation )
like
surgical reduction and internal fixation of fractures &
prosthetic devices
spread from soft-tissue infection
spread from adjacent septic arthritis
( b)
Indirect spread via the blood stream
Hematogenous spread
(a) microorganisms are introduced into bone
hematogenously from surrounding structures
or
from
a distant site such as the nose or mouth, the respiratory
tract, the bowel or the genitourinary tract
(b) the vertebrae are the most common site
(c) more common in infants and children
(d) S. aureus is the most common pathogenic organism
(e) IV drug abuse, Dental extraction , GIT Infection & UTI
are also associated
The clinical picture of infection resul
ts from
inoculation of microorganisms in bone and joint
tissues and, the interaction of microorganisms with
host environment
.
Etiology & Pathophysiology
Important factors in pathogenesis
virulence of the infecting organism
underlying disease
immune status of the host
the type, location, and vascularity of the
bone
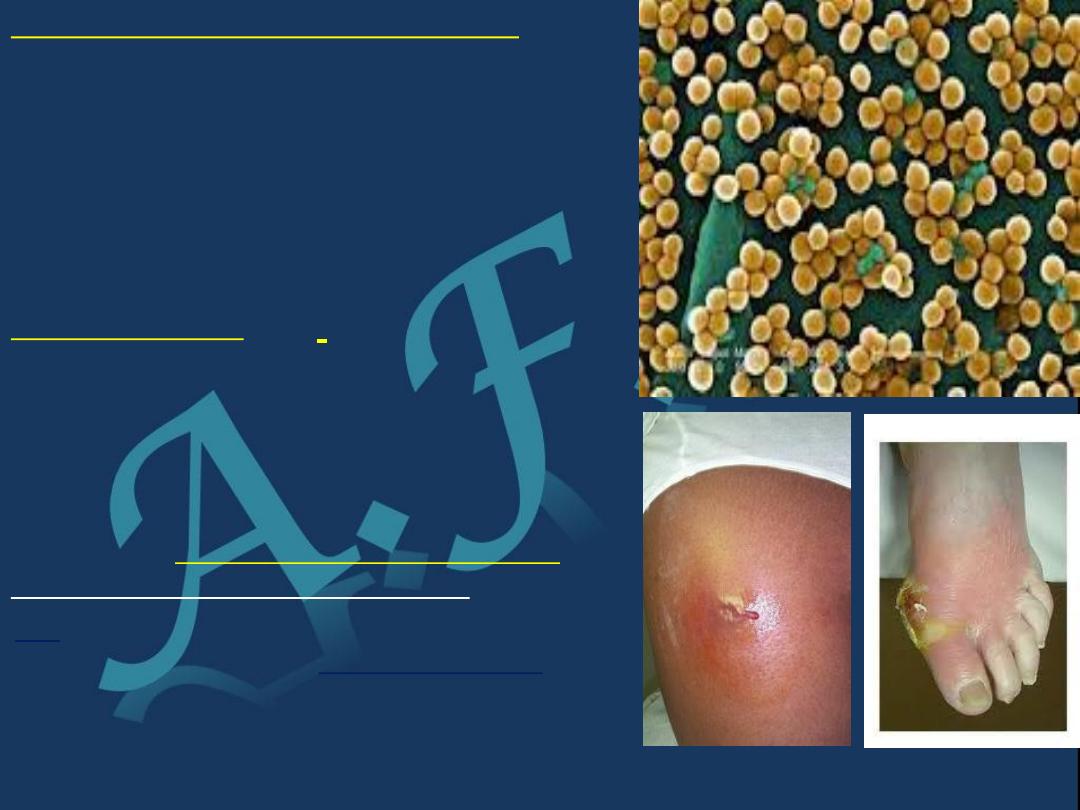
* The virulence
of the
microorganism
defined as the ability of
the organism to overcome the host
defenses and cause infection
it varies
among organism species eg .staph aures
which produce certin toxin plus the
presences of biofilm protein for self
protection
(Staphylococcus aureus )
found in over 70% of cases .
In
Latin . coccus = spherical bacterium,
aureus = golden) or golden staph is the
most common species of
staphylococcus bacteria causing
infections in human.
* Host response:
Local host factors
, that facilitate infection and they include:
Reduced vascularity. Peripheral N. Neuropathy. Trauma. Presence
of implants.
Systemic factors:
That may reduce the ability of the immune system to respond to a
pathogen, and they include: Age (very young and very old).
Renal and liver diseases. Malignancies. Diabetes mellitus.
Alcoholism. Malnutrition. Rheumatological disorders.
Immunocompromised conditions like ,(AIDS) , receiving
immunosuppressive drugs. Intravenous drug users.
* Site of infection
---------------------------------------------------------------------------------
This will lead to Two types of B. infection
1)
Pyogenic osteomyelitis or arthritis.
And this can be: Acute. Subacute. Chronic.
2
)
Chronic specific granulomatous reaction
(eg. tuberculosis).
This will lead to Two types of B. infection
1) Pyogenic osteomyelitis or arthritis.
And this can be: Acute. Subacute. Chronic.
2 )Chronic specific granulomatous reaction
(eg. tuberculosis).
------------------------------------------------------------------------
1-Acute Osteomyelitis
: infection develops within 2
weeks of an injury , initial infection or the start of an
underling disease
2-Sub acute Osteomyelitis
: infection develops within 1
or 2 months of an injury , initial infection or the start of an
underling disease
3-Chronic Osteomyelitis
: infection starts at least 2
months after an injury , initial infection or the start of an
underling disease
Acute Hematogenous Osteomyelitis:
Incidence;
almost invariably seen in children , Males > females. Mainly lower
limb lower affected more. Adults may also be affected due to
lower host resistance (debilitation, disease or drugs eg cyto toxic
,or steroid ).
Bacteriology:
The causative organisms:Usually and most common
1.
staphylococcus aureus
.
2.
Haemophilus influenza,
3.
Group B streptococcus & sometimes gram –ve pathogens in
younger children and in neonates.
4.
..Salmonella in patients with sickle-cell anemia.
5.
Mixed or unusual infection (fungus) in intravenous
drug users and in immuno -suppresed patient.

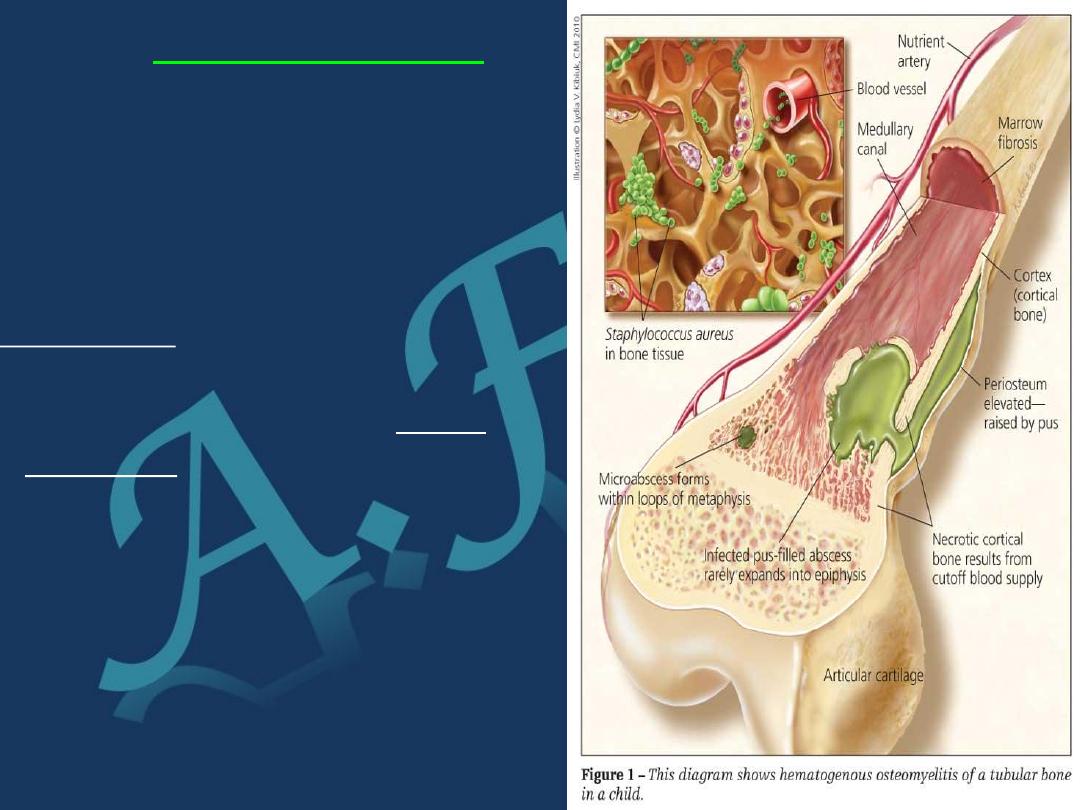
Pathogenesis
In Heamatogenous Osteomyelitis
the microorganisms spread through the
vascular system into the osseous tissue
producing secondary focus of infection
Site of infection In children
Were growth plat consider a barrier
for the bactria to penetrate .
The microorganisms usually settle
in the metaphysis of the growing end
of the long bone as proximal & distal
femur,, proximal tibia ; possibly bec
’ the non
anastomizing terminal branches of the nutrient artery
twisting back in hair-pin loops before entering the large
network of sinusoidal veins; the relative vascular stasis &
consequent lowered oxygen tension are believed to favor
bacterial colonization.
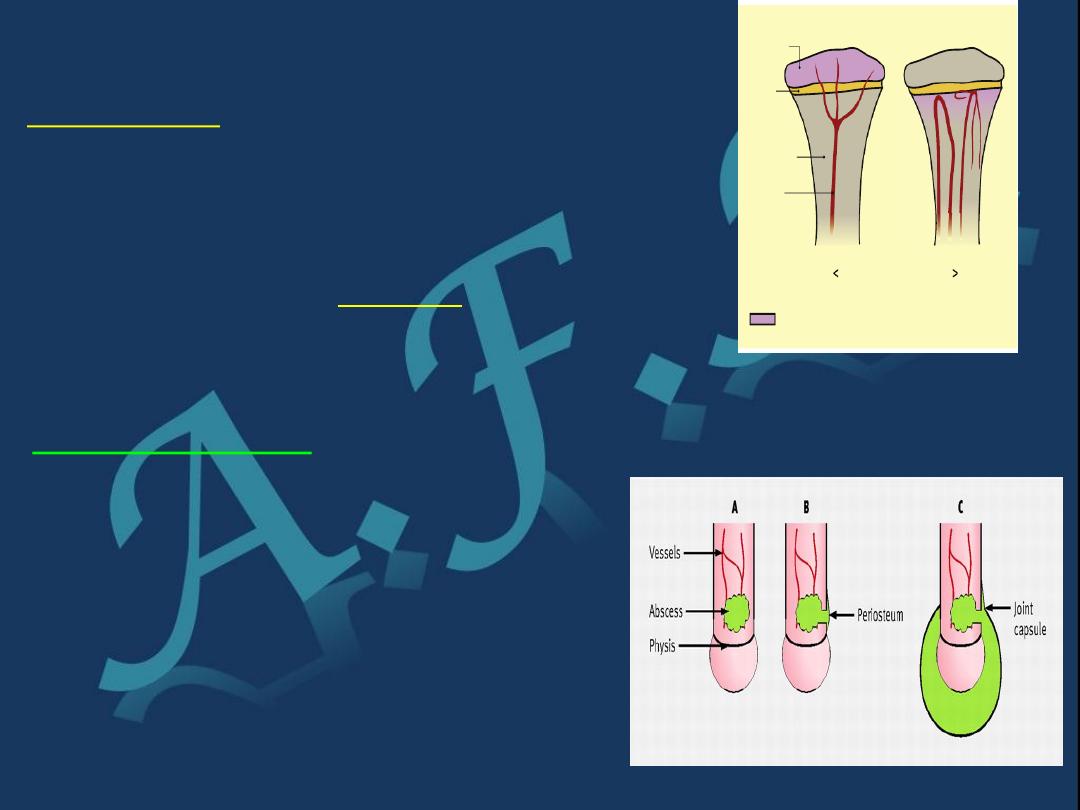
In infants
, in whom there are still
anastomoses between metaphyseal
and epiphyseal blood vessels,
infection can also reach the
epiphysis.
While in
adults
, the
infection appears almost anywhere.
Pathology
;-
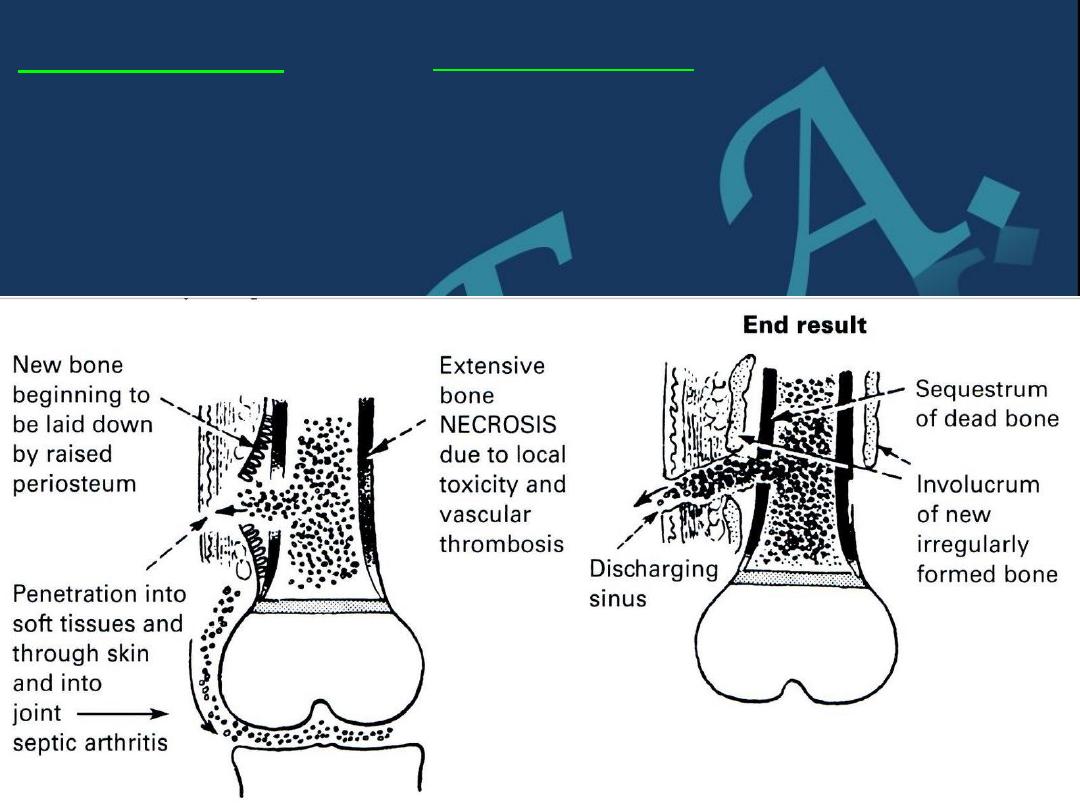
1) inflammation.
2) suppuration .
3 ) bone necrosis.
4 ) reactive new bone formation &
5) finally resolution & healing or
change to chronic inf.
204)4 )
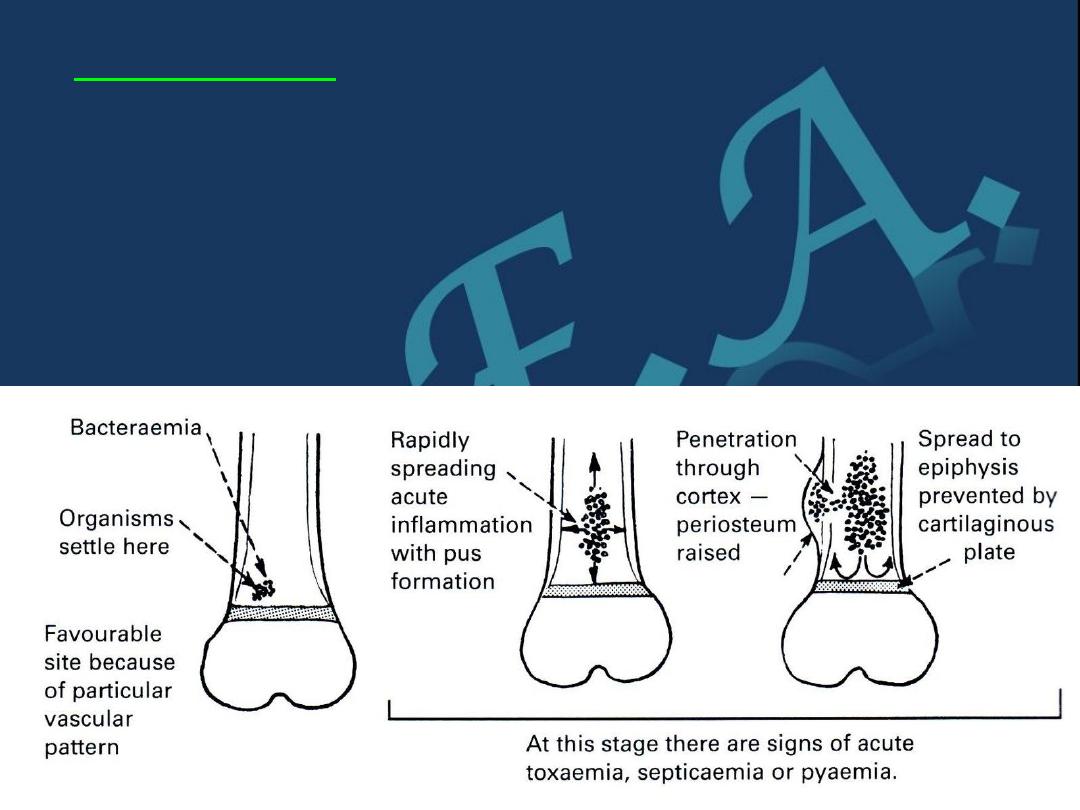
1) Inflammation:
vascular congestion, exudation of fluid and
infiltration by polymorphonuclear leucocytes. The Intra -
osseous pressure rises rapidly, causing intense pain, obstruction
to blood flow and intravascular thrombosis with high risk of
impending ischemia and resorption due to a combination of
phagocytic activity and the local accumulation of cytokines,
growth factors, prostaglandin & bacterial enzyme
Pathology;_
2
) Suppuration
.
By the second day pus appears in the medulla and forces its way
along the Volkmann's canals of the metaphyseal bone to the surface
where it forms a subperiosteal abscess From the subperiosteal
abscess pus can spread along the shaft, to re-enter the bone at
another level or burst into the surrounding soft tissues.
2) Suppuration
where the metaphysis is partly
intra-capsular (e.g. at the hip,
shoulder or elbow) pus may
discharge through the
periosteum into the joint
.
In infants
, the infection often
extends into the epiphysis & then
into the joint, ..while in
older
children
the epiphyseal plate
(physis) acts as a barrier to the
direct spread.
.
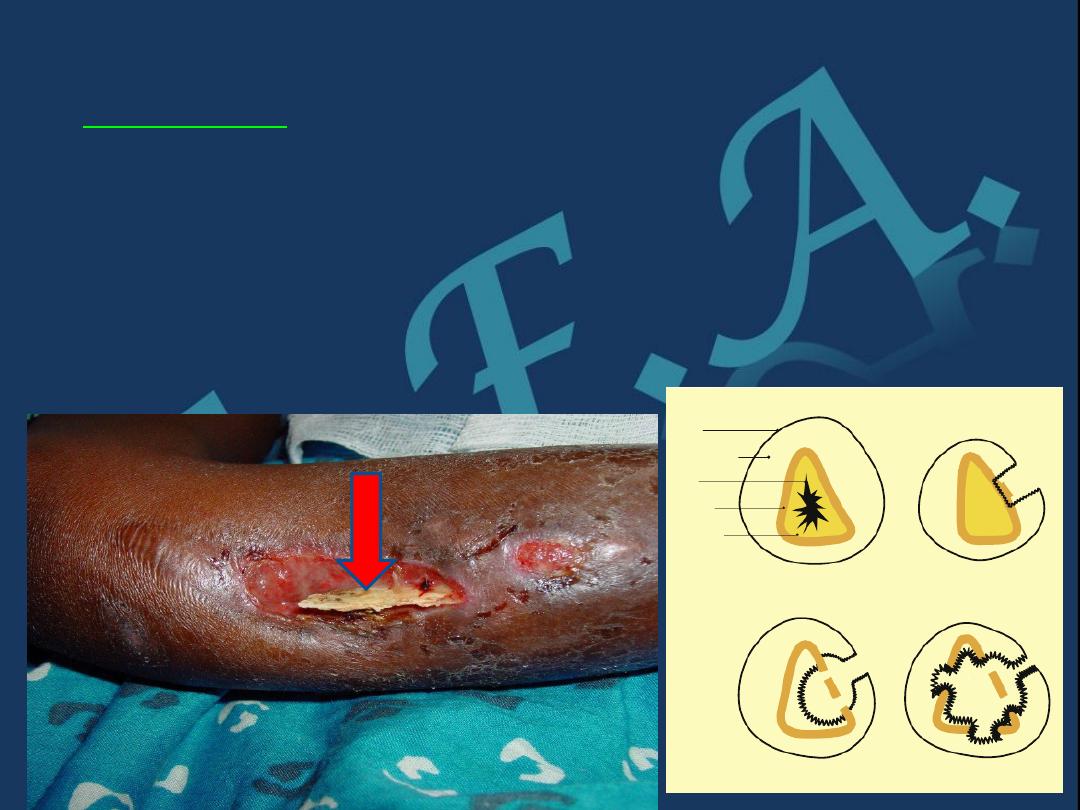
pathology
3)Necrosis
The rising intraosseous pressure, the vascular
stasis, infected thrombosis &periosteal stripping , will
increasingly compromise the blood supply, & by end of the
week there is evidence of necrosis, Pieces of bone separate
sequestrum ( means dead bone fragment) which later on acts
as a foreign body causing persistent purulent discharge
through a sinus.
Sequesterum
4) New bone formation:
New bone forms from the deep layers
of the periosteum, and with time the
new bone thickens to form
involucrum
enclosing the infected tissue & sequestra.,
,If the infection persists pus
may discharge through perforations
(cloacae)
in the involucrum and tract
by sinuses to skin surface
(the
condition now is established as
( chronic osteomyelitis)
5) Resolution:
If infection is controlled & intraosseous
pressure is released,,the bone will
heal although it may remain thickened.
involucrum
sequestrum
Clinical features
Patient usually is a child presents with
pain, malaise
and , in
neglected cases there may be
toxemia.
.Sometimes there is
a history of sore throat, skin lesion or trauma.
On examination:
The limb held immobile ,Local tenderness near one of the
joints. …Joints movement is restricted and painful
Local tenderness, swelling, warmth and oedema are late signs
and signify presence of pus.
In infants
(especially newborn) the constitutional
disturbance can be absent or mild; the baby fails to
thrive, drowsy but irritable
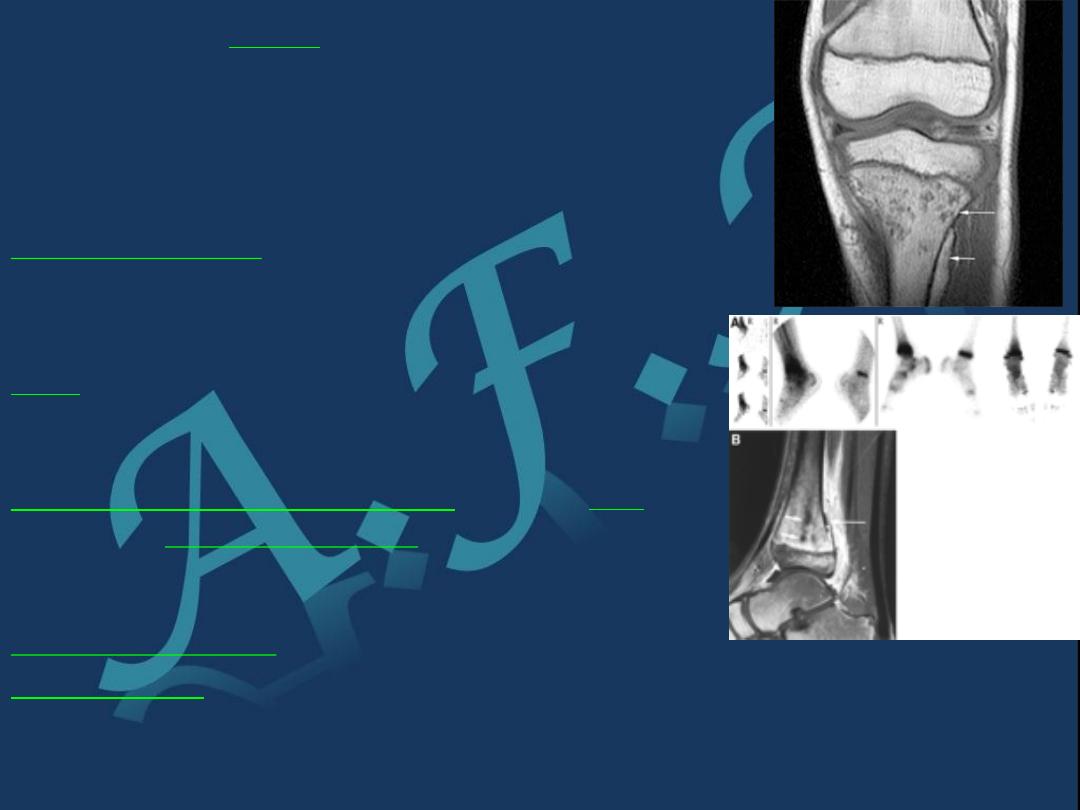
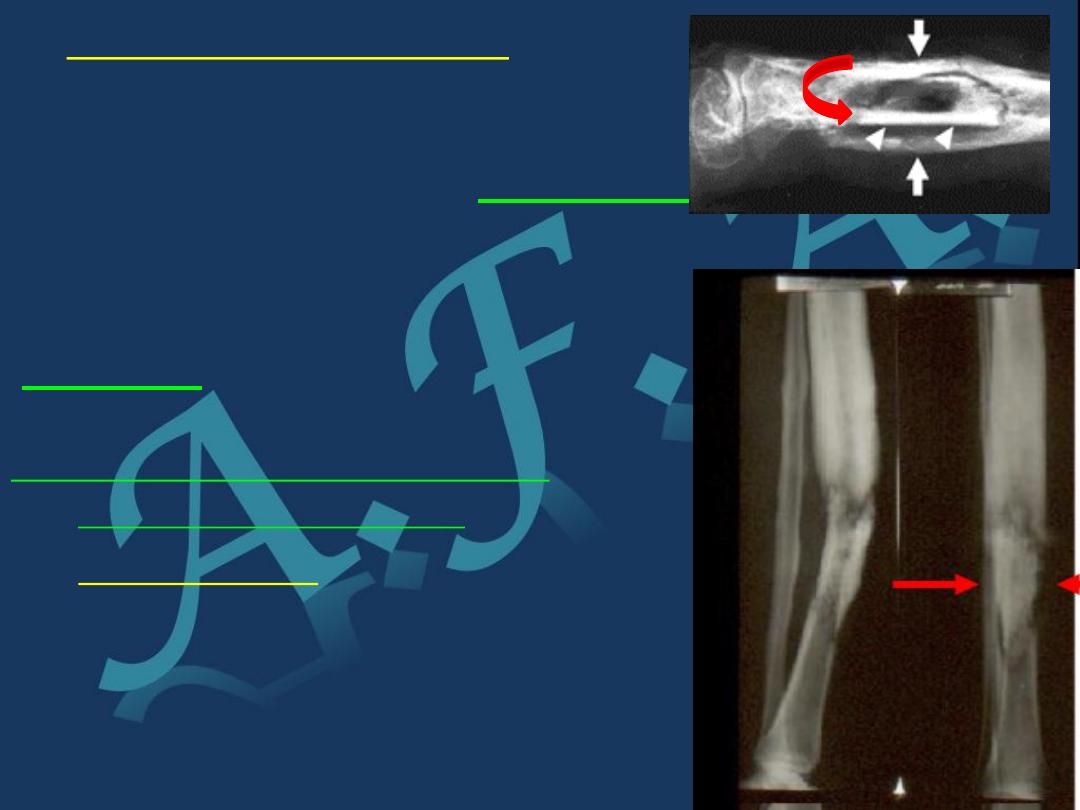
Imaging:
X-Ray:
For the first 10 days no bone abnormalities, only soft tissue
swelling. Later there is rarefaction of the metaphysis and
periosteal new bone formation. With healing there is
sclerosis. Sometimes there are sequestra separates from
the surrounding bone by radiolucent line.
Bone scintography:
Shows osteoblastic activity, it is used
for. Localization of pathologic process to anatomic area
at earlier stage. Also useful for finding out
polyostotic lesions especially in neonate
MRI:
Detect marrow changes secondary to infection
at early stage & help in evaluation of potential
spread of infection to adjacent bone or joint.
Laboratory investigations
:
Elevated
ESR
…
Elevated
C-reactive protein
.(Both are markers of
acute phase response.)(In addition C-reactive protein (CRP)
is used as monitor for response to treatment.)
Raised WBC count
with polymorphonuclear .
Blood culture
: may be positive here, blood must be taken before
the start with antibiotic therapy. Aspiration from the site of
infection specimen is sent for gram-stain and for culture (also it
should be done before antibiotic therapy).
Differential diagnosis
1)Acute rheumatism
.
There is pain, swelling, localized tenderness; but the onset is gradual pain
less acute and swelling confound to a joint.
2)Erysipelas.
Because redness of the skin but there is less pain and general toxaemia
.The margin of the red area is raised.
3)Haemophilia.
Muscle bleed or Bleeding into a joint produce marked local pain and
tenderness with general malaise and fever..
4)Cellulitis.
In the region of the metaphysis. In pure cellulitis there is no intense pain
and general malaise is less.
5)Acute pyogenic arthritis
.
Manifestation in the joint is more ,,spasm of muscle is more marked, joint
movement are more limited, effusion is earlier than in osteomyelitis.
6) Ewing’s tumour or osteosarcoma
.
Much less intense general illness, little inflammatory reaction
,,Radiological signs are obvious and earlier than osteomyelitis

Treatment:
General
;- Complete bed rest, rehydration, sedation and analgesia and
Antibiotics:
Should be started immediately and not waiting for the result of
culture and aspirate. ..The selection of appropriate antibiotics
is dependant on the knowledge of the microbiology of the bone
and joint infection
The initial treatment for old children
. And previously fit adult who
probably have staphylococcal infection are started on
intravenous flucloxacillin and fusidic acid
. (this may have to be
changed when the result of sensitivity tests are known) ..
This
treatment is to be continued until there is clinical and
laboratory evidence of improvement usually 1-2 weeks then this
is followed by oral antibiotics for another 3-6 weeks.
In children under age of 4 years
(who might have a high incidence
of haemmophilus influenza infection) or any other gram
negative organism seen in the direct gram stain smear, it is
advisable to give one of the
cephalosporins new generation
. (
Claforan generic name: cefotaxime )
Local treatment.
Splintage and traction
.
A splint is desirable, but it should not conceal the affected
area. With acute osteomyelitis of upper femur: traction is
needed to prevent possible hip dislocation.
Drainage.
If antibiotics are given early surgery for drainage is not necessary but
surgery is indicated: A) If pyrexia and local tenderness persist for
more than 24 hours after adequate antibiotics. B) Subperiosteal
abscess.,,Overlying oedema is useful sign..Pus should be evacuated
surgically. This will also allow the organism to be identified
Complications:
1) Spread
.
Infection may spread to Joint (septic arthritis)..or
Other bones (metastatic osteomyelitis)
…..
2)
Growth disturbance
: if the physis damaged
there may be shortening or deformity.
3) Persistent infection
Treatment of acute
osteomyelitis
must be prompt and effective ‘too little,
too late’ treatment may result in chronic osteomyelitis.
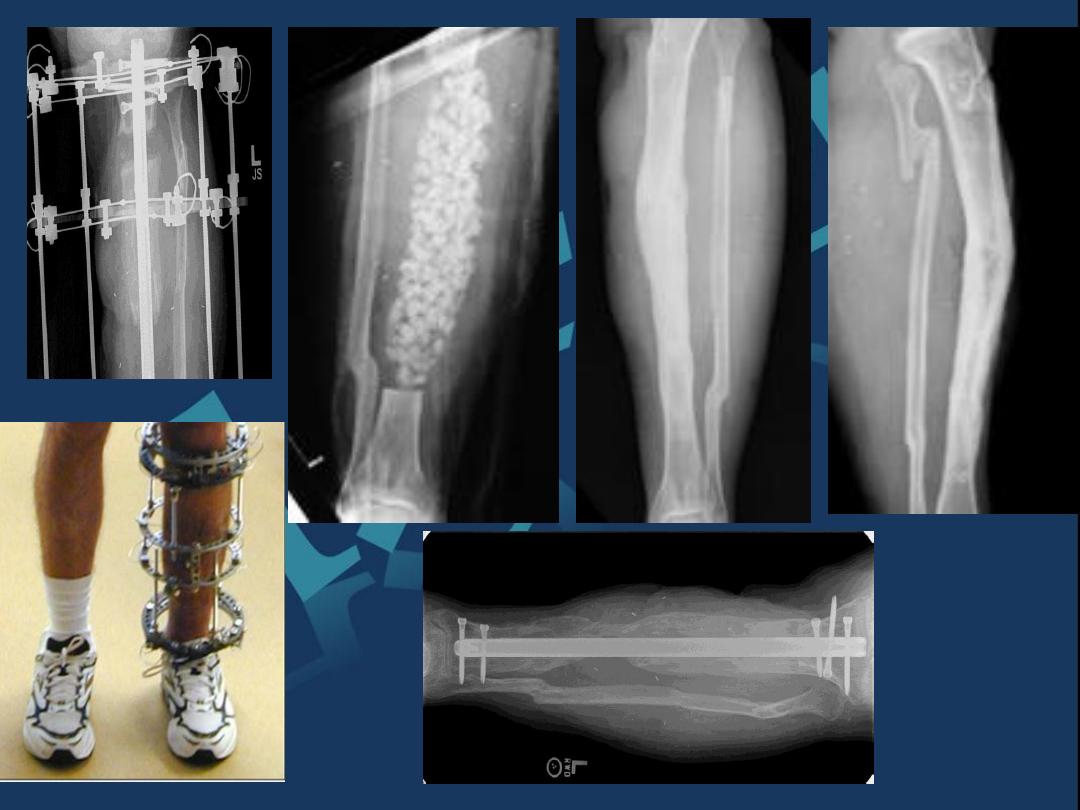
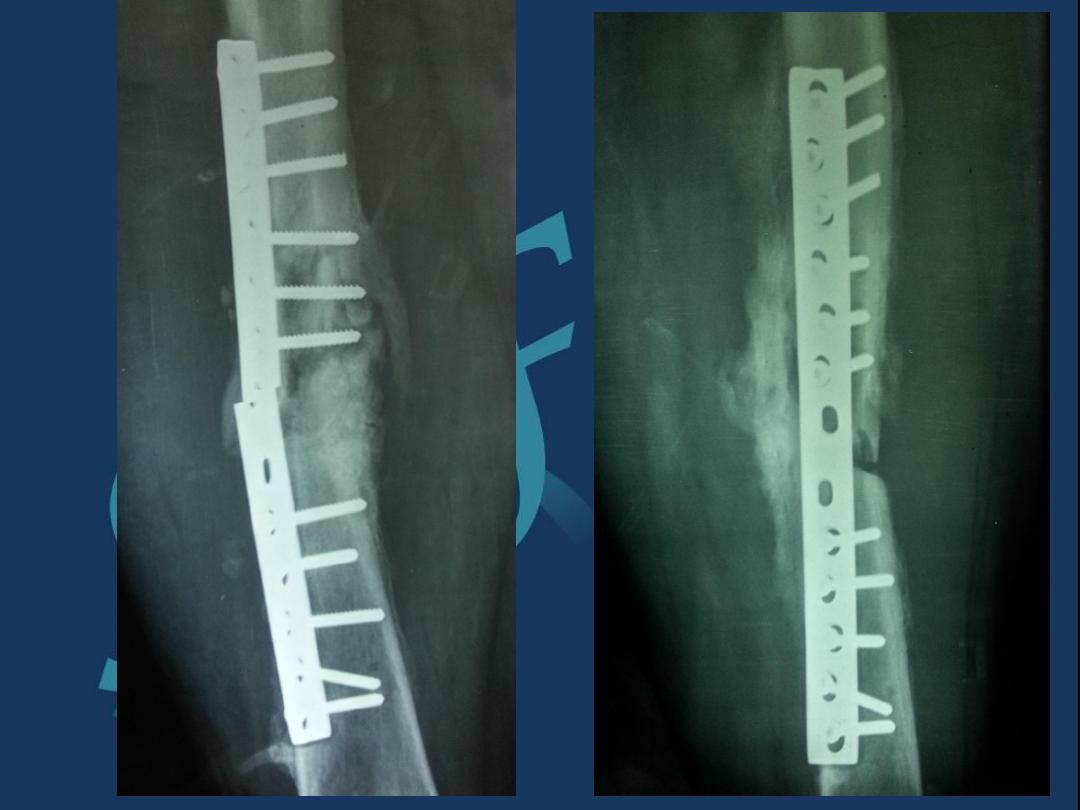
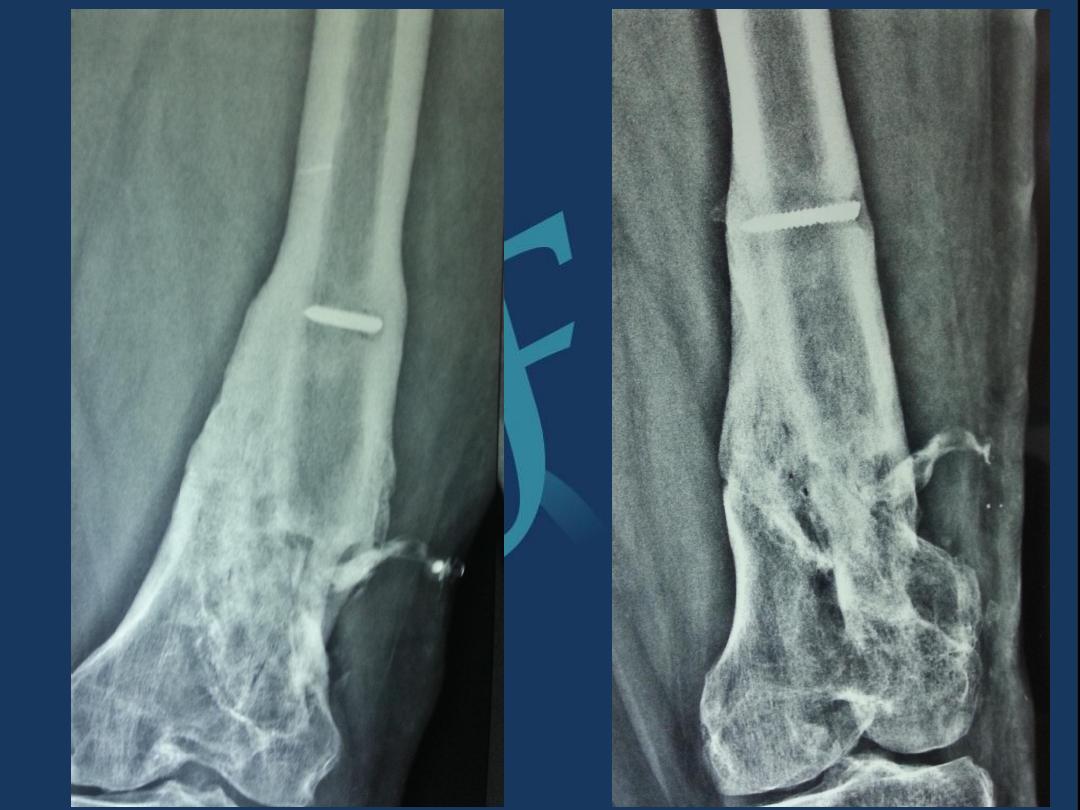
Post traumatic and post operative osteomyelitis.
1)
Post
traumatic osteomyelitis.
An open fracture may become infected
It is the usual cause of acute osteomyelitis
in adult.
Bacteriology
:
The causative organism maybe multiple but staphylococcus aureus
is the most common one
.
Clinical features:
Fever, pain, swelling over the site of fracture.
The wound is inflamed and there may be seropurulant discharge
.
Investigations:
Elevated ESR and C-reactive protein (CRP)
,
Leucocytosis.
,,
Wound swab sent for culture and sensitivity to
identify the causative organism
.
Treatment:
The wound should be left open for inspection and
frequent dressing, and then delayed primary closure for fewdays
and the fracture is fixed
by external fixator
.
Appropriate antibiotic should be given from the beginning
.
2) Post operative
osteomyelitis
.
;-
It is not uncommon.
,,,,,
The incidence in
general hospital is 3-5%
Predisposing factors.;- Debility
.
,,
Previous infection,,Corticosteroid
therapy. ,,
,
Haematoma formation.
•There is an increased risk with the use of foreign material (metal, plastics)
for internal fixation or joint replacement.
Treatment: Prophylactic
•Cleans surgical environment.
•Metaculous operative technique and careful heamostasis.
•The high risk situations, prophylactic antibiotics should be given.
In established infection
,,,
As for post traumatic above.




Sub-acute heamatogenous
osteomyelitis [Brodies abscess]
Sometimes because of the low virulence of the microorganism
and good resistance of the host; a mild form of osteomyelitis is
found.
Incidence:
Patient is usually child or adolescent.
Clinical features:
Pain n
ear one of the large joints for several weeks.
X-Ray
•Typically shows small oval radiolucent area
surrounding
by sclerotic bone (the classical brodies
abscess).
Differential diagnosis
:
It is early mistaken far osteoma (a benign bone
tumour) diagnosis is made after exploration.
Treatment:
The abscess is surgically
opened under antibiotic cover.
Chronic Osteomyelitis
It is used to be a sequel of acute haemtogenous infection, but now adays it is
more frequently follows open fracture or postoperative complication.
Pathology:
There is destruction of bone that follows acute infection leaving sequestra
surrounded by dense sclerotic bone.
The imprisoned sequestra provoke a chronic seropurulent discharge, that
escape through a sinus. Bacteria may remain dormant for years giving rise to
recurrent flare of acute infection.
Clinical features:
Pain, pyrexia, redness and tenderness: recurrence or ‘flare’ of infection
Or with discharge sinus.
Imaging:
•X-Ray: shows area of rarefaction surrounded by sclerosis.
And sometimes with sequestra.
•Sinogram helpful to localize the site.
•Bone scan: useful for revealing hidden foci of infection.
Treatment:
•Conservative
:
Sinus maybe painless needs dressing.
Flare often settles within few days with antibiotic therapy most antibiotic fail to
penetrate the fibrous tissue or sclerotic bone barriers; fusidic acid and
cephalosporin are exception and may be useful.
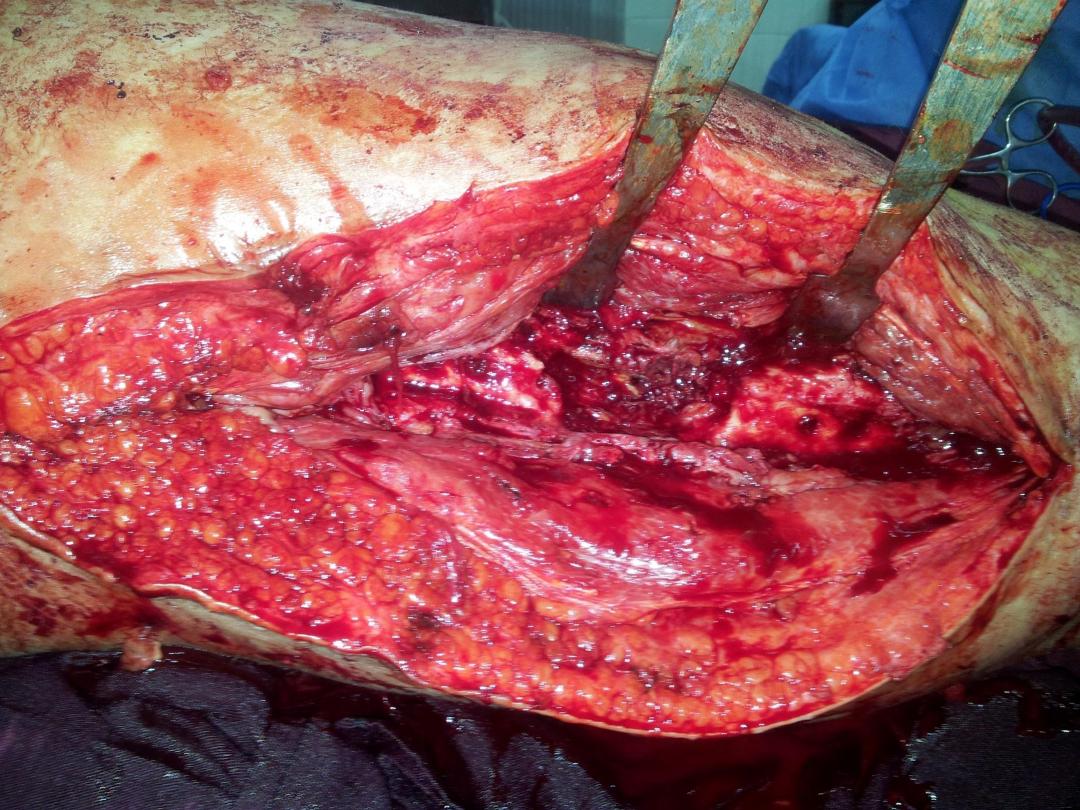
Surgical:
When abscess is formed, it should be incised and drained.
Sequestrectomy (removal of sequestrum) when a sequestra is radiological
visible after sequestrectomy the dead space should be injected with antibiotic
solution and then allowed to fill with granular tissue, sometimes when the
cavity is big, it needs bone graft muscle flap.
Complications
:
1)
Pathological fracture: when the bone is much weakened by
disease.
,, ,,
2)
Malignancy: chronic draining sinus may be
complicated by malignant transformation and develop squamous
cell carcinoma [Marjolins’s ulcer]
,,,,,
3)
Amyloidosis may complicate
long continued chronic osteomyelitis, with persistent discharge of
pus.



Quiz
Group A
:- Define osteomyelitis ,,Enumerat its
types & the methods of spread ?
Group B
;- what the clinical featuers & presention
of a child with acute osteomy ilis of the upper tibia
?Write a short nots about its lab investigation ?
Group C
:-
what are the differential DX. Of an
osteomylitius & enumerate the steps of treatment

Tuberculosis
Incidence:
Common in Asian and African countries, it is on the increase, especially in our country.
•Bones and joints are affected in 5% of the patients.
•In endemic areas with pulmonary tuberculosis; the skeletal tubercolosis is mostly seen in
children and young adults.
•In non-endemic areas, tuberculosis appear in patients with chronic debilitating disorder or
immunocompromized patients (e.g AIDS)
Causative organisms:
Is mycobacterium tuberculosis.
….
Human>bovine type.
Sites:
Mycobacterium TB: has a predilection for the vertebral bodies and large synovial joints.
Pathology:
•Route of infection: haematogenous spread from lungs or intestine.
•Inflammation: chronic inflammatory reaction develops, characteristically leading to granuloma
formation and caseation.
•Abscess formation: spread to soft tissue leads to subacute abscess (cold abscess) which may
track along tissue planes and “pointes” somewhere quite remote from the original site of bone
infection.
•Sinus formation: someties the abscess ruptures and the infected material may discharge through
the skin leading to chronic tuberculous sinus.
•Secondary infection: the sinus may provide a route for secondary infecting pyogenic organisms.
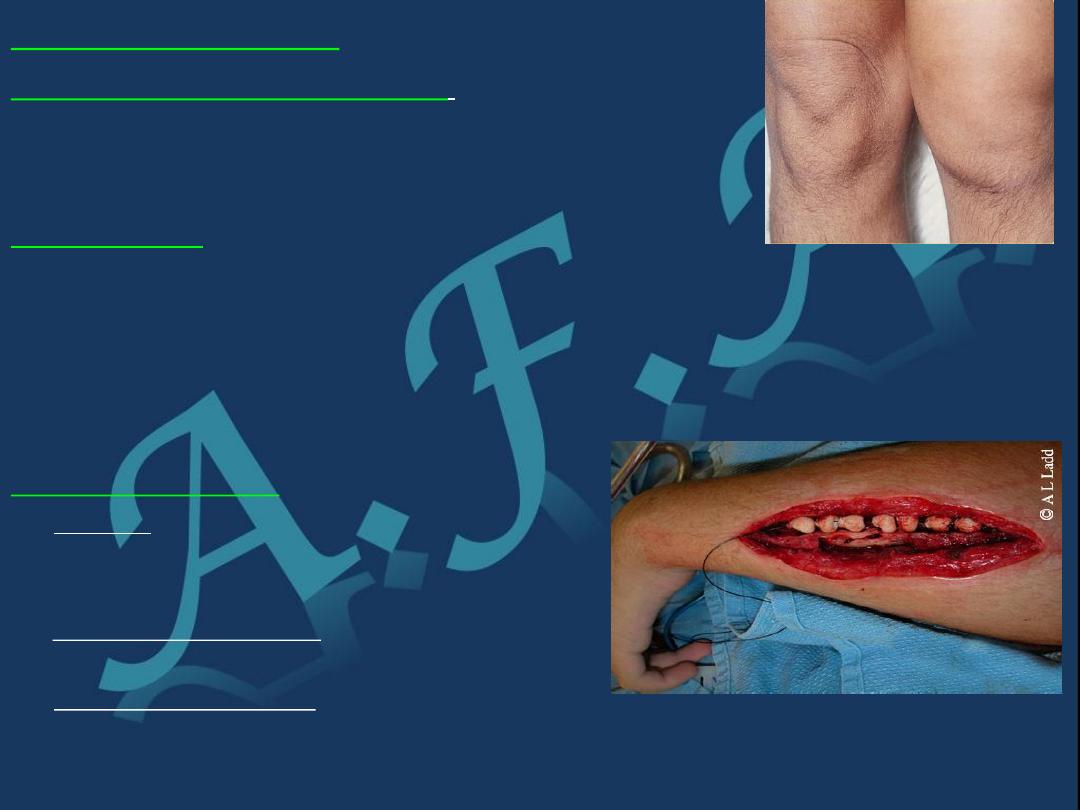
Joint tuberculosis
•It may start in the synovium, the synovial membrane is much
thickened by the inflammatory reaction which is of a characteristic
type. With round cell infiltration and giant cell system.
•Or it may start in the nearby metaphysis and then spread across the
physis through the articular surface into the synovial cavity.
•Site: usually monoarticular, and affecting a large joint (Hip and knee
most common).
Shoulder and ankle: less frequency.
•If the condition is not arrested, the articular surface is destroyed.
•Healing is by fibrosis if it occurs before the articular cartilage and
bone have damaged, the function of the joint is restored virtually to
normal.
But if the cartilage or bone has been damaged before healing; there will
be a permanent damage resulting in a tight ‘fibrous ankylosis’ of the
joint.
Clinical features:
•Usually there is impairment of the general health.
•Children and young adults are mostly affected; often there is a
•history of contact with a patient with pulmonary TB.
They present with:
•Pain.
•Swelling (in the superficial joint).
•Muscle wasting (characteristic of tuberculous arthritis).
•Synovial thickening is often permanent.
•Limitation of the movement of the joint in every direction.
•Joint stiffness and deformity when there is
p
rogression of the articular
erosion. May be sinus formation in late cases.

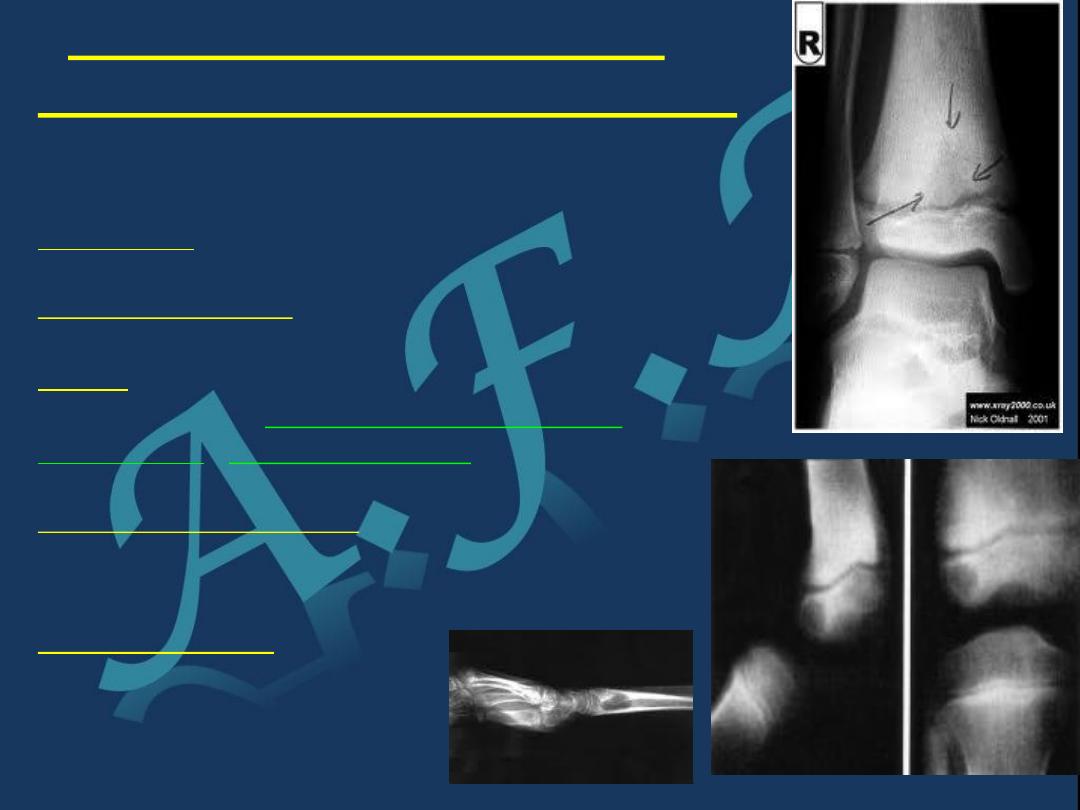
Imaging:
•X-ray:
•Soft tissue swelling.
•The earliest change is diffuse bone rarefaction throughout a wide area of bone adjacent to the
joint.
•In early stages: joint space retained.
•In later stages:
•Narrowing and irregularity of the joint space.
•Bone destruction on both sides of the joints.
•Cyctic changes may appear.
•MRI:
Determine the size and the location of the soft tissue component (i.e lymphadenitis, cold abscess
formation, marrow changes.)
Investigation:
•ESR: usually raised in active stage, gradually decrease, indication of healing.
•Mantoux test: positive.
•Biobsy from synovial membrane for histological examination is necessary for diagnosis. (It shows
the typical histological features of TB).
•Culture: incubation of the micro-organism in guinea pig may prove its tuberculous nature.
Diagnosis:
May be delayed in areas where TB is not common, but feature suggestive of TB include:
•Involvement of one joint.
,,,,
The long history. Marked synovial thckenning.
•Marked muscle wasting.
…
Periarticular osteoporosis.
Differential diagnosis:
•Rheumatoid arthritis: may resemble TB arthritis but the above 5 criteria
• differentiate it from rheumatoid arthritis.
•Chronic pyogenic osteomyelitis with acute or subacute flare.
There’s fever, local inflammatory signs, radiological changes:
sequestra, more sclerosis.
Treatment:
•Antituberculous chemotherapy: it is the mainstay of treatment.
Choice: combination of the following antituberculous drugs (start with a triple therapy),
drugs are:
(streptomycin, rifampicin, isoniazide(INH), ethambutol and pyrazinamide).
•Local treatment:
•Rest.
•Traction.
•Occasionally operation (aspiration or drainage of an abscess).
•Splintage (in early stages) continued for several months, by which time, it will be clear
whether the joint has been saved.
•If the articular surfaces are destroyed the joint is immobilized until all signs of disease
actively have disappeared and then:
If the disease remains quiescent then arthrodesis or joint replacement is
considered

Complication:
•Sinus formation.
•Secondary infection through sinus tract.
Spread of disease to another part of the body
