• Dr asmaa s
• (PATHOGENESIS & MANAGEMENT)
•
• WHAT IS OSTEOMYELITIS
• FACTORS PREDISPOSING TO OSTEOMYELITIS
• PATHOGENESIS OF OSTEOMYELITIS
• TYPES OF OSTEOMYELITIS
• PATHOGENESIS• CLINICAL FEATURES
• HISTOLOGY
• RADIOLOGY
• MANAGEMENT
• I. Suppurative osteomyelitis:
• Acute suppurative osteomyelitis• Chronic suppurative osteomyelitis
• Nonsuppurative osteomyelitis
• Chronic focal sclerosing osteomyelitis• Chronic diffuse sclerosing osteomyelitis
• Garre's chronic sclerosing osteomyelitis (proliferative osteomyelitis)
• III. Osteoradionecrosis /Radio osteomyelitis
• OSTEOMYELITIS
• WHAT’S IN THE NAME?
• The word “osteomyelitis” originates from the ancient Greek words osteon (bone) and muelinos (marrow)• and literally means infection of medullary portion of the bone.
WHAT IS IT?
• It is an acute & chronic inflammatory process in the medullary spaces or cortical surfaces of bone that extends away from the initial site of involvement.• FACTORS PREDISPOSING TO OSTEOMYELITIS
• LOCAL FACTORS
• (decreased vascularity/vitality of bone)• Trauma. Radiation injury. Paget’s disease.
• Osteoporosis. Major vessel disease.• SYSTEMIC FACTORS
(impaired host defense)
• Immune deficiency states.
• Immunosuppression Diabetes mellitus.• Malnutrition. Extremes of age.
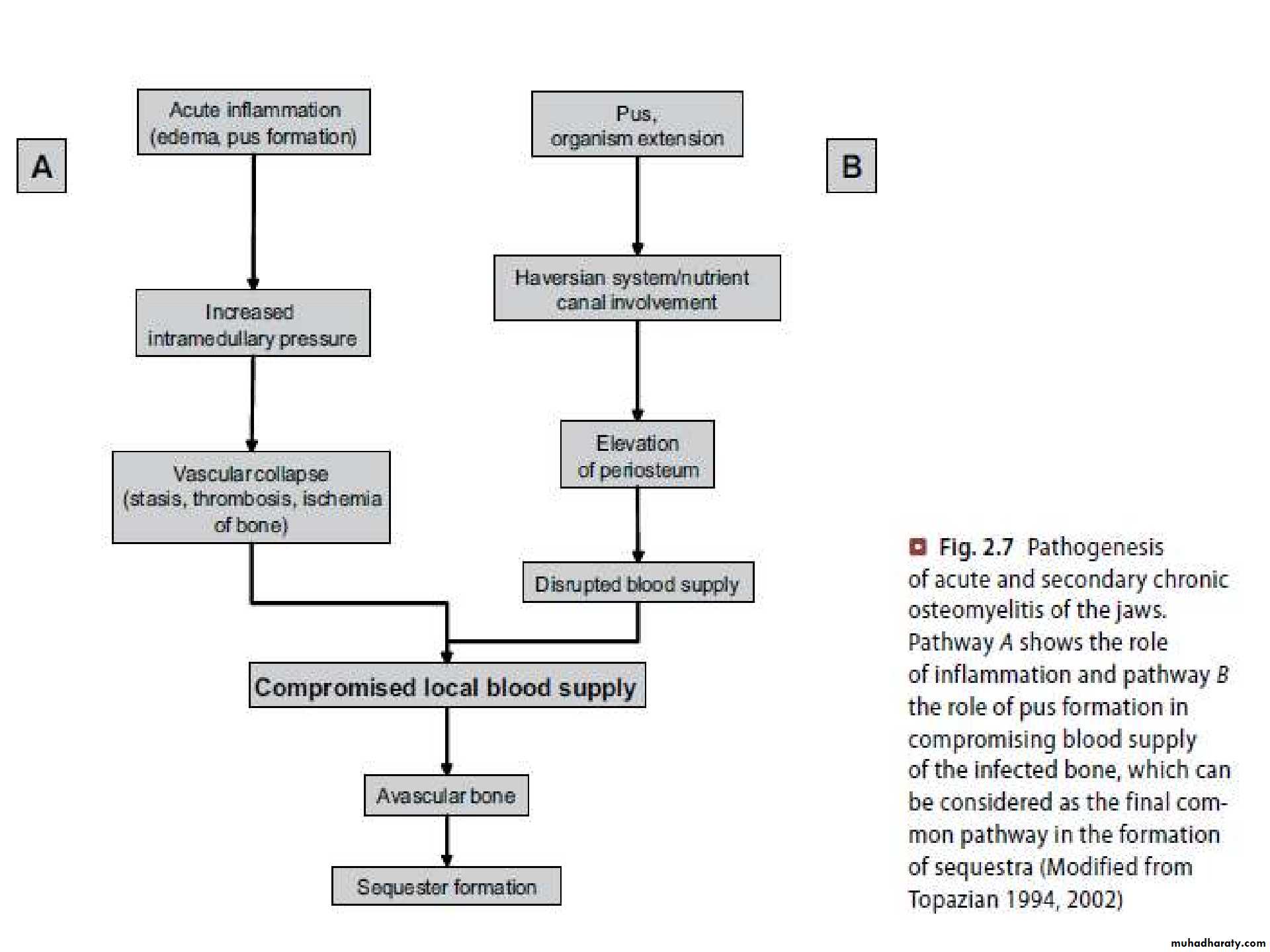
• PATHOGENESIS OF OSTEOMYELITIS
• Inflammatory process of entire bone including cortex & periosteum, not just confined to endosteum• Inflammatory condition beginning in medullary cavity & havarsian system & extending to involve periosteum of affected area
• Local factors decreases the vitality of bone Systemic conditions comprises the defense system of the host
(IV) PATHOLOGY
• Acute inflammation of marrow tissues
• Spread of exudate along the marrow spaces
• Thrombosis of vessels due to compression
• Necrosis of bone
• Liquefaction of necrotic tissues
• Lifting of periosteum causing further necrosis
• Finally ,Osteoclastic activity >>> SEQUESTRUM• TYPES OF OSTEOMYELITIS
• SUPPURATIVE OSTEOMYELITIS• FOCAL SCLEROSING OSTEOMYELITIS
• DIFFUSE SCLEROSING OSTEOMYELITIS
• PROLIFERATIVE PERIOSTITIS
• ONSET OF DISEASE
• 4 WEEKS
Acute suppurative
osteomyelitis
• Chronic suppurative osteomyelitis
• t
• Onset of disease
• Deep bacterial invasion into medullary & cortical bone
• SUPPURATIVE OSTEOMYELITIS
• SUPPURATIVE OSTEOMYELITIS• Source of infection is usually an adjacent focus of infection associated with teeth or with local trauma.
• It is a polymicrobial infection, predominating anaerobes such as Bacteriods, Porphyromonas or Provetella.
• Staphylococci may be a cause when an open fracture is involved.
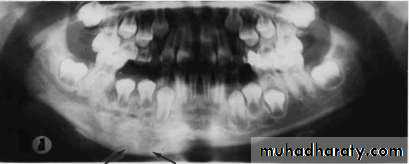
• Mandible is more prone than maxilla as vascular supply is readily compromised.• Cropped panoramic radiograph of suppurative osteomyelitis at the right side of mandible.
• ACUTE SUPPURATIVE OSTEOMYELITIS
• Organisms entry into the jaw, mostly mandible, compromising the vascular supply• Medullary infection spreads through marrow spaces
• Thrombosis in vessels leading to extensive necrosis of bone
• Lacunae empty of osteocytes but filled with pus , proliferate in the dead tissue
• Suppurative inflammation extend through the cortical bone to involve the periosteum
Stripping of periosteum comprises blood supply to cortical plate, predispose to• further bone necrosis
Sequestrum is formed bathed in pus, separated from surrounding vital bone
• ACUTE SUPPURATIVE OSTEOMYELITISCLINICAL FEATURES
• EARLY :
• Severe throbbing, deep- seated pain.
• Swelling due to inflammatory
• edema.
• Gingiva appears red, swollen & tender.
• LATE :
• Distension of periosteum with pus.• FINAL:
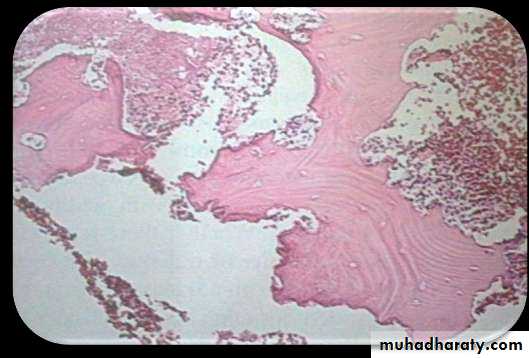
• Subperiosteal bone formation cause swelling to become firm.• HISTOLOGY
• Submitted material for biopsy predominantly consists of necrotic bone & is diagnosed as sequestrum• Bone shows:
• Loss of osteocytes from• lacunae.
• Peripheral resorption.
• Bacterial colonization.
• Acute inflammatory infiltrate consisting of polymorphonuclear leukocytes in haversian canals & peripheral bone.
• ACUTE SUPPURATIVE OSTEOMYELITIS
• ACUTE SUPPURATIVE OSTEOMYELITIS
• After sufficient bone resorption irregular, mot- eaten areas of radiolucency may appear.
• RADIOGRAPHIC FEATURES
• May be normal in early stages of disease . Do not appear until after at least 10 days.• Radiograph may demonstrate ill-defined radiolucency.
• MANAGEMENT
• ACUTE SUPPURATIVE OSTEOMYELITIS
• ESSENTIAL MEASURES
• Bacterial sampling & culture.• Emperical antibiotic treatment.
• Drainage.
• Analgesics.
• Specific antibiotics based on culture & sensitivity.
• Debridement.
• Remove source of infection, if possible.
• ADJUNCTIVE TREATMENT
• Sequestrectomy.• Decortication (if necessary)
• Hyperbaric oxygen.
• Resection & reconstruction for
• extensive bone destruction.
• ACUTE SUPPURATIVE OSTEOMYELITIS
• COMPLICATIONS• Rare but include:
• Pathological fracture
• Extensive bone destruction.
• Chronic osteomyelitis Inadequate treatment.
• Cellulitis Spread of virulent bacteria.
• Septicemia Immuno-compromised patient.• CHRONIC SUPPURATIVE OSTEOMYELITIS
• Inadequate treatment of acute osteomyelitis• Periodontal diseases
• Pulpal infections
• Extraction wounds
• Infected fractures
• Infection in the medulllary spaces spread and form granulation tissue
• Granulation tissue forms dense scar to wall off the infected area
• Encircled dead space acts as a reserviour for bacteria & antibiotics have great difficulty reaching the site• CHRONIC SUPPURATIVE OSTEOMYELITIS
• CLINICAL FEATURES
• Swelling• Pain
• Sinus formation Purulent discharge Sequestrum formation Tooth loss• Pathologic fracture
• CHRONIC SUPPURATIVE OSTEOMYELITIS
• HISTOLOGY
• Inflammed connective tissue filling inter-trabecular areas of bone.• Scattered sequestra. Pockets of abscess.
• CHRONIC SUPPURATIVE OSTEOMYELITIS
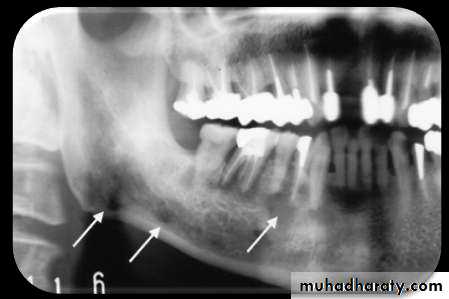
• RADIOLOGY
• Patchy, ragged & ill defined radiolucency. Often contains radiopaque sequestra.• Sequestra lying close to the peripheral sclerosis & lower border.
• New bone formation is• evident below lower border.
• CHRONIC SUPPURATIVE OSTEOMYELITIS
MANAGEMENT
• Difficult to manage medically.• Surgical intervention is mandatory, depends on spread of process.
• Antibiotics are same as in acute condition but are given through IV in high doses.
• SMALL LESIONS
• Curretage, removal of necrotic bone and decortication are sufficient.
• EXTENSIVE OSTEOMYELITIS
• Decortication combined with transplantation of cancellous bone chips.• PERSISTANT OSTEOMYELITIS
• Resection of diseased bone followed by immediate reconstruction with an autologous graft is required.• Weakened jawbones must be immobilized.
• FOCAL SCLEROSING OSTEOMYELITIS
• Also known as “Condensing osteitis”.
• Localized areas of bone sclerosis.• Bony reaction to low-grade peri-apical infection or unusually strong host defensive response.
• Association with an area of inflammation is critical.
• FOCAL SCLEROSING OSTEOMYELITIS• CLINICAL FEATURES
• Children & young adults are affected.• In mandible, premolar & molar regions are affected.
• Bone sclerosis is associated with non-vital or pulpitic tooth.
• No expansion of the jaw.
• HISTOLOGY• Dense sclerotic bone. Scanty connective tissue. Inflammatory cells.
• FOCAL SCLEROSING OSTEOMYELITIS
• RADIOLOGY
• Localized but uniform increased radiodensity related to tooth. Widened periodontal ligament space or peri-apical area.
• Sometimes an adjacent radiolucent inflammatory lesion may be present.
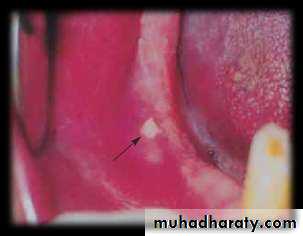
• Increased areas of radiodensity surrounding apices of nonvital mandibular first molar• MANAGEMENT
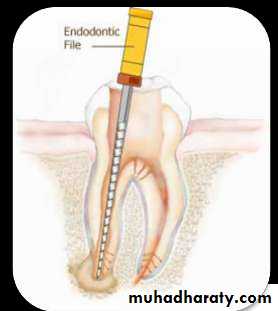
• Elimination of the source of inflammation by extraction or endodontic treatment.• If lesion persists and periodontal membrane remains wide, reevaluation of endodontic therapy is considered.
• After resolution of lesion, inflammatory focus is termed as bone scar.
• FOCAL SCLEROSING OSTEOMYELITIS• DIFFUSE SCLEROSING OSTEOMYELITIS
• It is an ill-defined, highly controversial, evolving area of dental medicine.
• Exact etiology is unknown.
• Chronic intraosseous bacterial infection creates a smoldering mass of
• chronically inflammed granulation tissue.• DIFFUSE SCLEROSING OSTEOMYELITIS
• CLINICAL FEATURES
• Arises exclusively in adult-hood with no sex pre-dominance.• Primarily occurs in mandible. No pain.
• No swelling.
• HISTOLOGY
• Bone sclerosis and remodling. Scanty marrow spaces.• Necrotic bone separates from vital bone & become surrounded by granulation tissue. Secondary bacterial colonization often is visible.
• RADIOLOGY
Increased radiodensity may be seen surrounding areas of lesion.
• DIFFUSE SCLEROSING OSTEOMYELITIS• Diffuse area of increased radiodensity of Rt. Side of mandible
• MANAGEMENT
• Elimination of originating sources of inflammation• via extraction & endodontic treatment.
• Sclerotic area remain radiographically.
• DIFFUSE SCLEROSING OSTEOMYELITIS
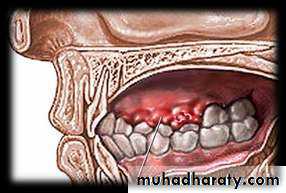
• PROLIFERATIVE PERIOSTITIS
• Also known as “ Periostitis ossificans” & “Garee’s osteomyelitis”.• It represents a periosteal reaction to the presence of inflammation.
• Affected periosteum forms several rows of reactive vital bone that parallel each other & expand surface of altered bone.PATHOGENESIS
• The spread of low-grade, chronic apical inflammation through cortical bonePeriosteal reaction occurs
Stimulates proliferative reaction of periosteum• PROLIFERATIVE PERIOSTITIS
• CLINICAL FEATURES
• Affected patients are primarily children & young adults.• Incidence is mean age of 13 years. No sex predominance is noted.
• Most cases arise in the premolar & molar area of mandible.
• Hyperplasia is located most commonly along lower border of mandible.
• Most cases are uni-focal, multiple quadrants may be affected.
• PROLIFERATIVE PERIOSTITIS
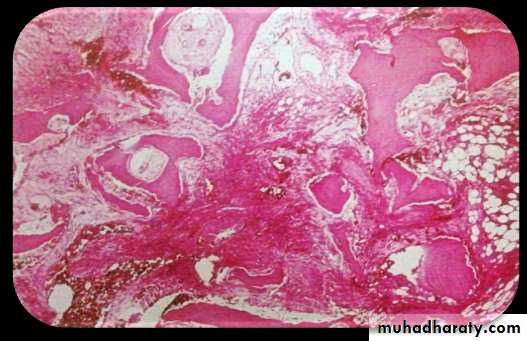
• HISTOLOGY
• Parallel rows of highly cellular• & reactive woven bone .
• Trabeculae are frequently oriented perpendicular to surface.
• Trabeculae sometimes form an interconnecting meshwork of bone.
• Between trabeculae, uninflammed fibrous tissue is evident.
• PROLIFERATIVE PERIOSTITIS
RADIOLOGY
• Radiopaque laminations of bone roughly parallel each other & underlying• cortical surface.
• Laminations may vary from 1-12 in number.
• Radiolucent separations often are present between new bone & original
• cortex.• PROLIFERATIVE PERIOSTITIS
• MANAGEMENT
• Removal of infection.• After infection has resolved, layers of bone will consolidate in 6-12 months .
• QUESTIONS• WHY IS MANDIBLE MORE PRONE TO OSTEOMYELITIS THAN MAXILLA?
• WHY RADIOGRAPHIC FEATURES IN ACUTE SUPPURATIVE OSTEOMYELITIS APPEAR AFTER 10- 14 DAYS OF DISEASE?
• REFRENCES:
• J.V. SOAMS 4TH EDITION.• NEVILLE & DAM 3RD EDITION.
• R.A. CAWSON 8TH EDITION.
• GOOGLE FOR IMAGES.