21 محرم 1435 هـ Pediatric Lec. by Dr.Haidar
25/11/2013
Birth asphyxia
Definition:
Perinatal asphyxia ( PA ) refers to an insult to the fetal or neonatal brain as a result of hypoxia occurring during labour &/or after delivery. When abnormal neurological activity such as impaired consciousness, disturbance in muscle tone or convulsion follows, a diagnosis of HIE is applied.
PA is one of the leading causes of perinatal death in both developed & developing countries (25% of all neonatal deaths in the developing countries have been found to be due to asphyxia).
Neonatal Evaluation and Resuscitation:
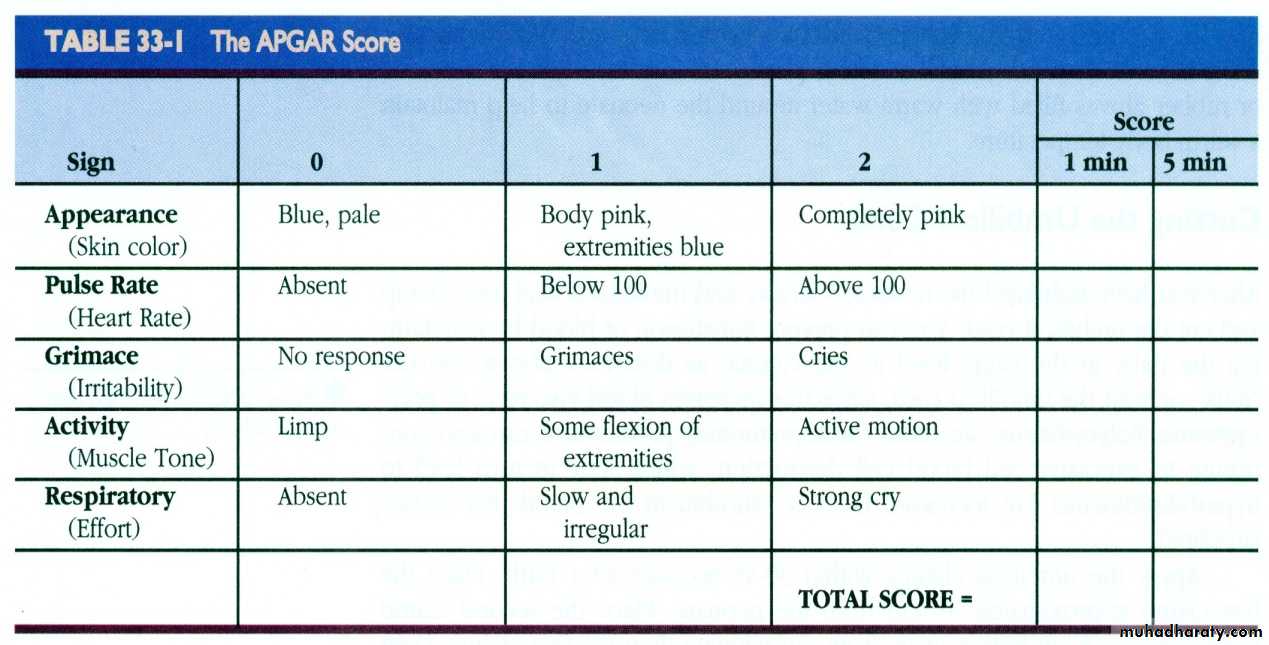
APGAR Scoring
A Appearance
P Pulse
G Grimace
A Activity
R Respirations
Apgar Score:
Total Score = 10score 7-10 normal
score 5-6 mild birth asphyxia
score 3-4 moderate birth asphyxia
score 0-2 severe birth asphyxia
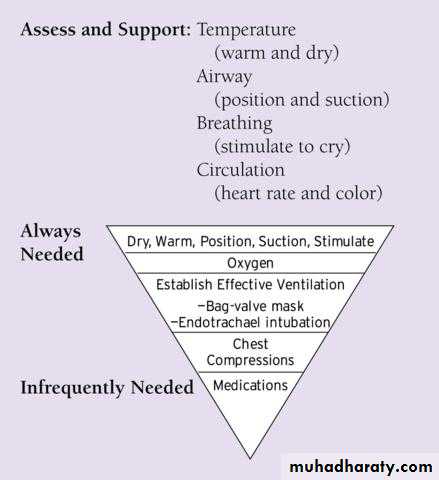
Neonatal Resuscitation
Risk factors:
a)Antepartum :Maternal diabetes Post-term gestation
Pregnancy induced hypertension Multiple gestation
Chronic hypertension Size-dates discrepancy
Previous Rh sensitization Maternal drug abuse
Previous stillbirth Maternal age >35 or<16
Bleeding in second or third trimester No prenatal care
Maternal infection Hypotension
Polyhydramnios or oligohydramnios Uterine tetany
b)Intrapartum :
Elective or emergency c/sPrecipitous labour, prolonged labour
Anemia ( severe hemorrhage or hemolysis )
Premature labour
Abnormal presentation
Rupture of membranes > 24 hours
Foul-smelling amniotic fluid
Massive blood loss
Use of general anesthesia
Prolapsed cord
Severe cardiac or pulmonary disease
Pathophysiology :
The initial response of hypoxic – ischemic insult is increase pulmonary vascular resistance & preferential perfusion of circulation to the brain, heart & adrenals.
The response to HIE is different between full term vs premature baby in that, in term baby, it usually cause focal or multifocal cortical infarcts & necrosis, whereas in premature baby, it cause PVL &/or IVH.
Systemic effects of Asphyxia :
Central nervous system
infarction,
intracranial hemorrhage,
cerebral edema,
seizure,
hypoxic-ischemic encephalopathy.
Cardiovascular
bradycardia,
ventricular hypertrophy,
arrhythmia,
hypotension,
myocardial ischemia,
poor contractility,
TR.
Respiratory system
apnea,
RDS,
pulmonary hemorrhage,
pulmonary hypertension,
cyanosis.
Renal
acute tubular necrosis,
bladder paralysis,
myoglobinuria.
Gastrointestinal tract
necrotizing enterocolitis ,
stress ulcer,
perforation,
adrenal hemorrhage.
Hematology
Disseminated intravascular coagulation
Metabolic
hypoglycemia,
hypocalcemia,
hyponatremia,
SIADH.
Integument
subcutaneous fat necrosis
Hypoxic-ischemic encephalopathy(HIE):
Hypoxic-ischemic encephalopathy is an important cause of permanent damage to central nervous system cells, which may result in- neonatal death
- manifest later as cerebral palsy or mental deficiency
Grading system of HIE :
Grade 1 :
mild encephalopathy with the infant being hyperalert, irritable & oversensitive to stimulation. There is evidence of sympathetic overstimulation with tachycardia, dilated pupils & jitterness. EEG is normal.
Grade 2 :
moderate encephalopathy with the infant displaying lethargy, hypotonia & proximal weakness. There is evidence of parasympathetic overstimulation with a low resting heart rate, small pupils & copious secretions. EEG is abnormal, & 70% of the infants will have seizures.
Grade 3 :
severe encephalopathy with the infant stuporous, flaccid & having absent reflexes. EEG is abnormal with decreased background activity &/or voltage suppression.
Investigations:
US of brain is of limited value except in premature baby.
CT scan has limited ability to identify cortical injury in 1st few days of life.
MRI is the preferred imaging because it has increased sensitivity & specificity.
Amplitude integrated EEG; it detect seizure activity & also it can determine which infants are at highest risk for significant brain injury in order to plan early intervention.
Treatment:
Before delivery: Fetal hypoxia is 1st indicated by IUGR & increase vascular resistance which should alert the obstetrician about the treatable causes of fetal distress.
During delivery: Fetal distress is indicated by bradycardia, decrease beat to beat variability, late (type 2) deceleration pattern & fetal scalp blood analysis may show acidosis (pH less than 7.20). These signs necessitate administration of high concentration of O2 to the mother & immediate delivery (prabably by C/S) .
After delivery: Asphyxiated baby is indicated by decrease Apgar score, so he/she need a vigorous resuscitation.
Seizures due to HIE is usually severe & should be treated by Phenobarbital (the best anticonvulsant in asphyxia), the loading dose may be given initially as 20 mg/kg, but can be given up to 40-50 mg/kg to control the seizure. Other anticonvulsants e.g Phenytoin 20 mg/kg or Lorazepam 0.1 mg/kg may be effective.
Systemic or Selective Cerebral Hypothermia sh. be done within the 1st 6 hrs after birth to a core temp. 33.5 C. It decrease the rate of apoptosis & suppresses production of neurotoxic mediators.
Other organ & systems involvement must be searched for & treated accordingly.
Prognosis :
It ranges from complete recovery to death depending on the timing & severity of the insult as well as the area of injury.Factors associated with poor prognosis include:
5-min Apgar score of 0-3,
fetal acidosis (pH less than 6.7),
coma,
apnea,
absent oculocephalic reflexes
refractory seizures.
Factors that predict death or severe cognitive & motor deficits include:
low Apgar score at 20 min,absence of spontaneous respiration at 20 min of age,
signs of other organs or systems involvement
persistence of abnormal neurological signs at 2 wk of age.
============================================
يقولون لي فيك انقباضٌ وإنما ** رأوا رجلاً عن موقفِ الذلِّ أحجماأرى الناسَ من داناهُمُ هان عندهم ** ومن أكرَمته عزةُ النفسِ أكرِما
ولم أقضِ حَقَّ العلمِ إن كان كُلَّمَا ** بدا طَمَعٌ صَيَّرتُه لي سُلَّما... وما زلتُ مُنحازاً بعرضيَ جانباً ** من الذلِّ أعتدُّ الصيانةَ مَغنما