21 محرم 1435 هـ Pediatric Lec.
27/12/2013
Approach to the management of Hyperbilirubinemia in Term Newborn Infant
Neonatal Hyperbilirubinemia:
Definition = (TSB) > 5 mg/dL
Significance:
Present in up to 60% of term newborns
Severe complications possible like Deafness, CP (kirnicterus)
Increase Kirnicterus 1990’s (related to early hospital discharge)
Recent concern
JACHO alert due to several case reports of kernicterus in healthy newborns
Term 35-38 weeks, dehydrated breastfeeding, and with extremely high bilirubin levels
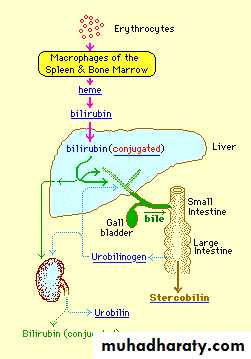
Bilirubin Production & Metabolism:
Classification:
BenignPhysiologic
Breast Milk
Breastfeeding
Pathologic
Physiologic Jaundice:
Features
Elevated unconjugated bilirubin
TSB generally peaks @ 5-6 mg/dL on day 3-4 and then declines to adult levels by day 10
Asian infants peak at higher values (10 mg/dL)
Exaggerated physiologic (up to 17 mg/dL)
Ethnic differences:
Exaggerated Hyperbilirubinemia (>12.8mg/dl)
4% African-Americans
6-10% Caucasian
25% Asian (>20mg% in 2%)
Effect of Type of Feeding:
2/3 of breastfeeding infants (BF) will have chemical jaundice for 2-3 weeks
TSB > 12mg% in 12% (BF) vs. 4% Formula Fed infants (FF)
TSB > 15mg% in 2% BF vs. 0.3% FF
Mechanism of Physiologic Jaundice:
Increased rbc’sShortened rbc lifespanImmature hepatic uptake & conjugationIncreased enterohepaticCirculationBreast Milk Jaundice:
Elevated unconjugated bilirubinProlongation of physiologic jaundice
Slower decrease to adult levels of bilirubin
66% of breastfed babies jaundiced into 3rd week of life
May persist up to 3 months
May have second peak @ day 10
Average max TSB = 10-12 mg/dL
TSB may reach 22-24 mg/dL
?Milk factor
Breast feeding Jaundice:
Elevated unconjugated bilirubin
Benign or pathologic
Elevated bilirubin in the 1st week of life tends to worsen breast milk jaundice during later weeks
Equivalent to starvation jaundice in adults
Mandates improved/increased breastfeeding
No water or dextrose supplementation
Formula OK
Pathologic Jaundice:
Features
Jaundice in 1st 24 hrs
Rapidly rising TSB (> 5 mg/dL per day)
TSB > 17 mg/dL
Categories
Increased bilirubin load
Decreased conjugation
Impaired bilirubin excretion
Increased Bilirubin Load:
@Hemolytic Disease:Features: elevated reticulocytes, decreased Hgb
Coomb’s + Rh incompatibility, ABO incompatibility, minor antigens
Coomb’s - G6PD, spherocytosis, pyrovate kinase deficiency
@Non-hemolytic Disease
normal reticulocytes
Extravascular sources – I.e. cephalohematoma
Polycythemia
Exaggerated enterohepatic circulation – I.e. CF, GI obstruction
G6PD Deficiency:
A cause of kernicterus in up to 35% of cases
Always suspect if severe hyperbili or poor response to phototherapy
Ethnic origin
11-13% of African Americans
Mediterranean, Middle East, Arabian peninsula, SE Asia, Africa
Requires intervention at lower TSB levels
Testing
Levels may be normal or elevated early Especially in presence of hemolysis
Repeat level at 3 months
Decreased Bilirubin Conjugation:
Elevated unconjugated bilirubin
Genetic Disorders
Crigler-Najjar
2 types
Severe hyperbilirubinemia
Gilbert Syndrome
Mild hyperbilirubinemia
Hypothyroidism
Impaired Bilirubin Excretion:
Elevated unconjugated and conjugated bilirubin (> 2 mg/dL or > 20% of TSB)
Biliary Obstruction
Structural defects – I.e. biliary atresia
Genetic defects – Rotor’s & Dubin-Johnson syndromes
Infection – sepsis, TORCH
Metabolic Disorders – I.e. alpha1 antitrypsin deficiency
Chromosomal Abnormalities – Turner’s syndrome
Drugs – I.e. ASA, sulfa, erythromycin
Diagnosis & Evaluation:
1.Physical Exam
Bilirubin > 5 mg/dL
Milder jaundice - face & upper thorax
Caudal progression generally signifies higher bilirubine levels
Should not rely on this system
Liberally check bilirubin values
2.Laboratory
Blood
Transcutaneous
Generally within 2mg/dL of serum test
Most useful if serum bili < 15
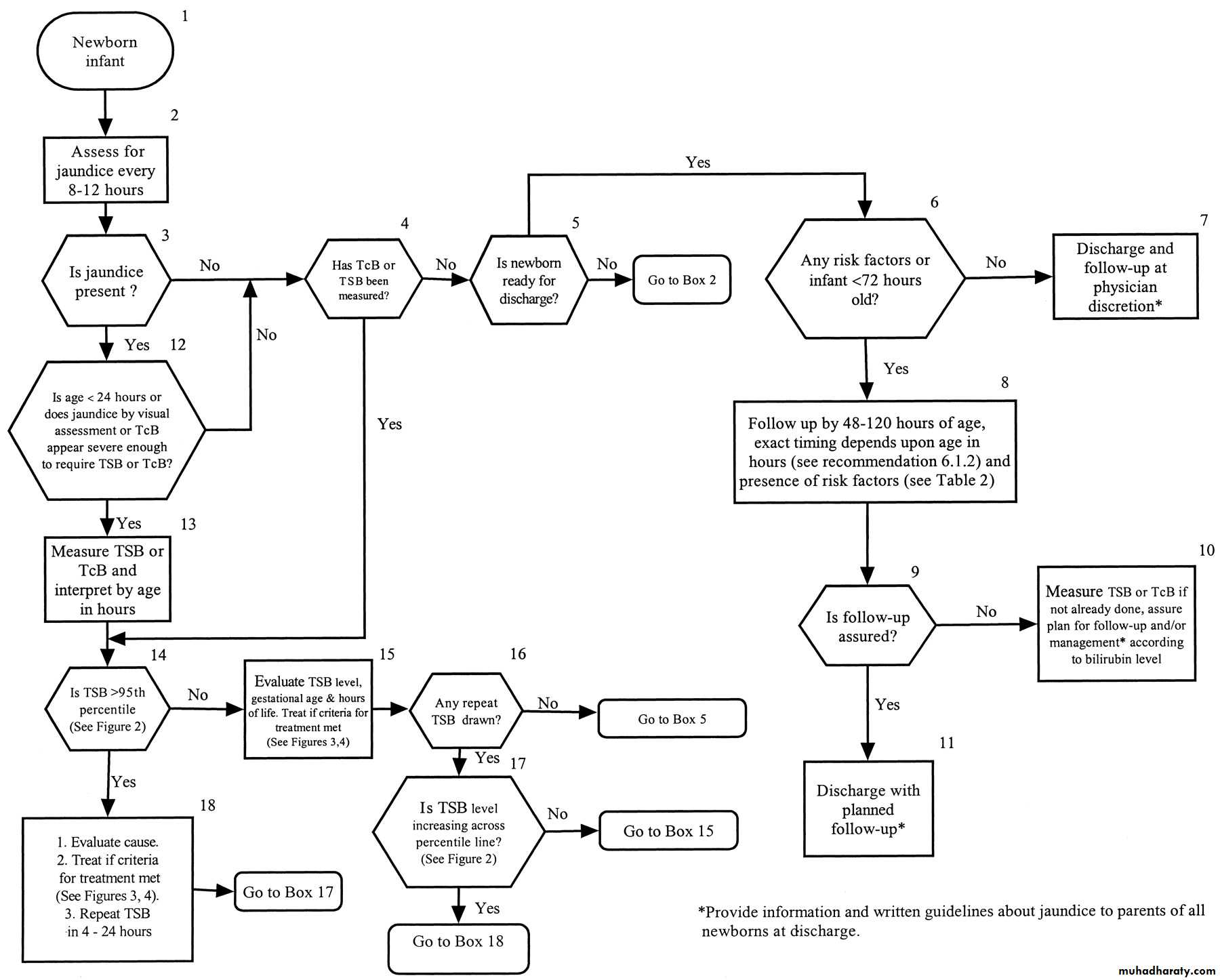
Management of Hyperbilirubinemia in the Newborn Infant 35 or More Weeks of Gestation
Prevention:
Breastfeeding
Should be encouraged for most women
8-12 times/day for 1st several days
Assistance and education
Avoid supplements in non-dehydrated infants (Do not decrease level & severity of hyperbili)
Ongoing assessments for risk of developing severe hyperbilirubinemia
Monitor at least every 8-12 hours
Don’t rely on clinical exam
Blood testing
Prenatal (Mom): ABO & Rh type, antibody
Infant cord blood
Mom not tested, Rh (-): Coomb’s, ABO, Rh
Mom O or Rh (+): optional to test cord blood
Laboratory investigation:
Indicated (if bilirubin concentrations reach phototherapy levels)
Serum total or unconjugated bilirubin concentration
Serum conjugated bilirubin concentration
Blood group with direct antibody test (Coombs’ test)
Hemoglobin and hematocrit determinations
Optional (in specific clinical circumstances)
Complete blood count including manual differential white cell count
Blood smear for red cell morphology
Reticulocyte count
Glucose-6-phosphate dehydrogenase screen
Serum electrolytes and albumin or protein concentrations
Risk Factors for Severe Hyperbilirubinemia:
Major risk factorsPredischarge bili in high-risk zone
Jaundice in 1st 24 hrs
Blood group incomp with + direct antiglobulin test, other known hemolytic disease (eg, G6PD deficiency)
Gestational age 35–36 wk
Previous sibling received phototherapy
Cephalohematoma or significant bruising
Exclusive breastfeeding
East Asian race
Minor risk factors
Bili in high intermed-risk zone
Gestational age 37–38 wk
Jaundice before discharge
Previous sibling with jaundice
Macrosomia infant with diabetic mother
Maternal age ≥ 25
Male
Decreased Risk
Bili in low-risk zone
≥ 41 wks gestation
Exclusive bottle feed
Black race
D/c from hospital > 72hrs
Discharge:
Assess risk
Predischarge bili (Use nomogram to determine risk zone)
TSB Zone
Newborns (%)
% with TSB >95th %
High risk
6
39.5
High intermed
12.5
12.9
Low intermed
19.6
2.26
Low
61.8
0
And/or Assessment of risk factors
Close follow-up necessary
Individualize based on riskWeight, % change from BW, intake, voiding habits, jaundice
Management: * look at the algorithm above
PhototherapyMechanism: converts bilirubin to water soluble form that is easily excreted
Forms
Fluorescent lighting
Fiberoptic blankets
Goal is to decrease TSB by 4-5 mg/dL or < 15 mg/dL total
Breastfed infants are slower to recover
Severe rebound hyperbilirubinemia is rare
Average increase is 1 mg/dL
Intensive
Special blue tube with light in blue-green spectrum
Close to infant
Expose maximum surface area
Exchange Transfusion
Mechanism: removes bilirubin and antibodies from circulation and correct anemiaMost beneficial to infants with hemolysis
Generally never used until after intensive phototherapy attempted
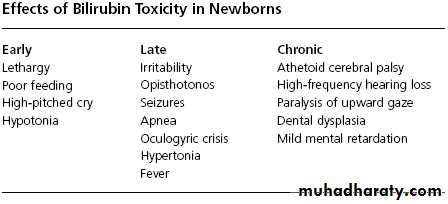
Complications:
Toxicity to Basal Ganglia and brainstem nuclei
2 terms
Acute bilirubin encephalopathy
Kernicterus
Multiple phases
Risk of Kirnicterus
TSB level > 25-30 mg/dlAcidosis
Increased free bilirubin
low albumin, drug displacement
Blood-brain barrier disruption
prematurity, sepsis, ischemia
Kernicterus cases potentially correctable causes:
Early discharge (<48hrs) without f/u within 48 hrs
Failure to check bilirubin level if onset in first 24 hours
Failure to note risk factors
Visual assessment underestimate of severity
Delay in testing jaundiced newborns or treating elevated levels
Lack of concern for presence of jaundice or parental concern
Common Clinical Risk Factors for Severe Hyper-bilirubinemia:
Jaundice in the first 24 hours
Visible jaundice at discharge
Previous jaundiced sibling
Near term gestation 35-38 weeks
Exclusive breastfeeding
East Asian (4), Mediterranean (1), African origin (12) (G6PD deficiency), 19/61 kernicterus cases = G6PD
Bruising, cephalohematoma, birth trauma
Hemolysis risk, O + maternal blood type, sepsis
Medications increasing bilirubin toxicity:
Sulfisoxazole (displacement or G6PD hemolysis)
Ceftriaxone (displacement from albumin)
Trans cutaneous bilirubin:
Older devices affected by skin pigmentation
Newer multi-wavelength spectral reflectance correlate 0.88 with the serum value,
example SpectRx, ± 3 mg/dl
? Confirm values > 40% per age
Carbon monoxide exhaled
Direct Coombs Testing:
@Strongly positive:Rh
Kell
Kidd
Duffy
@Negative or “weakly positive:
Anti-A
Hemolysis consider present:
Hct < 45%
Abnormal blood smear with 3-4+ spherocytes
Reticulocyte count is 4.5% in the first 72 hrs, or
Reticulocyte count is >1-2% in the first 1-2 wks