Dental Implant
Dental Implant• History
• Definition
• Advantages & disadvantages
• Classifications
• Materials used for dental implant.
• Osseointegration
• Biomechanics of osseointegrated implant.
History
1809 Maggiolo - Gold roots which were fixed with adjacent teeth bymeans of spring
1887 Platinum post coated with lead
1895 Gold or iridium tubes were implanted – Bonewell1905 Porcelain corrugated root implant
1913 Hollow basket implant meshwork or iridium , platinum , gold
- Greenfield1948 Insertion of first viable subperiosteal implant – Goldberg
1952 Threaded implant design of pure titaniumEndosteal implants - Branemark
Definition
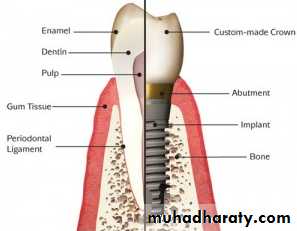
Dental Implant:A prosthetic device or alloplastic material that is surgically inserted into soft or hard tissues, to be used for functional or cosmetic purposes.
Dental implants
Advantages of implant over conventional treatment
• Better maintenance of residual bone.• Better improvement of occlusion, occlusal vertical dimension, phonetics and facial esthetics.
• Improve / regain oral proprioception
• Increase prosthesis success
• Maintains muscle of mastication and facial expression
• Reduce size of prosthesis
• Improve stability and retention of removable prosthesis
• More permanent replacement
• More psychological health
• In cases of partial missing, adjacent teeth do not require splinted restoration, therefore this decreases adjacent tooth loss and maintains bone in site.
Disadvantages of implant treatment
• Expensive.• The patient requires surgery.
• Time consuming.
• Technically complex.
Classifications ofDental implants
I) Depending on the placement within the tissues
• Epithelial / mucosal implants
• Epiosteal / Subperiosteal implants
• Endosteal / endosseous implants
• Transosteal / transosseous implants
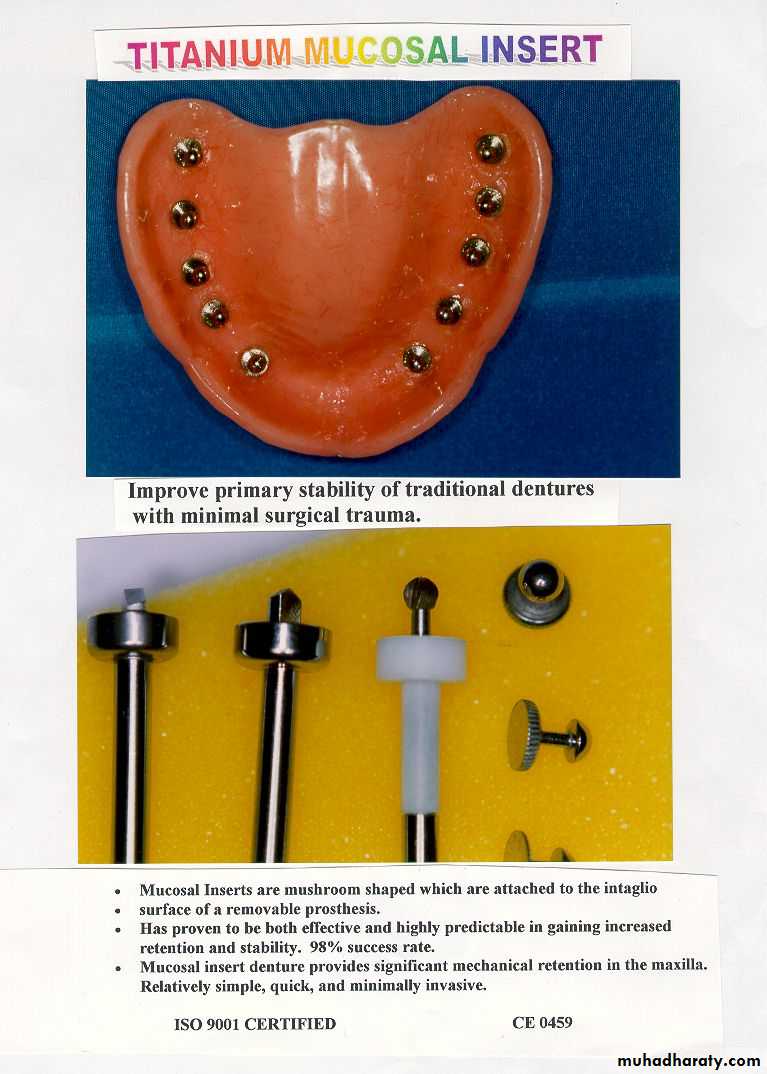
Epithelial / mucosal implants
They are inserted into the oral mucosa.Disadvantages
1. painful healing2. requirement of continual wear
Titanium Mucosal Implants
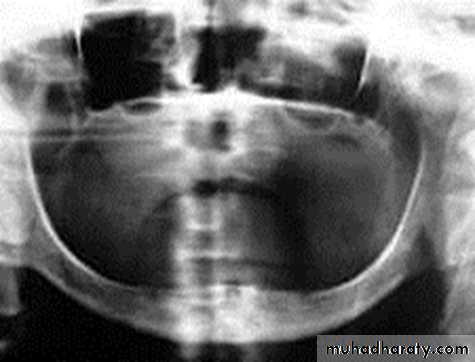
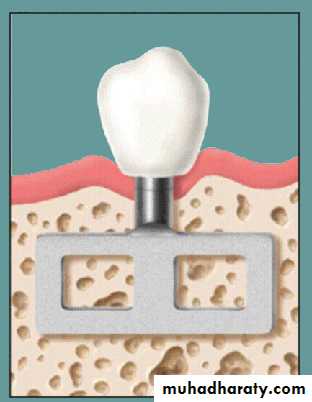
Epiosteal / Subperiosteal Implants
They placed directly beneath the periosteum overliying the bony cortex (not anchored inside the bone)Receive primary bone support by resting on it.
Disadvantages :
1) Slow, predictable rejection of the implant
2) Bone loss associated with failure
• Usually indicated in a severely resorbed, completely edentulous mandible which does not offer enough bone height to accommodate root form implants as anchoring devices.
Endosteal / Endosseous Implants
• Extends into basal bone for support• It transects into 1 cortical plate
Endosteal implants
1-Root form implants3-Plate form implants
• Cylinder
• Screw root form
• Cone shaped
• Combination
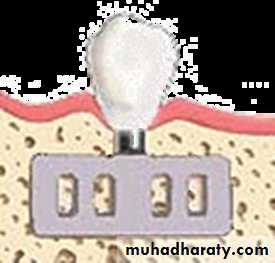
2-Ramus frame implants
Endosteal or Endosseous implantA. Plate-form implant :
• Blade Implants have a long track record, much longer than the Root form Implants. Their name is derived from their flat, blade-like (or plate-like) portion, which is the part that gets embedded into the bone.
•
These implants are designed for the edentulous lower jaw only and are surgically inserted into the jaw bone in three different areas: the left and right back area of the jaw (the approximate area of the wisdom teeth), and the chin area in the front of the mouth.
It’s indicated in a severely resorbed, edentulous mandible which does not offer enough bone height to accommodate Root form Implants.
It provides a tripodial stabilization of the thin lower jaw and protects it from fracturing.
• Ramus-frame implant
Ramus-frame implant
Ramus-frame implant
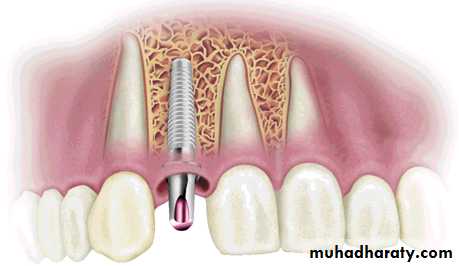
C. Root form implantThe most popular implants in the world today.
come in a variety of shapes, sizes, and materials
can be placed wherever a tooth or several teeth are missing when enough bone is available to accommodate them.
if the bone volume is not sufficient to place Root form Implants, Bone grafting procedures within reasonable limits should be initiated, in order to benefit from these implants.
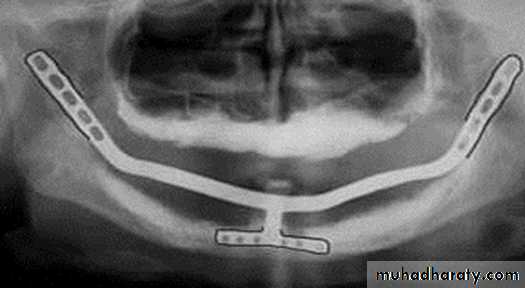
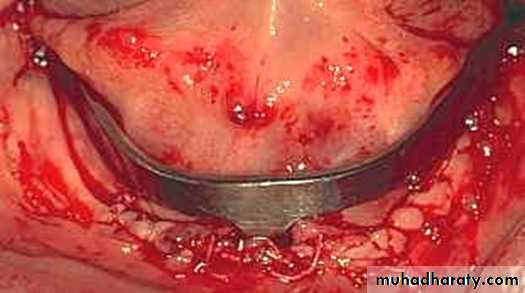
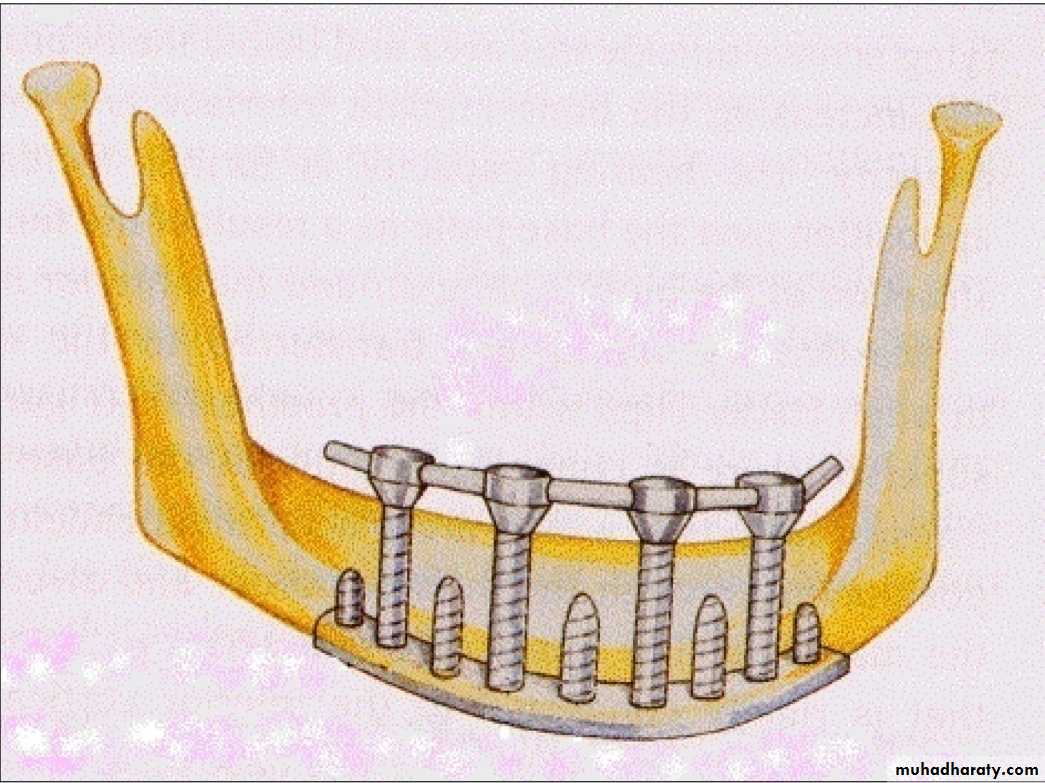
Transosteal / Transosseous Implant
Also called as Staple Bone Implant, Transmandibular ImplantPenetrates both cortical plate and passes through the entire thickness of the alveolar bone
Use restricted to anterior area of mandible
It is not used much any more because they necessitate an extraoral surgical approach.
II) Depending on the materials used
• METALLIC IMPLANTSTitanium
Titanium aluminum vandium
Cobalt chromium molybdenum
Stainless steel
Zirconium
Tantalum
Gold
Platinum
2) NON – METALLIC IMPLANTS
- ceramics- carbon
The bone integration shows no difference to the two different types of titanium.
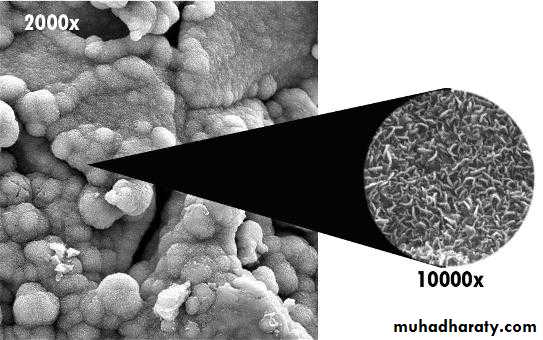
Some implants have an outer coating of Hydroxyapatite (HA). Other implants have their surface altered through plasma spraying, or beading process. This was developed to increase the surface area of the titanium implant and, thus, in theory, give them more stability. These surface treatments were also offered as an alternative to the HA coatings, which on some implants have shown to break loose or even dissolve after a few years.III) Depending on Their Reaction With Bone
Based on the ability of implant to stimulate bone formationBio active
• Hydroxyapatite
• Tri Calcium Phosphate
• Calcium Phosphate
2. Bio inert
metals
Osseointegration
Definition:
A time-dependant healing process where by clinically symptomatic rigid fixation of alloplastic materials is achieved, and maintained, in bone during functional loading.
Factors affecting osseointegration
• Implant biocompatibility
• Implant design
• Implant surface
• Bone quality and surgical site
• Surgical technique
• Loading condition
• Infection control
• Implant biocompatibility
• Cp titanium (commercially pure titanium)• Titanium alloy (titanium-6aluminum-4vanadium)
• Zirconium
• Hydroxyapatite (HA), one type of calcium phosphate ceramic material
• Implant design (root-form)
Cylindrical Implant- most conducive
Threaded Implant
- maintenance of a clear steady state bone response.
- To enhance initial stability and increase surface contact, most implant forms have been developed as a serrated thread.
• Implant surface
Increased pitch (the number of threads per unit length) and increased depth between individual threads allows for improved contact area between bone and implant.Mild rough surface improved contact area between bone and implant surface.
Reactive implant surface by anodizing (Oxide layer) ,acid etching or HA coating enhanced osseointegration• Bone quality and surgical site
Good bone quality and healthy surgical siteQuality I
Was composed of homogenous compact bone, usually found in the anterior lower jaw.
Quality II
Had a thick layer of cortical bone surrounding dense trabecular bone, usually found in the posterior lower jaw.
Quality III
Had a thin layer of cortical bone surrounding dense trabecular bone, normally found in the anterior upper jaw but can also be seen in the posterior lower jaw and the posterior upper jaw.
Quality IV
Had a very thin layer of cortical bone surrounding a core of low-density trabecular bone, It is very soft bone and normally found in the posterior upper jaw. It can also be seen in the anterior upper jaw.
5. Surgical technique
Minimum possible trauma and Minimal tissue violence at surgery is essential for proper osseointegration.
Careful cooling while surgical drilling is performed at low rotatory rates
Use of sharp drills
Use of graded series of drills
Proper drill geometry is important, as intermittent drilling.
The insertion torque should be of a moderate level because strong insertion torques may result in stress concentrations around the implant, with subsequent bone resorption.
• Loading condition
• A two-stage surgical protocol (is advocated)• One-stage surgical protocol
• Immediate occlusal loading (placed within 48 hours postsurgery) - will cause failure
• Immediate non-occlusal Loading (in single-tooth or short-span applications)
• Early loading (prosthetic function within two months)
Biomechanics of osseointegrated implant.
In all incidences of clinical loading, occlusal forces are first introduced to the prosthesis and then reach the bone implant interface via the implant. This is affected by:Force directions and magnitudes,
Prosthesis type,
Prosthesis material,
Implant design,
Number and distribution of supporting implants,
Bone density, and
The mechanical properties of the bone-implant interface.
Dental Implant Treatment Planning and Types of Dental Implants
Depend on :
How many teeth are missing?
What is the degree of bone loss?
Are the remaining teeth in a good position and do they have a long-term prognosis?
What does the patient expect for an end result?
What treatment will result in the best cosmetic outcome?
What is the patient's budget?
Overall...
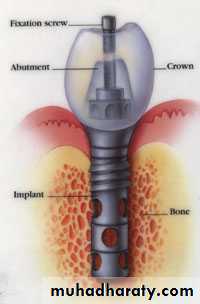
What is the most practical and feasible implant treatment that will produce optimal chewing function and optimal cosmetic results in a timely and affordable manner?PARTS OF DENTAL IMPLANTS(Root Form Implants)
Dr,salah hegazycrest module ( cervical geometry )
bodyapex
Implant Body Regions
3 parts
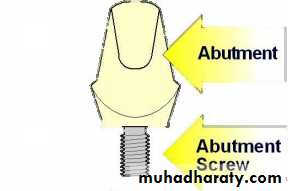
Prosthetic Attachments:
1. Implant abutment2. Implant superstructure
Implant abutment:
A portion of the implant that supports or retains a prosthesis or implant superstructure.Categories of implant abutment
based on method by which prosthesis or superstructure is retained to the abutmentScrew retention
cement retentionfor attachment
• attachment device to retain a removable prosthesisSuper structure:
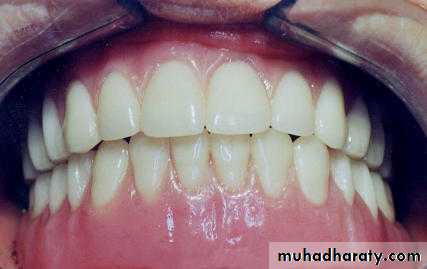
Recently, it is defined as the superior part of multiple layer prosthesis that includes the replaced teeth and associated structuresThe superstructure for completely edentulous patients can be classified as follows:
• Implant retained removable overdenture
• Implant supported removable overdenture
• Fixed detachable prosthesis (Hybrid prosthesis)
• Implant supported Fixed Bridge
1) Screwed-in Fixed Bridge
• 2) Cemented Fixed Bridge
Design Concepts for Removable Implant Prostheses
Removable options can now be either nonrigid (resilient) or rigid. A removable rigid overdenture will function in a similar manner as a fixed implant prosthesis.Rigid
ResilientResilient Design
Removable implant prostheses can be restored using a combined implant-retained and soft tissue-supported overdenture (ie, the two- implant overdenture).Fabrication of this type of restoration can be completed using individual unsplinted retainers that allow rotation or a bar-clip prosthesis equipped with a hinging mechanism for rotation. The use of a bar (ie, Dolder bar-joint) allows movement between the two components.
In either case, the classic principles of complete denture fabrication apply adequate denture base extension and proper adaptation are essential. These design concepts should not be extrapolated to the maxillary arch.
Rigid Design
The implant-retained and implant-supported removable overdenture (ie, multiple implant bar overdenture with three or more implants) may or may not require the same number of implants as the fixed and usually has multiple retentive elements.
This type of prosthesis does not, however, contain a rotational device. The bar used in these types of restorations is a bar unit (ex, Dolder bar-unit). It allows no movement between the bar and sleeve.
Treatment Plan Selection
Treatment planning and the decision-making process is a balance between the patient’s preferences, finances and clinical factors.Clinical factors
Quality, quantity, and shape of supporting alveolar bone.The cantilever design can be avoided if the implants are placed posterior to the foramen. A fixed option could be utilized but will display less teeth, while a removable option will provide increased tooth display. .
A patient who has the bone quality to support a fixed prosthesis could also be a candidate for an implant overdenture supported by fewer implants.
Extraoral Diagnostic Guidelines
• Removable• Fixed
• High
• Low
• Lip line
• Distinct
• Little
• Tooth display
• Necessary
• No need
• Facial/Lip support
Intraoral Diagnostic Guidelines
• Removable
• Fixed
• Buccal inclination
• Buccal convex
• Vertical convex
• Ridge (shape)
• > 15 mm
• ~10 mm
• Intermaxillary distance
• Skeletal
• Neutral
• Intermaxillary relationship
• Thin, mobile
• Thick, keratinized
• Mucosa
Implant-overdenture
The most common line of treatmentTreatment Planning Determinants
1. Changes in Oral Structures in Edentulism2. Posterior Ridge Anatomy
3. Occlusal Forces
4. Quality, Location and Quantity of Bone
5. Implant Size
6. Implant Location
7. Arch configuration
8. "Mapping" the Mandible
9. Cantilevering
Treatment Planning
When all the diagnostic information has been assembled, a variety of available treatment options must be assessed:
1. One-Implant Overdenture
2. Two-Implant Overdenture
3. Three-Implant Overdenture
4. Four-Implant Overdenture
5. Five-Implant Overdenture
One-Implant Overdentures
Indications:The maladaptive or dissatisfied denture patient who demands greater stability and oral comfort,
Elderly patients desiring a more stable mandibular denture,
Or, as a minimal implant treatment objective for the partially edentulous patient with severely compromised teeth in which removal would convert a patient to a fully edentulous stateIn the two-implant over-denture, an attachment is used to greatly enhance the retentive potential of what is essentially a tissue-supported prosthesis.
If only two implants are placed, which are 13mm long or longer, and they are in dense bone, they can be left as individual supporting units with little risk.
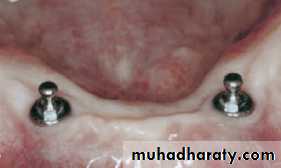
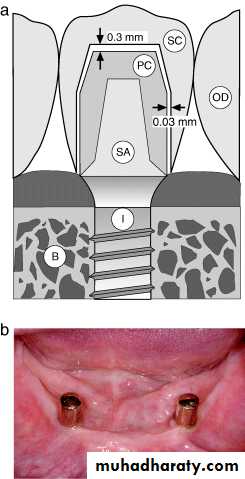
. Two-Implant Solitary Overdenture
Two-Implant Solitary Overdenture
2. Two-Implant Bar Overdenture
If the two implants are 10 mm long or shorter, or the bone quality is compromised, then ideally:
They should be splinted.
They should be at least 10 mm apart (in order to allow room for a clip or fastening mechanism)
They should be no further than 18 mm apart in order to limit bar flexure.
Two-Implant Bar Overdenture
Two-Implant Bar Overdenture
3. Three-Implant OverdentureThe three-implant overdenture is still essentially a tissue-supported prosthesis with enhanced retention supplied by the attachment/bar complex.
Three-Implant Over-denture
4. Four-Implant OverdentureAt this level, the prosthesis begins to derive a larger part of its support and retention from the implant/bar complex, and the importance of tissue support decreases.
Also, the attachments selected for a four-implant bar over-denture can be more rigid, as the torquing forces generated by the prosthesis will be better tolerated.
This number allows for some "insurance" in case one implant fails to integrate.
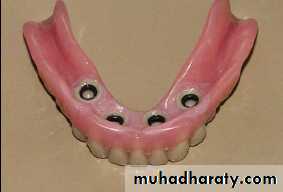
Unsplinted Implant Overdenture
Implant-Bar Overdenture
5. Five-Implant OverdentureAt this level, a prosthesis can be fabricated that is completely implant supported and retained.
The decision to fabricate a bar over-denture over five implants, rather than a fixed detachable restoration, usually relates to the patients’ ability to maintain proper oral hygiene.
Five-Implant Overdenture
Five-Implant Overdenture
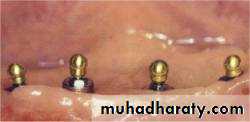
PROSTHETIC PROTOCOLOverdenture abutments were cemented or scrowed into the implants.
Pressure indicating paste was placed on each overdenture ball.
The denture was seated so that the pressure indicating paste could mark the exact location of the overdenture abutments. Then, a recess was cut into the denture at each abutment location
The resulting depressions in the mucosal aspect of the denture were lined with polyvinylsiloxane material and seated in the patient's mouth.
The denture was either lined with a lab-processed material or O-rings were used for retention.
Overdenture abutments were cemented or scrowed into the implants.
Pressure indicating paste was placed on each overdenture ball.
Then, a recess was cut into the denture at each abutment location
lined with polyvinylsiloxane material and seated in the patient's mouth.
The denture was either lined with a lab-processed material or O-rings were used for retention