1
THE CORNEA
Introduction
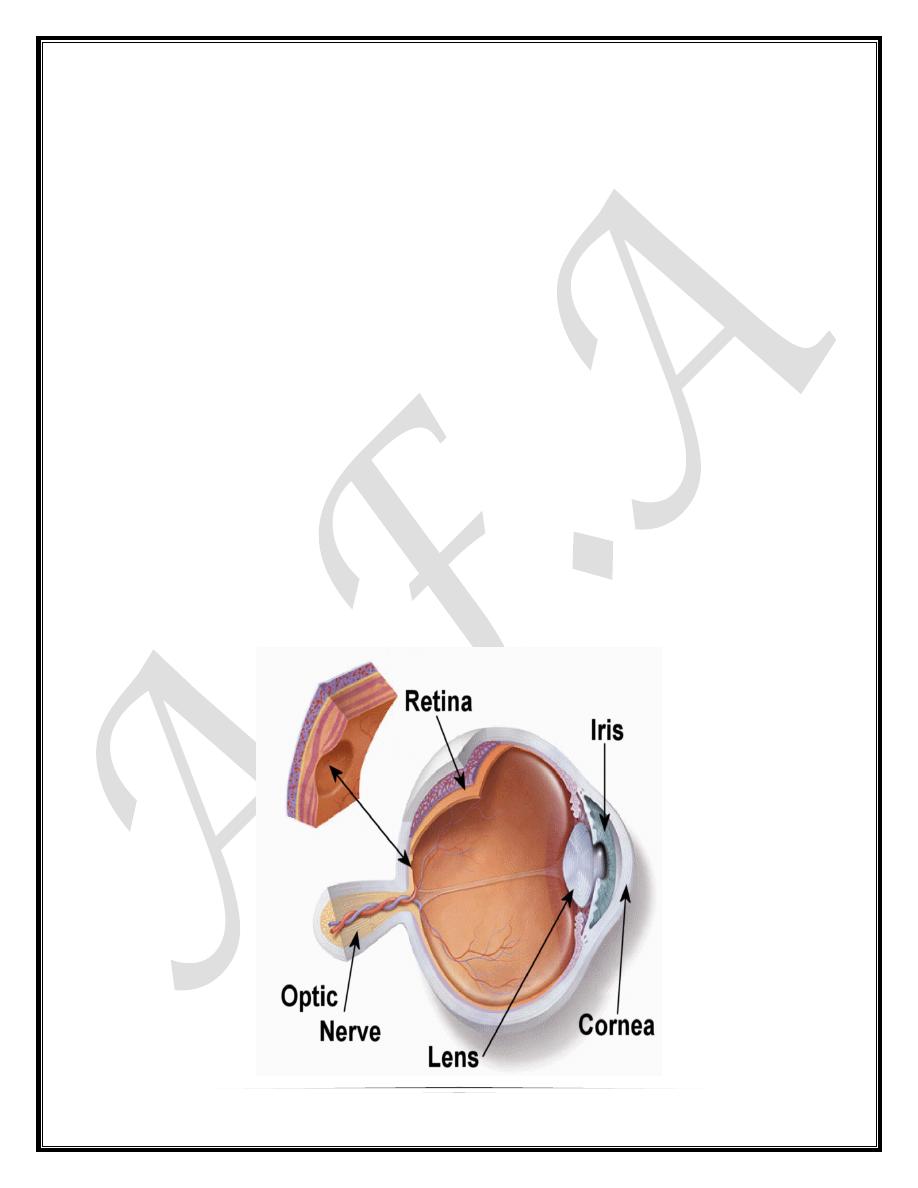
The cornea is the transparent front part of the eye that covers the iris, pupil,
and anterior chamber, providing most of an eye's optical power. Together with
the lens, the cornea refracts light and, as a result, helps the eye to focus. The
cornea contributes more to the total refraction than the lens does, but, whereas
the curvature of the lens can be adjusted to "tune" the focus, the curvature of
the cornea is fixed.
1. The epithelium is stratified, squamous and non-keratinized,
2. Bowman layer is the acellular superficial layer of the stroma
3. The stroma makes up 90% of corneal thickness. It is principally composed of
regularly orientated layers of collagen fibrils whose spacing is maintained by
proteoglycan ground substance) with interspersed modified fibroblasts
(keratocytes).
4. Descemet membrane is composed of a fine latticework of collagen fibrils.
5. The endothelium consists of a single layer of hexagonal cells that cannot
regenerate. It plays a vital role in maintaining corneal deturgescence. The adult
cell density is about 2500 cells/mm
2
. The number of cells decreases at about
0.6% per year and neighbouring cells enlarge to fill the space as cells die. At a
cell density of about 500 cells/mm
2
corneal oedema develops and corneal
transparency is reduced.
2
BACTERIAL KERATITIS
Bacterial keratitis is very uncommon in a normal eye and usually only develops
when the ocular defences have been compromised. Bacteria that can penetrate
an apparently normal corneal epithelium are N. gonorrhoeae, N. meningitides, C.
diphtheriae and H. influenzae. The virulence of the organism and the anatomic
site of the infection determine the pattern of disease. The most common
pathogens are:
1. P. aeruginosa
2. S. aureus.
3. S. pyogenes.
4. S. pneumoniae
Risk factors
Contact lens wear, particularly of soft lenses worn overnight, is the most
important risk factor for bacterial keratitis. Pseudomonas spp. account for over
60% of cases
Trauma such as accidental injury, surgical (refractive surgery) and loose sutures
Ocular surface disease such as herpetic keratitis, bullous keratopathy, dry eye
Other factors include topical or systemic immunosuppression, diabetes, Vitamin
A deficiency and measles.
Diagnosis
History with particular attention paid to risk factors mentioned above.
Presenting symptoms include pain, photophobia, blurred vision and discharge
Signs: An epithelial defect associated with an infiltrate around the margin
and base associated with circumcorneal injection . Severe infiltration
associated with enlarging hypopyon. Progressive ulceration may lead to
corneal perforation and endophthalmitis.
Differential diagnosis : includes fungal keratitis, acanthamoeba keratitis,
necrotic stromal herpes simplex keratitis and sterile inflammatory corneal
infiltrates associated with contact lens wear.
3
Treatment
Bacterial keratitis has the potential to progress rapidly to corneal perforation.
Even small axial lesions can cause surface irregularity and scar that can lead to
significant loss of vision.
Topical therapy can achieve high tissue concentration and initially should involve
broad spectrum antibiotics to cover the most common pathogens.
1. Dual therapy involves a combination of two fortified antibiotics (an
aminoglycoside and a cephalosporin) to cover common Gram-positive and
Gram-negative pathogens.
2. Monotherapy with a fluoroquinolone (i.e. ciprofloxacin 0.3% or ofloxacin
0.3%) is commercially available
Oral antibiotics (ciprofloxacin 750mg twice daily for 7-10 days) is not usually
necessary.
Subconjunctival antibiotics are only indicated if there is poor compliance with
topical treatment.
VIRAL KERATITIS
Herpes simplex keratitis
Herpetic eye disease is the major cause of unilateral corneal scarring worldwide,
and is the most common infectious cause of corneal blindness in developed
countries. As many as 60% of corneal ulcers in developing countries may be the
result of herpes simplex virus (HSV) and 10 million people worldwide may have
herpetic eye disease.
Herpes simplex virus
HSV is enveloped with a cuboidal capsule and a linear double-stranded DNA
genome.
HSV-1 primarily causes infection above the waist that may affect the face, lips
and eyes.
HSV-2 causes venereally acquired infection (genital herpes).
HSV transmission is facilitated in conditions of crowding and poor hygiene.
4
Primary infection
Primary infection (no previous viral exposure) usually occurs by droplet
transmission, or less frequently by direct inoculation. Due to protection bestowed
by maternal antibodies, it is uncommon during the first 6 months of life. Most
cases are probably subclinical or only cause mild fever, malaise and upper
respiratory tract symptoms. Children may develop blepharoconjunctivitis which is
usually benign and self-limited although corneal microdendrites develop in a
minority of cases.
Recurrent infection
After primary infection the virus is carried to the sensory ganglion for that
dermatome (e.g. trigeminal ganglion) where a latent infection is established.
Subclinical reactivation can periodically occur when HSV is shed and patients
are contagious. Stimuli such as fever, hormonal change, ultraviolet radiation,
trauma, and trigeminal injury may cause a clinical reactivation, when the virus
replicates and is transported in the sensory axons to the periphery where there is
recurrent disease.
Clinical features of epithelial keratitis
Presentation may be at any age with mild discomfort, watering and blurred
vision.
Sign
A linear-branching (dendritic) ulcer, most frequently located centrally.
The ends of the ulcer have characteristic terminal buds and the bed of the
ulcer stains well with fluorescein
Corneal sensation is reduced.
Inadvertent topical steroid treatment may allow progressive enlargement
of the ulcer to a geographical or 'amoeboid' configuration
Treatment of epithelial keratitis
Topical antiviral agents (trifluorothymidine, aciclovir, vidarabine and ganciclovir)
are equally effective. The most frequently used drug in Europe is aciclovir 3%
ointment administered five times daily. It is relatively non-toxic, even when given
for up to 60 days, because it acts preferentially on virus-laden epithelial cells. On
this treatment 99% will be resolved by 2 weeks.
5
Debridement may be used for dendritic but not geographic ulcers.
Herpes zoster ophthalmicus
Is a herpes Zoster attack that affect the ophthalmic division of trigeminal nerve
Pathogenesis:
The varicella-zoster virus (VZV) causes chickenpox (varicella) and shingles
(herpes zoster). VZV and HSV belong to the same subfamily of the herpes virus
group and are morphologically identical but antigenically different. After the initial
attack of chickenpox the virus travels in a retrograde manner to the dorsal root
and cranial nerve sensory ganglia where it may remain dormant for decades.
From there it can reactivate to cause shingles after VZV-specific cellular
immunity has faded.
Risk of ocular involvement
Hutchinson sign describes involvement of the external nasal nerve, which
supplies the side of the tip, and the side and root of the nose
Age. HZO occurs most frequently in the sixth and seventh decades
AIDS patients tend to have more severe disease. The development of shingles in
children or young adults (< 50 years) should prompt a search for
immunodeficiency or malignancy.
Clinical Features:
1. Acute epithelial keratitis develops in about 50% of patients within 2 days
of the onset of the rash and resolves spontaneously within a few days.
o
It is characterized by small, fine, dendritic lesions which, in contrast
to herpes simplex dendrites, have tapered ends without terminal
bulbs.
o
The lesions stain with fluorescein and rose bengal.
o
Treatment is with a topical antiviral, if appropriate.
2.Conjunctivitis, Episcleritis, Scleritis, Nummular keratitis, Stromal
keratitis, Disciform keratitis, Anterior uveitis
6
FUNGAL KERATITIS
Fungi are micro-organisms that have rigid walls and multiple chromosomes
containing both DNA and RNA. The main types are:
1. Filamentous fungi (Aspergillus spp., Fusarium solani, and pscedosporium
spp.)
2. Yeasts (Candida spp.)
The primary risk factors for infection are trauma (65% of cases in tropical areas)
particularly with vegetable matter, chronic ocular surface disease and epithelial
defects, diabetes, systemic immunosuppression and hydrophilic contact lenses.
Treatment: Antifungal agents ,topicall, subconjunctival and even systemic
NEUROTROPHIC KERATITIS
Neurotrophic keratopathy occurs when there is loss of the trigeminal innervation
to the cornea resulting in partial or complete anaesthesia.
Causes:
1. Acquired. Damage to the fifth cranial nerve or trigeminal ganglion e.g
following surgical ablation for trigeminal neuralgia , or tumour (acoustic
neuroma or neurofibroma).
2. Systemic diseases such as diabetes and leprosy.
3. Ocular disease such as herpes simplex and herpes zoster keratitis,
4. Congenital causes include familial dysautonomia (Riley-Day syndrome).
Treatment
1. Topical lubricants (non-preserved) for associated dry eye or corneal exposure
2. Protection of the ocular surface
a. Simple taping of the lids to provide temporary protection.
b. Botulinum toxin injection to induce protective ptosis.
c. Tarsorrhaphy to prevent drying and reduce exposure,
d. Therapeutic silicone contact lenses
7
EXPOSURE KERATITIS
Exposure keratopathy is the result of incomplete lid closure (lagophthalmos)
during blinking.
Causes
1. Neuroparalytic, especially facial nerve palsy which may be idiopathic or the
result of surgery for acoustic neuroma or parotid tumour.
2. Reduced muscle tone as in coma or parkinsonism
3. Mechanical :Eyelid scarring associated with cicatricial pemphigoid, burns (Fig.
9.29b) and trauma.
4. Abnormality of globe position: Severe proptosis resulting in lagophthalmos
due to thyroid ophthalmopathy or orbital tumour..
: Treatment depends on the severity of exposure and whether recovery is
anticipated.
Artificial tears (non-preserved) during the day and ointment at night.
Taping the lid closed at night.
Bandage contact lenses,
Temporary or permanent tarsorrhaphy
CORNEAL ECTASIAS
Keratoconus
Keratoconus is a progressive disorder in which the cornea assumes a conical
shape secondary to stromal thinning and protrusion . The onset is around
puberty with slow progression thereafter until the third or fourth decades of life,
when it usually arrests, although the ectasia can become stationary at any time.
Both eyes are affected, in almost all cases.
Presentation is typically during puberty with unilateral impairment of vision due to
progressive myopia and astigmatism, which subsequently becomes irregular.
8
Treatment
1. Spectacles in early cases.
2. Rigid contact lenses are required for higher degrees of astigmatism.
3. Keratoplasty, penetrating or deep lamellar, is indicated in patients with
advanced progressive disease,
CORNEAL DEGENERATIONS
Age-related degenerations
Arcus senilis
Arcus senilis is the most common peripheral corneal opacity, which frequently
occurs without predisposing systemic conditions in elderly individuals.
Occasionally arcus may be associated with familial and non-familial
dyslipoproteinaemias. Hyperlipoproteinaemia, most notably type II, is frequently
associated with bilateral arcus.
Band keratopathy
Band keratopathy is a common condition characterized by the deposition of
calcium salts in Bowman layer, epithelial basement membrane and anterior
stroma .
Causes may include chronic uveitis, advancing age ,and chronic renal failure.
