Infections of the Pharynx, Tonsils, and Adenoid
د. محمد رديف
Pharyngitis: It is inflammation of the mucosal lining of the pharynx.
Acute Non-specific Pharyngitis:
• Is viral infection in association with common cold and influenza, which may be followed by
secondary bacterial infection.
Clinical picture:
Symptoms: Sore throat worse by swallowing and pain may radiate to the ears, preceded by
symptoms of upper respiratory tract infection, fever, headache, malaise.
Signs: diffuse congestion of the pharyngeal mucosa with enlarged cervical lymph nodes.
Treatment:
• Warm fluids, analgesics, antipyretics, and antiseptic gurgle, antibiotics for secondary bacterial
infection.
Acute specific Pharyngitis:
1- Diphtheria.
2- Infectious mononucleosis (glandular fever).
3- Moniliasis.
4- Acute pharyngitis associated with blood disorders
Chronic non-specific Pharyngitis
Aetiology:
• Recurrent acute pharyngitis, chronic sinusitis, gastrooesophageal reflux, smoking and alcohol.
Clinical picture:
Symptoms:
• Long standing sore throat with sensation of discomfort and irritation in the throat, leading to
frequent hawking.
Signs:
• Hypertrophied lateral pharyngeal bands and submucosal lymphoid follicles on posterior
pharyngeal wall.
Treatment: Treatment of predisposing factors.
Chronic specific Pharyngitis
1- Tuberculosis.
2- Syphilis.
3- Scleroma
4- Toxoplasmosis.
5- Leprosy.

Acute Tonsillitis
• Acute inflammation of the palatine tonsils.
Aetiology:
• Causative organism: Group A β-haemolytic Streptococcus.
Symptoms:
1- Sore throat, painful swallowing, and foetor oris (halitosis).
2- Referred otalgia.
3- High fever, malaise and arthralgia.
Signs:
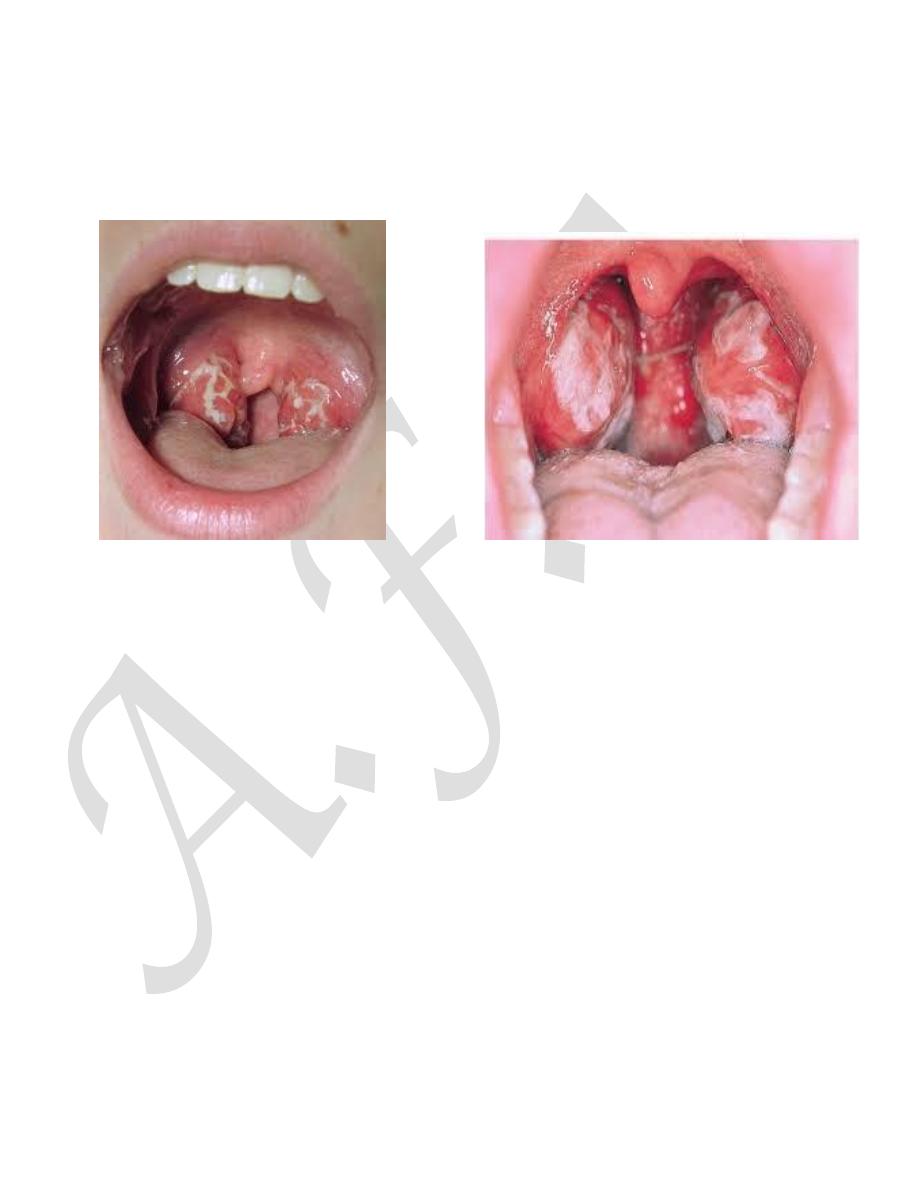
1- High temperature with tachycardia.
2- Throat examination: shows congested hypertrophied tonsils with yellowish spots on its
surface; which may coalesce to form yellowish membrane.
3- Enlarged jugulo-diagestric cervical lymph nodes.
Treatment:
1- Warm fluids, soft diet, analgesics, antipyretics and mouth wash.
2-Systemic antibiotics: penicillin for 7-10 days, if allergic to penicillin prescribes erythromycin.
Differential diagnosis:
1- Diphtheria.
2- Glandular fever (Infectious mononucleosis).
3- Scarlet fever.
Complications:
1- Peritonsillar abscess.
2- Parapharyngeal and retropharyngeal abscesses.
3- Acute glomerulo-nephritis.
4- Acute rheumatic fever.
5- Acute otitis media.
Tonsillectomy
Indications:
1- Repeated attacks of acute tonsillitis (more than 5 attacks per year).
2- Obstructive sleep apnea.
3- Peritonsillar abscess (Quinsy).
4- Suspected tumour of the tonsil.
5- Recurrent attacks of rheumatic fever,
6- Attacks of acute glomerulonephritis,
7-As a part of other operations: Excision of long styloid process or glossopharyngeal
neurectomy.

Contraindications:
1- Bleeding tendency as haemophilia.
2- Acute upper respiratory tract infections.
3- Epidemics of poliomyelitis.
4- Cleft palate.
Complications:
1- General anaesthesia: e.g. hypersensitivity to anaesthetic drugs or succinyl choline apnea.
2- Respiratory obstruction: This is the most serious complication; it may be due to early
extubation, laryngeal spasm, inhalation of blood clots, vomitius or falling back of the tongue
during recovery from anesthesia.
3- Haemorrhage(bleeding):
a) Primary: It is intra-operative blood loss. It is usually due to bad selection of the patient, bad
dissection or injury of blood vessels.
b) Reactionary: Occurs within the first 24 hours after return from the theatre, it is usually due to
oozing from the vessels after relaxation of the stretched blood vessels, slipping of a ligature, or
rise of blood pressure during recovery from anesthesia.
c) Secondary: usually occurs between the 3rd and the 10th post operative days due to infection
in the tonsillar fossa.
4- Pneumonia or lung abscess.
5- Trauma to the teeth, uvula, or the posterior pharyngeal wall.
6- Haematoma and edema of the uvula.
7- Infection of the tonsillar fossa, and acute otitis media.
8- Postoperative scarring of the palate.
9- Tonsillar remnant.
10- Subacute bacterial endocarditis.
Adenoid: (nasopharyngeal tonsil)
Mass of lymphoid tissue located in the upper and posterior wall of the nasopharynx, it is a
normal structure with definite function namely the production of antibodies.
Physiological enlargement occurs at the age of 3 to 7 years. Pathological enlargement is due to
inflammation during recurrent attacks of upper respiratory tract infection, which make it
sufficient to produce symptoms, but the size of the adenoid in relative to size of the
nasopharyngeal space is the more important factor in producing the symptoms.
Clinical picture: Enlargement of the adenoids will be sufficient to produce the following:
1- Nasal obstruction: this leads to mouth breathing, snoring and sleep disturbance, hyponasality
speech, and obstructive sleep apnea syndrome.
2- Nasal discharge ( mucoid or mucopurulent).
3- Post-nasal drip (mucoid or mucopurulent) which may leads to recurrent nocturnal cough.
4- Eustachian tube obstruction: predisposes to otitis media with effusion, recurrent attacks of
acute otitis media.

5- Adenoid face: May develop with pinched nostrils, prominent incisors, open mouth, and high
arched palate.
6-Mental dullness and apathy: due to day time sleepiness, hearing loss, chronic hypoxia.
Diagnosis:
1- Posterior rhinoscopy by post-nasal mirror examination: can show the adenoids but difficult
especially in young children.
2- Endoscopic examination by fibro-optic nasopharyngeoscopy is the best method.
3- Lateral X-ray soft tissue for nasopharynx is good.
Treatment:
Adenoidectomy.
Adenoidectomy
Indications:
Enlargement of the adenoids sufficient to produce persist symptoms or recurs regularly.
Nasal obstruction which lead to mouth breathing, obstructive sleep apnea, snoring and sleep
disturbance, adenoidal face, otitis media with effusion, recurrent acute otitis media.
Contraindications: similar to tonsillectomy.
Complications: Similar to tonsillectomy.
Other complications: include trauma to Eustachian cushions.