Phase II Periodontal Therapy
PERIODONTAL SURGERYPhase II therapy is used to surgically treat residual periodontal pockets and bone defects remaining after Phase I therapy. All patients treated surgically need to have a preoperative history of adequate plaque control with 20% or more of the tooth surfaces
free of plaque after oral hygiene procedures.
OBJECTIVES OF THE SURGICAL PHASE
The surgical phase of periodontal therapy has thefollowing main objectives:
1. Improvement of the prognosis of teeth and their
replacements.2. Improvement of esthetics.
The surgical phase consists of techniques performed for pocket therapy and for the correction of related morphologic problems, namely, muco-gingival defects.
In many cases, procedures are combined so that one surgical intervention fulfills both objectives.
The purpose of surgical pocket therapy is to eliminate the pathologic changes in the pocket walls; to create a stable, easily maintainable state; and if possible, to promote periodontal regeneration.
To fulfill these objectives, surgical techniques:
(1) Increase accessibility to the root surface, making it possible to remove all irritants;
(2) reduce or eliminate pocket depth, making it possible for the patient to maintain the root surfaces free of plaque; and
(3) reshape soft and hard tissues to attain a harmonious topography.
Surgical Pocket Therapy
Surgical pocket therapy can be directed toward(1) access surgery to ensure the removal of irritants from the tooth surface or
(2) elimination or reduction of the depth of the periodontal pocket.The effectiveness of periodontal therapy is dependent on success in completely eliminating calculus, plaque, and diseased cementum from the tooth surface.
The presence of irregularities on the root surface also increase the difficulty of the procedure.
These problems can be reduced by resecting or displacing the soft tissue wall of the pocket, thereby increasing the visibility and accessibility of the root surface. The flap approach and the gingivectomy technique attain this result
Results of Pocket Therapy
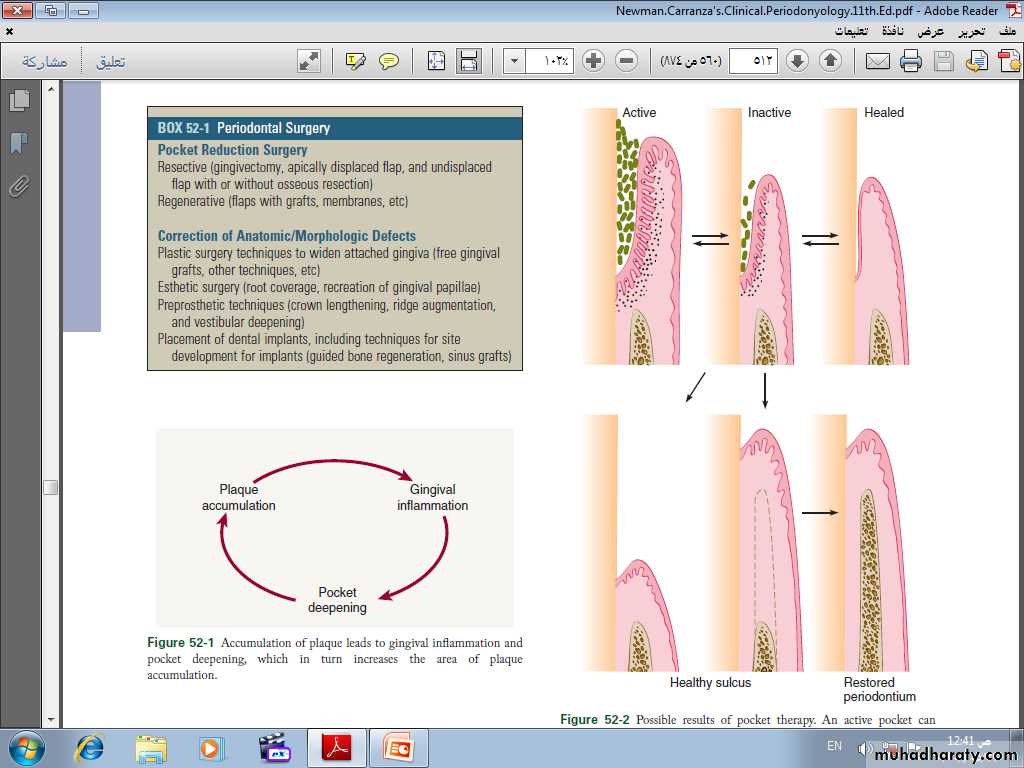
An active pocket can become inactive and heal by means of a long junctional epithelium. Surgicalpocket therapy can result in a healthy sulcus, with or without gain of attachment.
Improved gingival attachment promotes restoration of bone height, with re-formation of periodontal ligament fibers and layers of cementum.
Possible results of pocket therapy
Pocket depth is an extremely useful and widely employed clinical determination, but it must be evaluated together with level of attachment and the presence of bleeding, exudation, and pain. The most important variable for evaluating whether a pocket (or deep sulcus) is progressive is the level of attachment, which is measured in millimeters from the cementoenamel junction. The apical displacement of the level of attachment places the tooth in jeopardy, not the increase in pocket depth, which may be caused by coronal displacement of the gingival margin.POCKET ELIMINATION
VERSUS POCKET MAINTENANCE
Regardless of the surgical technique used for pocket therapy, a certain pocket depth recurs. Therefore maintenance of this depth without any further loss of attachment becomes the goal.
REEVALUATION AFTER PHASE I THERAPY
All patients should be treated initially with scaling and root planing and that a final decision on the need for periodontal surgery should be made only after a thorough evaluation of the effects of Phase I therapy.The assessment is generally made no less than 1 to 3 months and sometimes as much as 9 months after the completion of Phase I therapy. This reevaluation of the periodontal condition should include re-probing the entire mouth.
The presence of calculus, root caries, defective
restorations, and signs of persistent inflammation should also be evaluated.CRITICAL ZONES IN POCKET SURGERY
Criteria for the selection of one of the different surgical techniques for pocket therapy are based on clinical findings in the soft tissue pocket wall, tooth surface, underlying bone, and attached gingiva.Zone 1: Soft Tissue Pocket Wall
The clinician should determine the morphologic features, thickness, and topography of the soft tissue pocket wall and persistence of inflammatory changes in the wall.Zone 2: Tooth Surface
The clinician should identify the presence of deposits and alterations on the cementum surface and determine the accessibility of the root surface to instrumentation. Phase I therapy should havesolved many, if not all, of the problems on the tooth surface. Evaluation of the results of Phase I therapy should determine the need for further therapy and the method to be used.
Zone 3: Underlying Bone
The clinician should establish the shape and height of the alveolar bone next to the pocket wall through careful probing and clinical and radiographic examinations. Bony craters, horizontal or angular bone losses, and other bone deformities are important criteria in selection of the treatment technique.Zone 4: Attached Gingiva
The clinician should consider the presence or absence of an adequate band of attached gingiva when selecting the pocket treatment method.
An inadequate attached gingiva may be caused by a high frenum attachment, marked gingival recession, or a deep pocket that reaches the level of the muco-gingival junction.
All these possible conditions should be explored and their influence on pocket therapy determined.
INDICATIONS FOR PERIODONTAL SURGERY
1. Areas with irregular bony contours, deep craters, and other defects usually require surgical approach.2. Pockets on teeth in which a complete removal of root irritants is not considered clinically possible may call for surgery. This occurs frequently in molar and premolar areas.
3. In cases of furcation involvement of grade II or III, a
surgical approach ensures the removal of irritants; any necessary root resection or hemisection also requires surgical intervention.4. Intrabony pockets on distal areas of last molars, frequently complicated by mucogingival problems, are usually unresponsive to nonsurgical methods.
5. Persistent inflammation in areas with moderate to deep pockets may require a surgical approach. In areas with shallow pockets or normal sulci, persistent inflammation may point to the presence of a mucogingival problem that needs a surgical solution.
METHODS OF POCKET THERAPY
1. New attachment techniques
offer the ideal result because they eliminate pocket depth by reuniting the gingiva to the tooth at a position coronal to the bottom of the preexisting pocket. New attachment is usually associated with filling in of bone and regeneration of periodontal ligament and cementum.2. Removal of the pocket wall
is the most common method. The wall of the pocket consists of soft tissue and may also include bone in the case of intrabony pockets. It can be removed by the following:• Retraction or shrinkage, in which scaling and root-planing procedures resolve the inflammatory process, and the gingiva therefore shrinks, reducing the pocket depth.
• Surgical removal performed by the gingivectomy technique or by means of an undisplaced flap.
• Apical displacement with an apically displaced flap.
3. Removal of the tooth side of the pocketwhich is accomplished by tooth extraction or by partial tooth extraction (hemisection or root resection).
METHOD SELECTION
Approaches to Specific Pocket ProblemsTherapy for Gingival Pockets. Two factors are taken into
consideration: (1) the character of the pocket wall and
(2) the accessibility of the pocket.
The pocket wall can be either edematous or fibrotic.
Edematous tissue shrinks after the elimination of local
factors, thereby reducing or totally eliminating pocket depth. Therefore scaling and root planing are the technique of choice in these cases.
Pockets with a fibrotic wall are not appreciably reduced in depth after scaling and root planing; therefore they are eliminated surgically.
Until recently, gingivectomy was the only technique available; it solves the problem successfully, but in cases of marked gingival enlargement (e.g., severe phenytoin enlargement), it may leave a
large wound that goes through a painful and prolonged healing process. In these patients, a modified flap technique can adequately solve the problem with fewer postoperative problems.
Therapy for Slight Periodontitis
In slight or incipient periodontitis, a small amount of bone loss has occurred, and pockets are shallow to moderate. In these patients, the conservativeapproach with good oral hygiene will generally suffice to control the disease. Incipient periodontitis that recurs in previously treated sites may require a thorough analysis of the causes for the recurrence.
Occasionally, a surgical approach may be required to correct the problem.
Therapy for Moderate-to-Severe Periodontitis in
Anterior Area.The anterior teeth are important esthetically;
therefore the technique that causes the least amount of visual root exposure should be considered.Anterior teeth offer two main advantages to a conservative approach:
(1) they are all single rooted and easily accessible and
(2) patient compliance and thoroughness in plaque control are easier to attain. Therefore scaling and root planing are the technique of choice for the anterior teeth.
Sometimes, however, a surgical technique may be necessary because of the need for improved accessibility for root planing or regenerative surgery of osseous defects. The papilla preservation flap is the first choice when a surgical approach is needed.
When the teeth are too close interproximally, the papilla preservation technique may not be feasible, and a technique that splits the papilla must be used. The sulcular incision flap offers good esthetic results and is the next choice.
When esthetics are not the primary consideration, the modified Widman flap can be chosen.
Therapy for Moderate-to-Severe Periodontitis inPosterior Area.
Treatment for premolars and molars usually
poses no esthetic problem but frequently involves difficult accessibility. Bone defects occur more often in the posterior than the anterior sector, and root morphologic features, particularly in relation to furcations, may offer insurmountable problems for instrumentation in a close field. Therefore surgery is frequently indicated in the posterior region.The purpose of surgery in the posterior area is either enhanced accessibility or the need for definitive pocket reduction requiring osseous surgery.
Accessibility can be obtained by either the undisplaced or the apically displaced flap.
Most patients with moderate to severe periodontitis have developed osseous defects that require some degree of osseous remodeling or reconstructive procedures.When osseous defects amenable to reconstruction are present, the papilla preservation flap is the technique of choice because it better protects the interproximal areas where defects are frequently present.
Second and third choices are the sulcular flap and the modified Widman flap, maintaining as much of
the papilla as possible.
When osseous defects with no possibility of reconstruc-tion are present, such as interdental craters, the technique of choice is the flap with osseous contouring.
To be continued……